Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Genetics | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Larqué AB. C3 glomerulonephritis / dense deposit disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneydensedepdisease.html. Accessed April 2nd, 2025.
Definition / general
- C3 related glomerulopathy manifested by broad, linear, extremely electron dense deposits with C3 within glomerular basement membrane, mesangium, Bowman capsule and tubular basement membrane (Colvin: Diagnostic Pathology - Kidney Diseases, 2nd Edition, 2015)
Essential features
- Rare C3 related glomerulonephritis affecting mostly children and older people
- Clinical syndrome of glomerulonephritis with low level of serum C3, related to abnormalities of alternative complement pathway
- Varied glomerular pathology by light microscopy with predominant C3 and little or no immunoglobulin deposition by immunofluorescence
- Hyperdense intramembranous deposits in the glomerular basement membrane by electron microscopy (pathognomonic)
- Recurs in almost all renal allografts
Terminology
- Membranoproliferative glomerulonephritis, type II
ICD coding
- ICD-10: N00-N08 - glomerular diseases
Epidemiology
- Rare; estimated at 1 - 3 cases/million (Kidney Int 2018;93:977)
- Mean age at diagnosis 19 years; 45 - 60% in children 5 - 15 years old; 40% > 60 years old (J Am Soc Nephrol 2005;16:1392)
- F:M = 1.5:2 (Kidney Int 2012;82:454)
Sites
- Kidney (glomerular disease)
Pathophysiology
- Chronic activation of alternative complement pathway by precipitant factors / autoantibodies / genetic predisposition, resulting in the accumulation of complement components in the tissue, recruitment of leukocytes and inflammatory damage of glomerulus (Pediatr Nephrol 2017;32:43)
Etiology
- Autoantibodies: C3 nephritic factor, autoantibodies to complement factor H, factor B or C3
- Genetic predisposition in complement component genes: CFH, CFI, C3, CFHR5 and factor H
- Precipitating factors: infection, post chemotherapy for breast cancer, monoclonal gammopathy
- Reference: Clin Exp Nephrol 2017;21:541
Clinical features
- Hematuria (~90%)
- Proteinuria (~95%) that may be in the nephritic range (~60%)
- Acute nephritic syndrome (~50%)
- Usually some degree of renal insufficiency
- Ocular drusen (yellow deposits) common
- Associated with acquired partial lipodystrophy (3 - 5%) (Nefrologia 2018;38:258)
- References: J Am Soc Nephrol 2005;16:1392, Pediatr Nephrol 2012;27:773
Diagnosis
- Clinical syndrome of glomerulonephritis
- Light microscopy: varied glomerular pathology
- Immunofluorescence microcsopy: C3 dominant glomerular staining and little or no immunoglobulin deposition (C3 staining intensity ≥ 2 orders of magnitude more than any other immune reactant on a scale of 0 - 3+) (Kidney Int 2013;84:1079)
- Electron microscopy: hyperdense intramembranous deposits in the glomerular basement membrane (pathognomonic)
Laboratory
- ↓ Serum C3 in ~80% of patients (↓ C3dg and C3d)
- More common in children (100%) than adults (40%)
- C3NeF (Ab to C3bBb) present in > 80%
- Persists in > 50%
- CFH mutations 17%
- Reference: Colvin: Diagnostic Pathology - Kidney Diseases, 2nd Edition, 2015
Prognostic factors
- Spontaneous remissions are uncommon (J Am Soc Nephrol 2005;16:1392)
- End stage renal disease occurs in 40 - 50% after 10 years (Pediatr Nephrol 2017;32:43)
- Best predictors of outcome are kidney function, degree of proteinuria and arterial hypertension at initial manifestation (Pediatr Nephrol 2017;32:43, Clin J Am Soc Nephrol 2014;9:46)
- In allografts, recurrence is the norm, typically in first 3 years, with a 50% graft failure rate (Clin J Am Soc Nephrol 2014;9:600)
Case reports
- 10 year old boy with dense deposit disease mimicking a renal small vessel vasculitis (J Am Soc Nephrol 2016;27:59)
- 11 year old girl with dense deposit disease treated with eculizumab (N Engl J Med 2012;366:1161)
- 12 year old boy with dense deposit disease and febrile sore throat (Saudi J Kidney Dis Transpl 2017;28:925)
- 52 year old man with dense deposit disease associated with monoclonal gammopathy (BMC Nephrol 2018;19:108)
- 63 year old woman with dense deposit disease associated with multiple myeloma (Clin Nephrol 2018;89:300)
Treatment
- At this time, there is no universally effective treatment
- Mycophenolate mofetil (MMF) and steroids (Clin J Am Soc Nephrol 2020;15:1287)
- Optimal blood pressure control (Kidney Int 2017;91:539)
- Steroids, immunosuppression (not yet proven effective) (Semin Nephrol 2013;33:493)
- Complement inhibitors such as eculizumab (anti-CD5Ab) under evaluation (Clin J Am Soc Nephrol 2012;7:748, Clin J Am Soc Nephrol 2015;10:1773)
- In patients with CFH mutations, plasma exchange and recombinant CFH (Colvin: Diagnostic Pathology - Kidney Diseases, 2nd Edition, 2015)
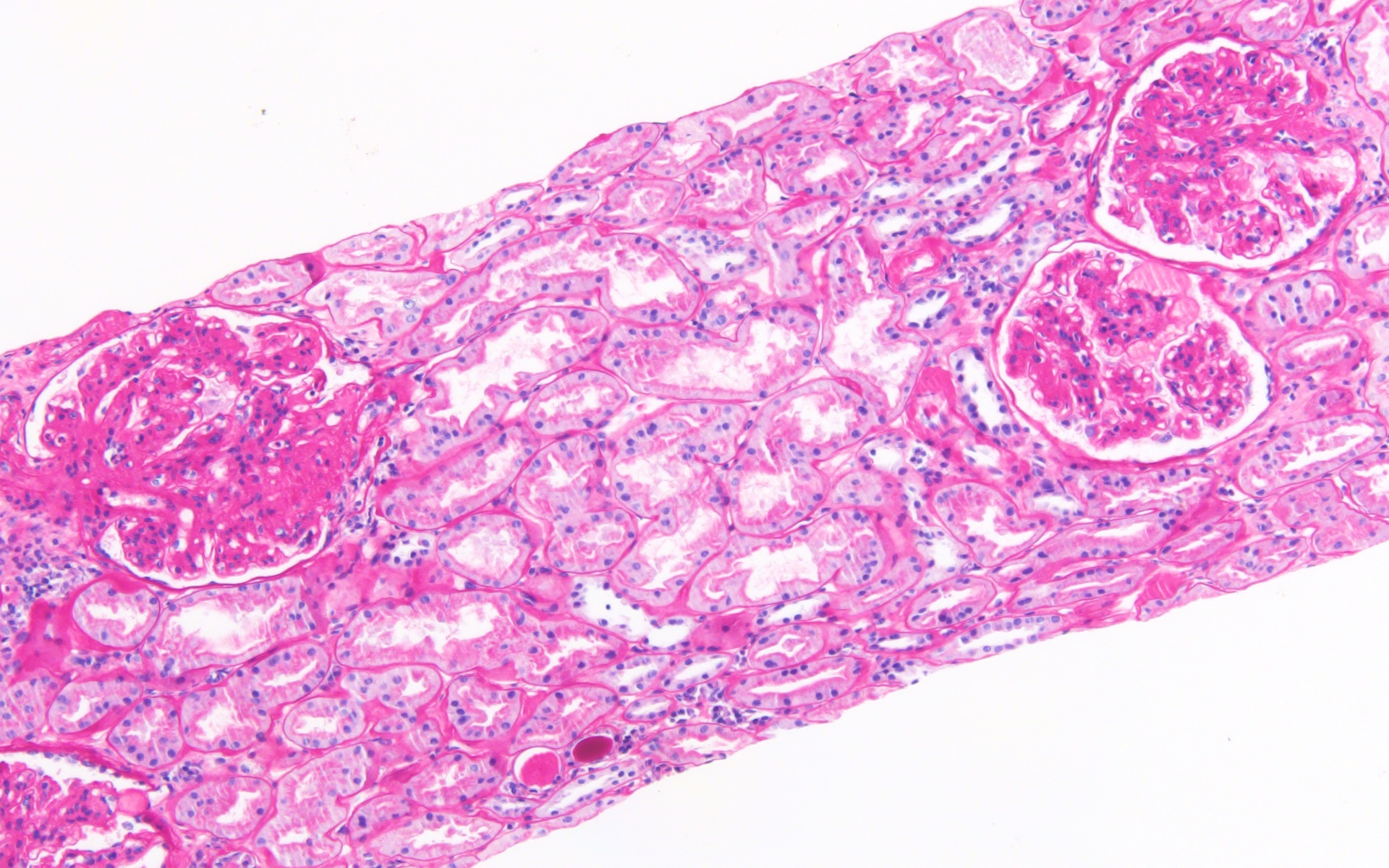
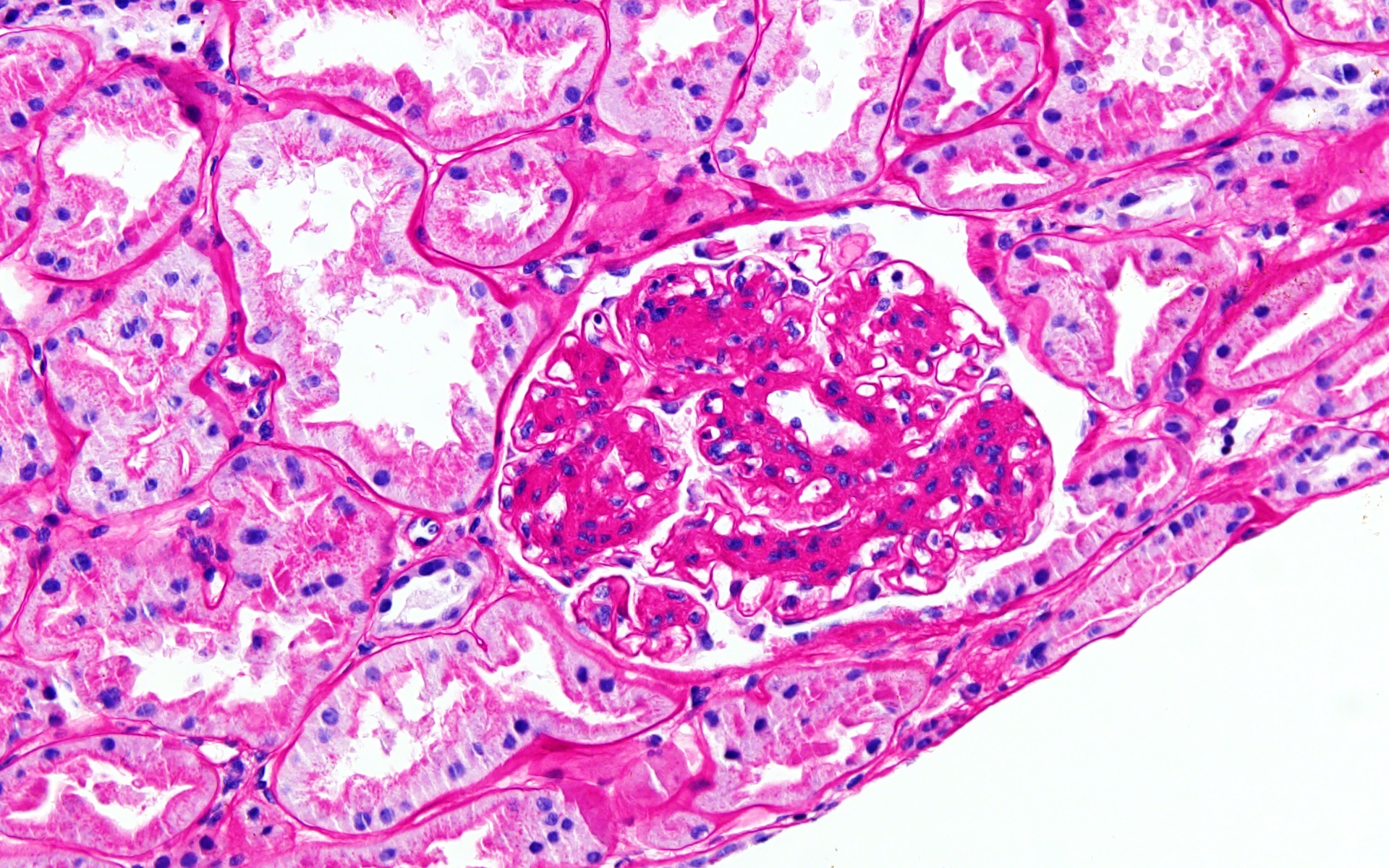
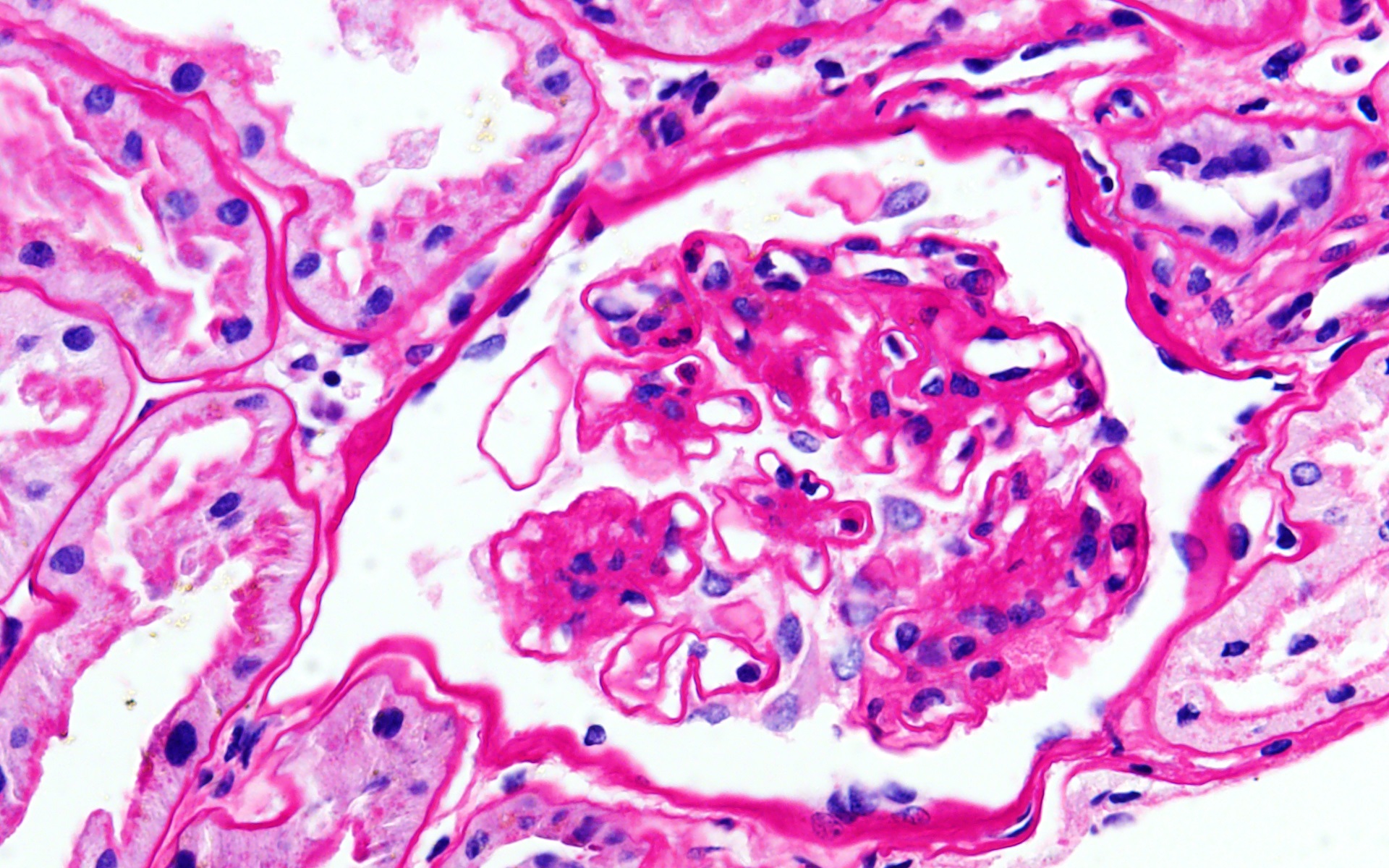
Microscopic (histologic) description
- Varied glomerular pathology (Mod Pathol 2007;20:605):
- Mesangial proliferation (30 - 50%)
- Membranoproliferative glomerulonephritis (25 - 45%)
- Acute exudative glomerulonephritis (10 - 20%)
- Crescentic glomerulonephritis (10 - 20%)
Microscopic (histologic) images
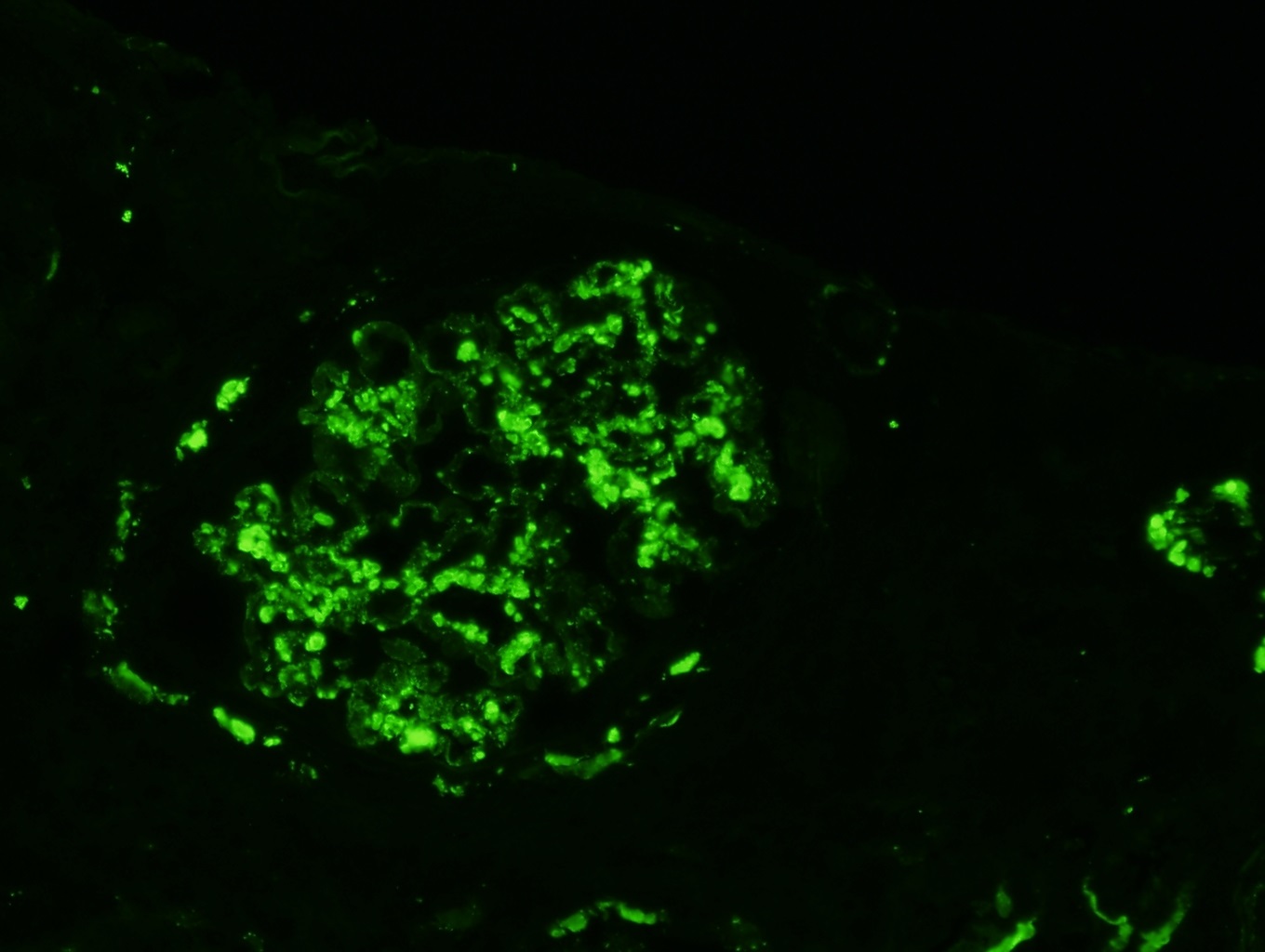
Immunofluorescence description
- Predominant C3 staining (ribbon-like [garland] pattern) in glomerular basement membranes with or without railroad track or double contour pattern along glomerular basement membranes; coarse mesangial spherules or ring-like deposits
- Focal Ig deposits in minority (almost always 2 levels of fluorescence intensity less than C3)
- Reference: Colvin: Diagnostic Pathology - Kidney Diseases, 2nd Edition, 2015
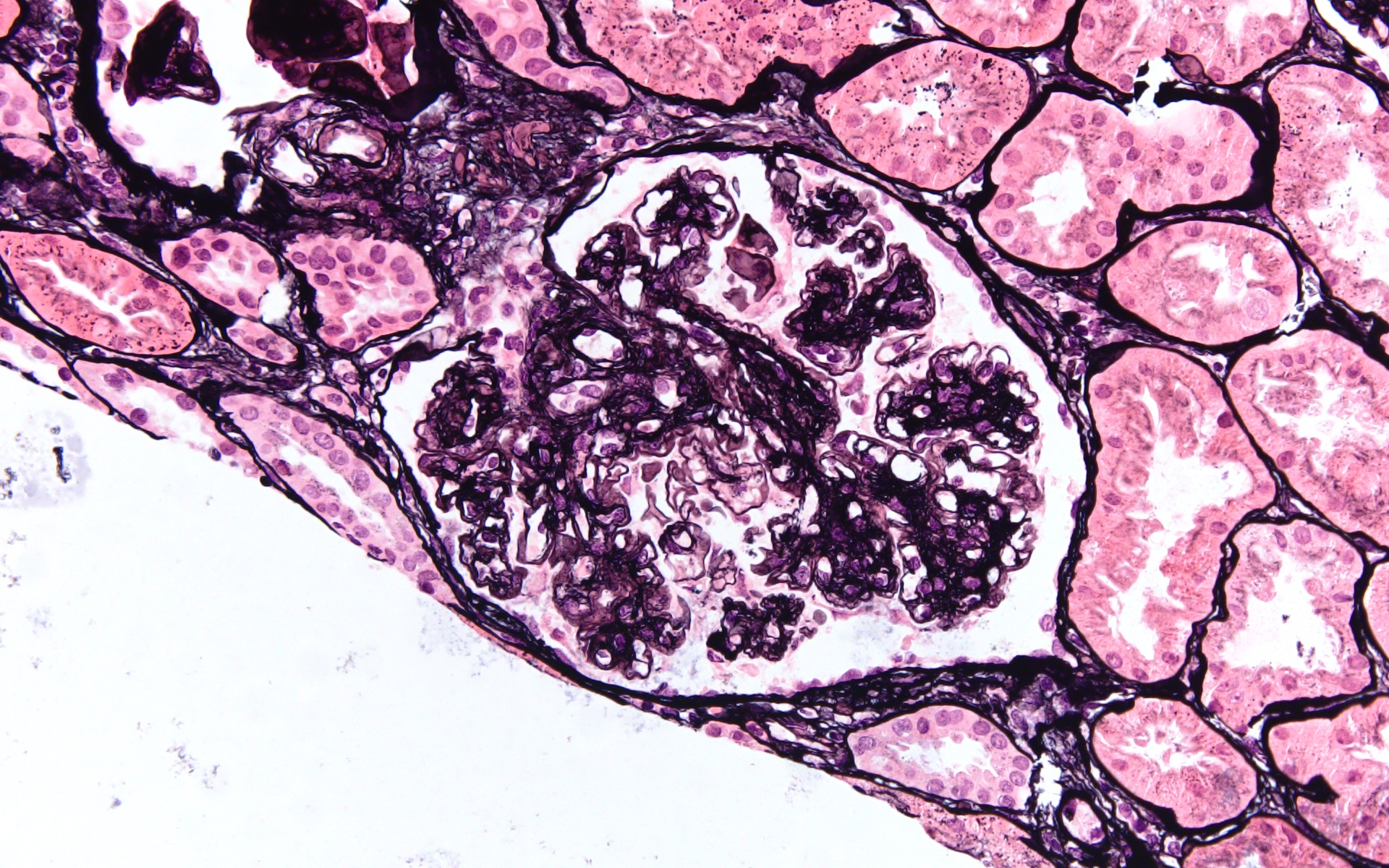
Positive stains
- Immunohistochemistry not used for diagnosis
- PAS, Jones silver and trichrome are used to evaluate morphology but are not specific for the type of glomerular disease
- Glomerular basement membranes are thickened, eosinophilic, refractile and brightly PAS+; fuchsinophilic on trichrome
- Reference: Zhou: Silva's Diagnostic Renal Pathology, 2nd Edition, 2017
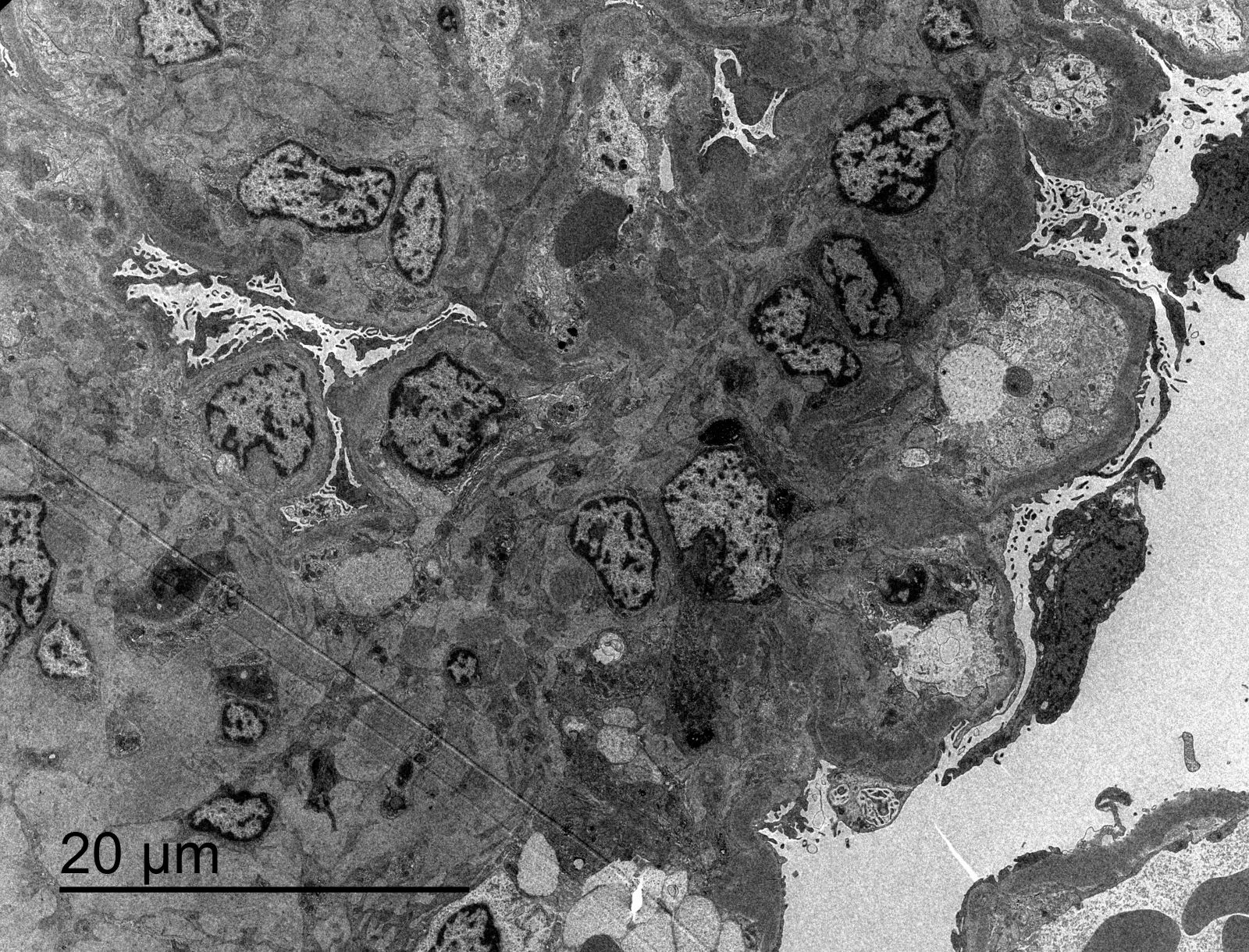
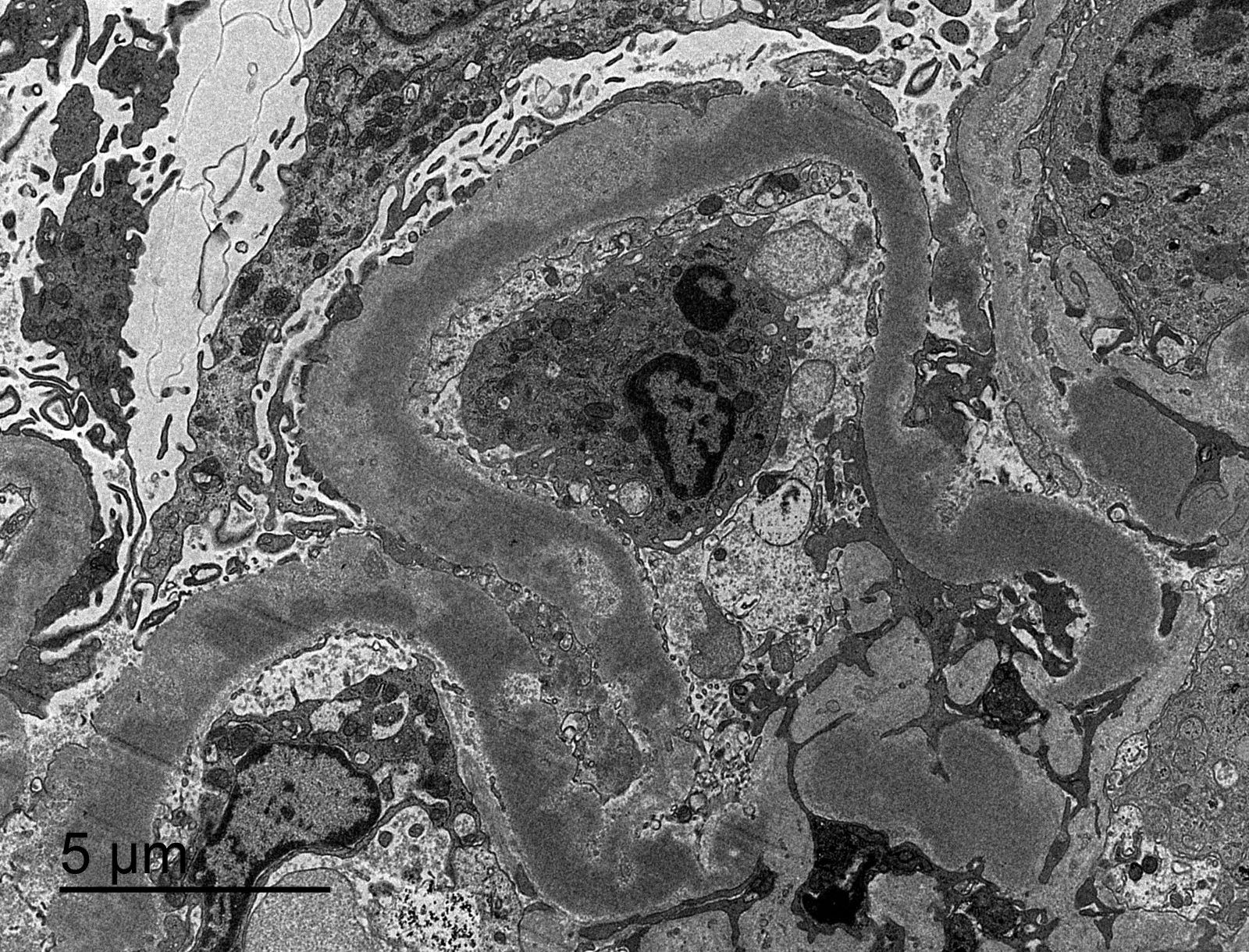
Electron microscopy description
- Accumulation in the glomerular basement membrane of uniquely electron dense material in a continuous, elongated, ribbon-like pattern or in small nodular aggregates within the irregularly thickened lamina densa; these dense deposits usually involve long segments of basement membrane but occasionally only a few loops are involved (sausage string pattern)
- Same type of deposit is characteristically also present in the mesangium, Bowman capsule, tubular basement membranes and occasionally in the walls of arterioles and peritubular capillaries
- Similar dense deposits have been noted in splenic sinusoidal basement membranes and in the eye involving the choriocapillaris basement membranes and Bruch membrane
- Podocyte injury eventually occurs
- Reference: Dickersin: Diagnostic Electron Microscopy - A Text/Atlas, 2nd Edition, 2000
Electron microscopy images
Genetics
- Genetic predisposition in complement component genes (CFH, CFI, C3, CFHR5 and factor H) (J Am Soc Nephrol 2007;18:2447)
Videos
Membranoproliferative GN
Sample pathology report
- Right kidney, biopsy:
- Dense deposit disease with C3 membranoproliferative glomerulonephritis pattern
- Adequacy: adequate (cortex 80%, medulla 20%)
- Microscopic description:
- 23 glomeruli, 4 of these with global sclerosis
- Majority of glomeruli showed a diffusely thick glomerular basement membrane and mesangial hypercellularity with increased mesangial matrix
- Some glomerular basement membrane showed double contour
- Fibrosis occupying 15% of the interstitium with minimal lymphoplasmacytic infiltrate
- Immunofluorescence microscopy:
- Number of glomeruli: 4
- All glomeruli showed granular C3 (+++) deposits in mesangium and capillary walls
- There were no deposits of IgA, IgM, IgG, C1q or fibrin
- Ultrastructural study:
- A glomerulus was evaluated that showed a preserved general structure with thickening of the basement membranes due to deposits in the lamina densa of glomerular basement membrane
- These deposits were extensive, of different thickness and showed a very electron dense appearance
- These morphological findings are characteristic of dense deposit disease
Differential diagnosis
- C3 glomerulonephritis:
- C3GN and DDD are a shared spectrum of disease: similar pathogenesis of aberrant activation of alterative complement pathway
- Similar light and immunofluorescence microscopy findings
- Lacks hyperdense deposits in densa lamina
- Monoclonal gammopathy of renal significance:
- C3 glomerulonephritis and dense deposit disease in older adults (≥ 65 years) is often associated with and may be driven by a monoclonal protein (Kidney Int 2018;94:178)
- Distinct from childhood form of C3GN and DDD; clone directed therapy should be considered (Kidney Int 2018;94:178)
- “Masked” monotypic immune deposits
- Paraffin immunofluorescence should be performed in older adults with C3GN / DDD to exclude masked monotypic deposits (Kidney Int 2015;88:867)
- Acute post-streptococcal or acute post-infectious glomerulonephritis:
- Post-infectious GN has prominent exudative features / neutrophilic influx, lacks chronic injury and often has a different clinical scenario
- IgG present and lacks hyperdense deposits in densa lamina
- Immunoglobulin mediated glomerulonephritis:
- Immune complex present, lacks hyperdense deposits in densa lamina
- Monoclonal Ig deposition disease:
- By definition, has Ig deposition (single light chain or heavy chain)
- C4 dense deposit disease:
- C4d present in deposits but little or no C3
- Lectin pathway activated rather than alternative pathway
Board review style question #1
Board review style answer #1
Board review style question #2
The final diagnosis of dense deposit disease is established based on
- Clinical symptoms alone
- Combination of clinical symptoms and light microscopy
- Electron microscopy
- Light microscopy alone
- Low C3 levels alone
Board review style answer #2