Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ibrahim DY. Hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyBMtransplant.html. Accessed December 24th, 2024.
Definition / general
- Definition: renal injury after hematopoietic stem cell transplantation (HSCT)
- It can be multifactorial; risk factors include radiotherapy, chemotherapy, nephrotoxic medications, infections and graft versus host disease
Essential features
- History of hematopoietic stem cell transplant
- Endothelial cell injury
- Bloodless glomerulus
- Arterial mucoid intimal thickening
- Subendothelial widening on electron microcopy
Terminology
- Bone marrow transplantation nephropathy
- Bone marrow transplantation associated thrombotic microangiopathy
- Radiation nephropathy / nephritis (old terminology)
ICD coding
- ICD-10
- Z94.81 - bone marrow stem cell transplantation status
- N17 - acute kidney failure
- N18.1 - chronic kidney disease, stage 1
- N18.2 - chronic kidney disease, stage 2 (mild)
- N18.3 - chronic kidney disease, stage 3 (moderate)
- N18.4 - chronic kidney disease, stage 4 (severe)
- N18.5 - chronic kidney disease, stage 5
- N18.6 - end stage renal disease
- N18.9 - chronic kidney disease, unspecified
Epidemiology
- 25 - 40% of patients received total body high dose radiation
- Pediatric patients have higher susceptibility (Int J Radiat Oncol Biol Phys 2017;99:486)
- Other risk factors include older age, female gender, unrelated donor transplant, high dose conditioning regimen, calcineurin inhibitor use and human leukocyte antigen (HLA) mismatch (Am J Kidney Dis 2013;61:809)
Sites
- Kidney
Pathophysiology
- Endothelial cell injury is the central and defining feature of hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA) (Mediterr J Hematol Infect Dis 2010;2:e2010033)
- Endothelial cell injury may result from multiple factors (Bone Marrow Transplant 2021;56:1805)
- Chemotherapy
- Infection
- Cyclosporine
- Conditioning regimen for HSCT
- Endothelial cell injury leads to endothelial cell activation and subsequent activation of platelets and the coagulation system
- Complement activation plays a significant role in HSCT-TMA (J Blood Med 2016:7:181)
Etiology
- Allogeneic HSCT is associated with a higher risk of acute kidney injury than autologous HSCT
- Acute kidney injury can be associated with medications such as myeloablative conditioning regimens and immunosuppressive agents, infections, acute graft versus host disease (GVHD), renal ischemia or total body irradiation (Am J Kidney Dis 2013;61:809)
- Chronic kidney injury has been associated with chronic GVHD, medications, acute injury, exposure to high dose radiation and total body irradiation
- Radiation dose thought to be implicated is 20 - 25 Gy to the kidneys for more than 1 month
Clinical features
- Renal dysfunction, hypertension, pedal edema, proteinuria, hematuria (Radiat Oncol 2021;16:43)
Diagnosis
- Imaging studies
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Renal ultrasound
- Percutaneous renal biopsy
Laboratory
- Laboratory workup includes (Nephron 1995;70:217)
- Serum creatinine
- Blood urea nitrogen (BUN)
- Urinalysis
- 24 hour urine
- Complete blood count (CBC)
- Peripheral blood smear
- Serologies (antinuclear antibody, antineutrophil cytoplasmic antibodies [ANCA], antiglomerular basement membrane, complement C3, C4)
Radiology description
- Can be normal (Kidney Int 2014;86:1063)
- Renal atrophy
- Renal scarring
- Cortical thinning (Wiad Lek 2022;75:128)
Prognostic factors
- Variable
- May lead to chronic kidney disease
Case reports
- 38 year old man presented with proteinuria and renal failure after allogeneic bone marrow transplantation from HLA identical sibling (Intern Med 1996;35:489)
- 51 year old woman presented with hematuria and low urine output 2 months after autologous bone marrow transplantation for acute lymphoblastic leukemia (Transplant Proc 2006;38:295)
- 54 year old man with IgG kappa multiple myeloma developed acute kidney injury after allogeneic hematopoietic stem cell transplant (Exp Hematol Oncol 2018:7:14)
Treatment
- Treatment modalities include (J Blood Med 2016:7:181)
- Supportive treatment
- Prednisone
- Plasma exchange
- Eculizumab (complement blocking therapy)
Microscopic (histologic) description
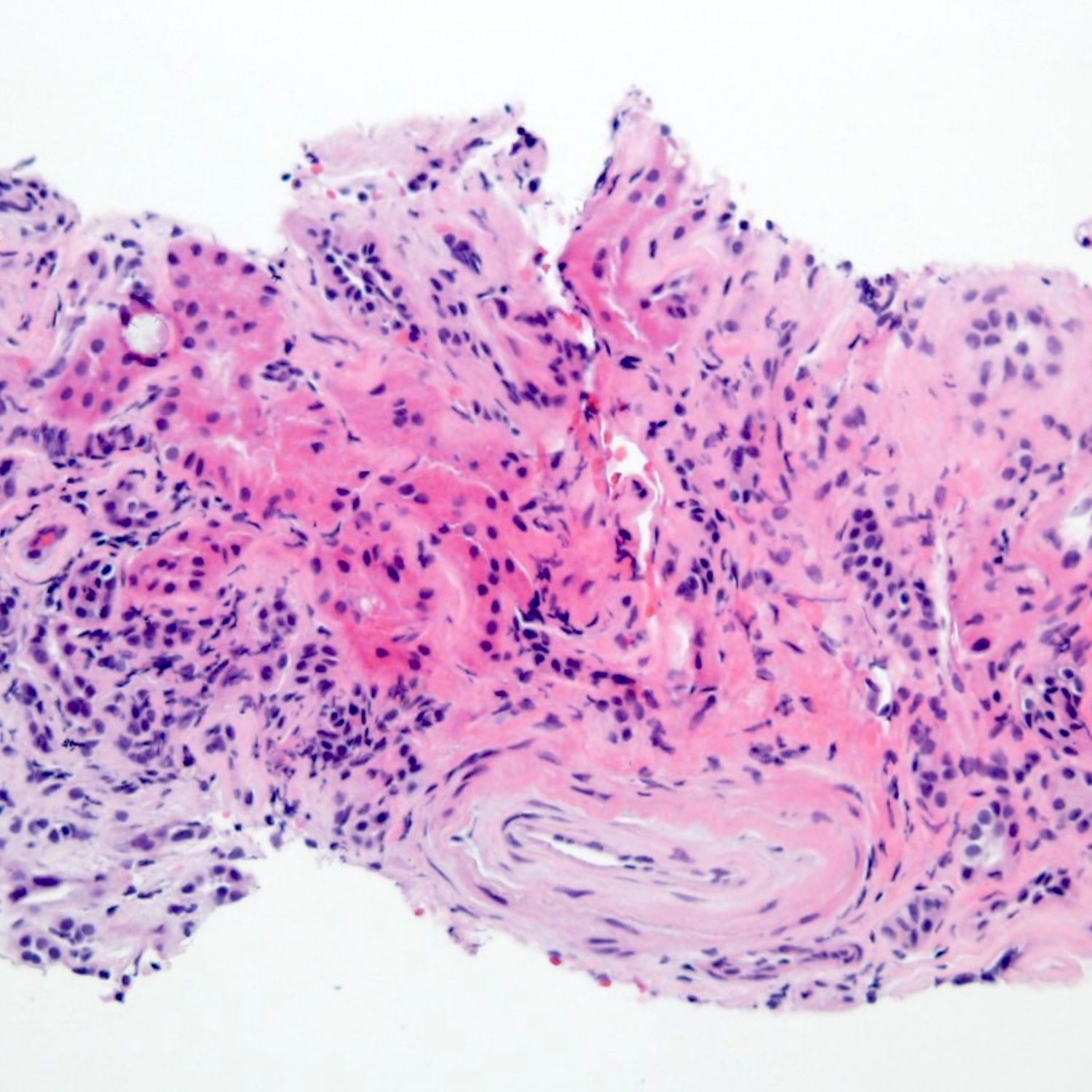
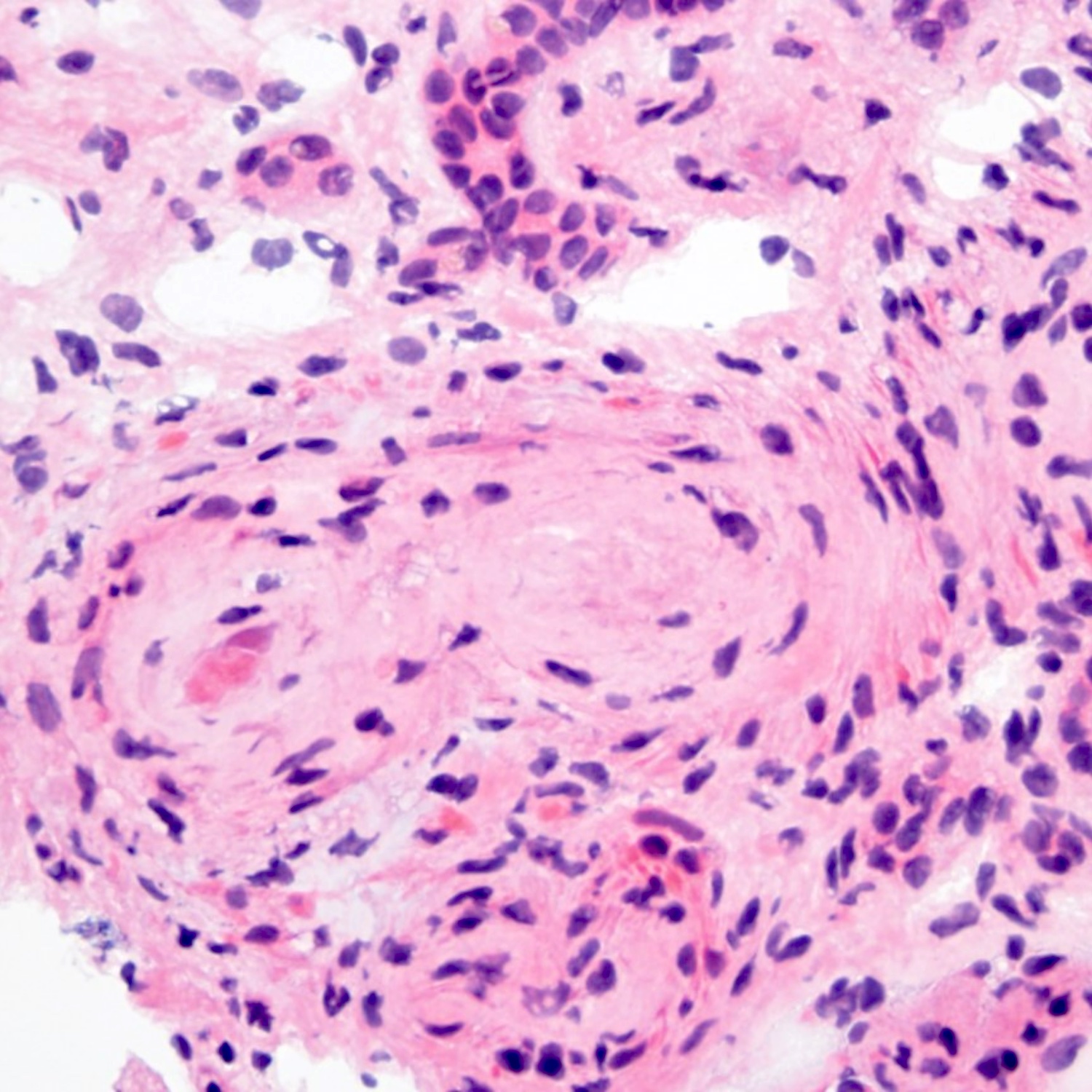
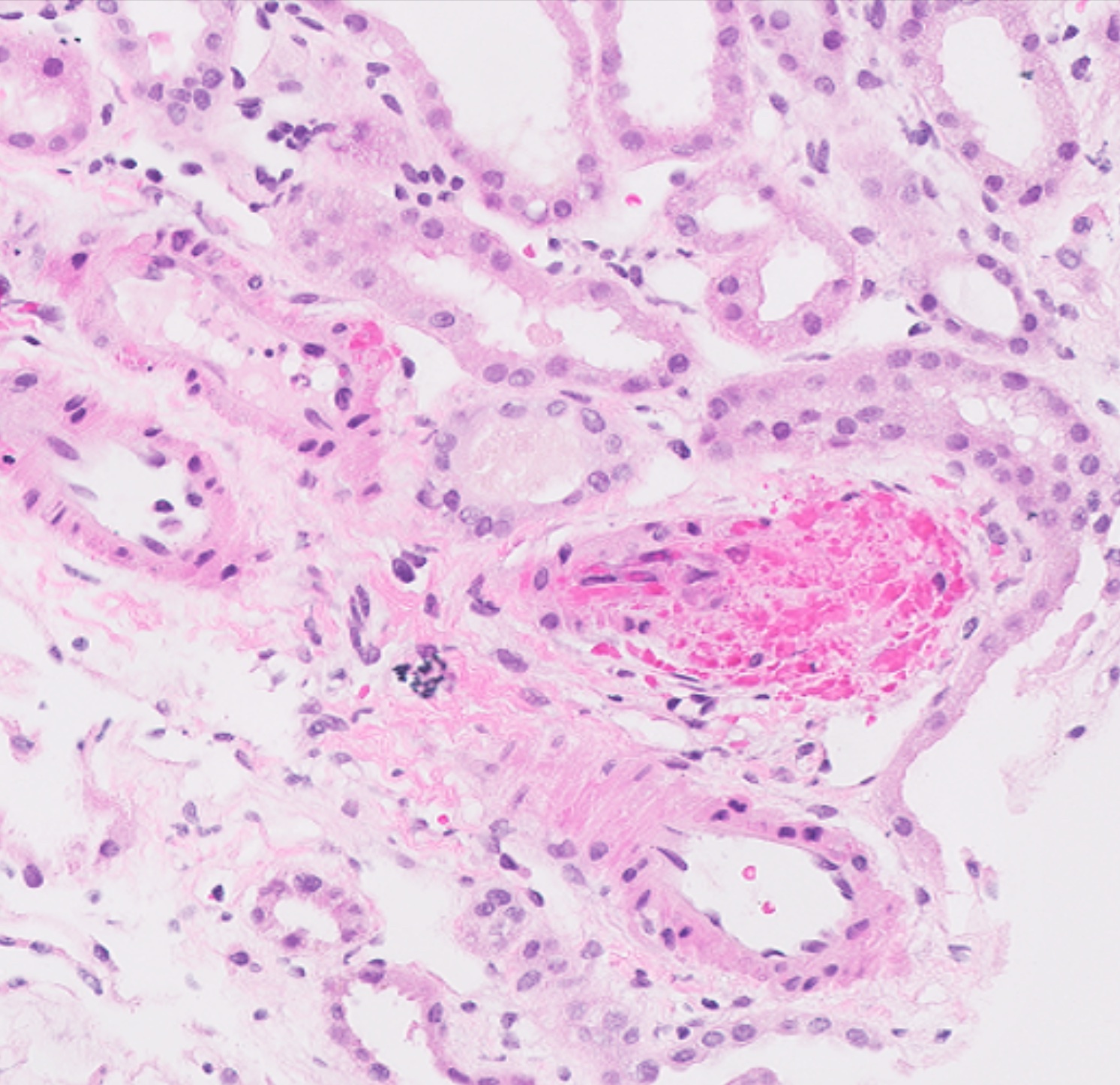
- Light microscopy examination (Mod Pathol 2008;21:396)
- Glomeruli
- Mesangiolysis
- Capillary thrombi
- Duplication of glomerular basement membrane (GBM), if chronic
- Global or segmental glomerular sclerosis
- Interstitium and tubules
- Interstitial edema
- Interstitial fibrosis and tubular atrophy
- Arteries and arterioles
- Mucoid intimal change
- Thrombi
- Hyalinosis
- Glomeruli
Microscopic (histologic) images
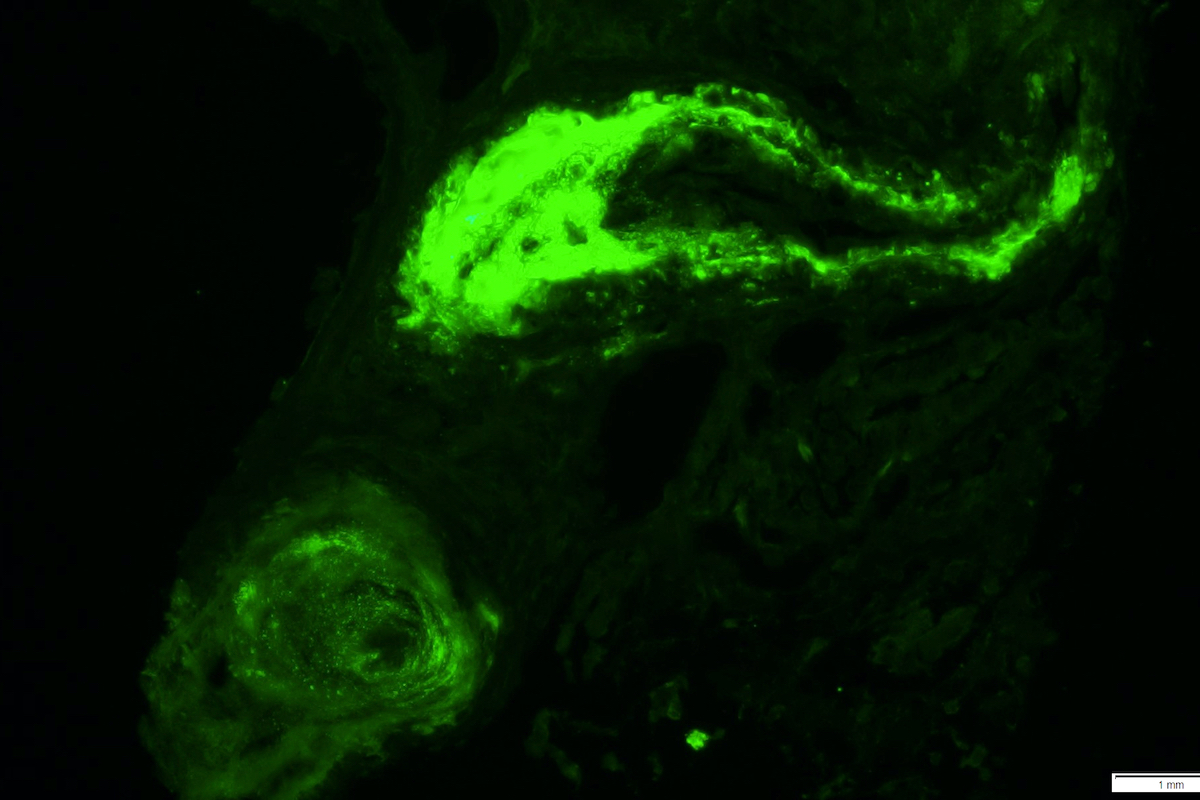
Immunofluorescence description
- Fibrinogen highlights thrombi
- IgM and C3 may show nonspecific trapping along GBMs and arterioles
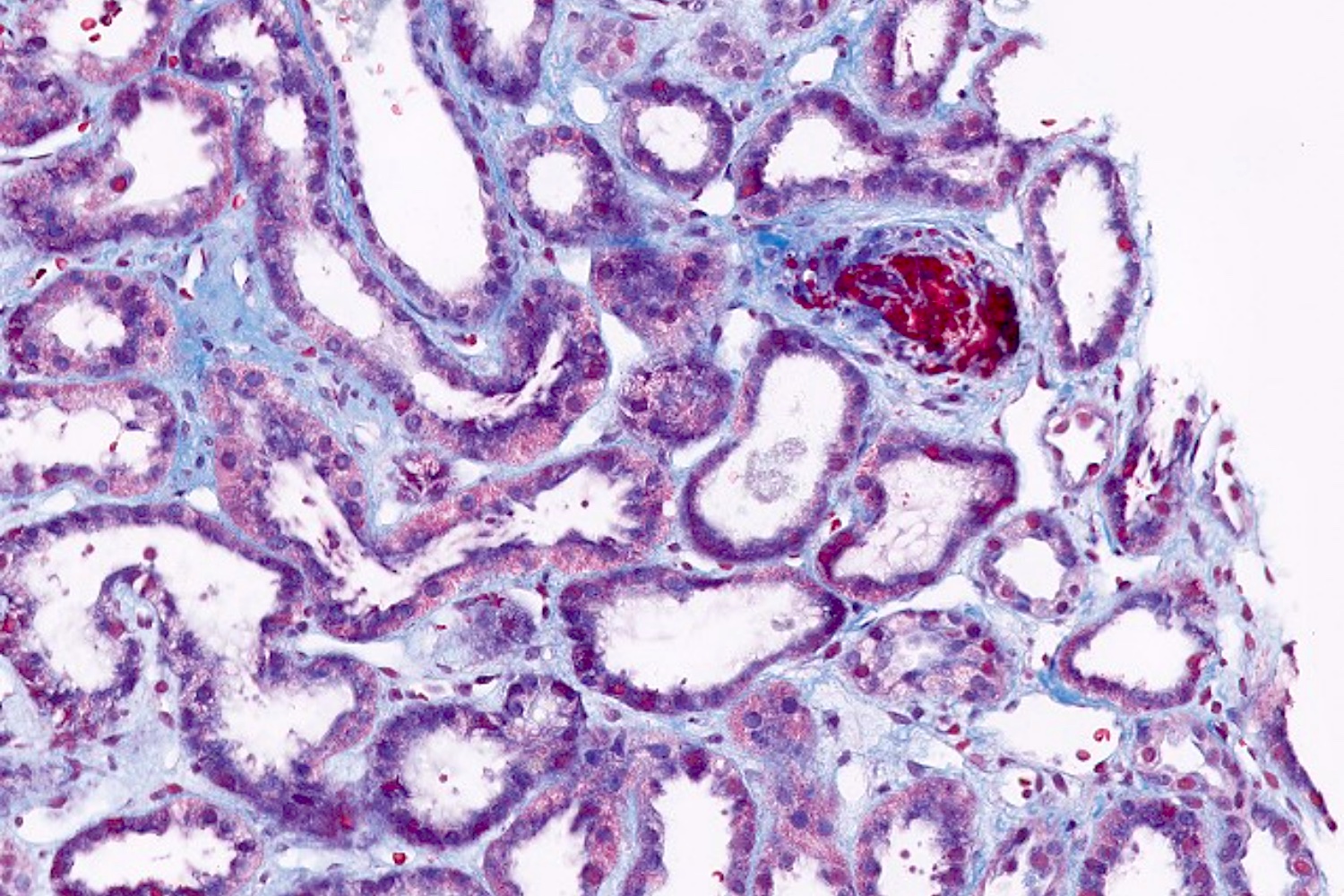
Positive stains
- Special stains: Masson trichrome stains fibrin thrombi strongly red
- CD61 highlights the platelets in thrombi
Electron microscopy description
- Separation of endothelial cells from GBM with widening of subendothelial space by electron lucent material
- Duplication of GBM, if chronic
Electron microscopy images
Sample pathology report
- Kidney, left, core biopsy:
- Acute thrombotic microangiopathy (see comment)
- Comment: The arteries show mucoid intimal thickening with focal fibrinoid necrosis of the wall and luminal thrombi. These findings are consistent with thrombotic microangiopathy. Due to the patient's history of allogenic hematopoietic stem cell transplant and exposure to radiation, this is most likely the underlying cause.
Differential diagnosis
- Thrombotic thrombocytopenic purpura:
- Associated with low ADAMTS13 levels or activity
- Hemolytic uremic syndrome:
- Enterohemorrhagic E. coli (O157:H7)
- Thrombotic microangiopathy from various causes such as drugs:
- Clinical correlation is necessary to identify the possible offending drug
- Examples include gemcitabine and cyclosporine
- Atypical hemolytic uremic syndrome (complement mediated TMA):
- Genetic or acquired abnormalities in alternative complement pathway
- Graft versus host glomerulopathies:
- Include membranous glomerulonephritis and minimal change disease
- Can also present similarly with thrombotic microangiopathy
Board review style question #1
A 65 year old woman with a history of hematopoietic stem cell transplant presented with acute renal failure. She underwent a percutaneous renal biopsy. The H&E of the biopsy is shown in the image above. Immunofluorescence was negative. What is the most likely diagnosis?
- Bone marrow transplant nephropathy
- Glomerulus looks normal
- Membranoproliferative pattern of injury
- Membranous nephropathy
Board review style answer #1
A. Bone marrow transplant nephropathy. The patient's history of hematopoietic stem cell transplant together with the glomerulus demonstrating amorphous material occluding the capillary loops (bloodless glomeruli) makes bone marrow transplant neuropathy the most likely diagnosis. Answer D is incorrect because in membranous nephropathy, the glomerulus would show thickening of the basement membrane and glomerular granular IgG staining on immunofluorescence. Answer B is incorrect because the glomerulus shown is not normal. Answer C is incorrect because in cases with membranoproliferative pattern of injury, the glomerulus would demonstrate mesangial and endocapillary hypercellularity and immunofluorescence would be positive for IgG and C3.
Comment Here
Reference: Hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA)
Comment Here
Reference: Hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA)
Board review style question #2
Which of the following is most likely to be seen in a renal biopsy of a patient presenting with hematuria after bone marrow transplant and high dose radiation?
- Focal segmental glomerulosclerosis (FSGS)
- IgA glomerulonephritis
- Minimal change disease
- Thrombotic microangiopathy
Board review style answer #2
D. Thrombotic microangiopathy.
Of all the choices, bone marrow transplantation and high dose radiation are known to be associated with thrombotic microangiopathy.
Answer C is incorrect because rare cases of bone marrow transplant have been associated with secondary form of membranous glomerulonephritis. However, it is not known to be associated with minimal change disease.
Answer A is incorrect because bone marrow transplant and radiation therapy have not been associated with focal segmental glomerulosclerosis (FSGS).
Answer B is incorrect because bone marrow transplant and radiation therapy have not been associated with IgA glomerulonephritis.
Comment Here
Reference: Hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA)
Comment Here
Reference: Hematopoietic stem cell transplantation associated thrombotic microangiopathy (HSCT-TMA)