Table of Contents
Definition / general | Essential features | Terminology | Applications | Implementation | Validation | Data security and privacy | Obstacles to implementation | Advantages | Limitations | Diagrams / tables | Clinical images | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4Cite this page: Saleh J, Borys D, Tanveer N. Teledermatopathology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/informaticsteledermgen.html. Accessed March 31st, 2025.
Definition / general
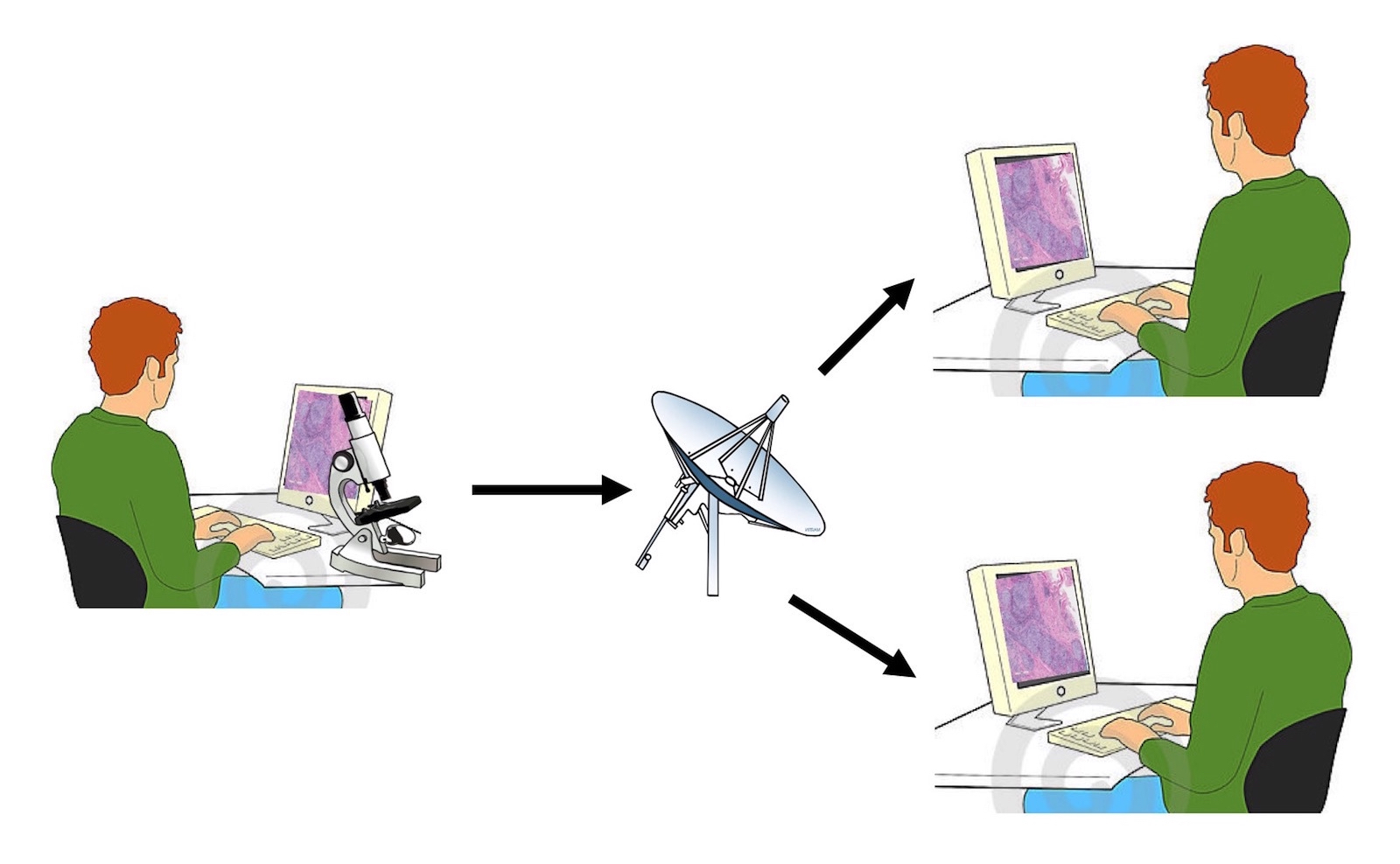
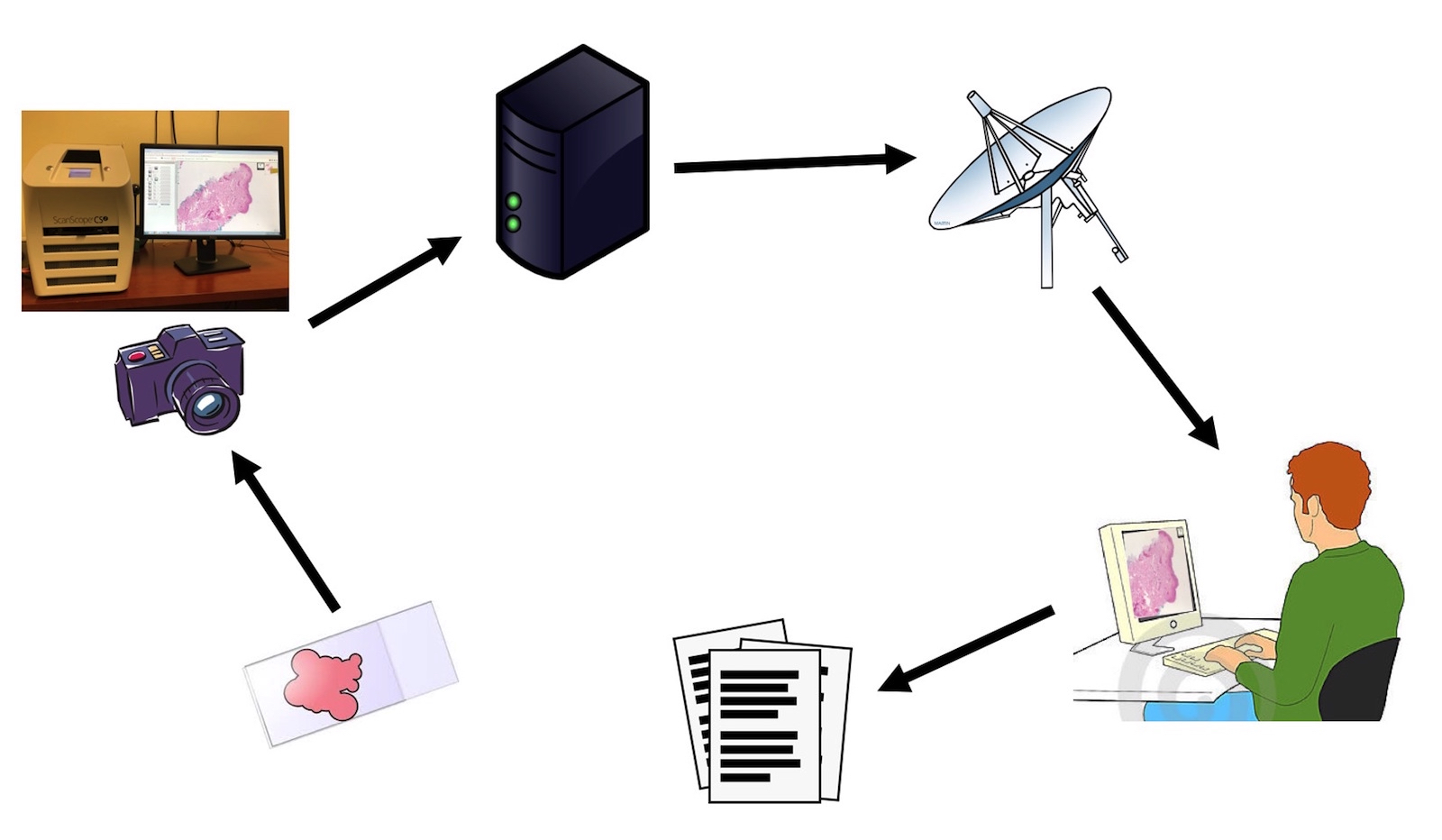
- Digital transfer of image rich dermatopathology data using telecommunication technology
- Classified into real time, store and forward or hybrid
Essential features
- Goal is to provide the highest quality of dermatologic care by moving patient information efficiently (Semin Cutan Med Surg 2002;21:179)
- Composed of telecommunication lines, a virtual slide system and a public web server (Diagn Pathol 2012;7:177)
- Implementation requires adequate infrastructure, internet connectivity and healthcare provider basic training related to imaging and storage (BMC Res Notes 2014;7:588)
Terminology
- Interchangeable terms may include digital pathology, digital microscopy, teleconference, teleconsultation, virtual microscopy and whole slide imaging (J Pathol Inform 2010;1:15)
- Virtual slide system: an automated scanner that digitizes microscopic slides into high resolution images
- Mobile / smart teledermatopathology: the use of a smartphone camera to acquire dermatopathology images and the use of smartphone or tablet to retrieve image rich slides from digital server (J Cutan Pathol 2013;40:513)
- Morrison technique: a freehand method of using a smartphone without adaptor for taking images for telepathology (J Cutan Pathol 2016;43:472)
- Real time (dynamic): live images are examined in real time, using a telecommunications link (J Pathol Inform 2010;1:15)
- Robotic: utilizes a remote controlled microscope and video conferencing equipment (J Am Acad Dermatol 2014;70:952)
- Nonrobotic: the pathologist asking for a second opinion broadcasts the live video by videoconferencing application and moves the slide on the microscope stage according to the requests of the reporting pathologist (Hum Pathol 2018;78:144)
- Space independent but not time independent (Curr Dermatol Rep 2016;5:96)
- Both parties must be available at the same time
- May interrupt the routine workflow and make scheduling challenging
- Store and forward (static): referring providers transmit the digitalized images to consulting pathologists by email or web based uploading systems (Curr Dermatol Rep 2016;5:96)
- Uses a microscopy camera, smartphone camera with or without adaptor or automated scanner
- Space and time independent (Curr Dermatol Rep 2016;5:96)
- Does not require simultaneous presence of both parties
- Compared to real time, store and forward is less interactive (Curr Dermatol Rep 2016;5:96, J Pathol Inform 2010;1:15)
- Creates flexibility
- Shorter consultation time
- Less expensive
- Higher resolution digital images
- No or minimal interaction
- Delayed responses
- Consulting pathologist has no control over the magnification at which the images are captured; there are limited fields of view to examine
- Most commonly used modality of teledermatopathology (Curr Dermatol Rep 2016;5:96)
- This technique has been used in Alaska Federal Health Care Access Network, Medweb, TeleDerm Solutions and Second Opinion (Curr Dermatol Rep 2016;5:96)
Applications
- Communication with dermatologists and dermatopathologists in remote locations
- Consultations for rural and underserved areas lacking access of specialists
- Consultations for second opinion
- Utilization of image analysis software and computer aided diagnostic tools to enhance diagnostic accuracy
- Collaborative diagnostic research, tumor boards and scholastic endeavors
- Real time (BMC Res Notes 2014;7:588)
- Enables direct interaction between medical providers and pathologists
- Facilitates education for providers
- Allows for instant clarification of any issues that may arise
- Store and forward (BMC Res Notes 2014;7:588)
- Useful when physicians and pathologists have difficulty coordinating for in person or real time consultation
- Beneficial for low resource settings
- Educational tool to improve the clinical acumen of medical students, residents and practicing dermatologists and pathologists (Int J Dermatol 2018;57:1358)
- Tool for sharing cases on social media for second opinion and teaching learning activities (Ann Fam Med 2021;19:24)
- Intraoperative frozen section consultation for margin status for melanoma surgery (Eur J Surg Oncol 2021;47:1140)
Implementation
- Evaluation criteria before implementing teledermatopathology (including but not limited to) (Telemed J E Health 2010;16:424)
- Technical resources required
- Ability to store and transmit digital images, clinical history and consultant's diagnosis and recommendations in an organized fashion
- User friendliness and intuitiveness of the application
- Integration with existing electronic medical record (EMR) systems
- Scalability and ability to fit into organization
- Billing
- Cost of equipment
- Steps to incorporate teledermatopathology into practice (Semin Cutan Med Surg 2002;21:179)
- Understand how the organization delivers care
- Analyze the alternatives (i.e., cost benefit analysis)
- Obtain organizational support
- Formulate an execution plan
- Train staff
- Monitor the process and analyze outcomes (i.e., turnaround times)
Validation
- The College of American Pathologists in collaboration with the Association for Pathology Informatics and the American Society for Clinical Pathology have updated the guidelines for validating whole slide imaging systems for pathology diagnosis (Arch Pathol Lab Med 2022;146:440)
- 3 major recommendations and 9 good practice statements
- Good practice statements are statements that are not evidence based but they are likely to do more good than harm (Arch Pathol Lab Med 2022;146:440)
- 3 major recommendations are
- At least 60 cases for 1 use case or 1 application in validation set
- Must cover the entire spectrum of cases likely to be encountered in the routine practice
- Another 20 cases for additional applications like immunohistochemistry or special stains if not included in validation set
- Only intraobserver concordance considered for validation, if < 95%, appropriate remedial steps taken
- Minimum wash out period of 2 weeks to avoid recall bias for the validation study (Arch Pathol Lab Med 2022;146:440)
- At least 60 cases for 1 use case or 1 application in validation set
Data security and privacy
- Practicing telepathologists should also conform to the state and federal data security and privacy laws including Health Insurance Portability and Accountability Act (HIPAA)
- All data transmission in telepathology should use encryption that meets required standards
- Confidential data should only be stored in secure data storage locations (J Pathol Inform 2014;5:39)
Obstacles to implementation
- Varying reimbursements by insurance provider and state (Dermatol Pract Concept 2018;8:214)
- Privacy and security (Dermatol Pract Concept 2018;8:214)
- Legal risks (Curr Dermatol Rep 2016;5:96)
- Ethical issues (J Pathol Inform 2010;1:15)
- Lack of uniform technology
- Healthcare provider training
Advantages
- Improves access to specialists as the number of dermatopathologists is limited and unevenly distributed geographically
- Enhances quality of care and efficiency of workflow
- Reduces interpretive errors and optimizes patient outcomes
- Minimizes healthcare expenditures
- Facilitates international collaboration
- Prevents service disruption or loss
- Reduces pathologists' travel time (Am J Dermatopathol 2018;40:667)
Limitations
- Quality of images (Am J Dermatopathol 2018;40:667)
- Diagnostic reliability is comparable with conventional microscopes
- Concordance rates 73 - 100%
- Most studies conclude that the image quality is adequate for microscopic examination of melanocytic and inflammatory skin diseases
- May be more difficult to grade melanocytic dysplasia and identify eosinophils, neutrophils, melanin granules and apoptosis
- Images may be out of focus and require rescanning
- Certain dermatopathological features are too subtle to be picked up on static images
- Diagnostic reliability is comparable with conventional microscopes
- Possible technical issues (J Pathol Inform 2010;1:15)
- Networks with bandwidth limitations
- Firewalls that may block signals for remote device controls
- Computer or scanner malfunction
- Image deficiencies
- Corrupted images
- Images with poor resolution
- Potential technical delays (J Pathol Inform 2010;1:15)
- Waiting for images to download
- Pixelating images when zooming
- Slow internet connection
Clinical images
Board review style question #1
Which of the following is true about teledermatopathology?
- Does not increase access to specialists
- Facilitates international collaboration and widens global access to specialists
- Has a poor diagnostic concordance
- Increases interpretive errors
Board review style answer #1
B. Facilitates international collaboration and widens global access to specialists. Teledermatopathology helps pathologists to discuss cases with specialists from other states or countries. Answer A is incorrect because teledermatopathology improves access to specialists. Answer C is incorrect because teledermatopathology has a good diagnostic concordance. Answer D is incorrect because teledermatopathology reduces interpretive errors by facilitating a second opinion.
Comment Here
Reference: Teledermatopathology
Comment Here
Reference: Teledermatopathology
Board review style question #2
Which of the following is the most commonly used modality in teledermatopathology?
- Hybrid
- In person consultation
- Real time
- Store and forward
Board review style answer #2
D. Store and forward. Store and forward is widely used due to its ease of application. Answer A and C are incorrect because they are used less often. Answer B is incorrect since it is not a modality for teledermatopathology.
Comment Here
Reference: Teledermatopathology
Comment Here
Reference: Teledermatopathology
Board review style question #3
A dermatologist sends the patient’s clinical history and microscopic images of her dermatologic condition to a pathologist, who subsequently views them and provides diagnosis and recommendations. Which of the following modalities did these physicians use?
- Hybrid
- In person consultation
- Real time
- Store and forward
Board review style answer #3
D. Store and forward. The images are first stored on the dermatologists computer or mobile phone and then forwarded to the pathologist for opinion. Answer A is incorrect because only one modality is being used to share the static images. Answer B is incorrect because the consultation is online and not in person. Answer C is incorrect because the live images are not being sent in real time.
Comment Here
Reference: Teledermatopathology
Comment Here
Reference: Teledermatopathology
Board review style question #4
A dermatologist emails a pathologist with the patient’s clinical history and microscopic images of her dermatologic condition. The pathologist reviews the information and responds to the email with diagnosis and recommendations. He also sets up a video consultation with the dermatologist. Which of the following modalities best describes the method used by the physicians in this scenario?
- Hybrid
- In person consultation
- Real time
- Store and forward
Board review style answer #4
A. Hybrid. 2 modalities are being used to discuss the case, static images (store and forward) and video consultation (real time). Answer B is incorrect answer because the meeting is taking place online and not in person. Answer C is incorrect because both static images and videoconferencing are being used to discuss the case. Answer D is incorrect because store and forward technique is being used in conjunction with videoconferencing.
Comment Here
Reference: Teledermatopathology
Comment Here
Reference: Teledermatopathology