Table of Contents
Definition / general | Essential features | Small lymphocytes | Intermediate sized cells | Plasma cells | Large lymphocytes | Blasts | Diagrams / tables | Peripheral smear images | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Li J, Pozdnyakova O. Neoplastic WBC. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/hematologyneoplasticWBC.html. Accessed November 27th, 2024.
Definition / general
- Neoplastic hematolymphoid cells circulating in the peripheral blood
Essential features
- Morphologic identification of neoplastic hematolymphoid cells on peripheral blood smears
Small lymphocytes
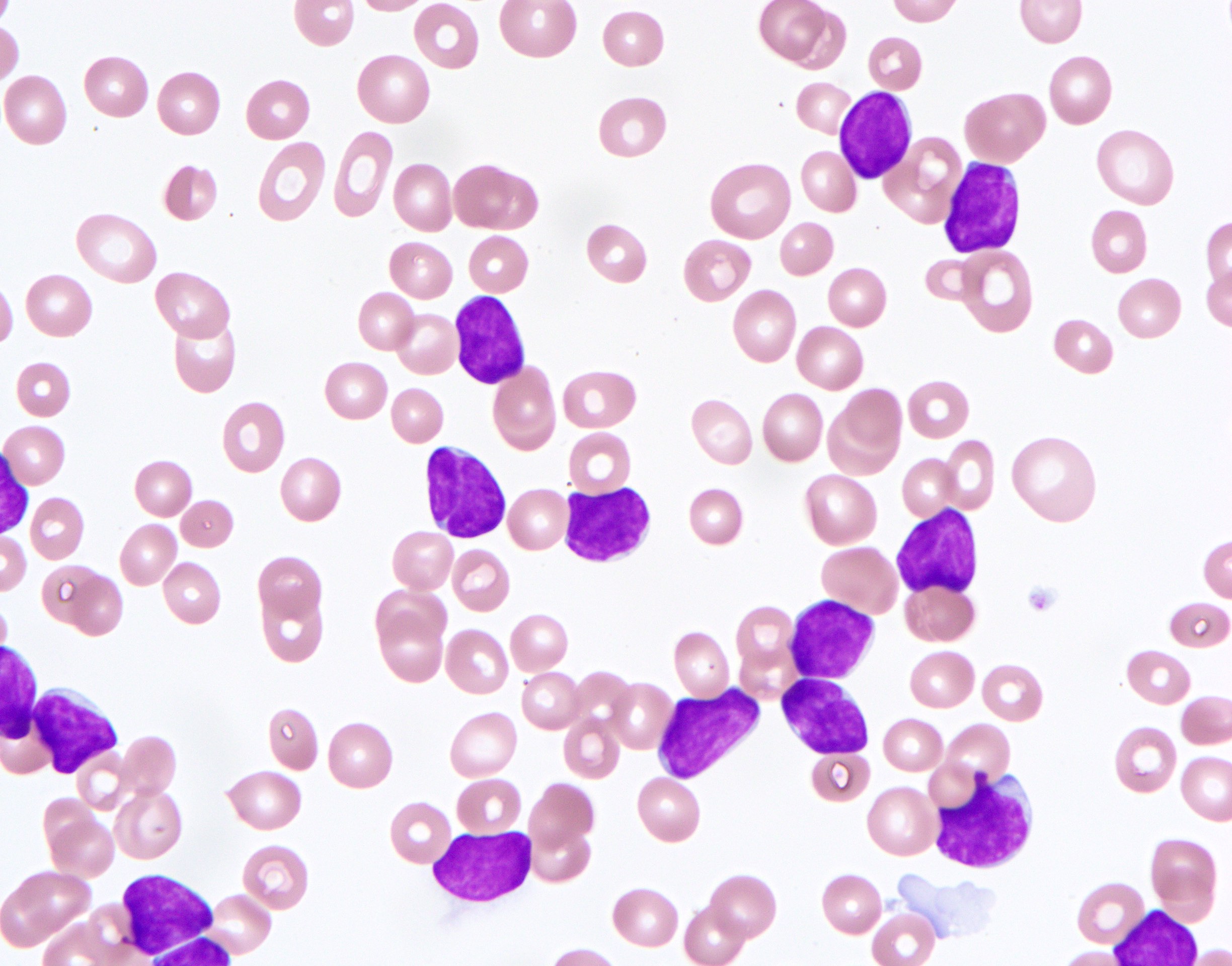
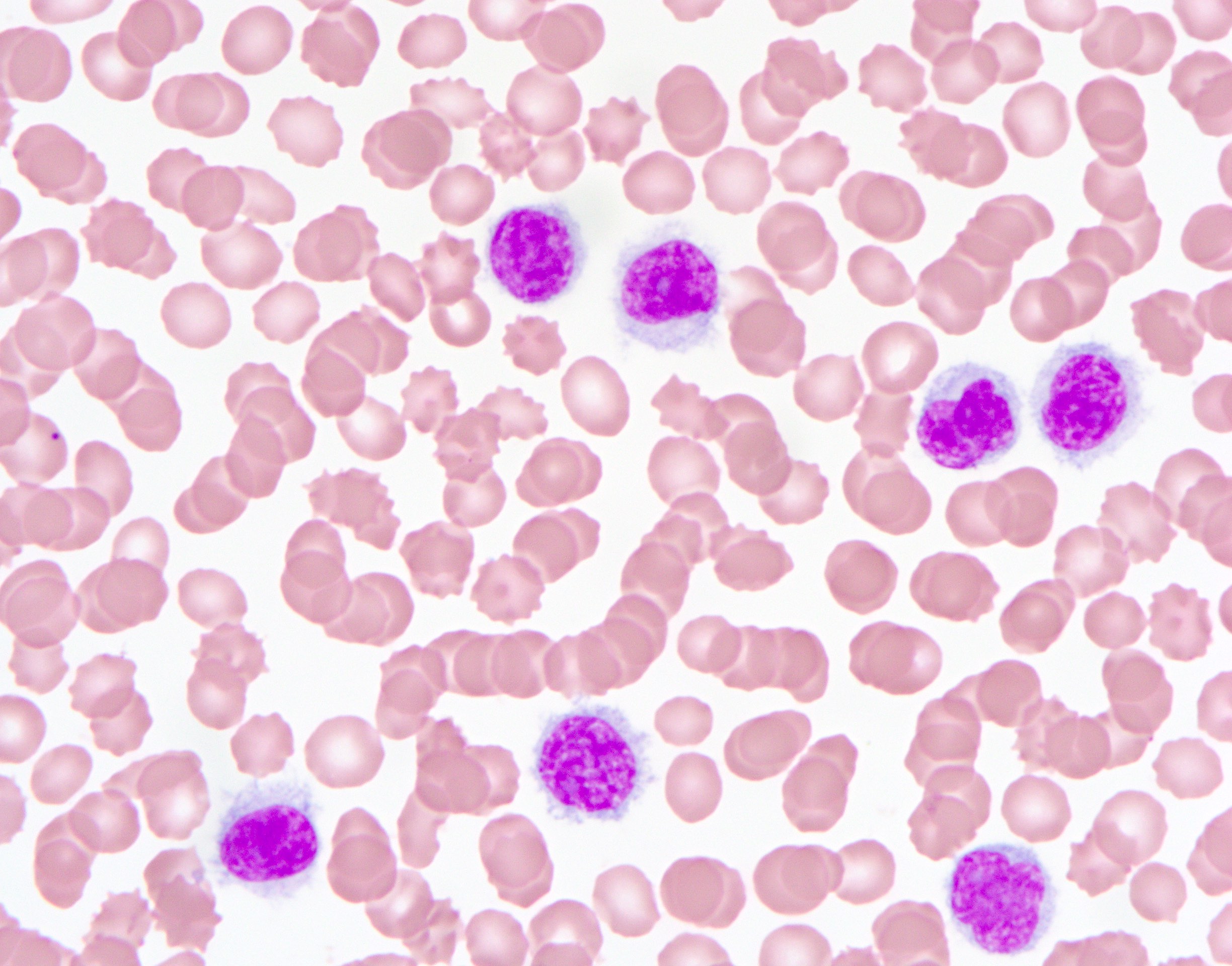
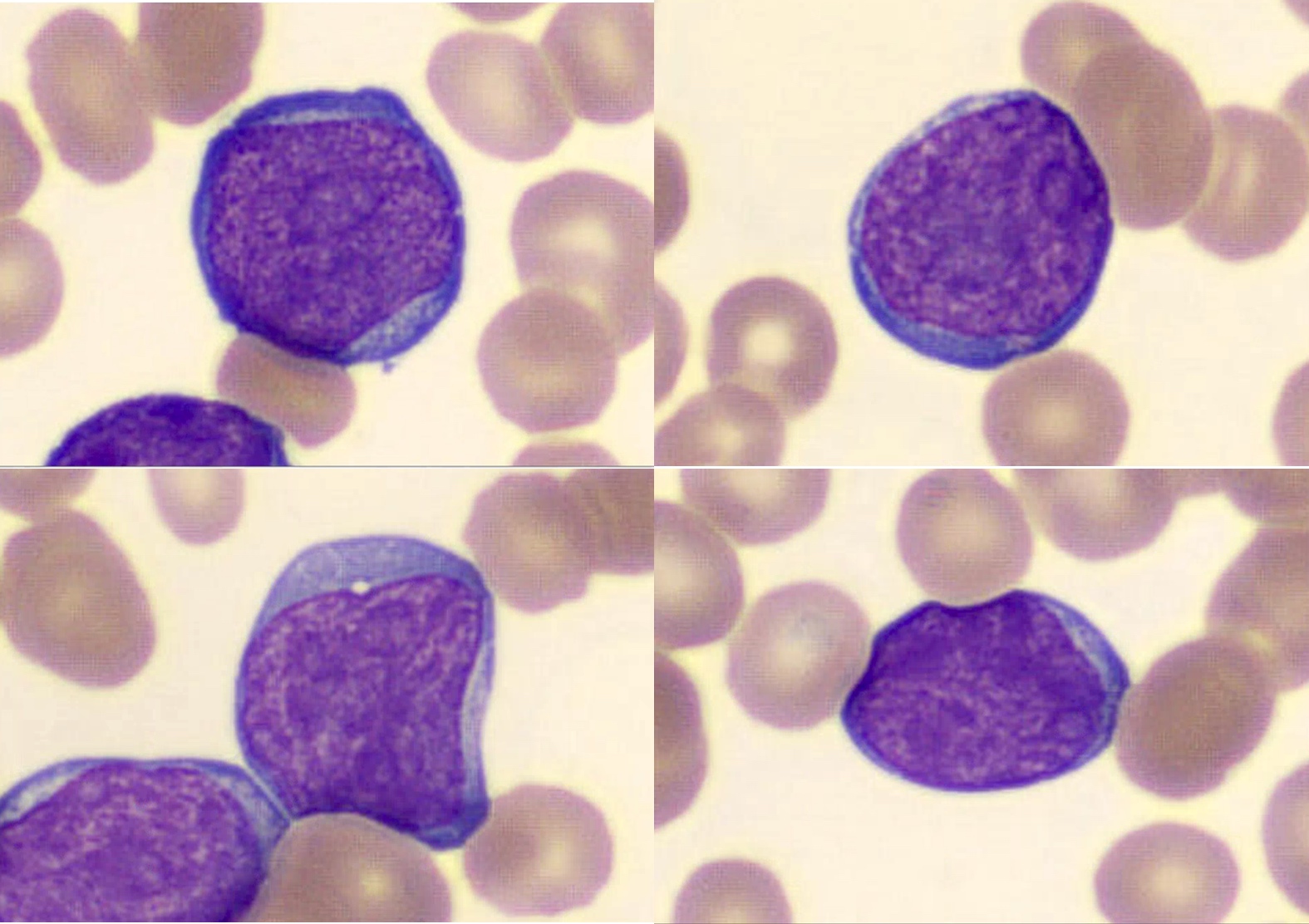
- Chronic lymphocytic leukemia (CLL) / small lymphocytic lymphoma
- Mature B cell neoplasm
- Monomorphic small lymphocytes with a minor proportion of prolymphocytes
- Round to slightly irregular nuclear contours
- Clumped chromatin
- Scant amount of pale blue cytoplasm
- Smudge cells are often seen
- CD5+, CD19+, CD20+ (dim), CD23+, CD79a+, LEF1+, CD200+, FMC7-, cyclin D1-, SOX11-, kappa or lambda surface immunoglobulin light chain (dim)
- IGHV genes are mutated in the majority of cases, while del13q is the most common cytogenetic finding
- See figure 1
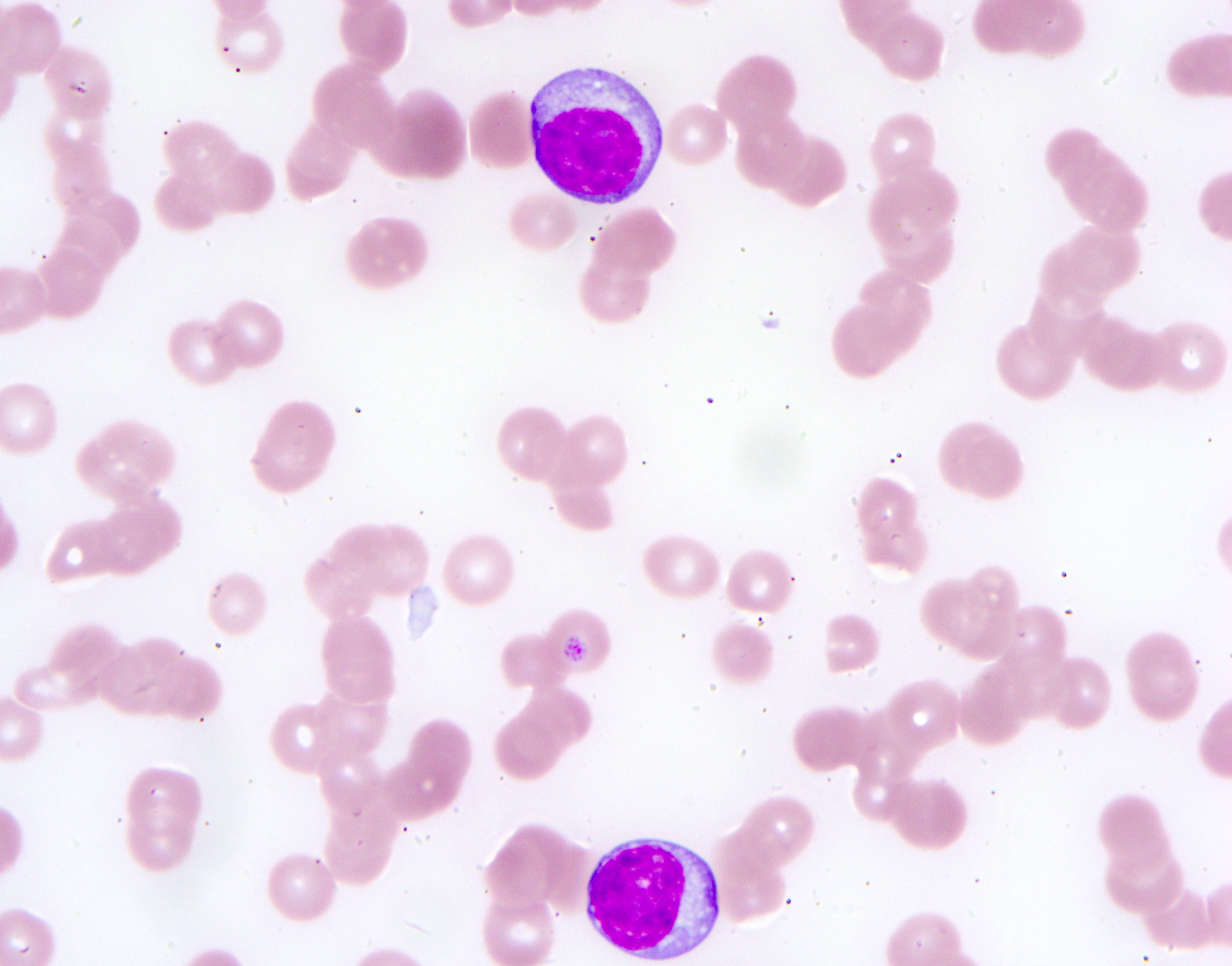
- Mantle cell lymphoma
- Mature B cell neoplasm
- Monomorphic small - intermediate sized lymphocytes
- Irregular nuclear contours (indented, folded or cleaved)
- Moderately clumped chromatin
- Scant amount of pale blue cytoplasm
- Morphologically indistinguishable from CLL cells
- Prolymphocytic-like morphology is common during leukemic phase
- CD5+, CD19+, CD20+, cyclin D1+, SOX11+, CD200-, CD23-, FMC7+
- Associated with t(11;14)(q13;q32) / CCND1::IGH translocation (95%)
- See figure 2
- Follicular lymphoma
- Mature B cell neoplasm
- Irregular nuclear contour with frequent indentations, folding, angulations and cleaved nuclei
- Moderately clumped chromatin
- Occasional small nucleoli
- Scant amount of basophilic cytoplasm
- CD19+, CD20+, CD79a+, CD10+, FMC7+, CD5-, CD23-
- Genetically characterized by t(14;18)(q32;q21), a translocation resulting in fusion of the IGH and BCL2 genes
- See figure 3
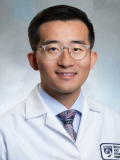
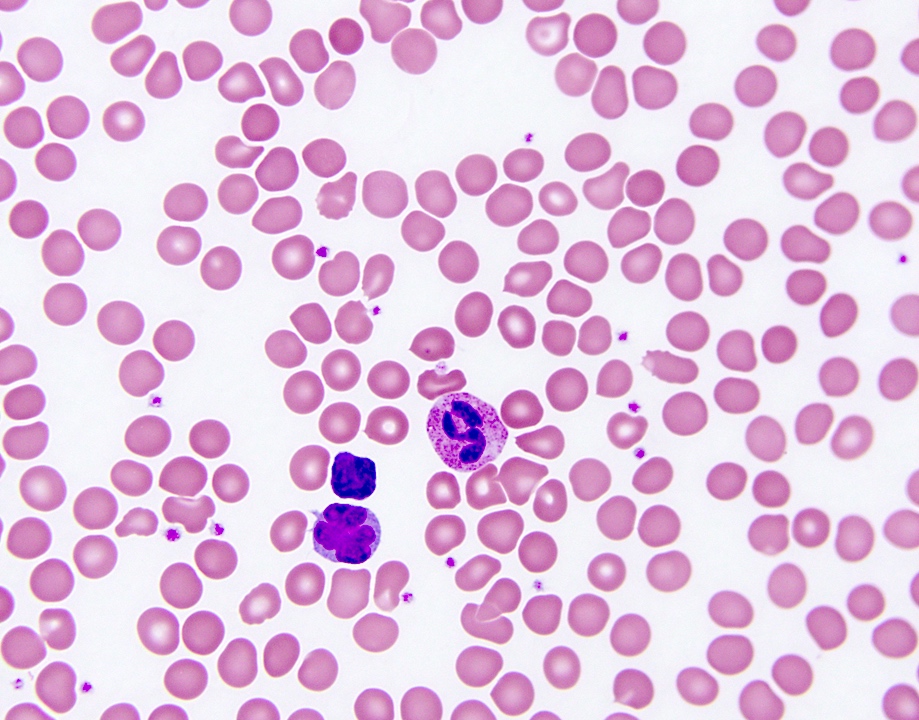
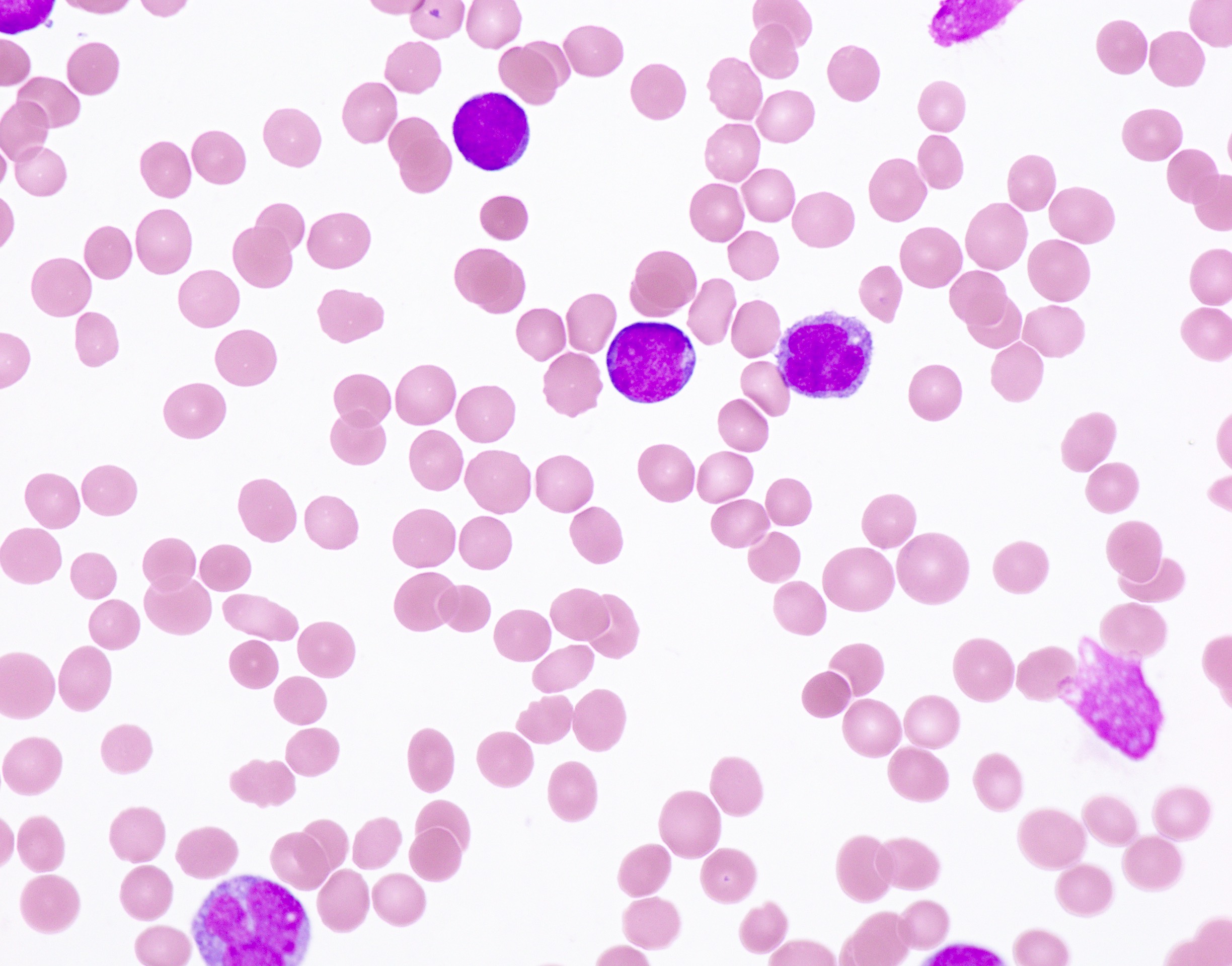
- Hairy cell leukemia
- Mature B cell neoplasm
- Monomorphic small to intermediate sized lymphocytes
- Smooth chromatin with inconspicuous nucleoli
- Moderate amount of pale blue cytoplasm classically seen with fine, hair-like projections
- CD19+, CD20+ (bright), TRAP+, CD11c+, CD25+, CD103+, CD200+, annexin A1+ (most specific), CD5-, CD10- (80 - 90%), CD23-
- Splenic B cell lymphoma / leukemia with prominent nucleoli (WHO 5th edition) and hairy cell leukemia variant (ICC 2022), a chronic lymphoproliferative disorder whose morphologic characters resemble hairy cell leukemia; neoplastic cells have prominent nucleoli and are negative for HCL markers (CD25, annexin A1 and TRAP)
- BRAF V600E mutation is found in most (> 90%) classic hairy cell leukemia cases
- Associated with pancytopenia and splenomegaly
- See figure 4
- Reference: Leuk Lymphoma 2015;56:2000, Leukemia 2022;36:1720, Blood 2022;140:1229
Intermediate sized cells
- T cell prolymphocytic leukemia
- Mature T cell neoplasm
- Small to intermediate sized lymphocytes
- Round to irregular nuclei
- Distinct nucleoli
- Basophilic cytoplasm with cytoplasmic blebs
- CD2+, CD3+, CD5+, CD7+, TdT-, CD4+/-, CD8+/-, TCL1+
- Most cases are found with inv(14)(q11q32) and TCL1 gene rearrangement detectable by FISH, while deletion or mutations in ATM have also been observed
- Aggressive disease
- See figure 5
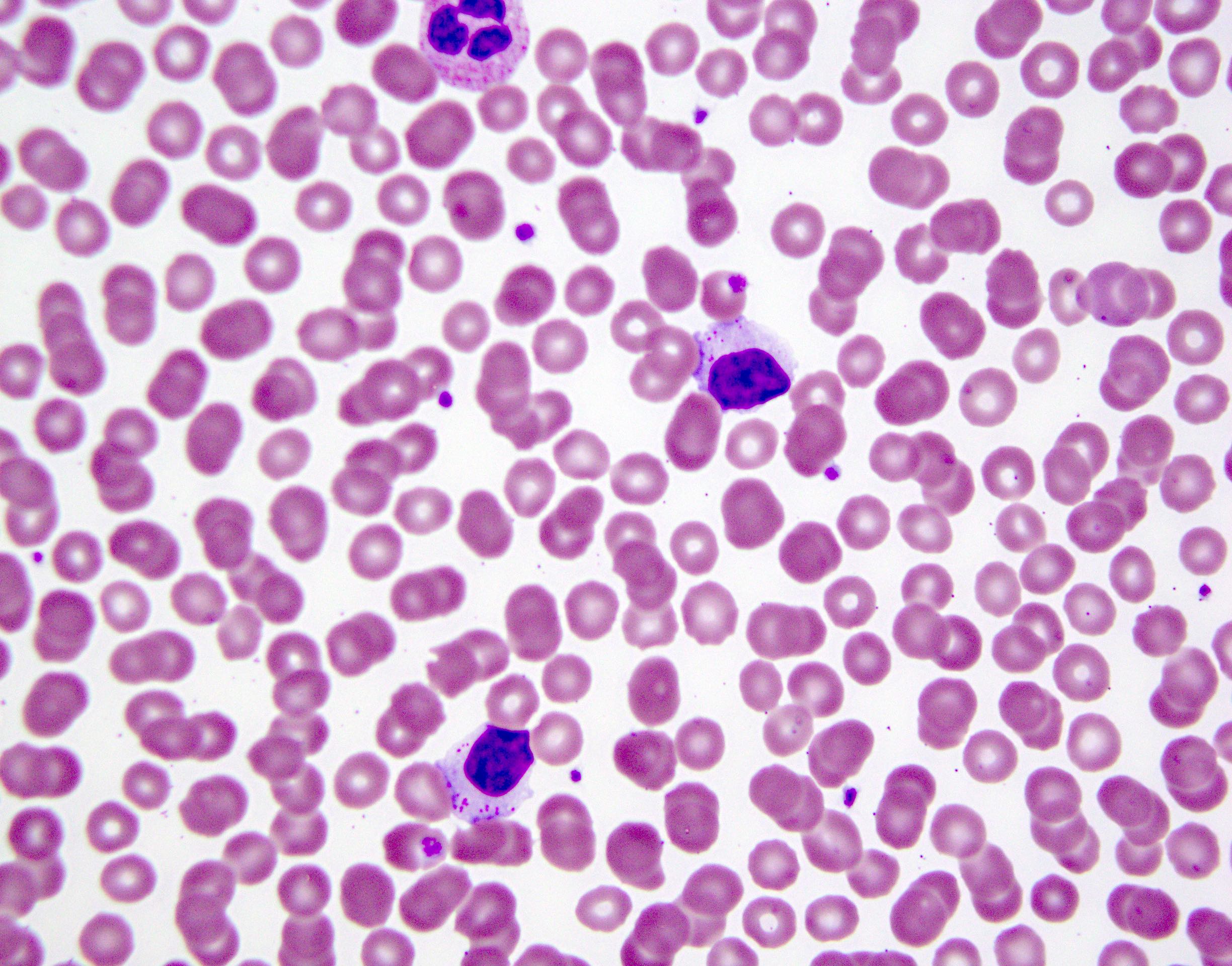
- Sézary syndrome
- Mature T cell neoplasm
- Medium sized to larger lymphocytes
- Irregular nuclear contour, often described as cerebriform pattern
- Condensed chromatin
- Inconspicuous nucleoli
- Abundant basophilic cytoplasm
- CD2+, CD3+, CD5+, TCRαβ+, CLA+, usually CD4+, CD8-, CD7- and CD26-
- T cell receptor gene rearrangements are present; recurrent balanced chromosomal translocations have not been identified
- Aggressive form of mycosis fungoides
- See figure 6
- Adult T cell leukemia / lymphoma
- Mature T cell neoplasm, caused by human retrovirus HTLV1
- Several morphological variants have been identified: small, medium, large cell and anaplastic variants
- Convoluted and polylobated nuclei, often described as flower cells
- Condensed chromatin
- Small or inconspicuous nucleoli
- Moderate amount of basophilic cytoplasm
- CD2+, CD3+, CD5+, CD4+/- and CD8-/+, CD25+, CD7-
- Clonal T cell receptor gene rearrangement
- Associated with hypercalcemia
- See figure 7
- Reference: Am J Hematol 2019;94:1027
Plasma cells
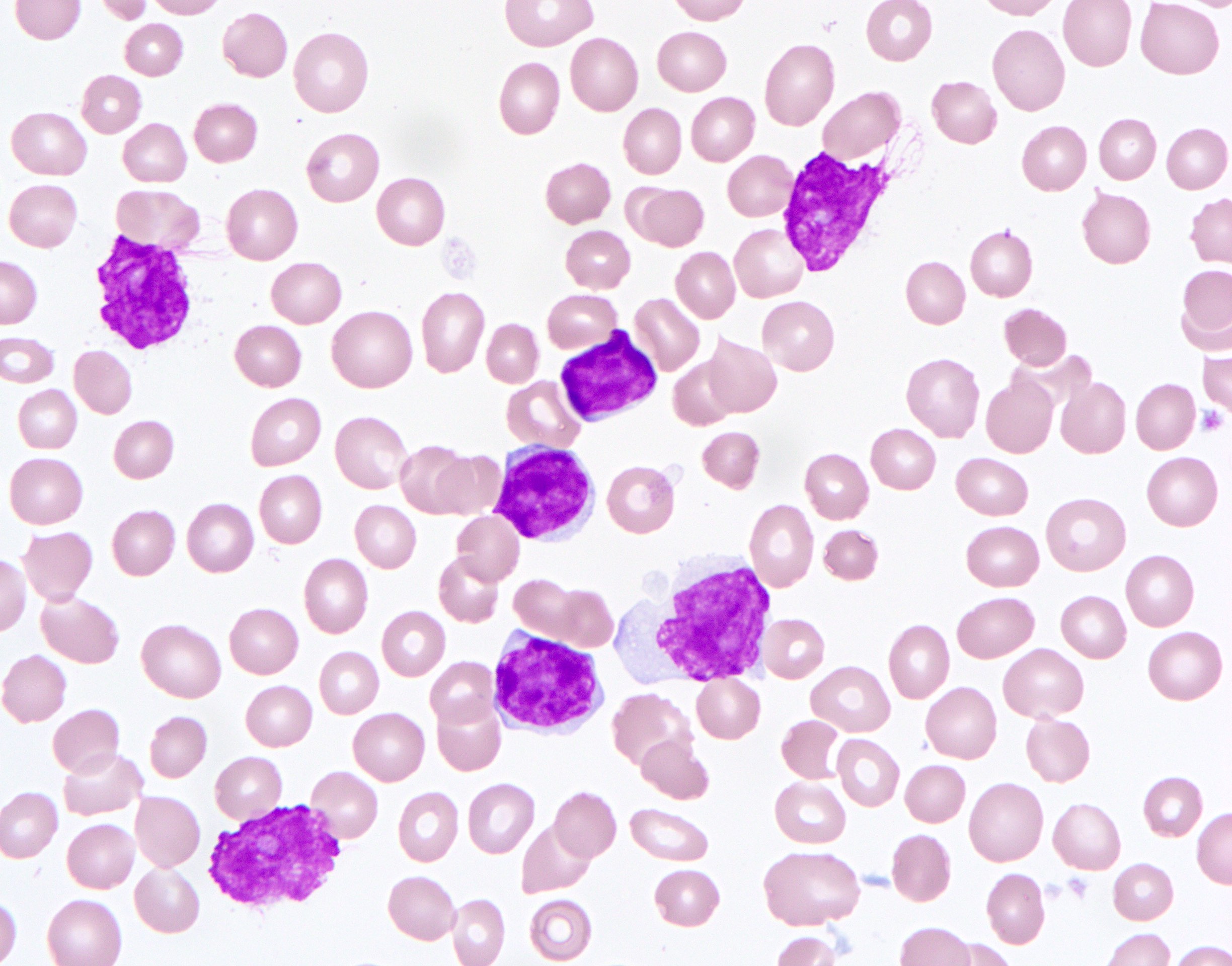
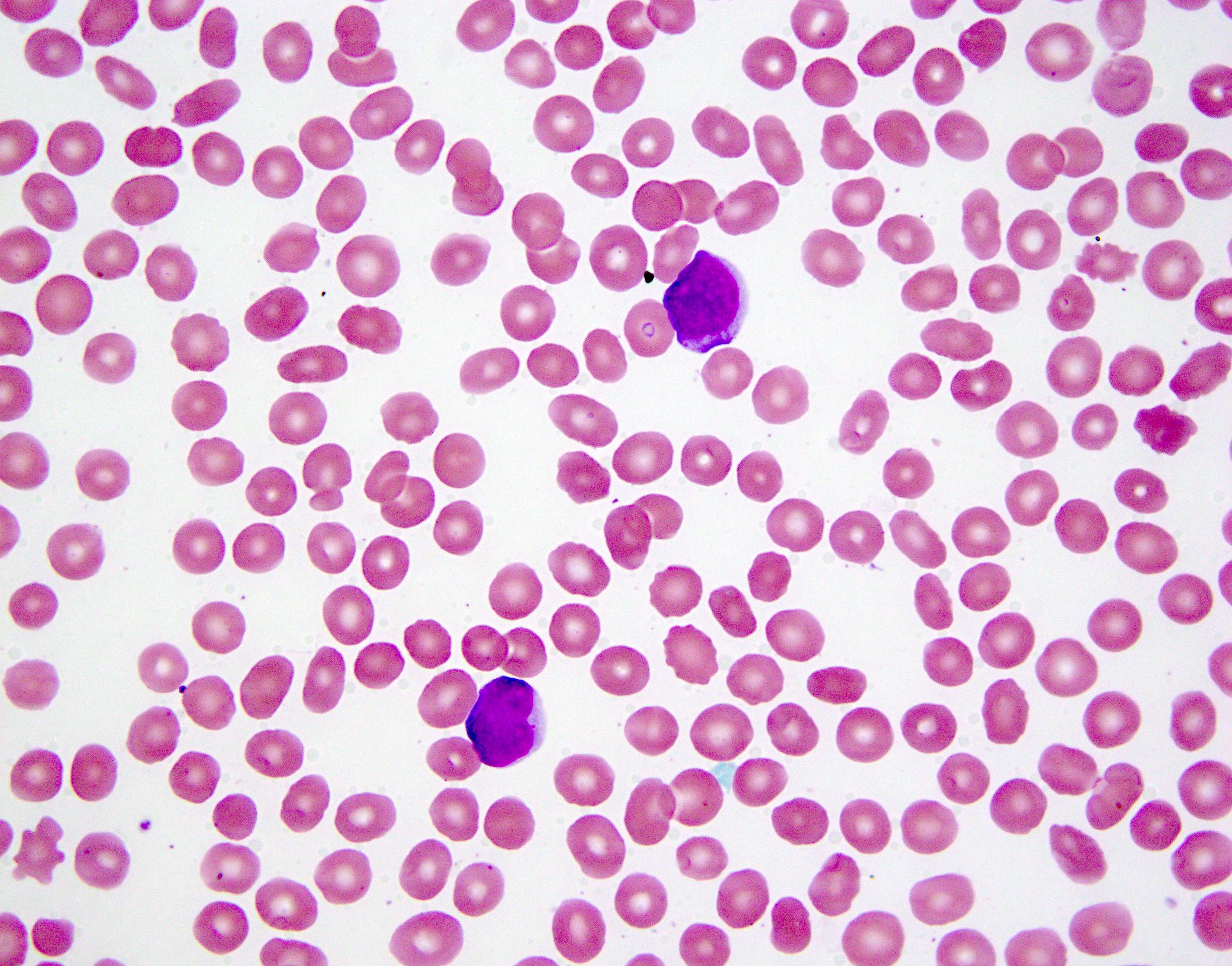
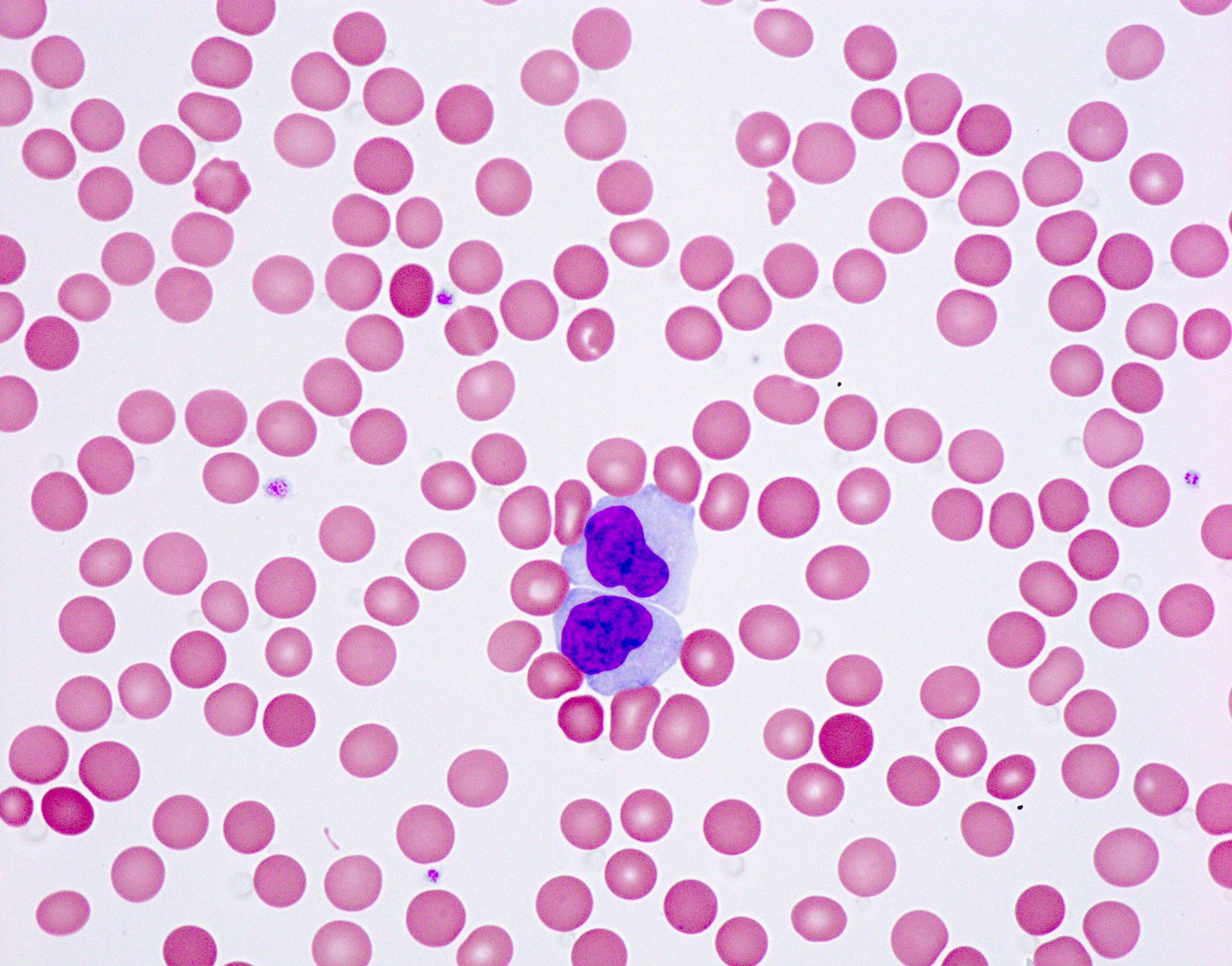
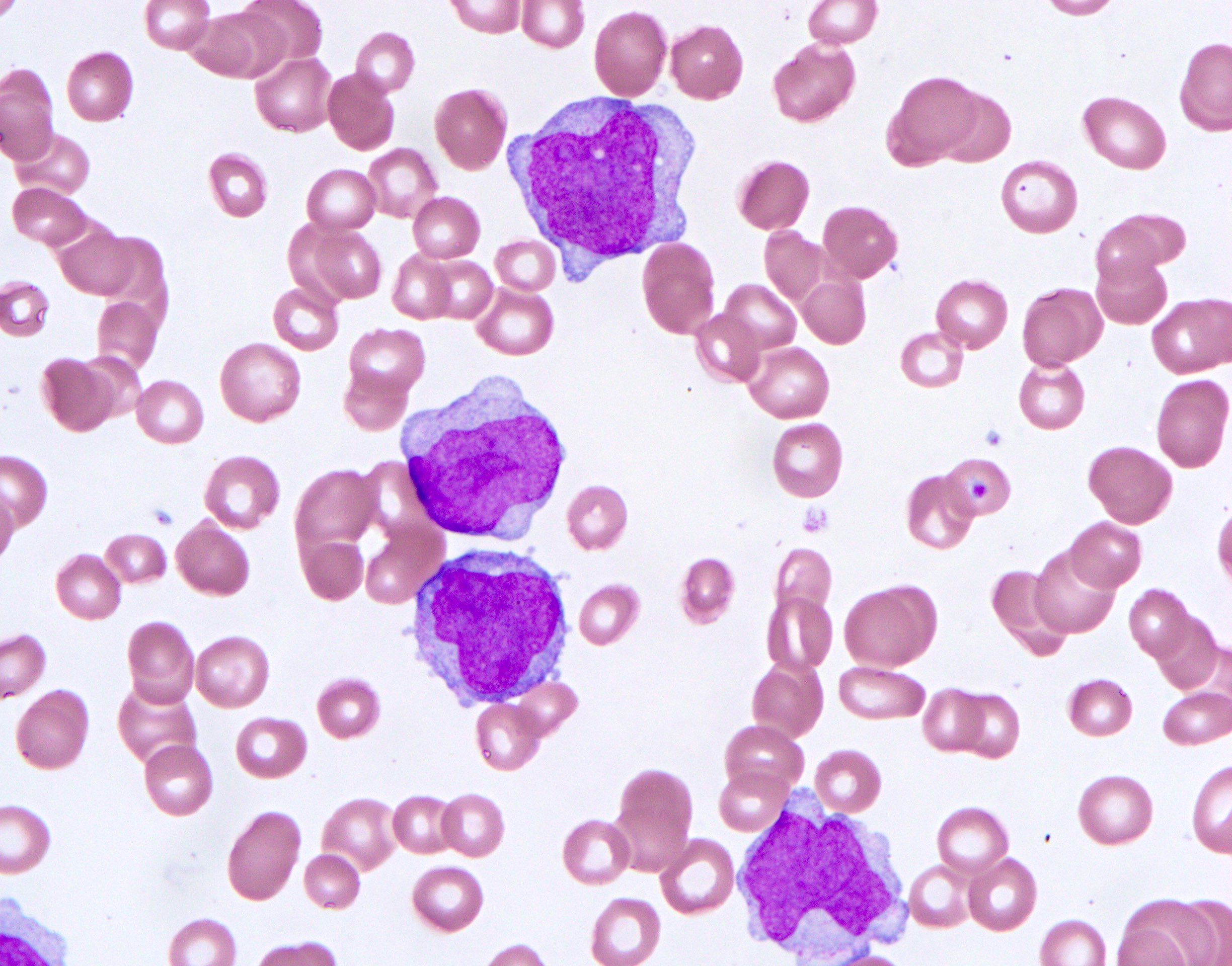
- Multiple myeloma - plasma cell leukemia (primary or secondary)
- Plasma cell neoplasm
- Medium sized neoplastic cells
- Eccentric round nucleus
- Coarse chromatin, often seen in a clockface pattern
- Abundant amount of pale to basophilic cytoplasm with perinuclear clearing
- According to the 2021 International Myeloma Working Group recommendation, primary plasma cell leukemia is defined as "5% or more circulating plasma cells in peripheral blood smears in patients otherwise diagnosed with symptomatic multiple myeloma" (Blood Cancer J 2021;11:192)
- CD38+, CD138+, CD56+ (80%), CD45-, CD19- (95%)
- Immunoglobulin heavy and light chain gene rearrangement
- Associated with Rouleaux formation of RBCs and monoclonal gammopathy
- See figure 8
- Reference: Blood Rev 2011;25:107
Large lymphocytes
- Diffuse large B cell lymphoma (example: CLL status post-Richter transformation)
- T cell large granular lymphocytic leukemia
- Mature cytotoxic T cell neoplasm
- Large sized lymphocytes
- Irregular nuclear contour
- Coarse chromatin
- Indistinct nucleoli
- Abundant clear cytoplasm with azurophilic granules; cytologically indistinguishable from natural killer cells (CD3-)
- CD2+, CD3+, CD4-, CD8+, CD57+, CD56 variable, CD16+ (variable), loss of CD5 or CD7 is common
- Clonal T cell receptor gene rearrangement
- Indolent disease; associated with cytopenia, particularly neutropenia, and rheumatoid arthritis
- See figure 10
- Reference: Autops Case Rep 2016;6:41
Blasts
- Myeloid: acute myeloid leukemia (example: AML with inv(16))
- Immature myeloid neoplasm
- Medium to large sized myeloblasts
- Round to irregular or folded nuclei
- Dispersed chromatin
- Distinct nucleoli
- Moderately abundant cytoplasm
- Auer rods present in some cases, abundant in acute promyelocytic leukemia
- Typically, CD34+ and CD117+, may exhibit granulocytic lineage (positive for CD13, CD33, CD15, CD65 and MPO) or monocytic lineage (positive for CD14, CD4, CD11c, CD64, CD36 and lysozyme)
- See figure 11 showing an AML with inv(16)(p13.1;q22)
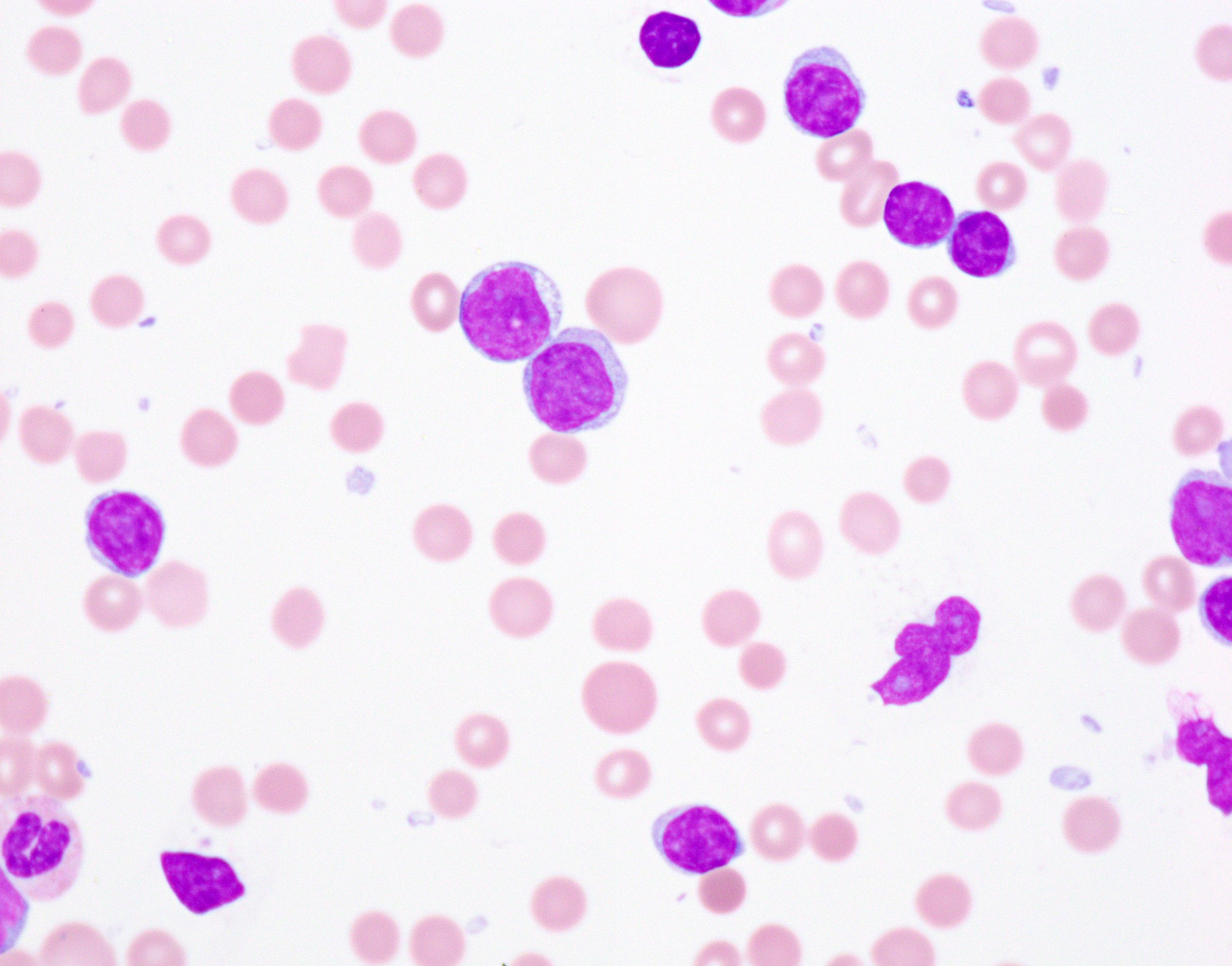
- Lymphoid: B lymphoblastic leukemia / lymphoma (example: B ALL with KMT2A rearrangement)
- Immature lymphoid neoplasm
- Intermediate sized lymphoblasts
- Round to irregular nuclei
- Dispersed chromatin
- Distinct nucleoli
- Scant amount of basophilic cytoplasm
- Typically, CD19+, CD22+, CD79a+, CD10+, CD45 (moderate intensity) and variable expression of TdT and CD34
- Recurrent genetic abnormalities include t(9;22)(q34.1;q11.2) BCR::ABL1, t(v;11q23.3) KMT2A rearranged, t(12;21)(p13.2;q22.1) ETV::RUNX1, t(5;14)(q31.1;q32.1) IGH::IL3 or t(1;19)(q23;p13.3) TCF3::PBX1
- See figure 12
- Blast equivalents (promonocytes) (example: acute myelomonocytic leukemia)
- Immature monocytic precursors that are counted towards the total blast count in monocytic and myelomonocytic neoplasms
- Irregular and convoluted nuclear contours with fine folds
- Fine chromatin
- Distinct nucleoli
- Moderate amount of gray to pale blue cytoplasm with occasional small vacuoles
- Immature monocytic precursor cells are usually CD14+/-, CD64+, CD15+, CD11b+, CD11c+, CD4+, CD36+, CD68+, CD163+ and lysozyme+
- Nonspecific cytogenetic abnormalities
- See figure 13
- Reference: StatPearls: Leukemia [Accessed 11 January 2023]
Diagrams / tables
Table 1: B cell lymphoproliferative disorders and markers
| CD45RA | CD19 | CD20 | CD79a | CD5 | CD10 | CD23 | Cyclin D1 | SOX11 | LEF1 | CD200 | CD103 | CD11c | CD25 | |
| Follicular lymphoma | + | + | + | + | - | + | - | - | -/+ | Unknown | - | - | -/+ | -/+ |
| Chronic lymphocytic leukemia / small lymphocytic lymphoma | + | + | + | + | + | - | + | - | - | +/- | + | - | -/+ | -/+ |
| Diffuse large B cell lymphoma | + | + | + | + | - | +/- | - | - | -/+ | -/+ | +/- | -/+ | -/+ | -/+ |
| Mantle cell lymphoma | + | + | + | + | + | - | - | + | + | - | - | - | - | -/+ |
| Marginal zone lymphoma | + | + | + | + | - | - | - | - | -/+ | - | - | - | -/+ | - |
| Lymphoplasmacytic lymphoma | + | + | + | + | - | - | - | - | Unknown | - | +/- | - | +/- | +/- |
| Hairy cell leukemia | + | + | + | + | - | - | - | + | +/- | - | + | +/- | + | + |
| +: positive; -: negative; +/-: majority positive; -/+: majority negative | ||||||||||||||
Table 2: T cell lymphoproliferative disorders and markers
| CD4 / CD8 | Pan-T cell markers (CD2, CD3, CD5, CD7) | CD30 | T cell receptor | |
| T cell prolymphocytic leukemia | CD4+ / CD8- > CD4+ / CD8+ | All expressed | - | Alpha / beta |
| Sézary syndrome | CD4 | CD7 loss | +/- | Alpha / beta |
| Adult T cell leukemia / lymphoma | CD4 | CD7 loss | -/+ | Alpha / beta |
| T cell large granular lymphocytic / leukemia | CD8 | CD2, CD5 and CD7 variably loss | - | Alpha / beta |
| +: positive; -: negative; +/-: majority positive; -/+: majority negative | ||||
Peripheral smear images
Board review style question #1
Which of the following lymphoproliferative disorders is associated with human retrovirus HTLV1?
- Adult T cell leukemia / lymphoma
- Hairy cell leukemia
- Sézary syndrome
- T cell large granular lymphocytic leukemia
- T cell prolymphocytic leukemia
Board review style answer #1
Board review style question #2
Board review style answer #2