Table of Contents
Definition / general | Epidemiology | Pathophysiology / etiology | Diagrams / tables | Clinical features - Plasmodium falciparum | Diagnosis | Laboratory | Life cycle | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Peripheral smear images | Differential diagnosis | Additional referencesCite this page: Fadel H. Plasmodium falciparum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parasitologymalariapfalciparum.html. Accessed December 23rd, 2024.
Definition / general
- Malaria (from the Italian "mal' aria," meaning "bad air") is an acute and sometimes chronic bloodstream infection characterized by fever, anemia and splenomegaly, caused by apicomplexan parasites of the genus Plasmodium
- Four species of plasmodia causing human malaria are Plasmodium vivax, Plasmodium falciparum, Plasmodium malariae and Plasmodium ovale
- Plasmodium falciparum causes 85% of malaria cases
- Because its infection is potentially life threatening, its presence must be considered in the differential diagnosis of unexplained fever and history of travel to endemic geographic areas should always be sought
Epidemiology
- Falciparum infection occurs principally in tropical areas worldwide
- U.S. civilian cases of malaria increased from 151 in 1970 to 1,838 in 1980 (McPherson: Henry's Clinical Diagnosis and Management by Laboratory Methods, 22nd Edition, 2011 [Chapter 62]) and reached a 40 year high of 1,925 cases in 2011 (CDC: Malaria Facts [Accessed 9 January 2018])
- Worldwide, disease generally occurs between 45° N and 40° S and rates have been declining (WHO: Malaria [Accessed 9 January 2018])
Pathophysiology / etiology
- Spreads exclusively by female anopheline mosquitoes
- Fever paroxysm (see below) occurs over 6 - 10 hours; is initiated by synchronous rupture of erythrocytes with release of new infectious blood stage forms known as merozoites
- Transfusion induced malaria occurs when blood donors have subclinical malaria and may prove fatal for recipient
- Similarly, congenital malaria may occur in infants of mothers from endemic areas; infant acquires infection at birth due to rupture of placental blood vessels with maternal fetal transfusion
- Typically, no relapse with transfusion or congenital malaria because exoerythrocytic schizogony does not occur
Clinical features - Plasmodium falciparum
- Most patients become symptomatic within 1 month of exposure
- Defining clinical features of a malarial attack or paroxysm consist of initial shaking chills, fever (up to 40° C or higher) and generalized diaphoresis, followed by resolution of fever
- Brain involvement, known as cerebral malaria, causes disorientation, progressing to delirium, coma and often death
- Exchange transfusion may be lifesaving in severe cases (McPherson: Henry's Clinical Diagnosis and Management by Laboratory Methods, 22nd Edition, 2011 [Chapter 62])
Diagnosis
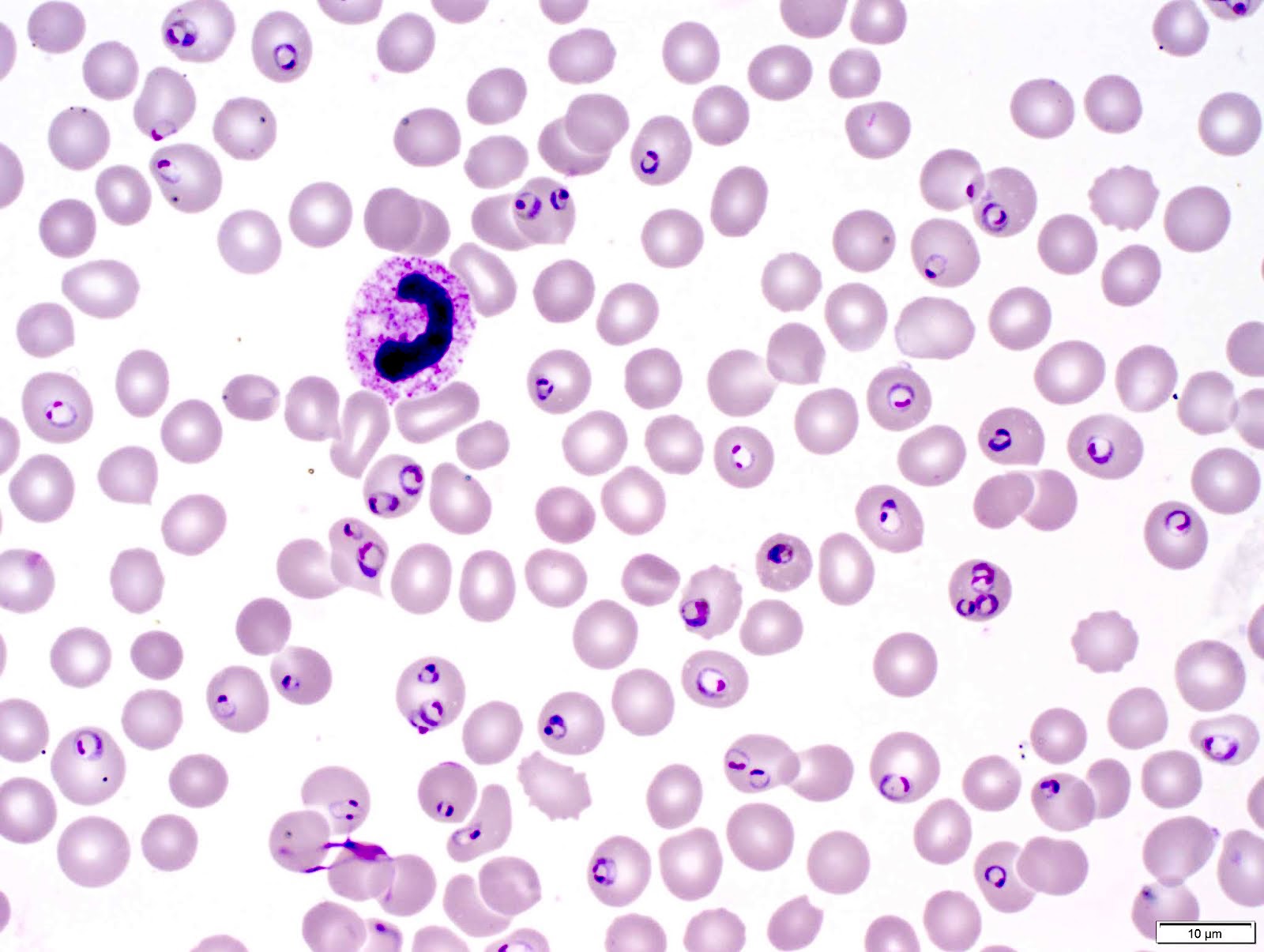
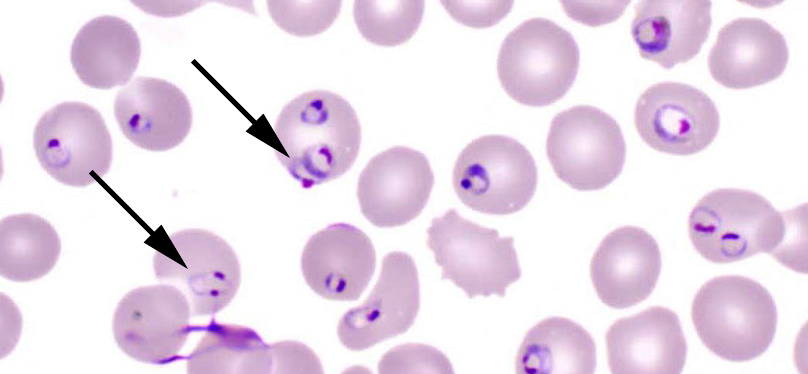
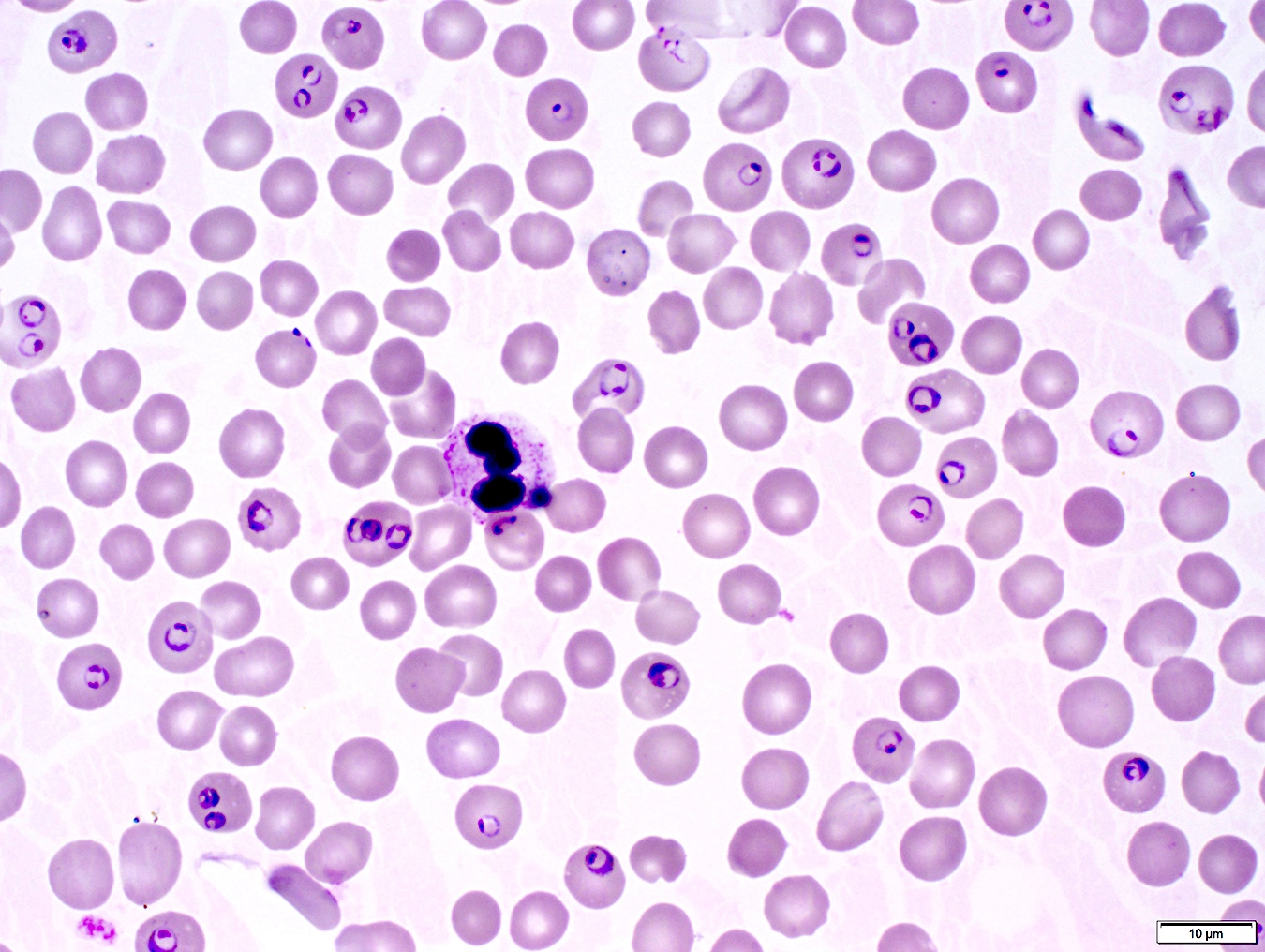
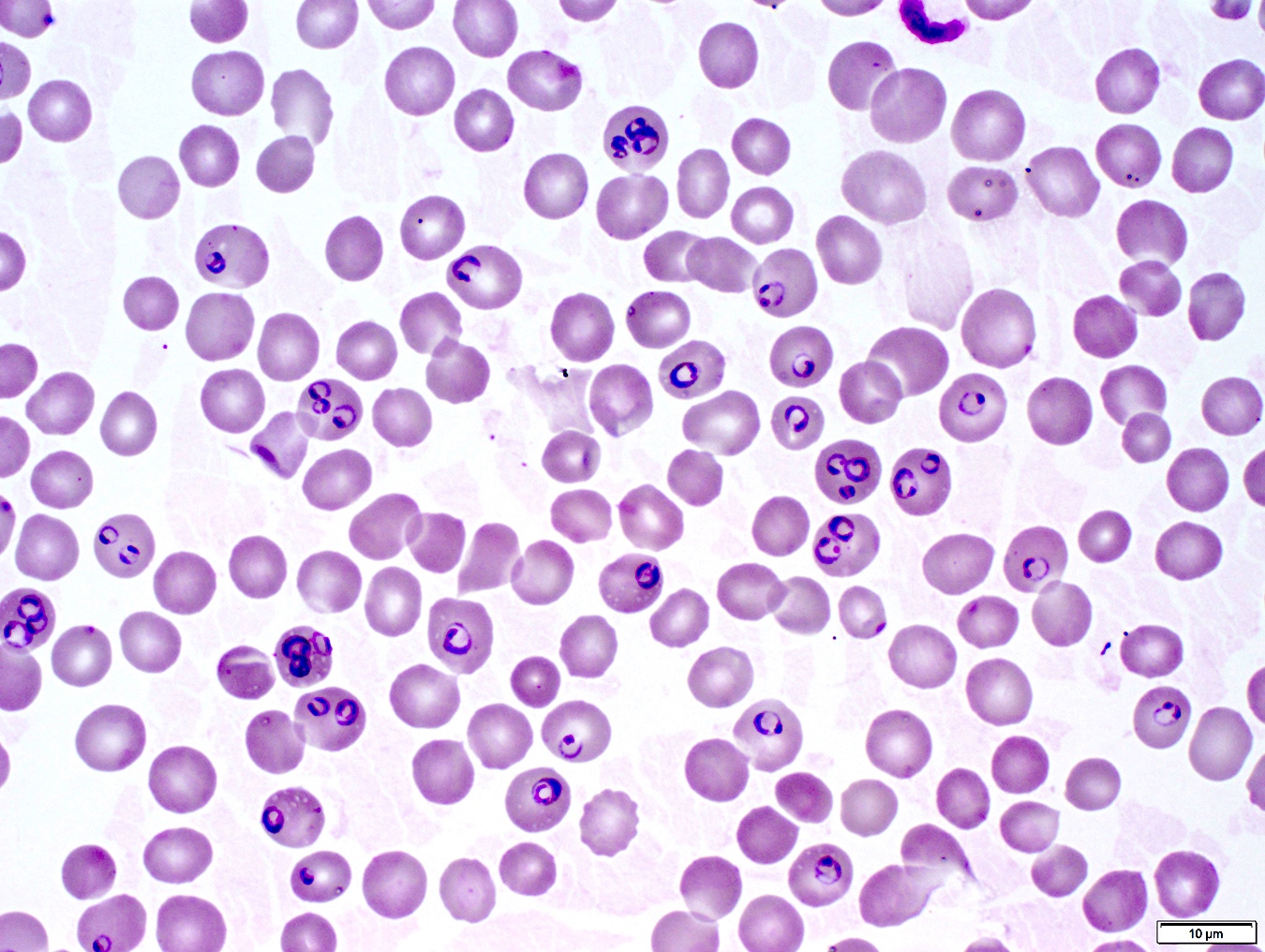
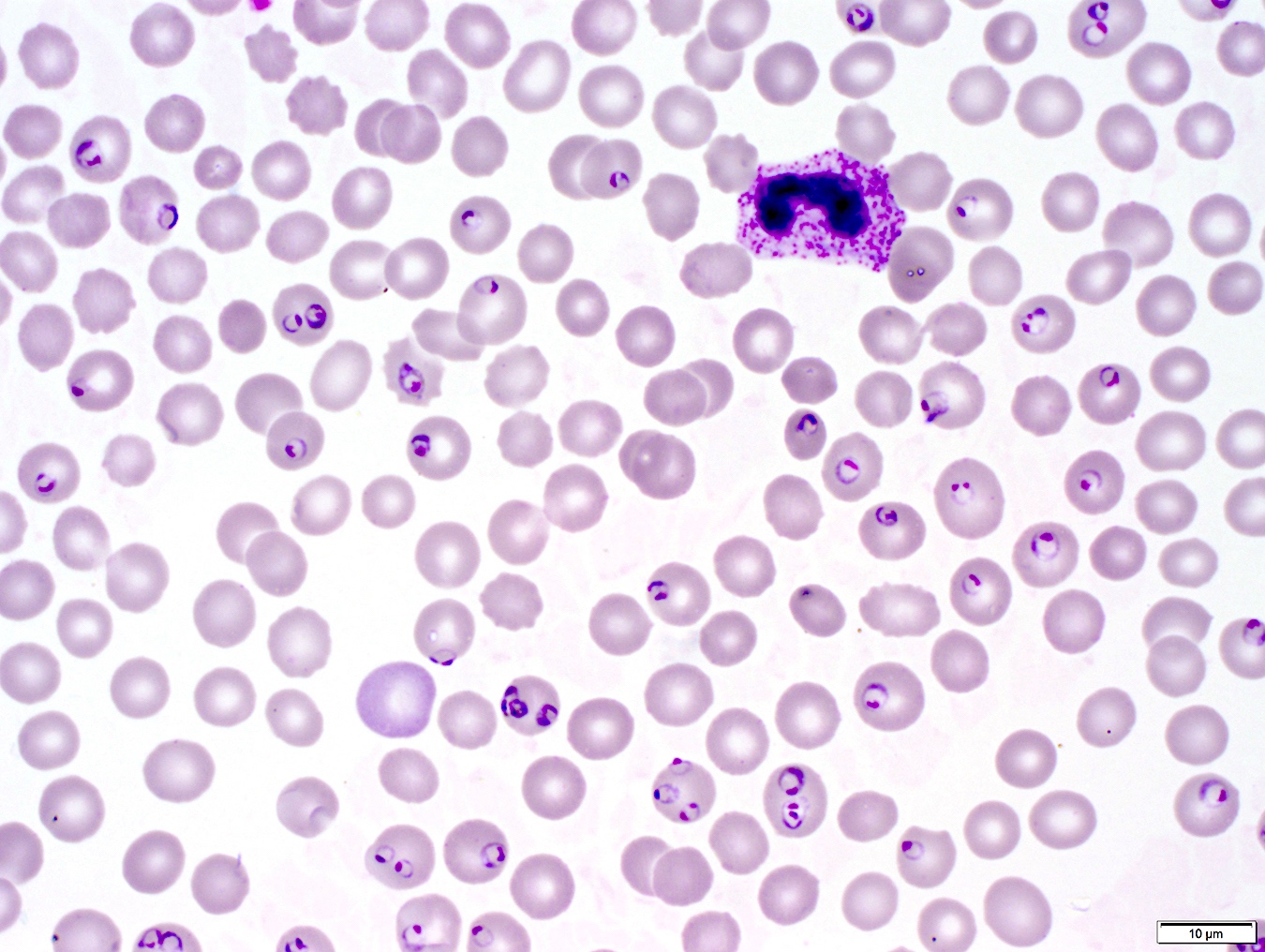
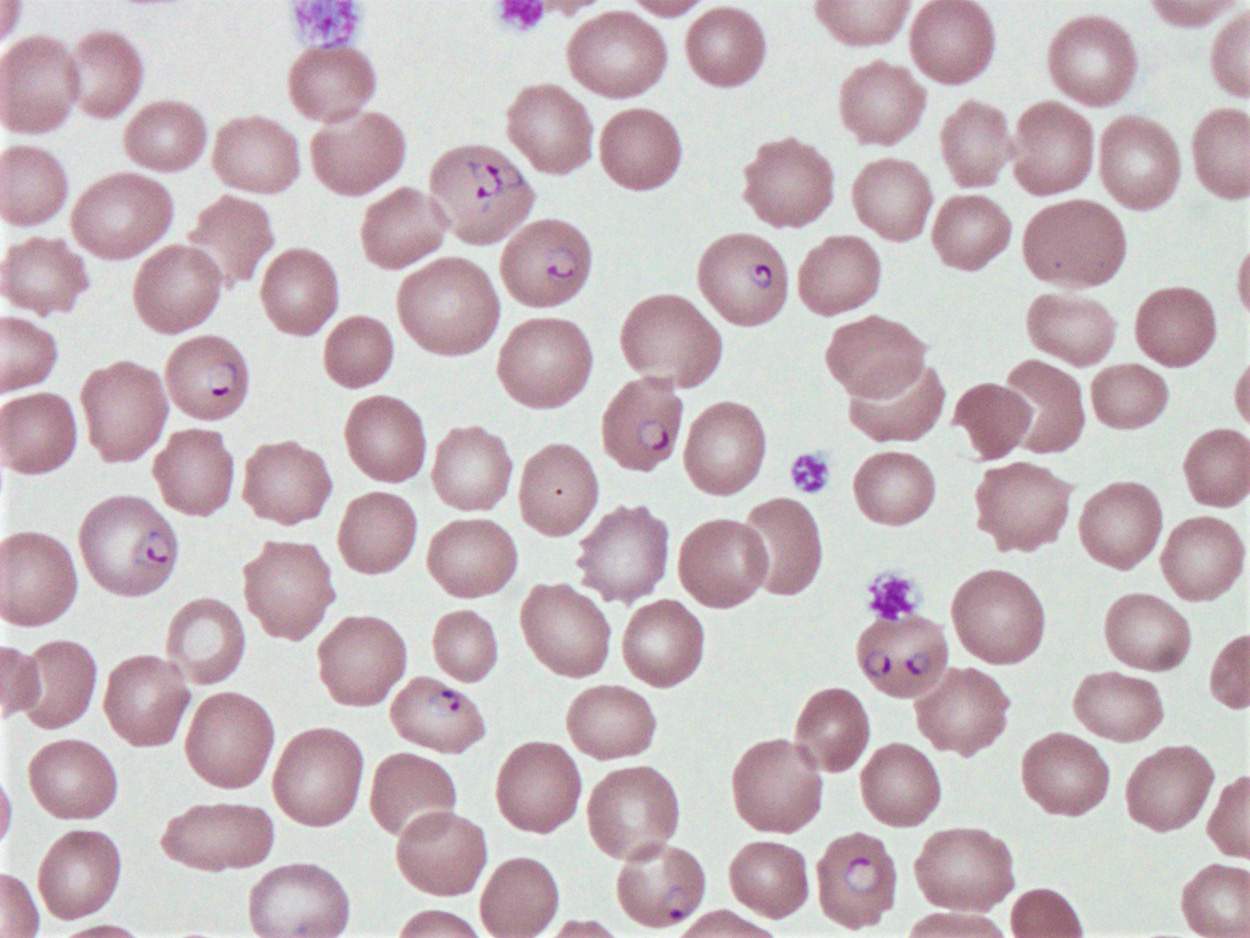
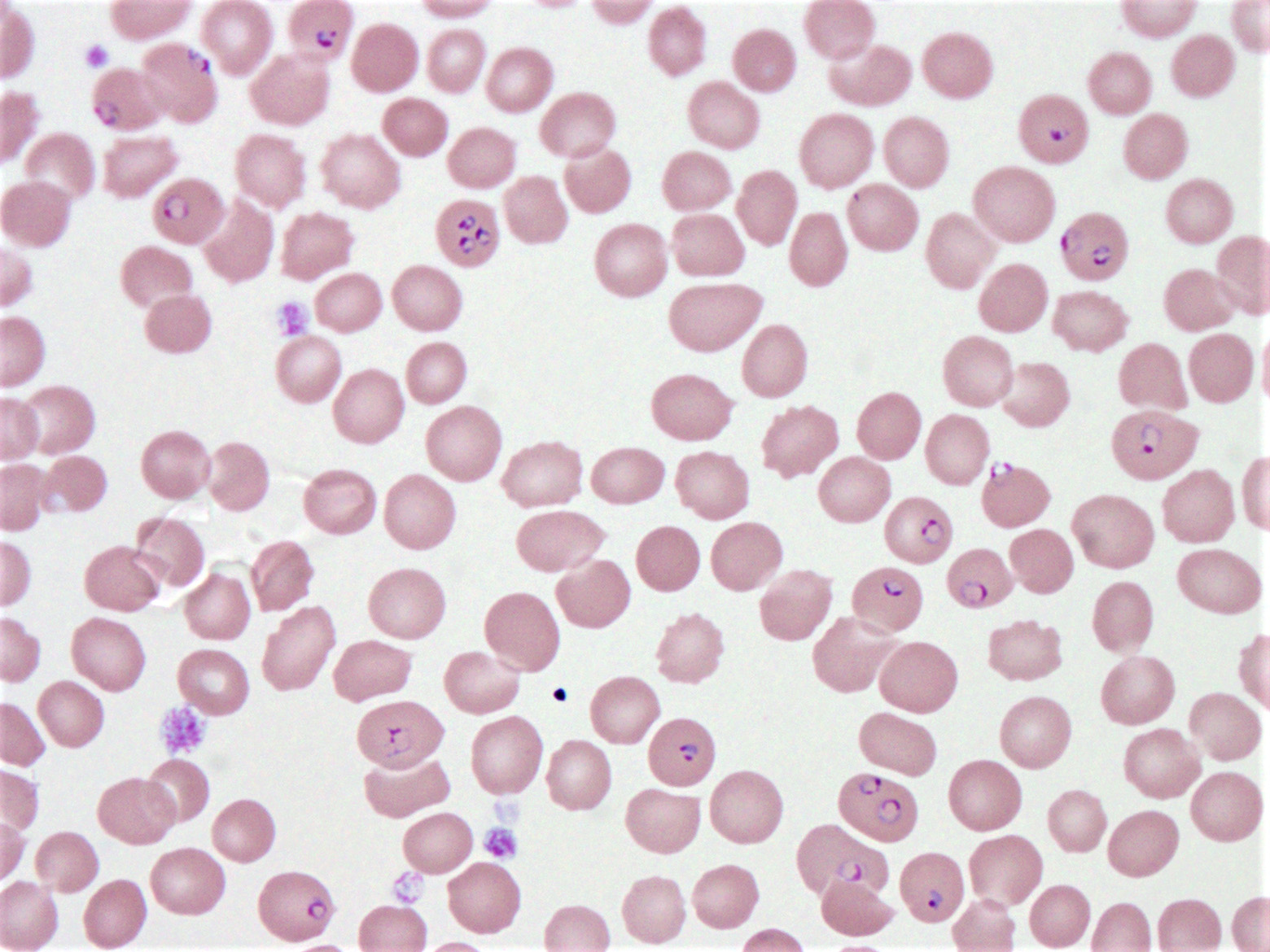
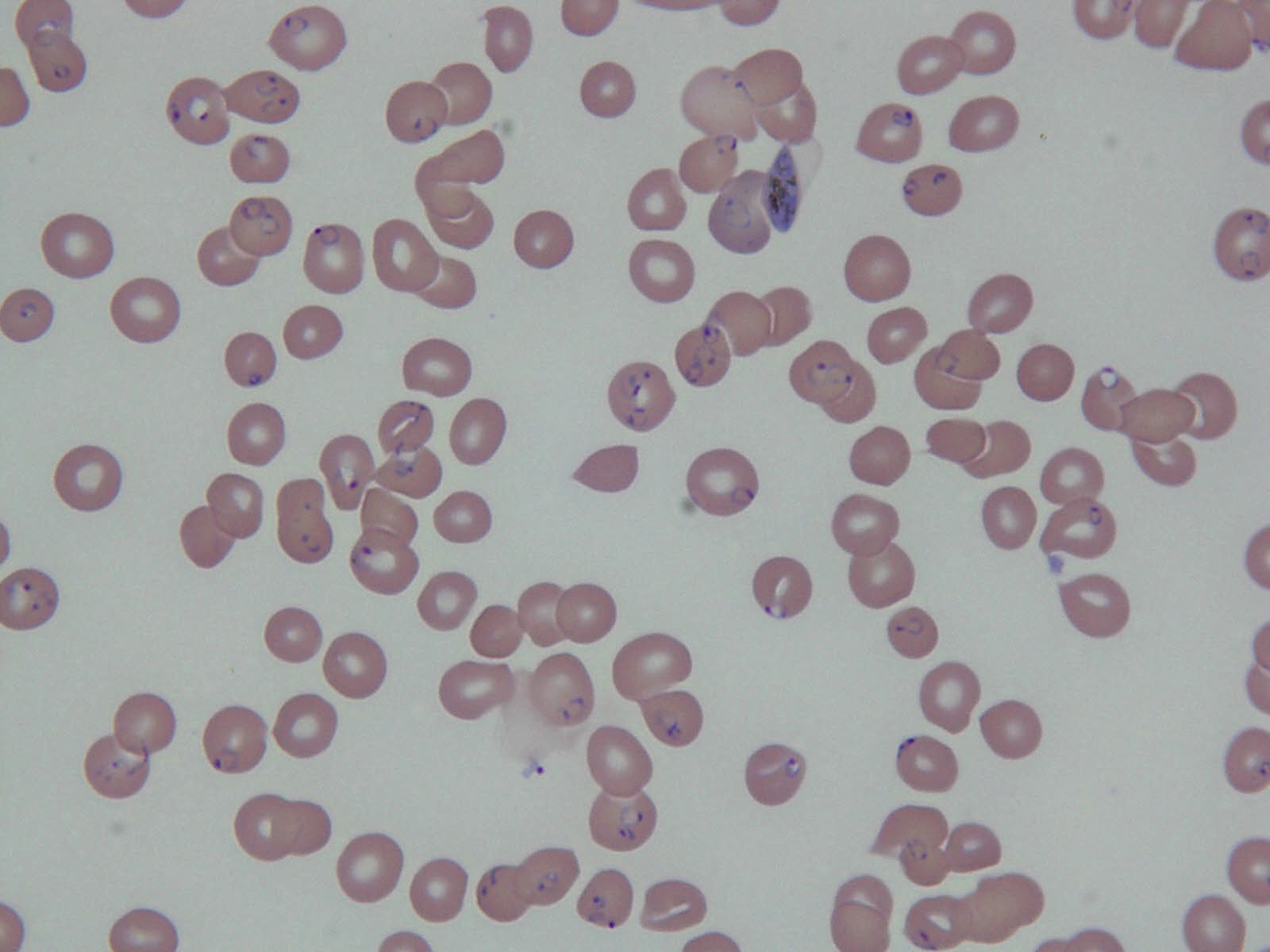
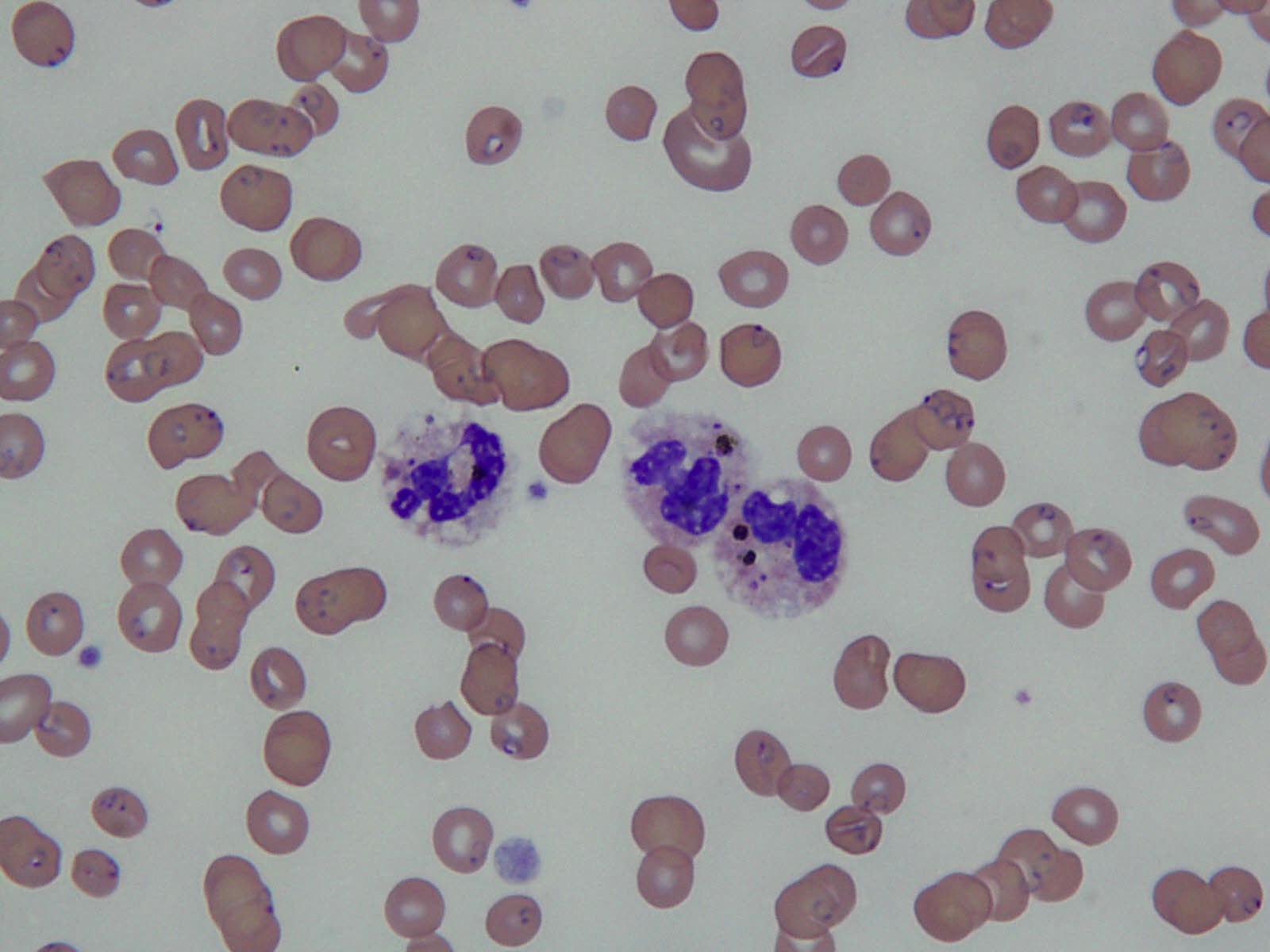
- Identification of malarial parasites on thin blood films requires a systematic approach
- Three major factors should be considered: appearance of infected erythrocytes, appearance of parasites and stages found
- Appearance of RBCs and size: normal size; multiple infected red blood cells are common
- Schüffner stippling: Maurer dots (comma shaped spots, dark blue by Giemsa staining, on RBC surface) are occasionally seen
- Parasite cytoplasm: young rings are small, delicate, often with double chromatin dots; gametocytes are crescent or elongate
- Appearance of parasite pigment: black; coarse and conspicuous in gametocytes
- Number of merozoites: 6 - 32; average is 20 - 24
- Stages found in circulating blood: rings or gametocytes; other stages develop in blood vessels of internal organs but are not seen in peripheral blood except in severe infection
Laboratory
- Laboratory evaluation relies on timely examination of thick and thin blood films to demonstrate the intraerythrocytic parasites
- More advanced laboratory methods include acridine orange staining and detection of parasite specific DNA (Exp Parasitol 2007;116:427)
Life cycle
- Morphologic stages seen in erythrocytes include trophozoites (growing forms), schizonts (dividing forms) and gametocytes (sexual forms)
- Malarial parasites undergo a sexual phase (sporogony) in Anopheles mosquitoes that produces infectious sporozoites and an asexual stage (schizogony) in humans that produces schizonts and merozoites
- In the bloodstream, some merozoites eventually differentiate into gametocytes (gametogony), which when ingested by female anopheline mosquitoes, mature into male microgametes and female macrogametes
- Fusion of a microgamete and a macrogamete results in the formation of the motile ookinete, which migrates to the outside of the mosquito stomach wall and forms an oocyst
- Within the oocyst, numerous spindle shaped sporozoites are formed
- Mature oocyst ruptures into the body cavity, releasing sporozoites, which then migrate through the tissues to the salivary glands, from which they are injected into the vertebrate host as the mosquito feeds
- Time required for development in the mosquito ranges from 8 - 21 days
- Sporozoites injected into the vertebrate host reach the hepatic parenchymal cells within minutes and initiate the proliferative phase known as exoerythrocytic schizogony
- Release of merozoites from ruptured hepatic schizonts initiates the bloodstream infection or erythrocytic schizogony and eventually the clinical symptoms of malaria
- P. vivax and P. ovale differ from P. falciparum and P. malariae in that true disease relapses of the former species may occur weeks to months following subsidence of previous attacks
- This occurs due to renewed exoerythrocytic and eventually, erythrocytic schizogony from latent hepatic sporozoites, which are known as hypnozoites
- Recurrence of disease due to P. falciparum or P. malariae, called recrudescences, arise from increased numbers of persisting blood stage forms to clinically detectable levels, not from persisting liver stage forms
- Liver cells are infected only by sporozoites from the mosquito; thus, transfusion acquired P. vivax or P. ovale infection does not relapse
- Merozoites released from infected hepatocytes subsequently infect erythrocytes
- Following amplification of parasites in the bloodstream for a period of time and the development of synchrony in their appearance, clinical attacks of malaria occur
- P. falciparum infects erythrocytes of all ages; P. vivax and P. ovale parasites primarily infect young erythrocytes; P. malariae infects older erythrocytes
Prognostic factors
- Individuals with sickle cell trait are less susceptible to P. falciparum malaria and persons who lack certain Duffy blood group determinants are protected against P. vivax infection
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency has been associated with protection from malaria but evidence is less striking than with these other genetic abnormalities
Case reports
- 45 year old man with disseminated intravascular coagulation in malaria (Niger Med J 2014;55:171)
- 45 year old man with high grade fever, rigors, chills and shortness of breath (Case of the Week #277)
- 50 year old woman with recent travel to Kenya presents with acute onset of fever and chills (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 558 [Accessed 13 September 2019])
- 51 year old man with severe Plasmodium falciparum infection mimicking acute myocardial infarction (Mala J 2014;13:341)
- A patient with recent travel to southern Africa presented with fever and myalgias (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 494 [Accessed 29 November 2018])
Treatment
- If parasitemia > 2%, contact the clinical team as if a critical value since patient is at high risk of death (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 494 [Accessed 29 November 2018])
- Therapy and prophylaxis of malaria have become highly complex due to widespread resistance by P. falciparum to chloroquine and other antimalarials and to a lesser extent, resistance by P. vivax to chloroquine
- These drugs are usually recommended by national malaria control programs but may not be effective due to local drug resistant strains (CDC: Guidelines for Treatment of Malaria in the United States [Accessed 9 January 2018]):
- Artemesinin containing combination treatments (for example, artemether-lumefantrine, artesunate-amodiaquine)
- Atovaquone-proguanil
- Chloroquine
- Doxycycline
- Mefloquine
- Quinine
- Sulfadoxine-pyrimethamine
- In addition to antimalarial treatment, red blood cell exchange may also be performed for patients with > 10% parasitemia (CDC paper arguing against red cell exchange for severe malaria: Clin Infect Dis 2013;57:923; ASA paper supporting red cell exchange: Clin Infect Dis 2014;58:302)
Microscopic (histologic) description
- Rings of P. falciparum can be found in blood smears
- Some may exhibit Maurer clefts
- Gametocyte may be present in blood smears
- Schizont of P. falciparum can be seen
- Rules for determining parasitemia (% RBC infected) (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 494 [Accessed 29 November 2018]):
- Count multiple infected RBCs as 1 only
- Don't count gametocytes, since they are a dead end stage in the human host
Peripheral smear images
Differential diagnosis
- Endocarditis, bacterial
- Gastroenteritis
- Pharyngitis
- Plague
- Pneumococcal bacteremia