Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ashfaq M, Husain AN. Giant cell arteritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/heartgiantcellarteritis.html. Accessed January 3rd, 2025.
Definition / general
- Giant cell arteritis (GCA) is a systemic inflammatory disorder characterized by granuloma formation in medium and large sized arteries, occurring most frequently in adults (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
- Very frequently it coexists with polymyalgia rheumatica
Essential features
- Commonly presents in older patients above age 50, mostly women, with new onset headache
- Most common in Scandinavian countries
- Timely diagnosis is essential to prevent irreversible vision loss
- Transmural inflammation of the vessel wall with giant cells is the main histological finding
- Important stains include elastic stain, CD68 and CD3
Terminology
- Horton arteritis
- Granulomatous arteritis
- Temporal arteritis
- Arteritis of the aged
- Cranial arteritis (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
ICD coding
Epidemiology
- Average age of diagnosis is 79 years
- F:M = 2.5:1
- Highest incidence in Scandinavia (6 times higher compared to Asia) and lowest in Asia
- Haplotype variations in certain MHC class II alleles with HLA-DRB1*04 being most common (Arthritis Res Ther 2021;23:82)
- Infectious diseases may lead to immune mediated hypersensitivity and play a role in the pathogenesis of the condition
Sites
- Medium vessel arteritis involving temporal artery, occipital artery and intraorbital blood vessels (ophthalmic and posterior ciliary)
- Large vessel arteritis involving the thoracic aorta, carotid arteries, subclavian and axillary artery (Circ Res 2023;132:238)
Pathophysiology
- Predominantly Th1 mediated immune response with significant expression of IFN gamma
- Initial endothelial injury results in activation of dendritic cells
- Activated dendritic cells release chemokines attracting CD4+ T cells and macrophages into the arterial wall
- Dendritic cells also release chemokines like IL16 and IL18, which cause T cell activation and interferon gamma release
- IFN gamma causes the characteristic chronic inflammation with formation of granulomas
- IFN gamma is also responsible for activation of mononuclear macrophages that tend to release enzymes called matrix metalloproteinase, resulting in breakdown of matrix proteins in the vessel wall and disruption of internal elastic lamina
- Role of IL6 in causing CD4+ helper T cell differentiation leading to development of Th17 cells while suppressing the T regulatory cells (StatPearls: Giant Cell Arteritis (Temporal Arteritis) [Accessed 24 May 2024])
Etiology
- Systemic inflammation largely driven by IL6 is a core feature of GCA
- Haplotype variations in MHC class II alleles (most commonly HLA-DRB1*04) seem to be a common finding among patients with this condition (Arthritis Res Ther 2021;23:82)
Clinical features
- Cranial involvement can present as
- New onset headache in the temporal region (most common presenting complaint)
- Scalp tenderness and visual disturbances
- Jaw and tongue claudication
- Transient visual disturbances
- Extracranial involvement can present as
- Limb claudication
- Vascular bruits
- Systemic symptoms like fatigue, weight loss, fever and flu-like symptoms
- Complications that can result without timely treatment include
- Ischemic optic neuropathy
- Central retinal artery occlusion
- Cerebrovascular accidents (transient ischemic attack or stroke)
- Aortic aneurysm and dissection (Rheumatology (Oxford) 2020;59:iii5)
Diagnosis
- Physical examination findings
- Temporal arteries may be thickened and tender on palpation
- Absent or diminished pulses
- Laboratory findings
- Raised erythrocyte sedimentation rate (ESR) or C reactive protein (CRP)
- Radiology
- Color Doppler ultrasound of temporal arteries
- Magnetic resonance imaging (MRI) or computed tomography (CT) angiography
- Pathology
- Temporal artery biopsy is gold standard (Rheumatology (Oxford) 2020;59:iii5)
Laboratory
- Raised ESR or CRP
Radiology description
- Doppler ultrasound findings
- Hypoechoic and diffuse thickening of arterial wall
- Halo sign: indicator of the thickness of the vessel wall caused by inflammation and considered a pathognomonic sign of GCA on ultrasound
- Reference: Ultrasound Med Biol 2021;47:201
Prognostic factors
- Factors associated with decreased risk of permanent blindness
- Fever
- Rheumatic symptoms
- Factors associated with increased risk of permanent blindness
- Age
- History of transient ischemic visual symptoms
- Jaw claudication (J Rheumatol 2016;43:1393)
Case reports
- 69 year old man with giant cell arteritis and the simultaneous onset of multiple intracranial vascular occlusions (Surg Neurol Int 2022;13:21)
- 73 year old man with an unusual presentation for giant cell arteritis (Pract Neurol 2021;21:228)
- 78 year old woman with giant cell arteritis who developed scalp necrosis (J Am Acad Dermatol 2009;61:701)
Treatment
- Corticosteroids are the mainstay of treatment, especially to prevent blindness
- Dosage: 1 mg/kg per day or 40 - 60 mg per day in divided doses for initial 4 weeks followed by gradual tapering as condition improves
- Steroid sparing agents like methotrexate, azathioprine and sulfasalazine
- Addition of a disease modifying antirheumatic drug (DMARD) may be needed in some cases (Dtsch Arztebl Int 2013;110:376)
Gross description
- Thickened, nodular and rubbery wall in the segment of the muscular artery involved
- Grossing should be done thoroughly to account for the possibility of skip lesions
- Submit whole specimen in 2 - 3 mm cross sections
- Reference: Rheumatology (Oxford) 2020;59:iii5
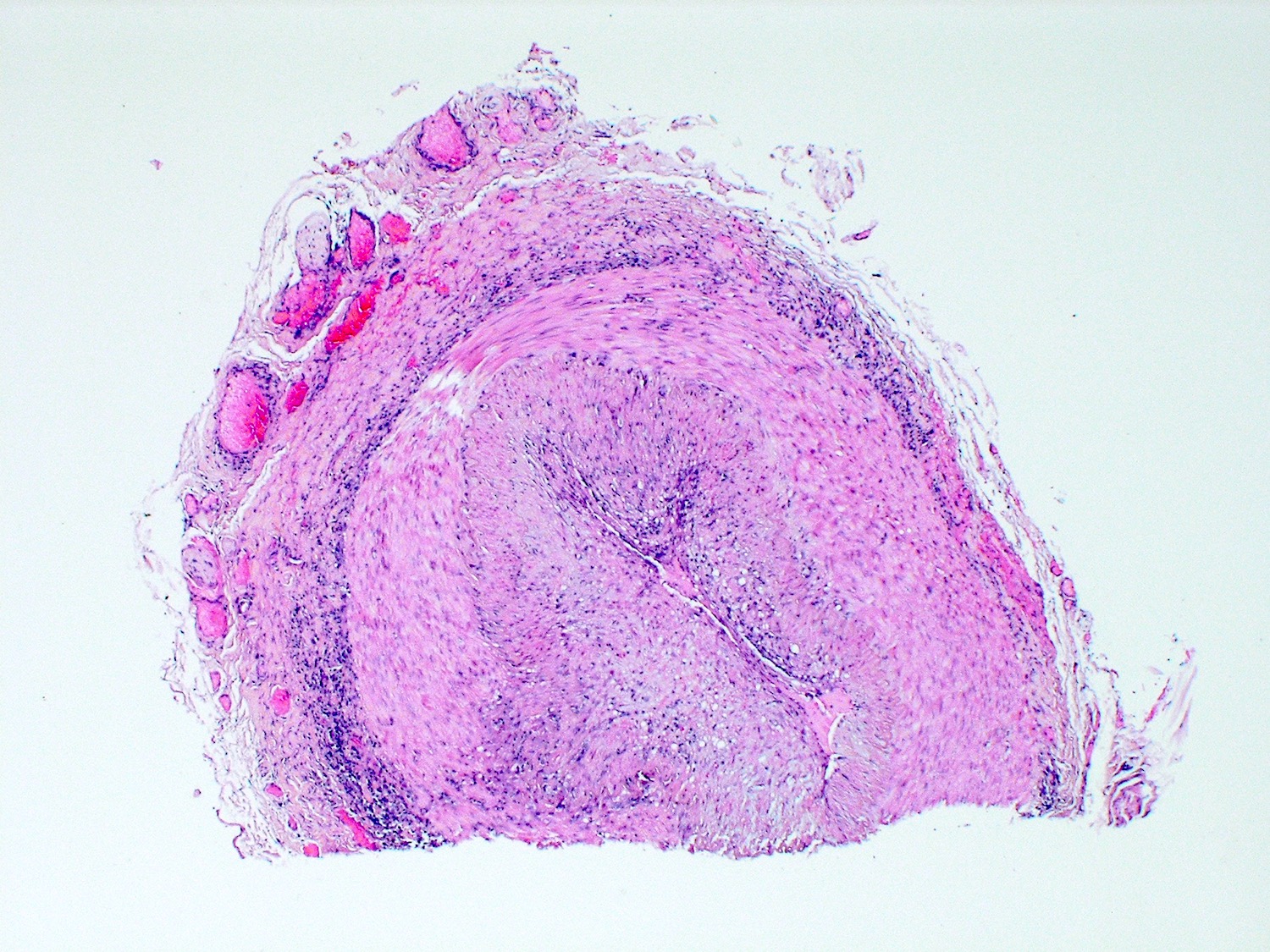
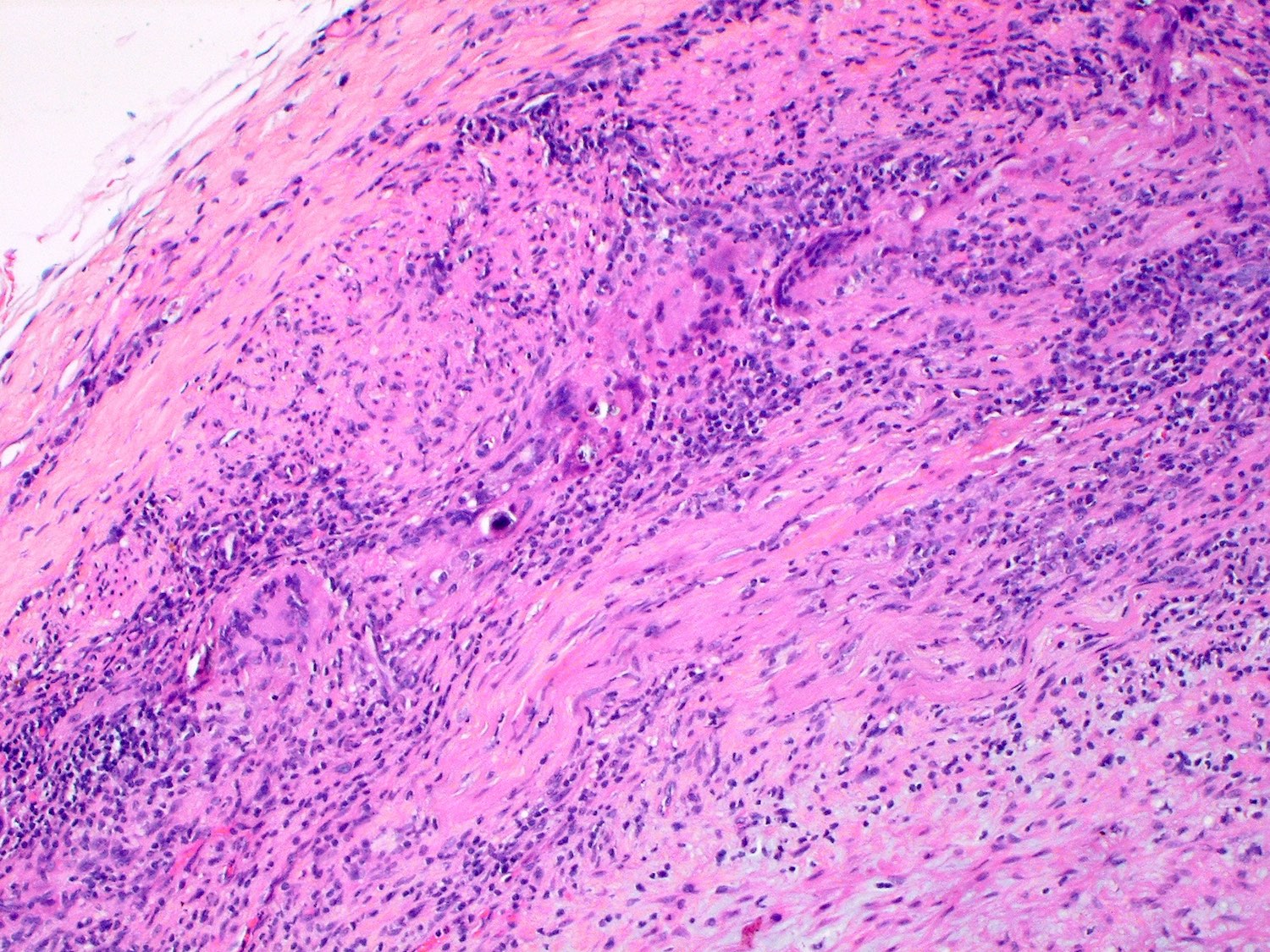
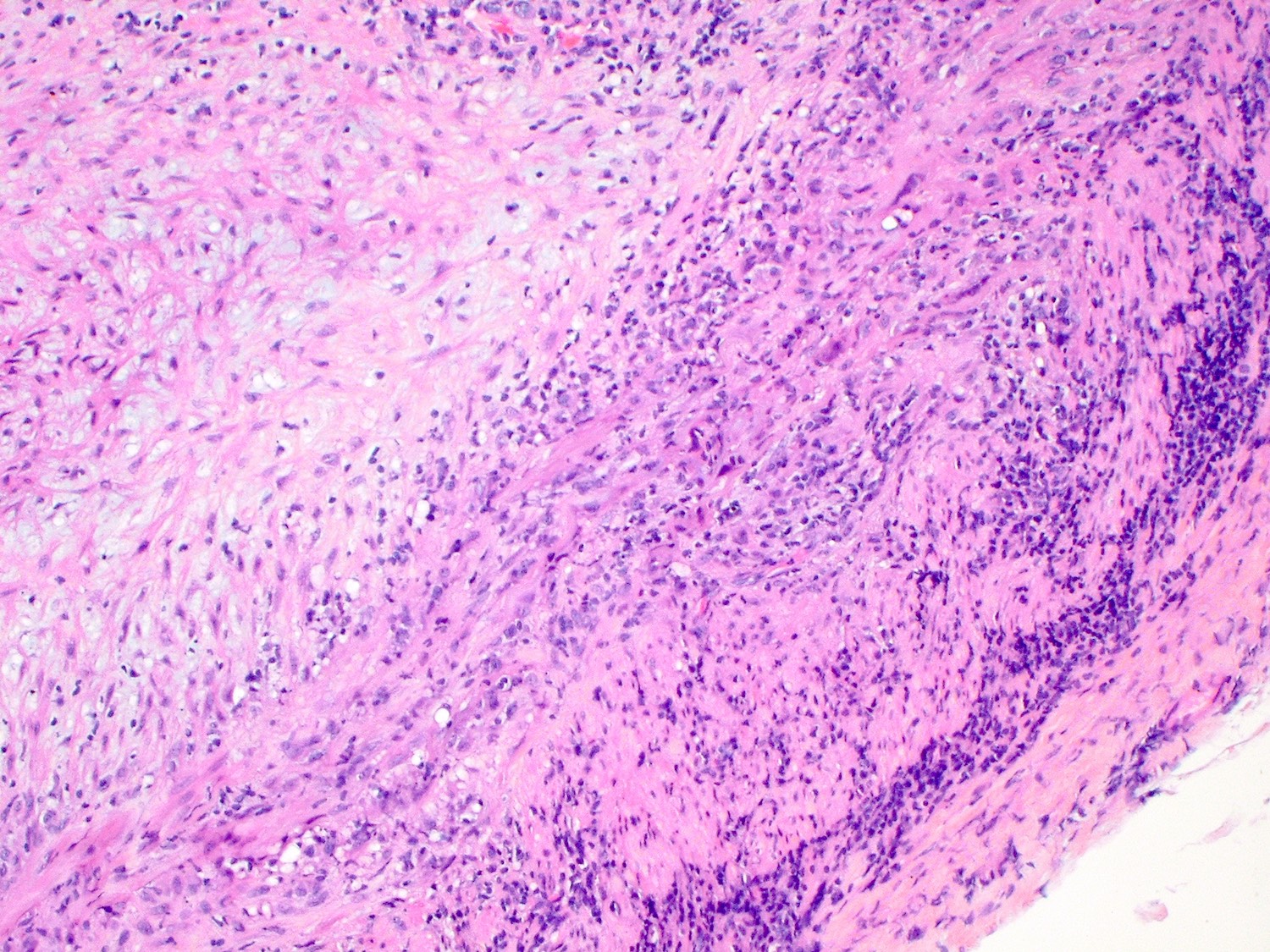
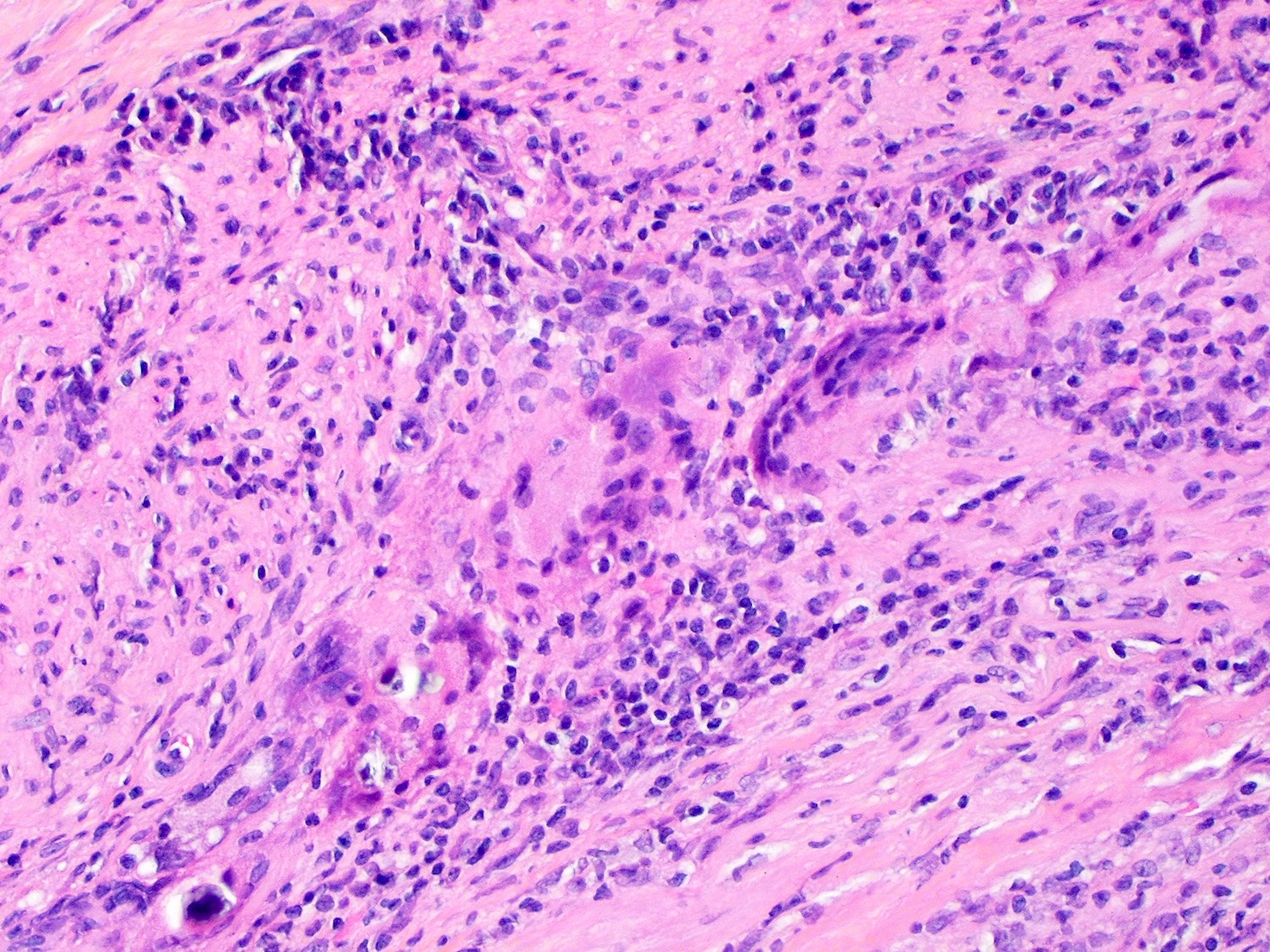
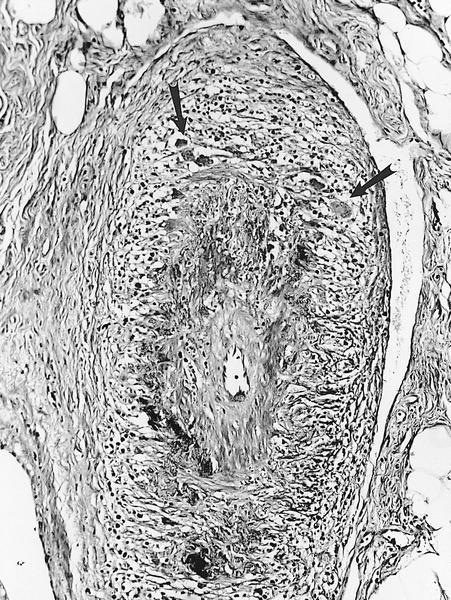
Microscopic (histologic) description
- The following findings are observed classically
- Multifocal segmental destructive arteritis involving all 3 layers of vessel wall
- Transmural inflammation with marked disruption of internal elastic membrane
- Granulomatous inflammation with giant cells at the intima - media junction (J Autoimmun 2016;69:94)
- More intense inflammatory infiltrate with a larger concentration of giant cells is seen during active disease while scant giant cells are seen during the inactive phase (Surg Neurol Int 2022;13:21)
- Transmural inflammatory infiltrate consisting of CD4+ T cells, macrophages, a few eosinophils and neutrophils seen in the highest concentration between the adventitia and media
- Intimal fibrosis and remodeling of blood vessels (Front Immunol 2021;12:623716)
- Other patterns of inflammation called restricted inflammation include small vessel vasculitis, vasa vasorum vasculitis and inflammation limited to adventitia
Microscopic (histologic) images
Positive stains
- Elastic stain shows fragmentation of elastic fibers in vessel wall
- CD68 and CD3 highlight macrophages and T lymphocytes respectively
Sample pathology report
- Left temporal artery, biopsy:
- Histological findings consistent with giant cell arteritis involving the temporal artery (see comment)
- Comment: There is transmural inflammation of the involved vessel with focal lymphocytic and macrophagic infiltrate and occasional giant cells. Disruption of the internal elastic membrane has been demonstrated with the elastic stain, further supporting the diagnosis.
- Gross description: Specimen A is received in formalin in a container and labeled with the patient's name and specimen number and designated left temporal artery. The specimen consists of a tan, tubular structure consistent with a muscular artery that measures 1.2 cm in length and is notably thick and nodular. The specimen is serially cross sectioned at 3 mm intervals, placed between sponges and submitted entirely in 1 cassette.
Differential diagnosis
- Vasculitides like Takayasu arteritis or granulomatosis with polyangitis:
- Histological findings lack granulomatous chronic inflammation and can include fibrinoid necrosis with neutrophilic infiltration
- Antineutrophil cytoplasmic antibodies (ANCA) titers are normal in GCA
- Varicella zoster virus infection:
- Biopsy would show inflammation without granulomas
- Systemic amyloidosis:
- Histological findings include amorphous, homogenous pale eosinophilic areas or hyaline deposits predominantly in the extracellular space that stain positive with Congo red stain
- Lymphoma:
- Biopsy will reveal atypical lymphoid cells with possible clonal proliferation
- Immunohistochemistry will reveal specific markers for specific lymphoma subtypes
- Reference: Front Immunol 2021;12:623716
Board review style question #1
Which of the following histopathological features is characteristic of giant cell arteritis (GCA) and distinguishes it from other vasculitides?
- Extensive eosinophilic infiltrates within vessel walls
- Fibrinoid necrosis with neutrophilic infiltration
- Granulomatous inflammation with giant cells at the intima - media junction
- Homogenous, pale eosinophilic areas
Board review style answer #1
C. Granulomatous inflammation with giant cells at the intima - media junction. The hallmark histopathological feature of GCA is granulomatous inflammation with giant cells at the intima - media junction. Answer A is incorrect because eosinophilic infiltrates within vessel walls are commonly seen in eosinophilic granulomatosis with polyangiitis. Answer B is incorrect because, in contrast, fibrinoid necrosis with neutrophilic infiltration is characteristic of granulomatosis with polyangiitis. Answer D is incorrect because homogenous, pale eosinophilic areas are suggestive of systemic amyloidosis.
Comment Here
Reference: Giant cell arteritis
Comment Here
Reference: Giant cell arteritis
Board review style question #2
Board review style answer #2
A. Chronic inflammation with multinucleated giant cells are the hallmark pathognomonic feature in H&E stained sections of biopsies in GCA.
Answer D is incorrect because intimal fibrosis can also be seen in GCA but it is not prominent in this image. Answers B and C are incorrect because duplication of elastic lamina and fragmentation of elastic fibers can be appreciated with the use of special elastic stain and not on routine H&E sections.
Comment Here
Reference: Giant cell arteritis
Comment Here
Reference: Giant cell arteritis