Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Diagnosis | Radiology description | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jameel R, Li H, Husain AN. Degenerative valve disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/heartdegenerative.html. Accessed April 2nd, 2025.
Definition / general
- Degenerative valve disease is a term used to describe deterioration of the valve over time, which leads to either stenosis or regurgitation from the valve (J Am Coll Cardiol 2006;47:1707)
Essential features
- Degenerative mitral valve disease is more common than aortic valve disease
- Degeneration happens over time due to multiple pathophysiologies
- Diagnosis is made clinically
- Aortic valve often needs replacement whereas mitral valve can be repaired
Terminology
- Calcific aortic stenosis
- Mitral annular calcification, mitral degenerative disease
- Mitral valve prolapse (Barlow syndrome), floppy valve disease, balloon mitral valve
ICD coding
- ICD-10: I35.9 - nonrheumatic aortic valve disorder, unspecified
Epidemiology
- Calcific aortic stenosis is seen in ~9 million people worldwide
- Calcific aortic stenosis is highly age related; an increasing trend is noted in developed countries (Nat Rev Cardiol 2021;18:853)
- Degenerative mitral valve disease is seen in ~24 million people (Nat Rev Cardiol 2021;18:853)
Sites
- Aortic and mitral valves
Pathophysiology
- In calcific aortic stenosis, prior injury due to hyperlipidemia, hypertension, inflammation and other factors precede calcification of the valve
- This leads to the release of VEGF, leading to angiogenesis and collagen X which leads to calcification of the valve
- These valves contain abnormal cells which resemble osteoblasts, which synthesize bone matrix and deposit calcium (J Cardiol 2018;71:215)
- In degenerative mitral stenosis, calcific deposits develop in the peripheral fibrous ring (annulus), which are stony hard, irregular ulcerated nodules which appear behind the leaflets
- In degenerative mitral valve prolapse, there are portions of the leaflets that become thick, redundant and rubbery
- Over time, the chordae tendineae become thinner and rupture, leaving the annulus dilated; this rupture allows the valves to become floppy and prolapse into the atrium during systole
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Etiology
- Old age is the most common cause of degenerative valve disease
- Early occurrence of degeneration can occur if the patient has a prior valve disease (Int J Stroke 2018;13:612)
Diagrams / tables
Diagnosis
- Many patients are not diagnosed until they develop symptoms
- Auscultation during routine checkup plays an important role in diagnosis
- Following auscultation, patients can undergo echocardiography for definite diagnosis
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Radiology description
- Calcified aortic valve
- Late in the disease, chest radiograph might reveal aortic calcifications and enlargement of the heart along with pulmonary congestion and alveolar edema
- On echocardiogram, severity is determined by various factors
- Mild aortic stenosis: jet velocity of 2.6 - 2.9 m/s and aortic valve area of > 1.5 cm
- Moderate aortic stenosis: jet velocity of 3 - 4 m/s and aortic valve area of 1 - 1.5 cm
- Severe aortic stenosis: jet velocity of > 4 m/s and aortic valve area of < 1 cm (Radiopaedia: Aortic Valve Stenosis [Accessed 19 January 2023])
- Mitral valve prolapse
- On echocardiography, the coaptation (closing of the valves) line lies behind the annular plane (Radiopaedia: Mitral Valve Prolapse [Accessed 7 April 2023])
- Mitral annular calcification
- On a frontal chest radiograph, calcification can be observed in the expected location of the mitral valve
- CT scan is more sensitive for detection of calcification on the annulus but it is subject to degree of motion artifact (Radiopaedia: Mitral Annular Calcification [Accessed 19 January 2023])
Case reports
- 39 year old man with epilepsy, hypertension and a 1 month history of worsening shortness of breath was diagnosed with pulmonary edema (BMJ Case Rep 2019;12:e228414)
- 50 year old man with a history of atrial fibrillation, hypertension, diverticulitis and asthma presented with fatigue and moderate exertional dyspnea (Autops Case Rep 2018;8:e2018058)
- 55 year old man with a history of erosive, seropositive rheumatoid arthritis and interstitial lung disease presented with shortness of breath (Front Cardiovasc Med 2017;4:14)
Treatment
- In severe aortic valve stenosis, transcatheter aortic valve replacement offers a better survival rate; percutaneous balloon valvotomy can also serve as a treatment option for poor surgical candidates
- In mitral valve disease, transcatheter mitral valve repair is considered better than open heart surgery due to the low risk associated with it (Mayo Clin Proc 2010;85:483)
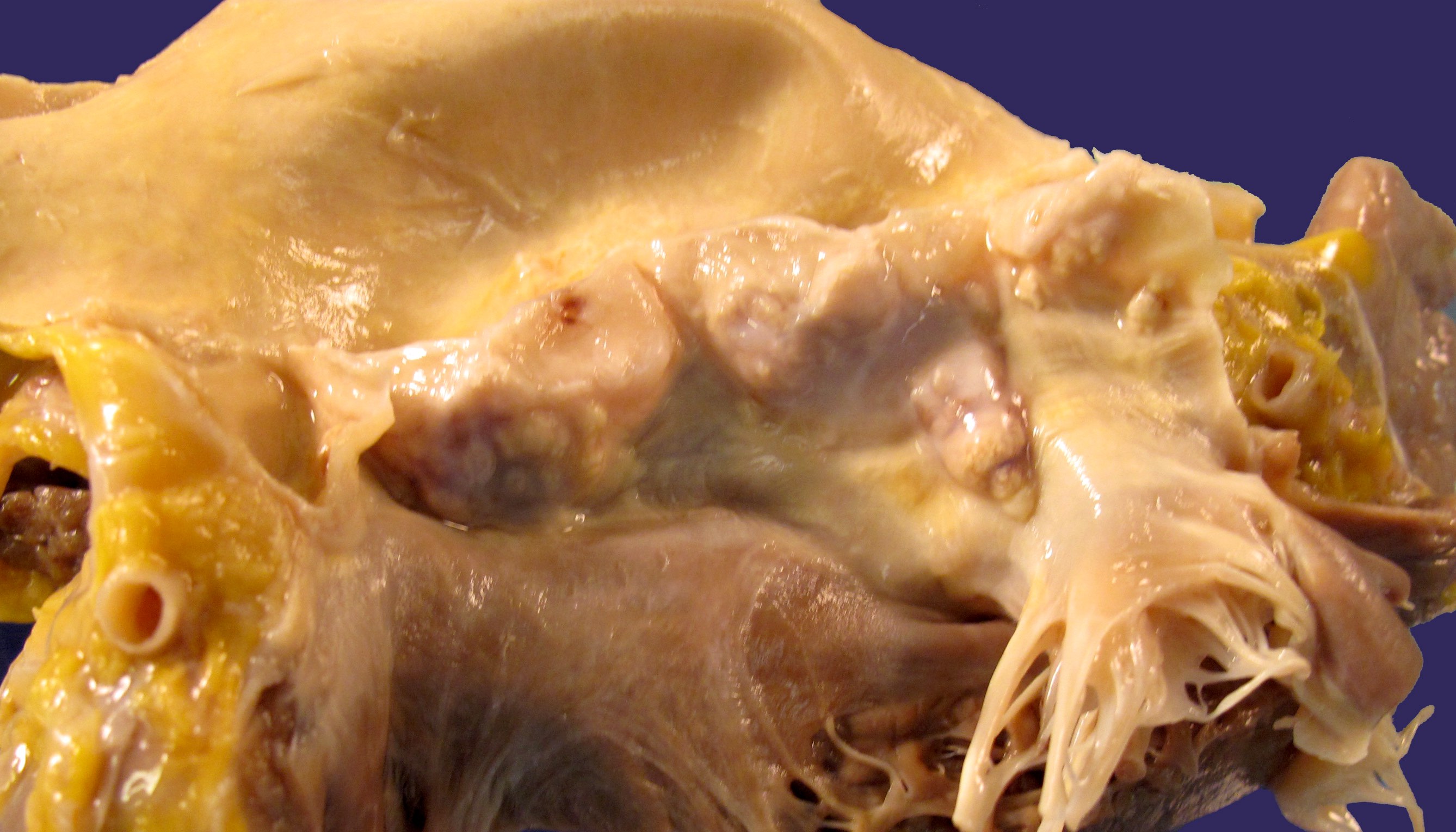
Gross description
- Calcified aortic valve
- Heaped up calcified cusps that prevent valve opening is hallmark
- In the early stages, calcification begins in the valvular fibrosa at the point of maximal cusp flexion
- Gradual narrowing of the orifice is noted
- Mitral annular calcification
- Calcific deposits are seen as irregular, stony hard and ulcerated nodules
- Mitral valve prolapse
- The leaflets appear enlarged, rubbery and thick with the connecting chordae tendineae appearing as thin, elongated or sometimes even ruptured
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Gross images
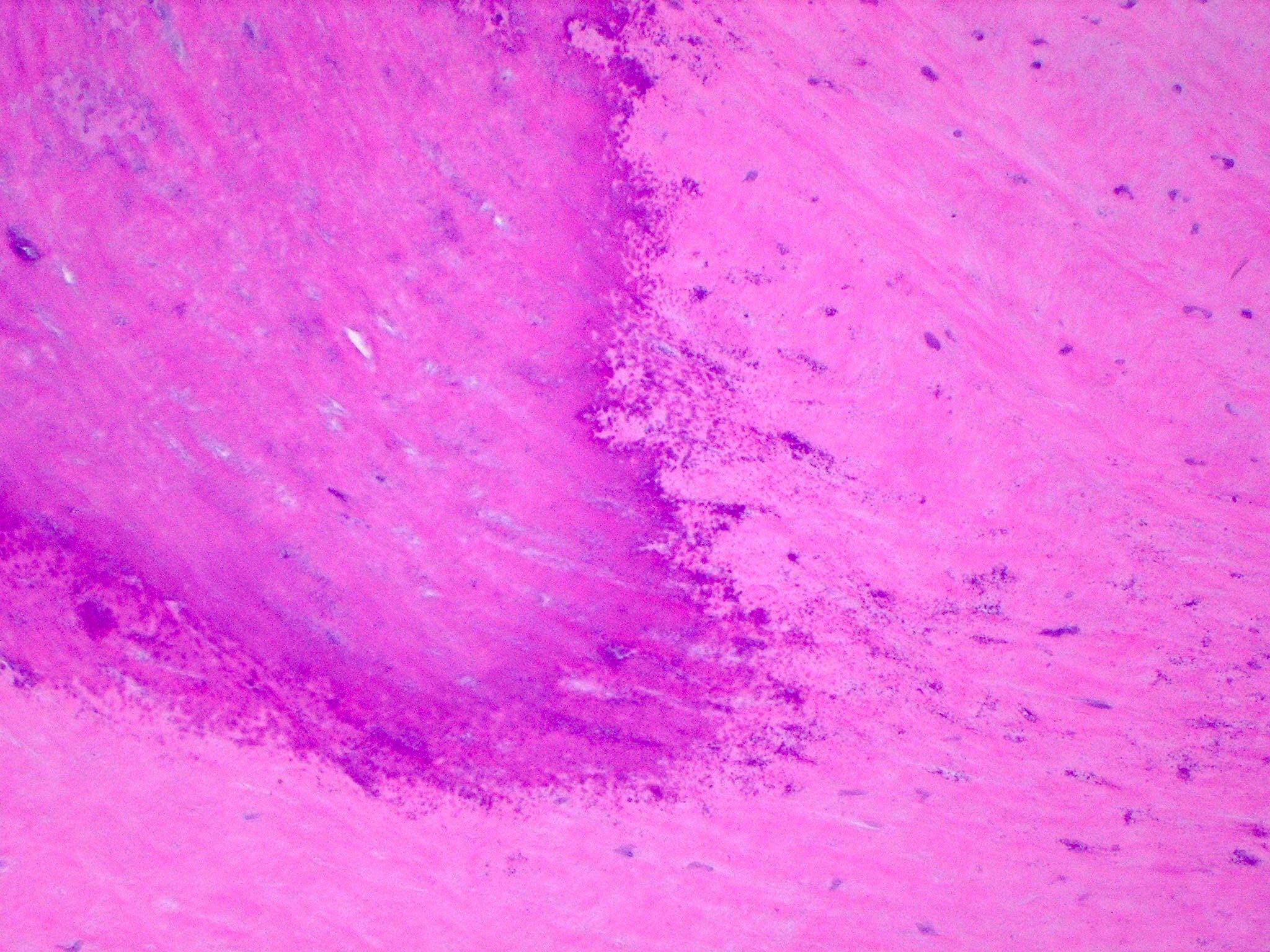
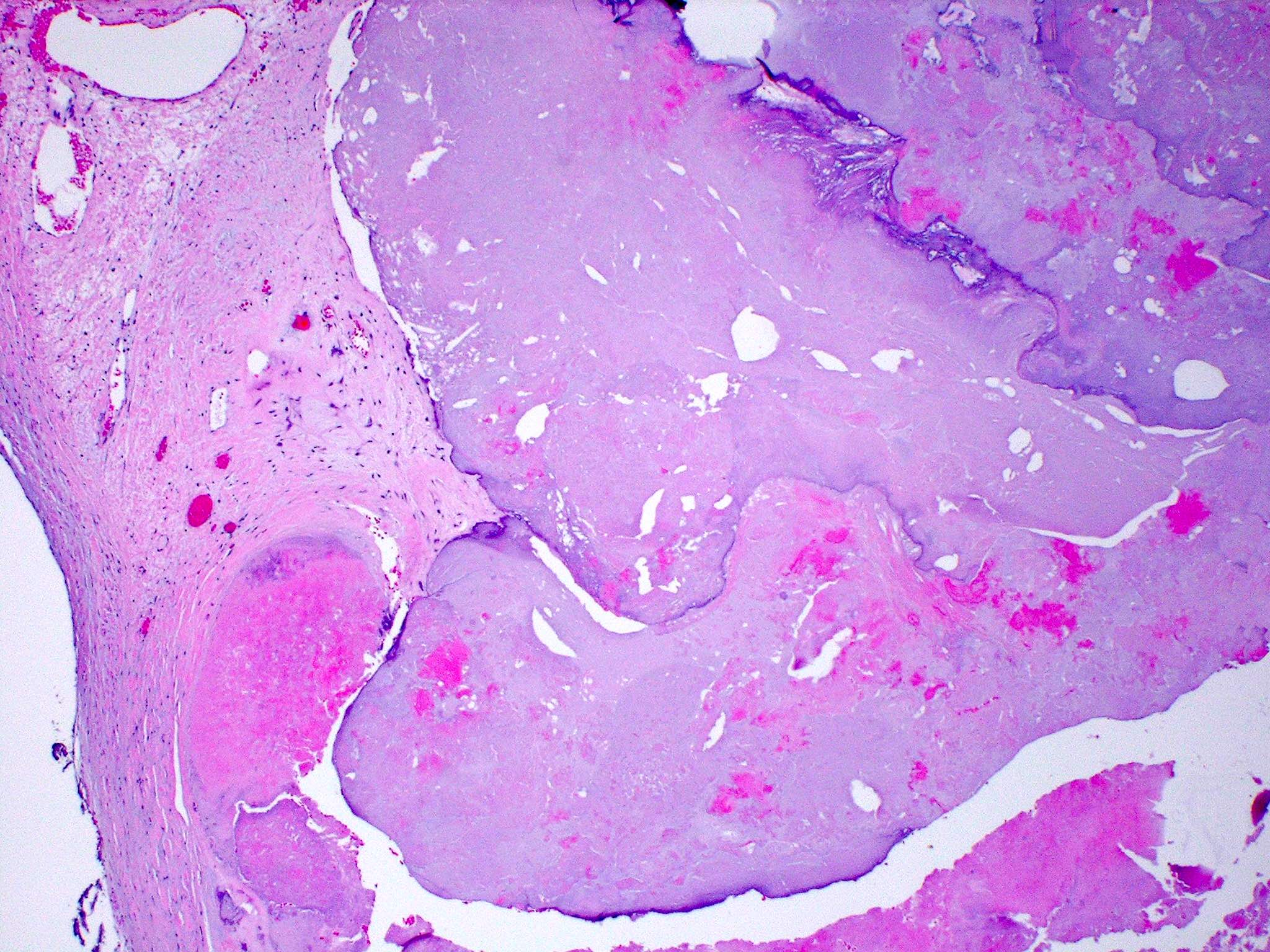
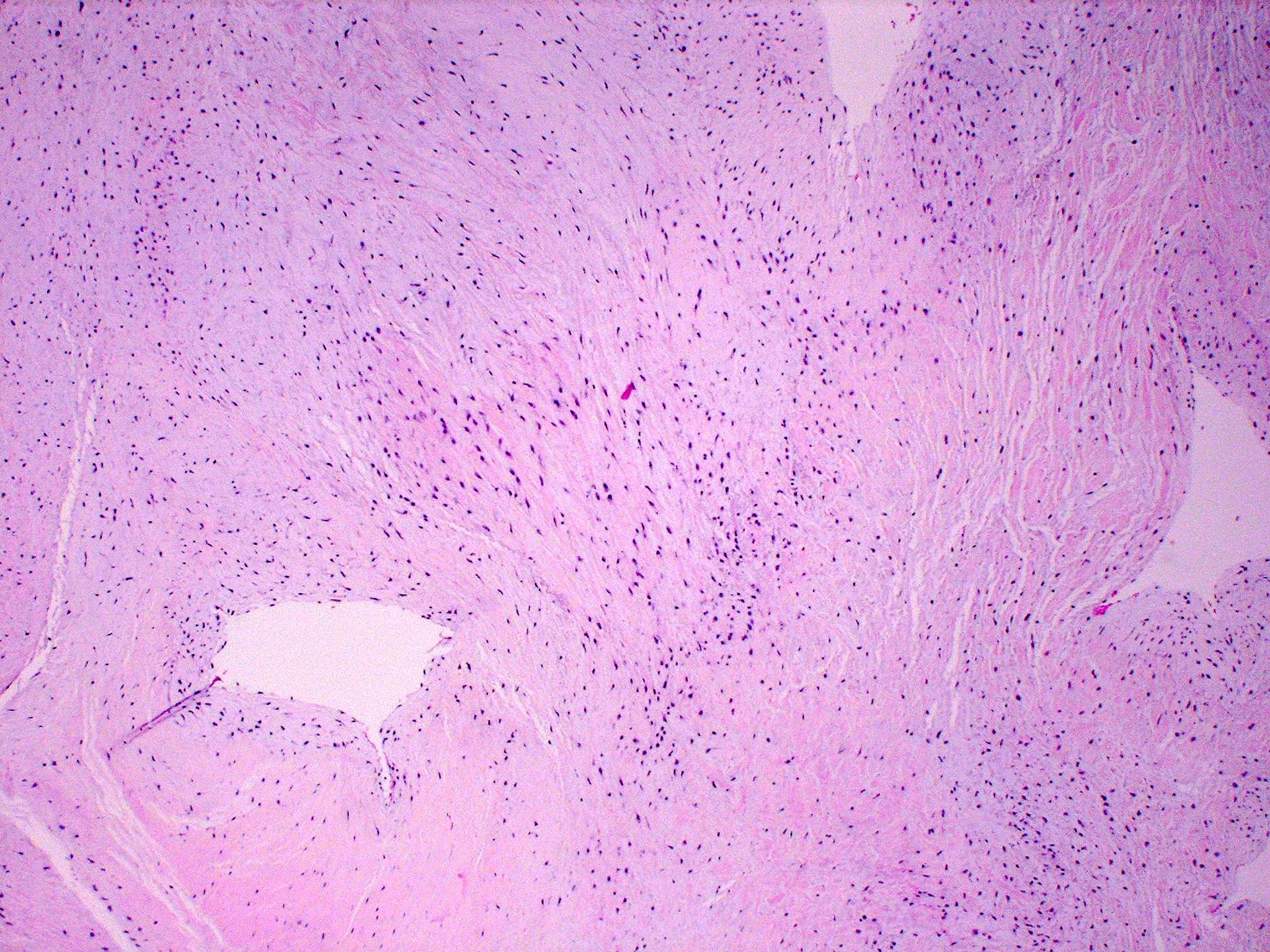
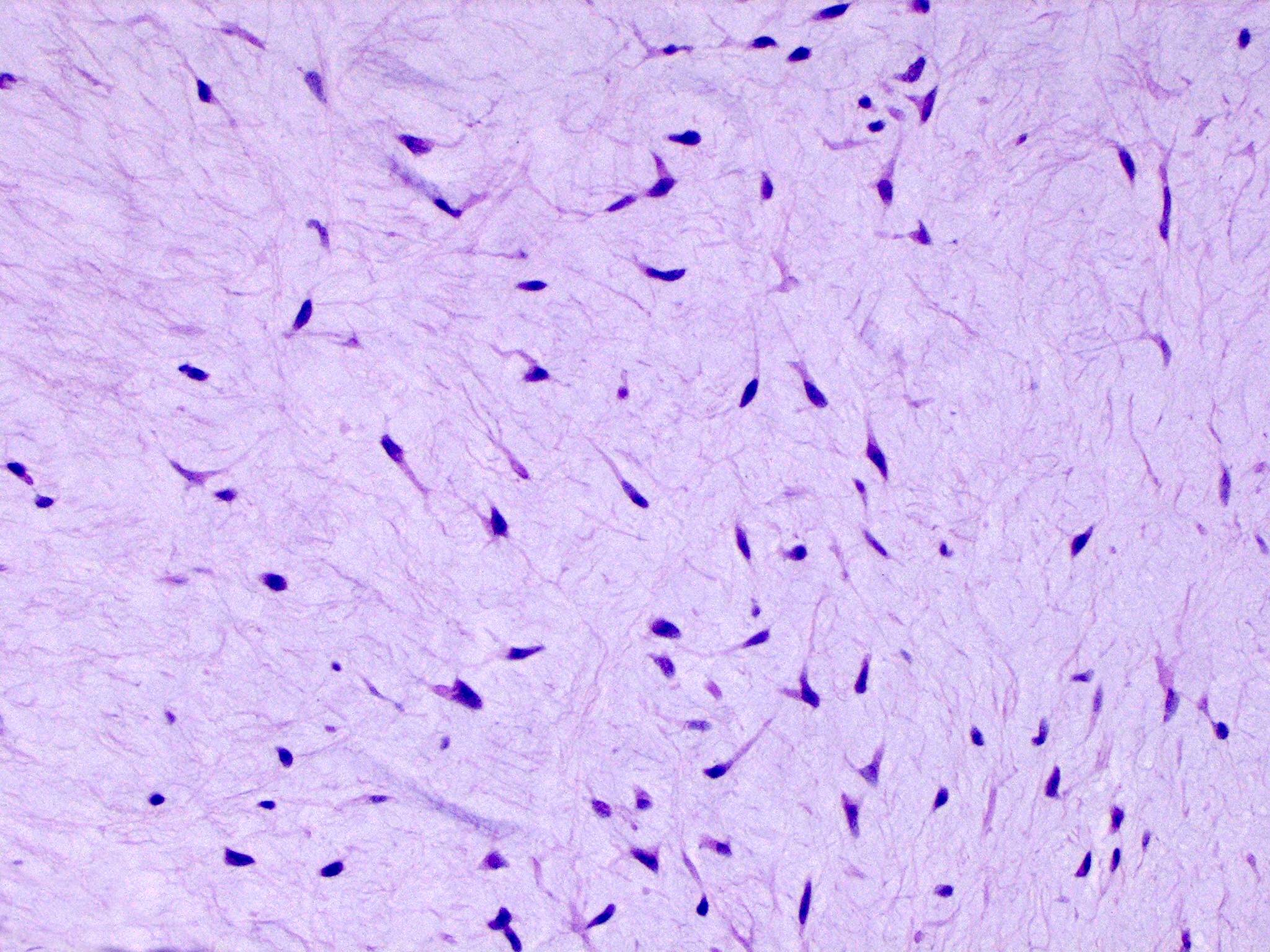
Microscopic (histologic) description
- Calcified aortic valve
- Large nodular calcific deposits obstructing the functional valve area
- Mitral valve prolapse
- Outer collagenous layer appears weakened, whereas the middle spongiosa layer appears thicker due to deposition of myxomatous material
- Over time, there is more deposition of myxomatous material leading to rupture of the chordae tendineae
- Reference: Kumar: Robbins & Cotran Pathologic Basis of Disease, 10th Edition, 2020
Microscopic (histologic) images
Sample pathology report
- Mitral valve, repair:
- Fibromyxoid valvular degeneration
Differential diagnosis
- Bicuspid aortic valve:
- Congenital disease
- On gross appearance, aortic valve presents with 2 cusps compared to a normal valve of 3 cusps
- Rheumatic heart valve:
- Acute rheumatic fever
- On gross examination, there are small vegetations on involved valves, typically mitral and aortic valves
- On microscopic examination, Aschoff bodies (collections of lymphocytes, plasma cells and activated macrophages) can be seen in any part of the heart, including valves and myocardium
- Chronic rheumatic fever
- On gross examination, valves exhibit leaflet thickening, commissural fusion and shortening along with fusion of the chordae tendineae
- On microscopic examination, the valves exhibit fibrosis and calcifications
- Acute rheumatic fever
- Infectious endocarditis:
- On gross appearance of both acute and subacute infectious endocarditis, friable and bulky vegetations are seen on the valve
- On microscopic examination, the vegetations consist of fibrin, inflammatory cells and microorganisms
- In subacute infectious endocarditis, granulation tissue may be present; fibrosis and calcification occurs over time
Board review style question #1
Which specific degenerative valve disease is the most common worldwide?
- Bicuspid aortic valve
- Calcific aortic stenosis
- Degenerative mitral valve
- Myxomatous mitral valve degeneration
Board review style answer #1
C. Degenerative mitral valve. Degenerative mitral valve disease is the most common, occurring in ~24 million people worldwide compared with 9 million with calcific aortic stenosis, which is the second most common.
Comment Here
Reference: Degenerative valve disease
Comment Here
Reference: Degenerative valve disease
Board review style question #2
What test is used for definitive diagnosis of degenerative mitral valve?
- Chest MRI
- Chest ultrasonography
- Echocardiogram
- Physical examination
Board review style answer #2
C. Echocardiogram. Patients undergo auscultation at regular intervals to confirm the diagnosis, whereas a definitive diagnosis can be made with an echocardiogram once the diagnosis has been established.
Comment Here
Reference: Degenerative valve disease
Comment Here
Reference: Degenerative valve disease