Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Musick A, Glass C. Chronic allograft vasculopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/heartchronicgraftvasculopathy.html. Accessed April 3rd, 2025.
Definition / general
- Diffuse, concentric hyperplasia of the coronary vasculature after orthotopic heart transplantation, resulting in progressive luminal narrowing, ischemic injury and allograft failure
Essential features
- Long term complication after heart transplantation
- Invasive coronary angiography is diagnostic
- Concentric intimal hyperplasia of the epicardial arteries / veins and medial disease of the intramyocardial microvasculature
ICD coding
Epidemiology
- Long term complication after orthotopic heart transplant causing over 10% mortality at 3 years and affecting 47% of patients within 10 years
- Increased incidence / risk:
- Donor factors: older age (≥ 50 year old), white race, male sex, elevated weight (≥ 85 kg) and history of hypertension, diabetes or tobacco use (Ann Thorac Surg 2010;90:168)
- Recipient factors: dyslipidemia, glucose intolerance, increased hsCRP and CMV IgG/IgM positivity (Transplant Proc 2008;40:3056, J Am Coll Cardiol 2004;43:1034, Transplantation 2003;76:1470, J Heart Lung Transplant 2007;26:324, J Am Coll Cardiol 2003;42:477)
- Increasing time after transplant (J Heart Lung Transplant 2017;36:1037)
- Earlier onset (within 5 years):
- Donor factors: hypertension and male
- Recipient factors: male, black race and pretransplant coronary artery disease (J Heart Lung Transplant 1998;17:744)
- Greater number of HLA-DR mismatches
- Increased transplant center volume (J Heart Lung Transplant 2007;26:769)
Sites
- Allograft epicardial and intramyocardial arteries and veins (Circulation 1997;96:2069)
- Sparing of recipient vessels (Can J Surg 2005;48:319)
Pathophysiology
- Host allorecognition of donor HLA on coronary endothelium → T cell activation → altered cytokine expression → endothelial activation, vascular smooth muscle proliferation and extracellular matrix deposition → intimal (epicardial) or medial (microvasculature) thickening and vasculopathy (Circulation 2007;116:1274)
- Formation of anti HLA or anti endothelial antibodies → increased risk of chronic allograft vasculopathy and cardiovascular mortality (J Heart Lung Transplant 2006;25:1277, J Heart Lung Transplant 2010;29:717, Circulation 1989;80:III122)
- Nonimmunological factors (e.g., coronary artery disease, tobacco use) → endothelial dysfunction and vascular inflammation → enhanced graft immunogenicity (Croat Med J 2014;55:562)
Etiology
- Interplay between immunologic (cellular / antibody mediated rejection and HLA matching) and nonimmunologic (e.g., recipient hyperlipidemia, donor hypertension) factors
Clinical features
- Rarely present with angina due to allograft denervation
- Arrhythmia, diaphoresis, exertional dyspnea, gastrointestinal distress, progressive heart failure, sudden cardiac death or syncope (Croat Med J 2014;55:562)
Diagnosis
- Concentric intimal hyperplasia of the left anterior descending artery (> 70% stenosis on angiography with clinically demonstrated allograft dysfunction; International Society for Heart and Lung Transplantation grade CAV 3)
- Multifocal mild acute cellular allograft rejection with focal myocyte necrosis (International Society for Heart and Lung Transplantation grade 1R; 1990 grade 2)
- pAMR 0: no significant evidence of antibody mediated rejection on immunohistology
- Quilty effect: moderate focal endocardial inflammatory cell aggregate with myocardial encroachment
- Clinical information
- Cardiac allograft vasculopathy status post orthotopic heart transplant
Radiology description
- Coronary angiography: diffuse, longitudinal and concentric luminal narrowing of primary or branch vessels (J Heart Lung Transplant 2010;29:717)
- Intravascular ultrasound: increased maximal intimal thickness of the coronary arteries, predominantly left anterior descending (J Am Coll Cardiol 2005;45:1532)
Radiology images
Prognostic factors
- Favorable: late onset (J Heart Lung Transplant 2010;29:717)
- Poor: stenotic microvasculopathy with minimal intimal thickening on intravascular ultrasound of ≥ 0.5 mm and abnormal dobutamine stress echocardiography within first year (Circulation 2007;116:1274, Circulation 2009;120:1561, Circulation 1999;100:509, Cardiovasc Revasc Med 2019 Jan 25 [Epub ahead of print])
Case reports
- 27 year old woman with pregnancy related HLA-II sensitization (Transplant Proc 2013;45:800)
- 32 year old man with Danon disease requiring repeat transplantation (Rev Cardiovasc Med 2018;19:69)
- 40 year old man with total vascular scaffold resorption following treatment for advanced disease (JACC Cardiovasc Interv 2017;10:1270)
- 43 year old woman with early disease (Case Rep Med 2012;2012:734074)
- 58 year old man treated with a drug eluting stent (Heart 2005 Feb;91:e11)
Treatment
- Preventative therapy: statins and posttransplantation immunosuppressants
- Palliative therapy: percutaneous coronary intervention and coronary artery bypass (Catheter Cardiovasc Interv 2018;92:E527)
- Repeat transplantation is the only definitive treatment (Croat Med J 2014;55:562)
Gross description
- Thickened intramural arteries on the ventricular cut surface (Arch Pathol Lab Med 2007;131:1169)
- Gross luminal narrowing of the epicardial coronary arteries
- Focal areas of myocardial scarring (J Heart Lung Transplant 2011;30:1044)
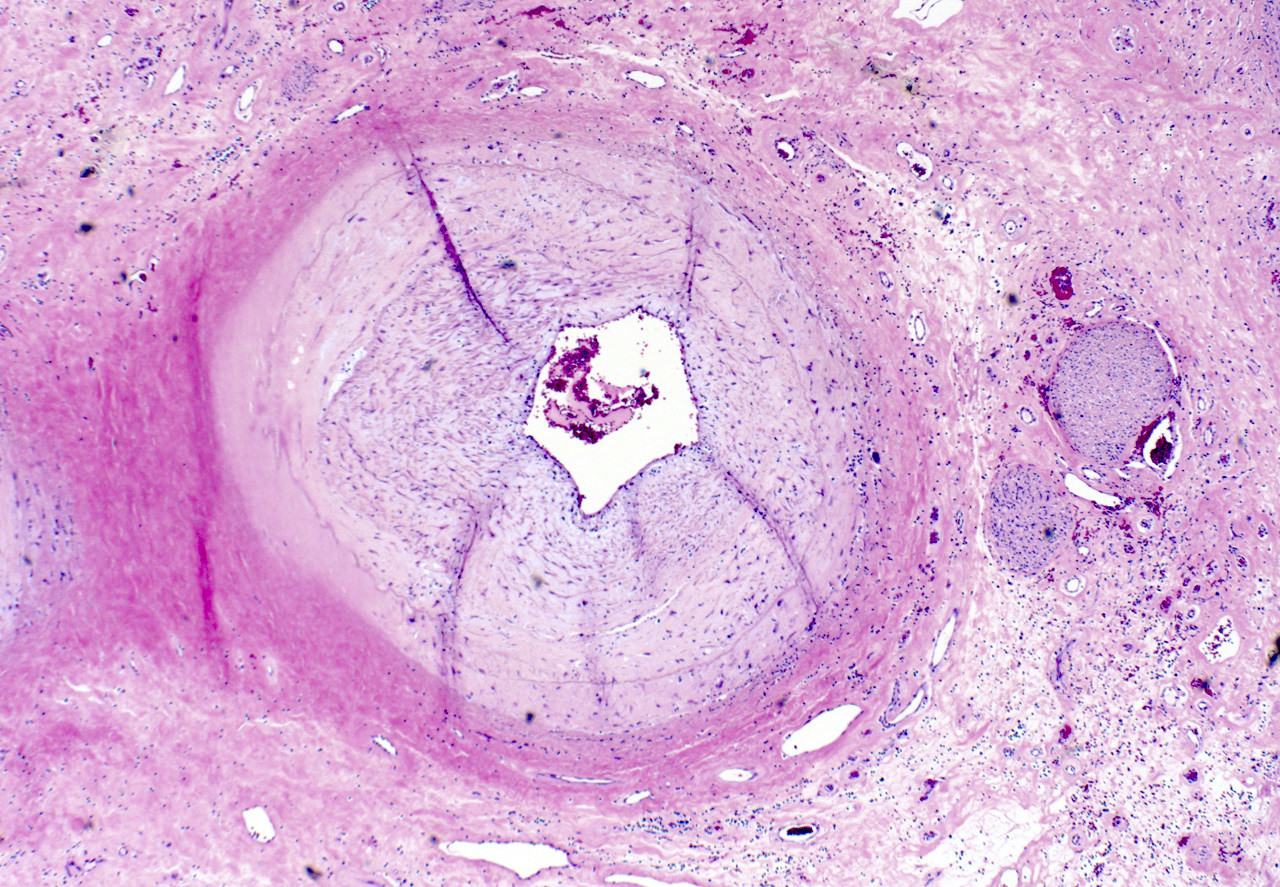
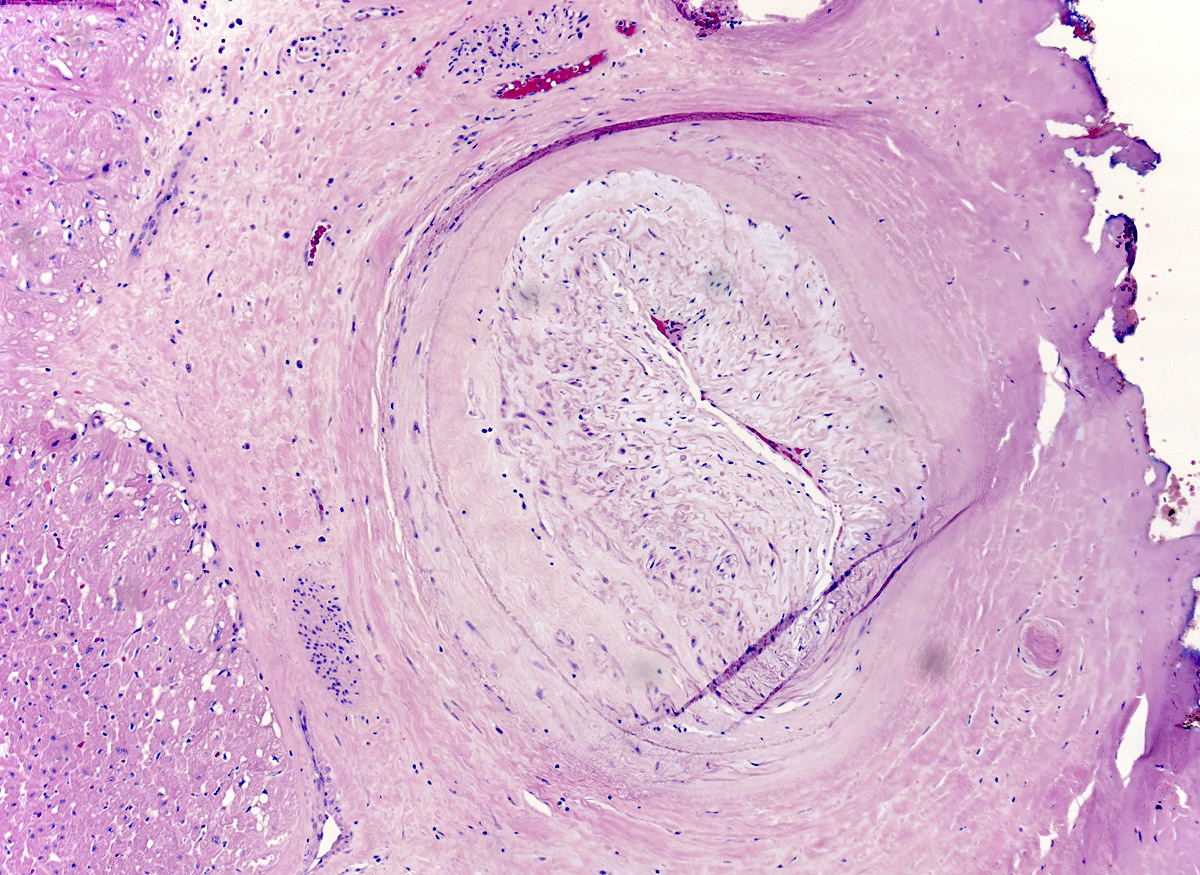
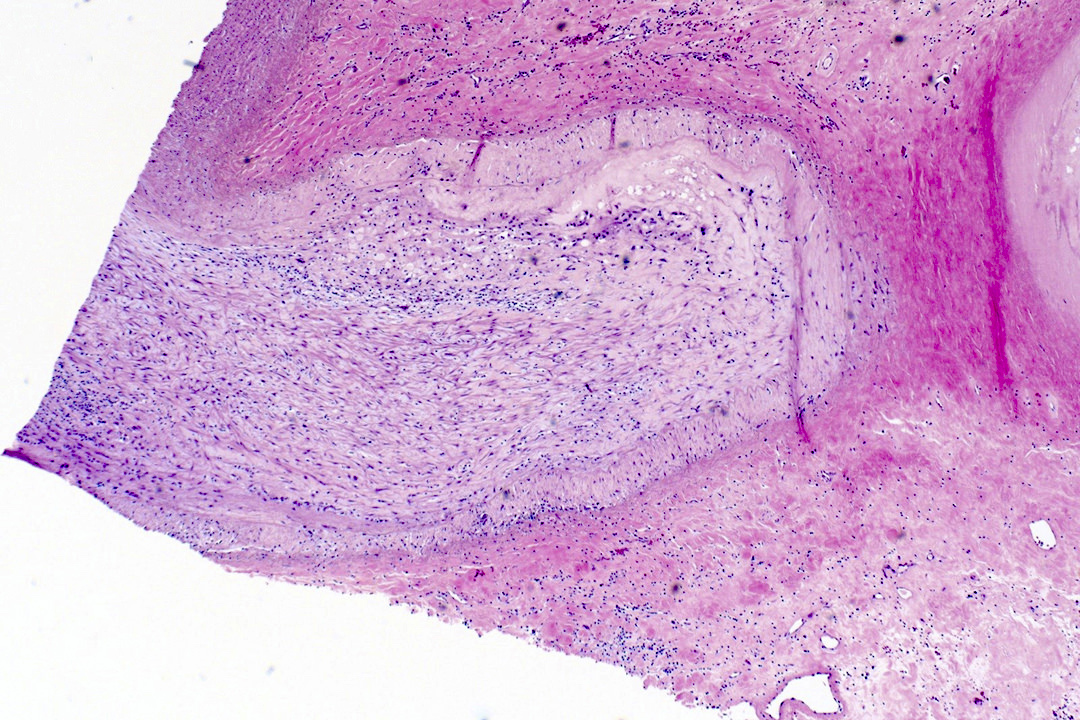
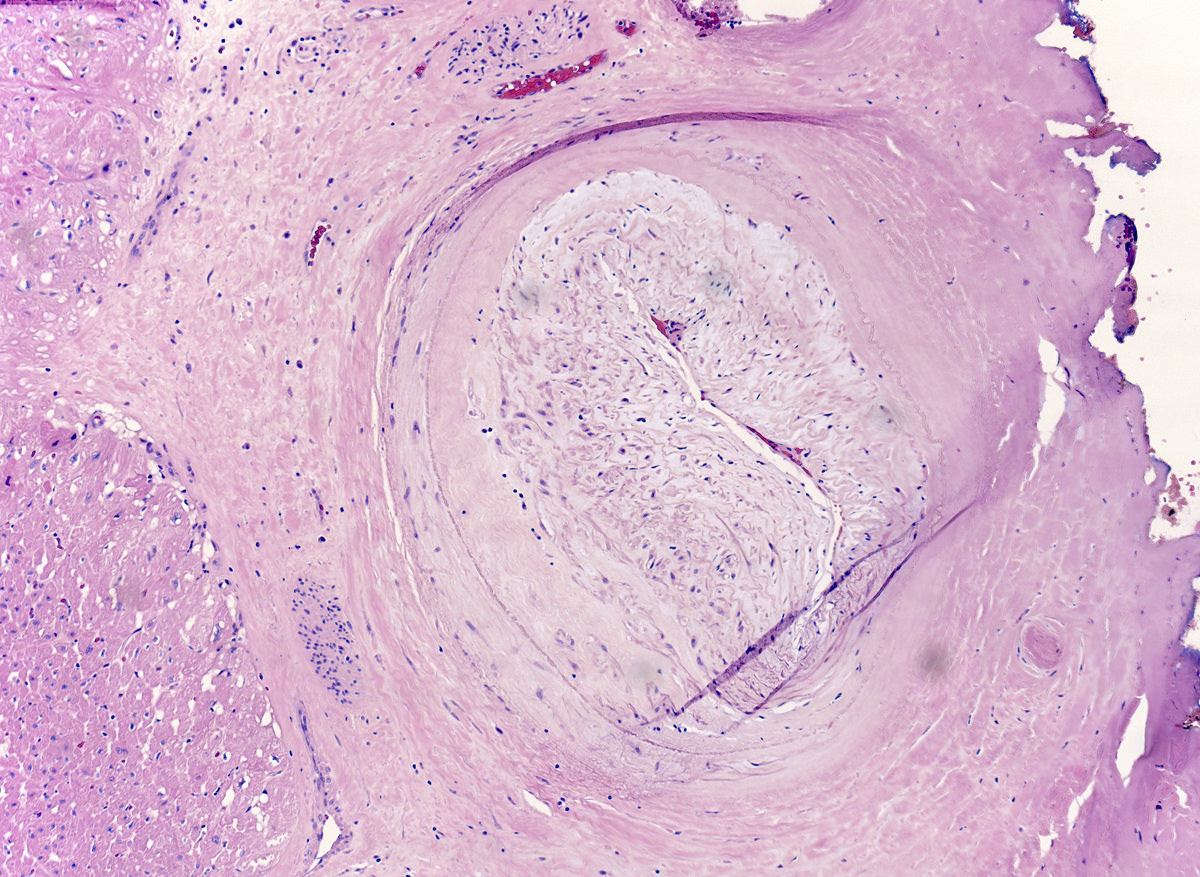
Microscopic (histologic) description
- Endomyocardial biopsy of intramyocardial arteries (J Heart Lung Transplant 2011;30:1044):
- Concentric fibromuscular intimal and medial thickening with luminal stenosis
- Subendothelial lymphocytic accumulation
- Perivascular fibrosis
- Epicardial artery and vein sections (Catheter Cardiovasc Interv 2018;92:E527):
- Concentric intimal thickening (proliferation of smooth muscle cells and myofibroblasts) along vessel length with luminal stenosis
- Variable mononuclear inflammatory infiltrate (T lymphocytes, macrophages and foam cells) in the intima, media, or adventitia
- May have fibrinoid necrosis of the media and damage to the inner elastic lamina
- Myocardial sections (Arch Pathol Lab Med 2007;131:1169):
- Bilateral, patchy ischemic injury (acute and healing) with myocytolysis, coagulative necrosis and interstitial fibrosis
- May have coincident atheromatous plaques, usually eccentric and proximal
Microscopic (histologic) images
Immunofluorescence description
- CD11c and IgM/IgG IF usually absent (Circulation 2015;131:1608)
Positive stains
- CD3 (Leu4) and CD68 may be positive particularly in subendothelium (Catheter Cardiovasc Interv 2018;92:E527)
Negative stains
- C4d deposition absent around interstitial capillaries
Sample pathology report
- Given the histological heterogeneity of chronic allograft vasculopathy, this is a diagnosis made clinically rather than microscopically. The ISHLT grading guidelines rely upon coronary angiography (demonstrating luminal narrowing of primary vessels) and assessment of allograft function (i.e. ultrasound or echo). While this entity does have distinct microscopic features, it is usually not included in a pathology report line diagnosis.
Differential diagnosis
- Acute cellular rejection:
- Presence of a mononuclear inflammatory infiltrate but lacks angiographic evidence supporting chronic allograft vasculopathy (J Heart Lung Transplant 2009;28:320)
- Acute antibody mediated rejection:
- Positive immunofluorescence for immunoglobulins, complement and CD68 staining for macrophages (J Heart Lung Transplant 2005;24:1710)
- Posttransplant lymphoproliferative disease:
- EBV seroconversion or reactivation of anti-EBV IgM with constitutional symptoms (J Heart Lung Transplant 2005;24:1710)
- Infectious myocarditis:
- Demonstration of infectious entity on endomyocardial biopsy
- Coronary artery vasospasm:
- Resolved with intracoronary nitroglycerin (Croat Med J 2014;55:562)
- Atherosclerotic coronary artery disease:
- Slow progression of focal lesions limited to the arteries (Circ Res 2006;99:801)
Board review style question #1
A 34 year old Hispanic man underwent an orthotopic heart transplantation six years ago following intractable idiopathic restrictive cardiomyopathy where he received a heart from a 25 year old white woman. Routine posttransplant endomyocardial biopsies showed no histological evidence of rejection but surveillance coronary angiography and intravascular ultrasound recently revealed diffuse, circumferential thickening of the left anterior descending artery with significant intimal thickening and 70% luminal stenosis. The patient has no history of dyslipidemia, diabetes or CMV infection. Which of the following is a significant risk factor in the development of this patient's disease?
- Absence of histological evidence of rejection
- Donor female sex
- Donor white race
- Donor young age
- Recipient CMV IgG/IgM seronegativity
Board review style answer #1
C. This patient has chronic allograft vasculopathy as indicated by diffuse concentric intimal hyperplasia and 70% stenosis of a single primary vessel (left anterior descending) on angiography. White race of the donor is associated with an increased incidence of cardiac allograft vasculopathy in the recipient. Recipient CMV IgG/IgM seropositivity, not seronegativity, is also associated with an increased risk of disease. Absence of histological evidence of rejection has no effect on incidence and may be reflective of sampling error (i.e., biopsies did not capture diseased microvasculature). Donor old age and male sex, not young age and female sex, are risk factors for the development of cardiac allograft vasculopathy.
Comment Here
Reference: Chronic allograft vasculopathy
Comment Here
Reference: Chronic allograft vasculopathy
Board review style question #2
A 51 year old woman received an orthotopic heart transplant four years ago due to end stage dilated cardiomyopathy. One year ago, she began experiencing mild exertional dyspnea. At that time, invasive angiography demonstrated 60% stenosis and diffuse narrowing of the left circumflex artery. Over time, the patient developed progressive heart failure and required a repeat transplantation. A representative section of her explanted heart is shown above.
Which of the following statements about this disease is true?
- Although donor vasculature is affected, recipient vasculature is spared
- Characteristic mononuclear inflammatory infiltrate is limited to the adventitia
- Concentric intimal thickening and luminal stenosis is found in epicardial arteries but not epicardial veins
- Development of the disease is closely associated with EBV seroconversion or reactivation of anti-EBV IgM
- Positive immunofluorescence for IgG, IgM or IgA is diagnostic of the disease
Board review style answer #2
A. This patient has chronic allograft vasculopathy as indicated by diffuse concentric intimal hyperplasia and 60% stenosis of a single primary vessel (left main coronary artery) on angiography. The patient's biopsy also shows severe intimal hyperplasia with marked luminal stenosis. In this disease, the donor coronary vasculature is affected while the recipient vasculature is spared. EBV seroconversion or reactivation is more associated with posttransplant lymphoproliferative disease. While acute antibody mediated rejection events (indicated by immunofluorescence in choice B) may occur in the context of cardiac allograft vasculopathy, it is not diagnostic. The inflammatory infiltrate seen in the disease may occur in any layer of the vessel and concentric intimal thickening may occur in both epicardial arteries and veins.
Comment Here
Reference: Chronic allograft vasculopathy
Comment Here
Reference: Chronic allograft vasculopathy