Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Arif U, Windon AL. Metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladdermetaplasia.html. Accessed April 2nd, 2025.
Definition / general
- Nonneoplastic change of the native biliary type epithelium to nonnative epithelium, most commonly as a consequence of chronic inflammation
Essential features
- Most commonly found in gallbladders with chronic mucosal injury from gallstones or from a chronic inflammatory condition
- Thought to be part of a metaplasia - dysplasia - carcinoma sequence related to chronic mucosal injury
- Intestinal and gastric foveolar type metaplasia are more commonly associated with dysplasia and adenocarcinoma
Terminology
- Intestinal metaplasia
- Gastric metaplasia (pseudopyloric / pyloric gland, foveolar, antral type)
- Squamous metaplasia
ICD coding
- ICD-10: K82.8 - other specified diseases of gallbladder
Epidemiology
- Found in ~26 - 54% of gallbladder specimens resected for cholelithiasis and chronic cholecystitis (J Clin Med Res 2014;6:26, Int J Clin Exp Pathol 2013;6:91)
- Age range: 18 - 93 years with a mean of ~50 - 60 years of age with a female predilection (Int J Clin Exp Pathol 2013;6:91, Beitr Pathol 1975;156:343)
- Commonly seen in populations with increased incidence of gallbladder carcinoma (India, Far East, Central / Eastern Europe, South America [especially Chile]) (Histopathology 2021;79:2, Mod Pathol 2011;24:147A)
Sites
- Gallbladder and biliary tree
Pathophysiology
- Epithelial damage and repair from a chronic inflammatory environment that promotes metaplastic transformation (Biochim Biophys Acta 2016;1865:245)
- Considered one of the initial steps in the development of gallbladder carcinoma through a metaplasia - dysplasia - carcinoma sequence (Am J Surg Pathol 2007;31:907)
- Similar molecular abnormalities are found in gallbladder carcinoma (Cancer Res 1995;55:2511)
Etiology
- Limited studies focus on metaplasia alone but it is assumed to occur in association with gallbladder carcinoma with similar risk factors
- Chronic inflammation of mucosa, most commonly from cholelithiasis but can also result from inflammatory conditions including primary sclerosing cholangitis (Histopathology 2021;79:2, Hum Pathol 1986;17:614, Am J Surg Pathol 2007;31:907)
- Intestinal metaplasia commonly found in gallbladders with dysplasia and early adenocarcinoma (50%) (Mod Pathol 2011;24:147A)
- Gastric foveolar change / metaplasia more commonly seen in gallbladders from high risk areas for gallbladder cancer, including Chile (Mod Pathol 2019;32:27)
- Squamous metaplasia can be found in mucosa adjacent to squamous cell and adenosquamous carcinoma (Mod Pathol 2011;24:1069)
- Infectious agents including Salmonella species in synergistic chronic inflammation (Aliment Pharmacol Ther 2014;39:745)
- Increased frequency in cases of anomalous arrangement of the pancreaticobiliary duct (Biochim Biophys Acta 2016;1865:245, Am J Surg Pathol 2017;41:1167)
Clinical features
- Clinical presentation of symptomatic cholecystitis or cholelithiasis including right upper quadrant pain (Murphy sign), nausea, vomiting, flatulence, abdominal distention
Diagnosis
- Same methodologies to assess for cholecystitis and cholelithiasis including abdominal ultrasound, endoscopic ultrasound, computed tomography (CT) scan, hepatobiliary iminodiacetic acid (HIDA) scan
Prognostic factors
- Pyloric gland metaplasia is ubiquitous and innocuous (Histopathology 2021;79:2)
- Intestinal metaplasia and gastric foveolar metaplasia have closer associations with dysplasia and carcinoma (Histopathology 2021;79:2)
Case reports
- 7 year old boy with cholecystitis, cholelithiasis, fasciitis-like proliferation and osseous metaplasia (Pediatr Dev Pathol 2011;14:80)
- 26 year old man with ectopic gastric mucosa in the gallbladder (Turk J Gastroenterol 2002;13:172)
- 51 year old woman with gallbladder mucocele and associated intestinal metaplasia (Int J Surg Case Rep 2024;116:109405)
- 56 year old woman with pseudoepidermoid cyst arising in chronic cholecystitis with exuberant squamous metaplasia (Arch Pathol Lab Med 2005;129:e138)
Treatment
- No specific treatment for metaplasia as it is usually an incidental finding
- Cholecystectomy, if patient is symptomatic from cholecystitis and cholelithiasis
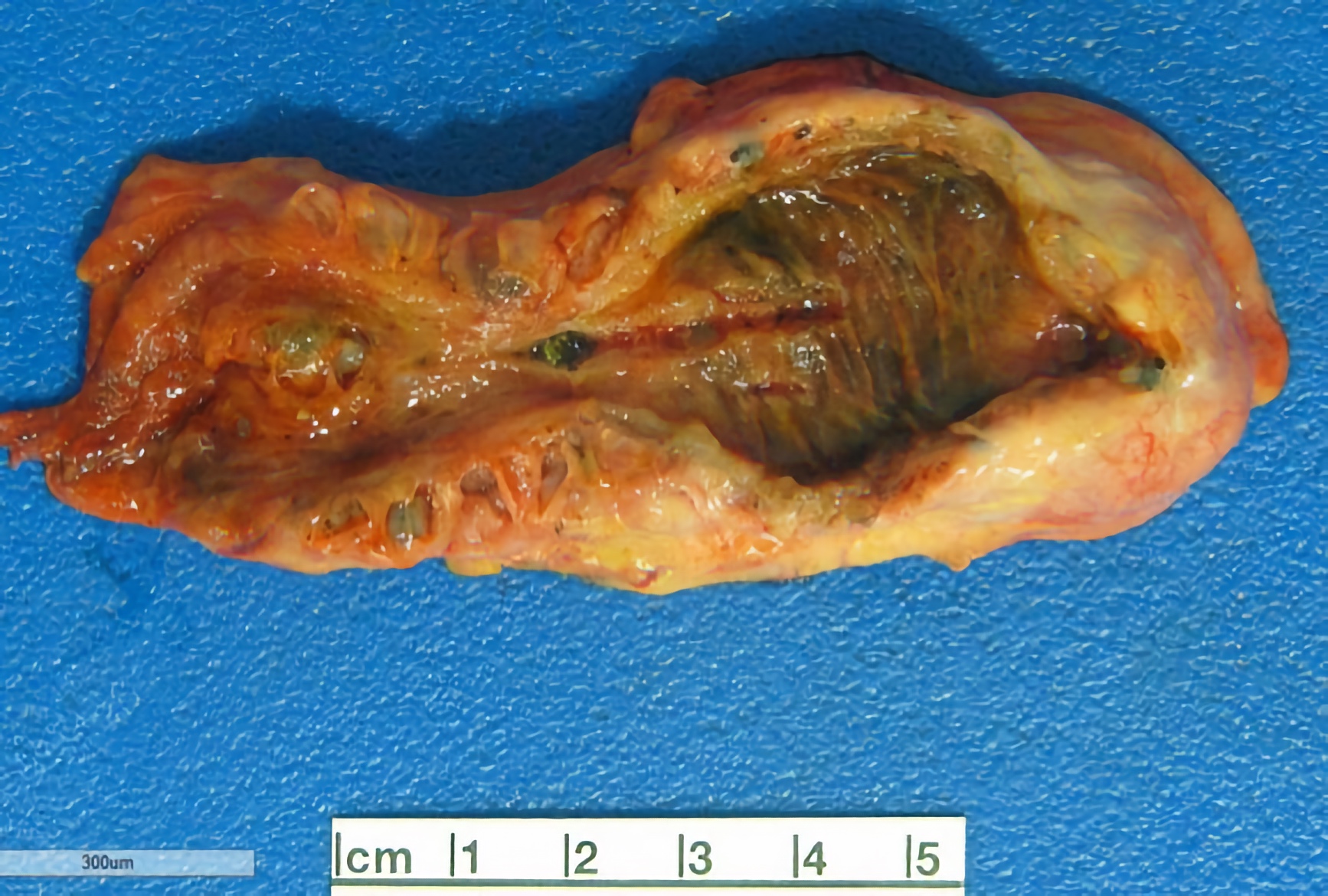
Gross description
- Gallbladder may display thickened wall with hemorrhagic, ulcerated, granular mucosa
- Sampling recommendations for metaplasia identified after initial sections
- Pseudopyloric / pyloric gland metaplasia < 3 mm
- No additional sections
- If > 3 mm, recheck specimen container and submit any detached polypoid fragments to rule out an adenomatous or mass forming preinvasive lesion (Am J Clin Pathol 2013;140:278)
- Intestinal or foveolar metaplasia
- Most studies do not recommend additional sampling (Am J Surg Pathol 2019;43:1668)
- Others recommend submitting a limited number of additional cassettes due to the association with dysplasia / carcinoma (Mod Pathol 2011;24:147A, Am J Clin Pathol 2013;140:278)
- Pseudopyloric / pyloric gland metaplasia < 3 mm
Gross images
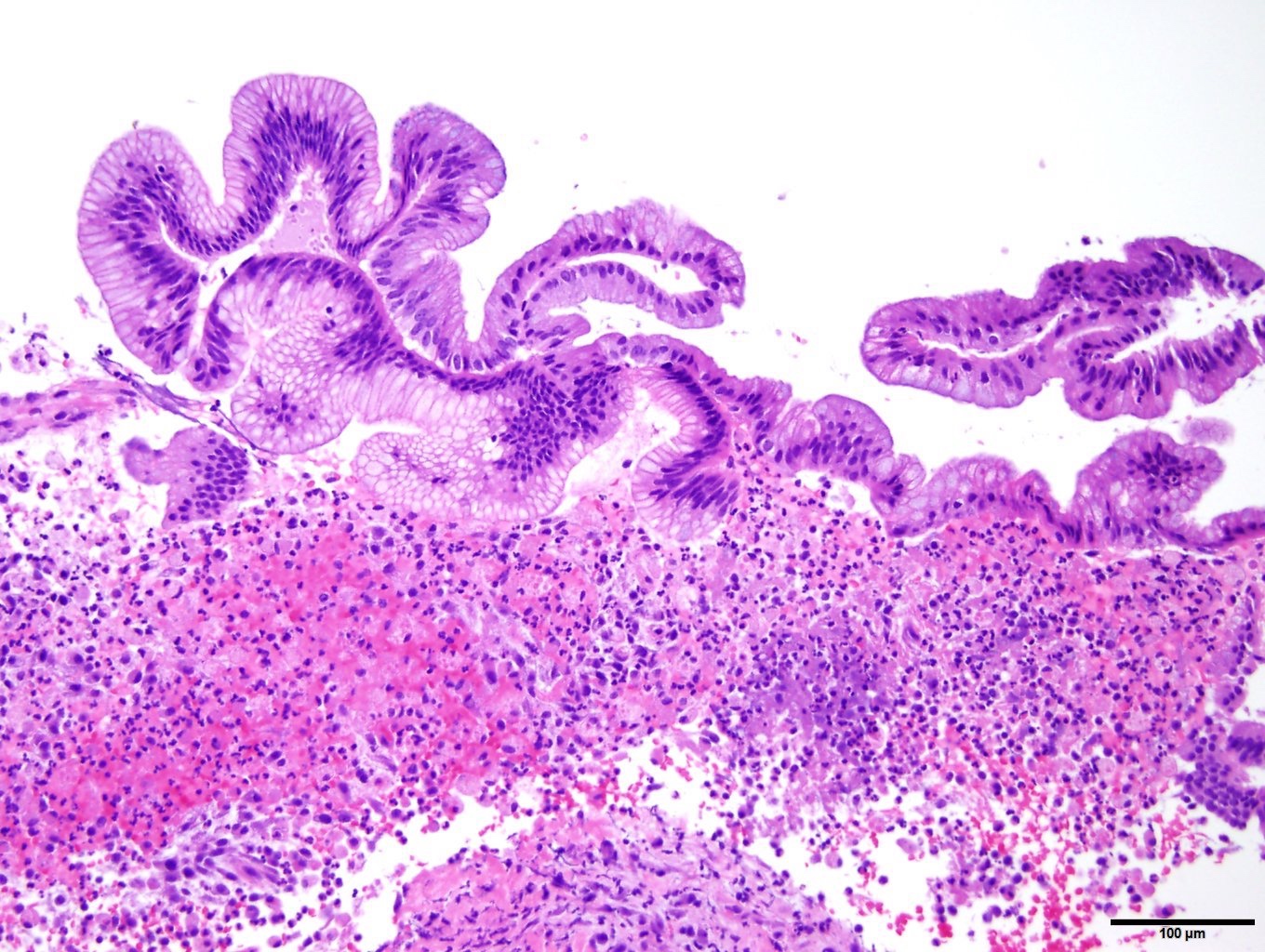
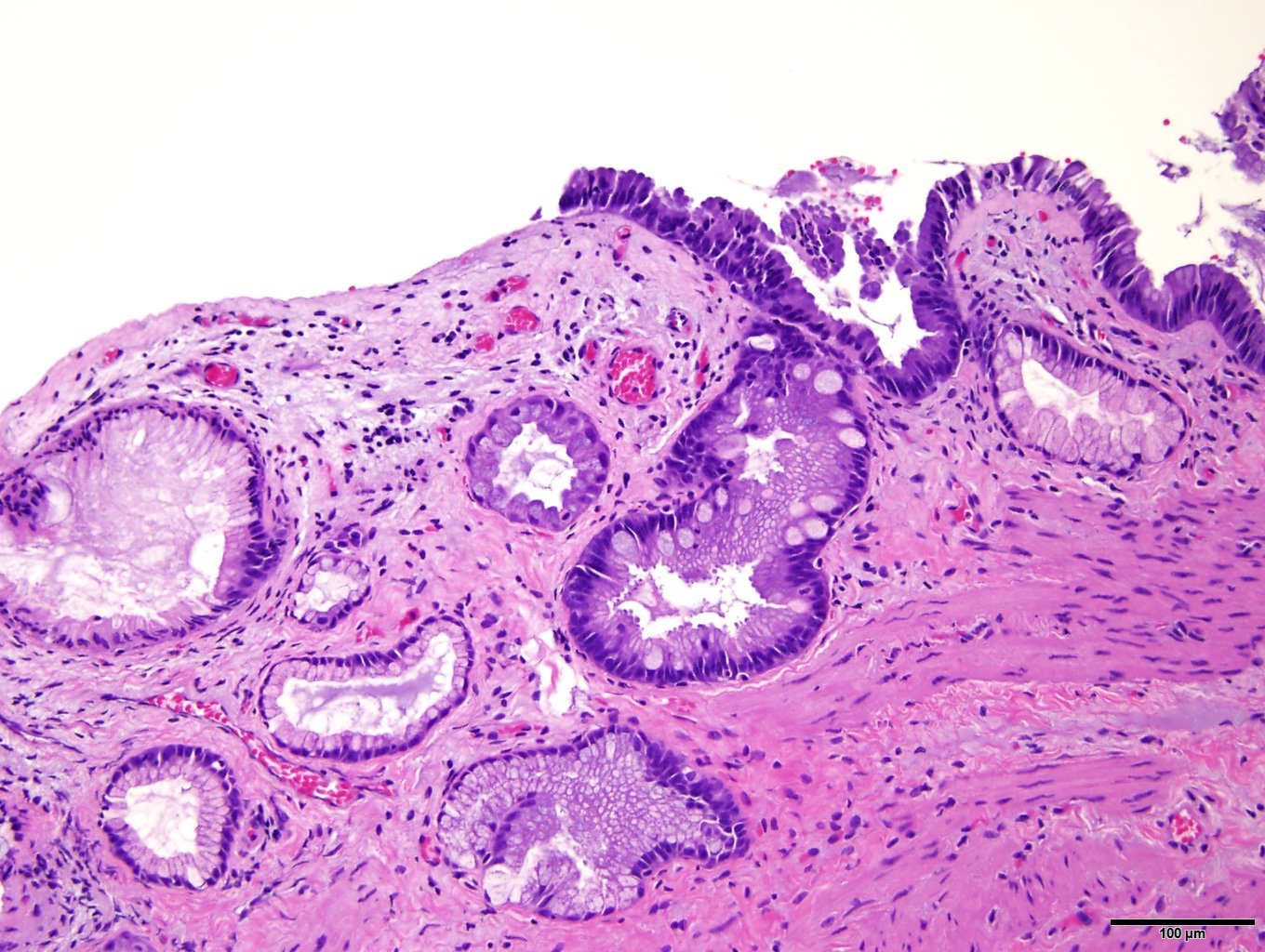
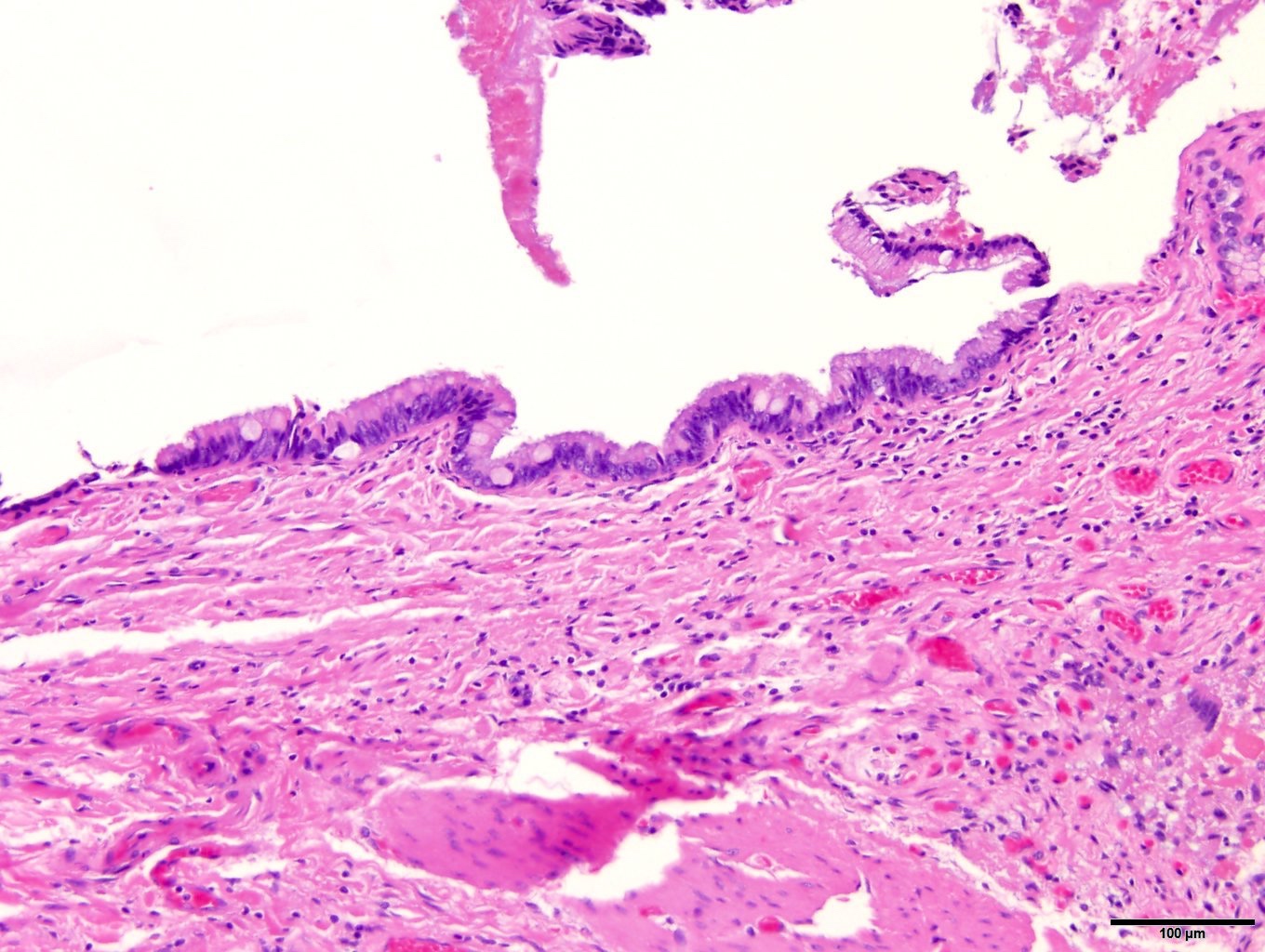
Microscopic (histologic) description
- Intestinal metaplasia
- Initially presents as a few goblet cells at the tip of mucosal folds and when fully developed Paneth cells, endocrine cells and columnar cells with a brush border (complete type) may be present, involving deeper glands within the lamina propria
- Formation of microvilli in developed cases (Beitr Pathol 1975;155:297)
- Typically admixed with glands lined by gastric foveolar epithelium and pyloric type glands
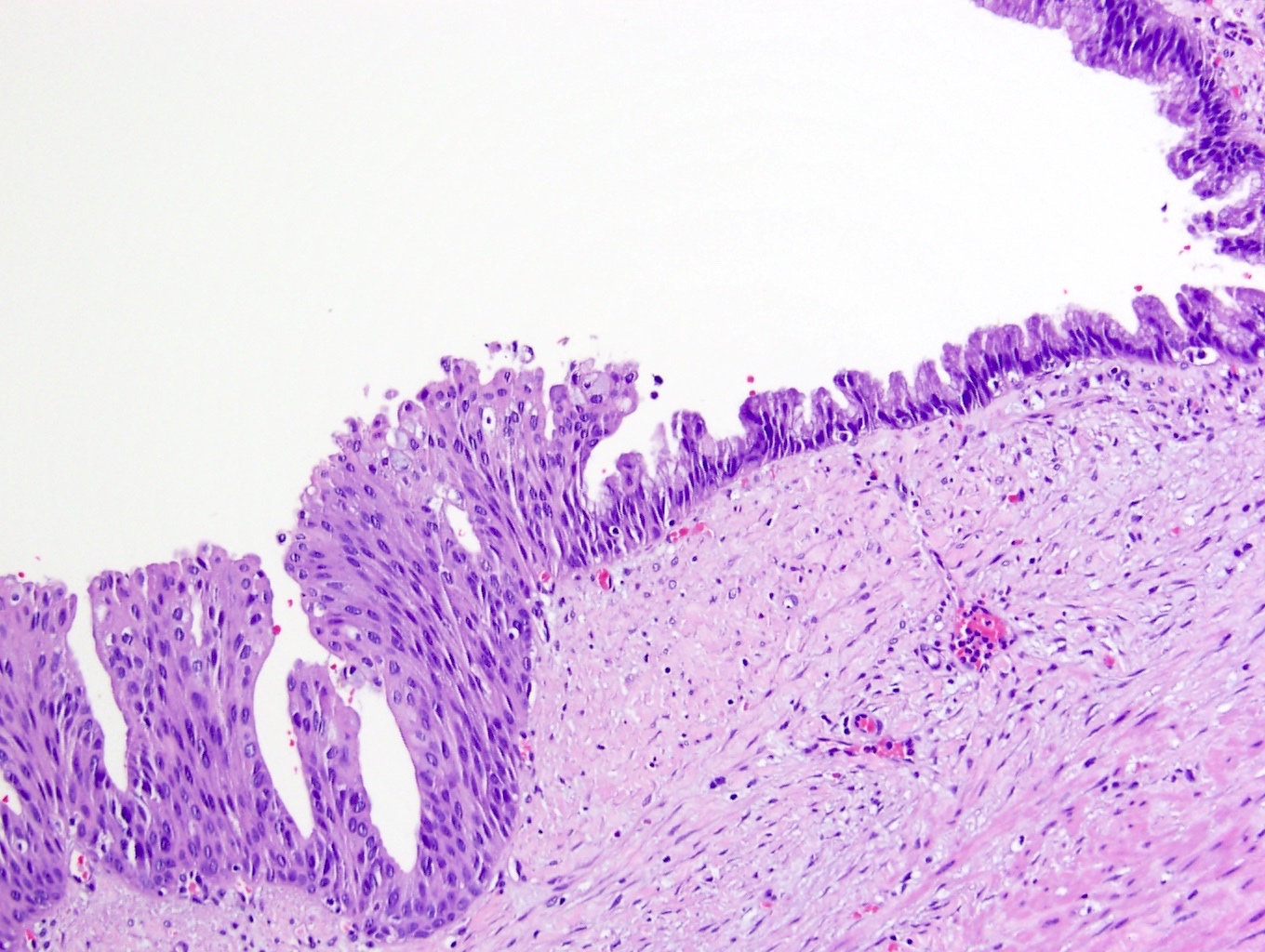
- Squamous metaplasia
- Replacement of columnar epithelium with mature, keratinized, stratified squamous epithelium
- Granular and keratin layer may be present
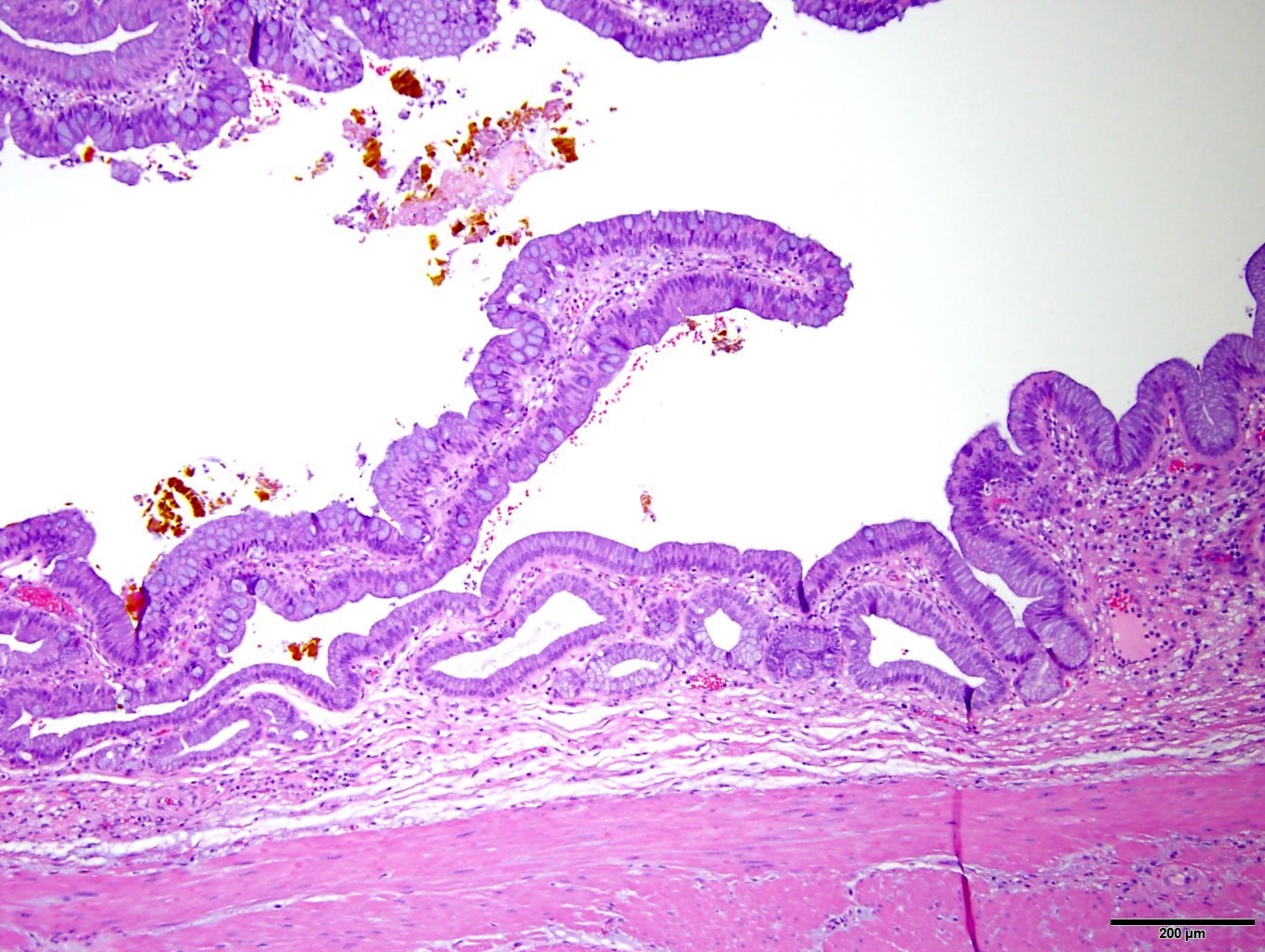
- Gastric metaplasia
- Pyloric gland / pseudopyloric gland metaplasia
- Cuboidal to low columnar mucinous epithelium resembling pyloric or Brunner gland epithelium with basal nuclei
- Endocrine and Paneth cells may be found between the mucin containing cells
- Small, mostly subsurface gland units arranged as lobules or displaying a diffuse growth pattern
- Often microscopically polypoid or nodular
- Florid lesions may extend deep through the muscular wall to the serosal surface and show perineural invasion (Cancer 1999;86:2625)
- Foveolar
- Voluminous, mucinous epithelium resembling gastric foveolar type
- Surface predominant changes
- May have acidophilic goblet-like cells (Histopathology 2021;79:2)
- Pyloric gland / pseudopyloric gland metaplasia
Microscopic (histologic) images
Positive stains
- Squamous metaplasia
- Intestinal metaplasia
- CDX2, MUC2, CK20 immunoreactive (Hum Pathol 2007;38:66, Am J Surg Pathol 2012;36:1279)
- Gastric foveolar type metaplasia
- Pyloric gland metaplasia
Negative stains
- No p53 overexpression by IHC compared to dysplasia or carcinoma in situ (Hum Pathol 1996;27:360)
Sample pathology report
- Gallbladder, cholecystectomy:
- Chronic cholecystitis with focal intestinal metaplasia and cholelithiasis (see comment)
- Comment: Following histologic examination of the initial sections, 4 additional sections of gallbladder tissue were submitted for histologic examination. There is no evidence of dysplasia or carcinoma.
Differential diagnosis
- Dysplasia (BilIN):
- Often coexists with intestinal and foveolar metaplasia
- At least moderately increased N:C ratio and cytologic atypia
- Low grade dysplasia may mimic intestinal metaplasia
- Loss of cell polarity in high grade dysplasia (Mod Pathol 2007;20:701)
- Normal tubuloalveolar mucous glands:
- Glands composed of low columnar cells with abundant, clear to lightly basophilic cytoplasm and round, basally oriented nuclei
- Located in the neck of the gallbladder
- Gastric heterotopia:
- Full thickness involvement of gallbladder wall by gastric fundic type mucosa with glands containing parietal and chief cells and focal dilatation (Tunis Med 2011;89:935)
- More commonly found in the gallbladder neck (Arch Pathol Lab Med 1992;116:138)
- May have surrounding adaptive intestinal metaplasia
- Pancreatic heterotopia:
- Presence of normal pancreatic structures including acini, small ducts and islets of Langerhans
- Pyloric gland adenoma:
- > 1.0 cm, grossly mass forming neoplasm
- Well demarcated group of tightly packed, glands lined by columnar or cuboidal cells with hyperchromatic nuclei and mucin containing cytoplasm
- Contain overt cytological dysplasia (Am J Surg Pathol 2012;36:1279)
Additional references
Board review style question #1
Board review style answer #1
A. CDX2, CK20, MUC2 positive. The image provided demonstrates intestinal metaplasia, which will demonstrate immunoreactivity for CK20, MUC2 and CK20. Answer B is incorrect because MUC5AC positivity is typically demonstrated in gastric foveolar metaplasia. Answer C is incorrect because MUC6 positivity is demonstrated in pyloric gland metaplasia. Answer D is incorrect because while intestinal metaplasia does exhibit MUC2 immunoreactivity, it is not the only marker of the listed choices that is positive.
Comment Here
Reference: Metaplasia
Comment Here
Reference: Metaplasia
Board review style question #2
Board review style answer #2
D. Women 40 - 50 years of age. It is thought that metaplastic changes occur as a result of chronic inflammation of the gallbladder mucosa secondary to chronic cholecystitis or cholelithiasis. Women of ~40 years of age are more likely to develop gallstones, resulting in epithelial metaplastic changes. Answer A is incorrect because inflammatory conditions of the gallbladder and gallstones are not typically seen in the pediatric population. Answers B and C are incorrect because cholecystitis is typically not regarded as a condition of younger people and is more likely to develop in older individuals.
Comment Here
Reference: Metaplasia
Comment Here
Reference: Metaplasia