Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Askan G, Basturk O. Intracholecystic papillary neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladderipn.html. Accessed April 1st, 2025.
Definition / general
- Grossly visible, mass forming, noninvasive epithelial neoplasm arising in the mucosa and projecting into the lumen of the gallbladder (Am J Surg Pathol 2012;36:1279, HPB (Oxford) 2015;17:811)
- First described in 2012 by Adsay et al. (Am J Surg Pathol 2012;36:1279)
- 2019 WHO recognizes as a distinct type of preinvasive neoplasm of gallbladder under the name of intracholecystic papillary neoplasm (ICPN)
- Exhibits many similarities to pancreatic intraductal papillary mucosal neoplasms as they demonstrate a spectrum of variable configurations, different cell lineages (often in a mixture) and dysplastic changes as well
- Seen in < 1% of all cholecystectomies (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Int J Surg Pathol 2016;24:504, Best Pract Res Clin Gastroenterol 2013;27:285)
Essential features
- Usually measures ≥ 1 cm in diameter
- Microscopically reveals papillary, tubular or tubulopapillary growth patterns
- 4 morphologic patterns (biliary, intestinal, gastric and oncocytic) are described
- May be associated with an invasive carcinoma
- Has relatively favorable overall outcome even if it is associated with an invasive carcinoma (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Mol Clin Oncol 2019;11:488)
Terminology
- Older terms (not recommended) are biliary adenoma, papillary adenoma, tubulopapillary adenoma, intracystic papillary neoplasm, intracholecystic papillary tubular neoplasm or papillary carcinoma
ICD coding
Epidemiology
- Mean age is 61 (Am J Surg Pathol 2012;36:1279)
- F:M = 2:1 (Am J Surg Pathol 2012;36:1279)
- Seen in < 1% of all cholecystectomies (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88; Int J Surg Pathol 2016;24:504, Best Pract Res Clin Gastroenterol 2013;27:285)
Sites
- More common in the fundus and body of the gallbladder (Int J Surg Pathol 2016;24:504, Ann Diagn Pathol 2019;40:88)
Etiology
- No known etiologic factor
- No association with gallbladder stones
Clinical features
- Some are incidentally detected (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Abdom Radiol (NY) 2018;43:1535)
- Others present with right upper quadrant pain (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88)
Radiology description
- Characteristic imaging findings include contrast enhanced tumor on CT image and on MR cholangiopancreatography examination a tumor-like defect within the gallbladder with dilatation of the upstream bile duct (Clin J Gastroenterol 2019;12:197)
- Radiologically, half of them are misdiagnosed as gallbladder cancer (Am J Surg Pathol 2012;36:1279)
Prognostic factors
- Even ICPN associated invasive carcinomas are relatively indolent neoplasms with significantly better prognosis compared with conventional (pancreatobiliary type) gallbladder carcinomas (Am J Surg Pathol 2012;36:1279)
- Papillary configuration, biliary or foveolar phenotype and especially presence of high grade dysplasia are considered significant pathologic risk factors for associated invasive carcinoma (Am J Surg Pathol 2012;36:1279, Indian J Pathol Microbiol 2018;61:516)
Case reports
- 58 year old woman with jaundice (Intern Med 2014;53:2313)
- 58 year old woman with fever (Mol Clin Oncol 2019;11:488)
- 59 year old man with anorexia (Clin J Gastroenterol 2019;12:197)
- 64 year old man with upper abdominal pain (Surg Case Rep 2016;2:62)
- 70 year old man with elevated liver function tests (Surg Case Rep 2018;4:124)
Treatment
- Treated primarily by surgical resection
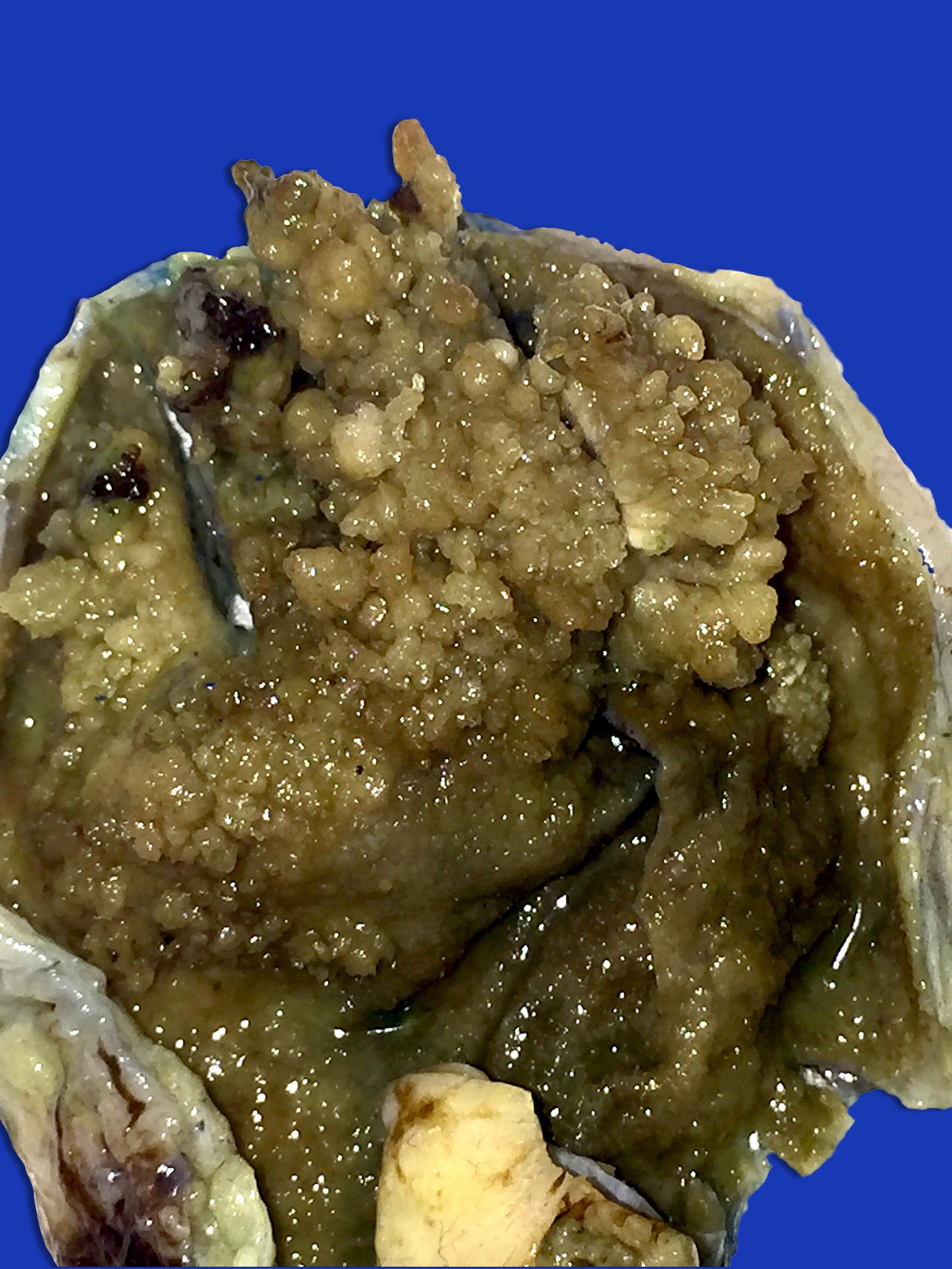
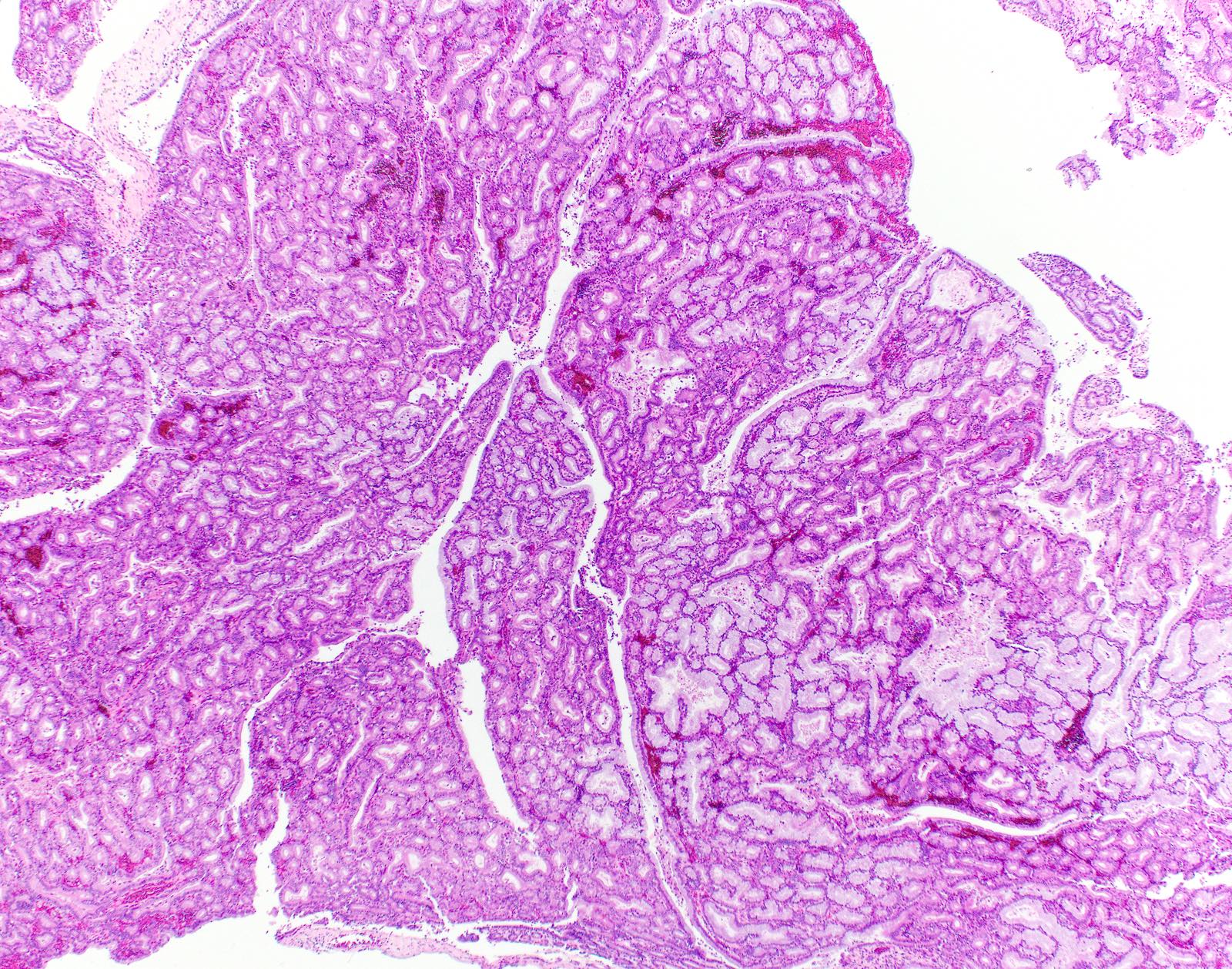
Gross description
- Prominent exophytic growth within the gallbladder or granular, friable soft tan excrescences
- Friable excrescences loosely attached to the lumen may be mistaken as sludge or debris in the lumen and not adequately sampled during initial macroscopic examination
- Median tumor size is 2.2 cm
- May be solitary or multifocal
- Reference: Am J Surg Pathol 2012;36:1279
Gross images
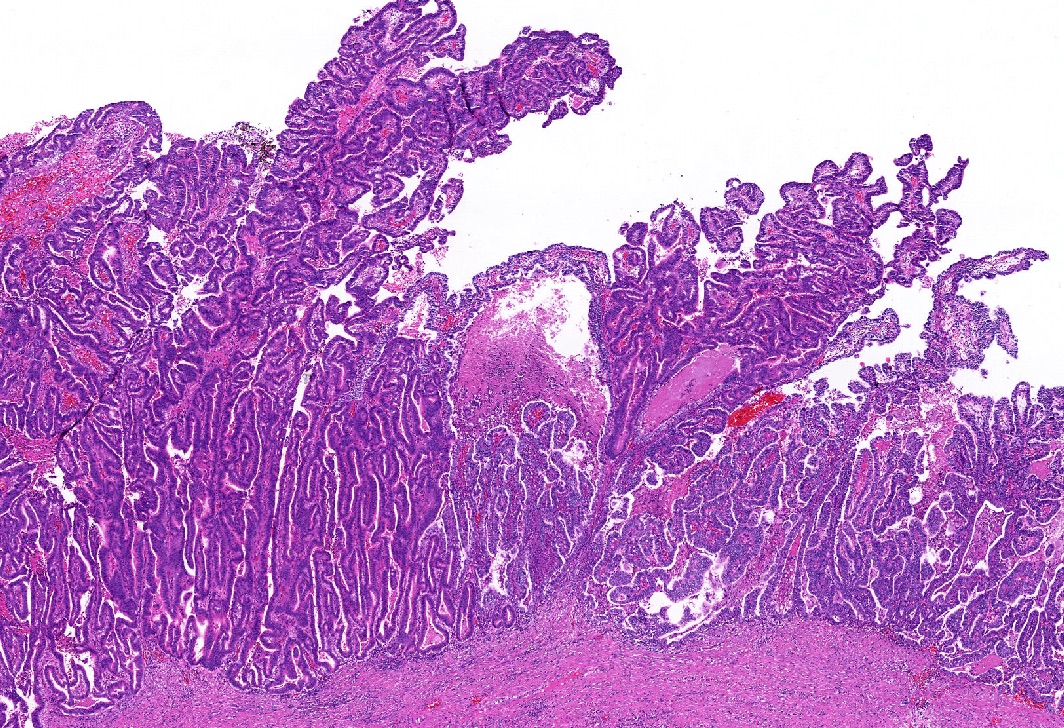
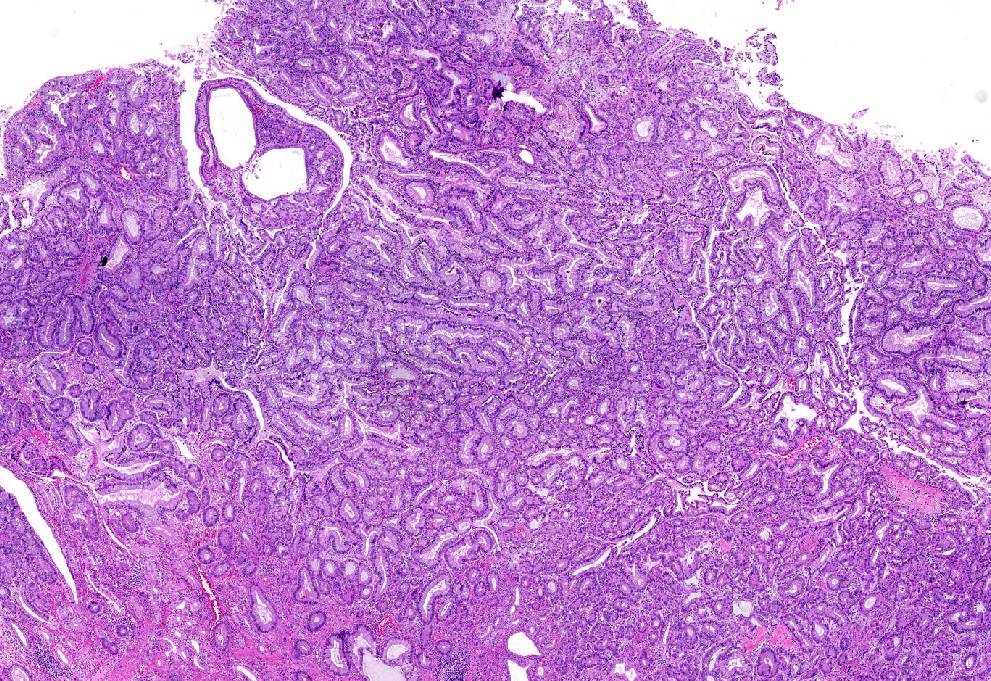
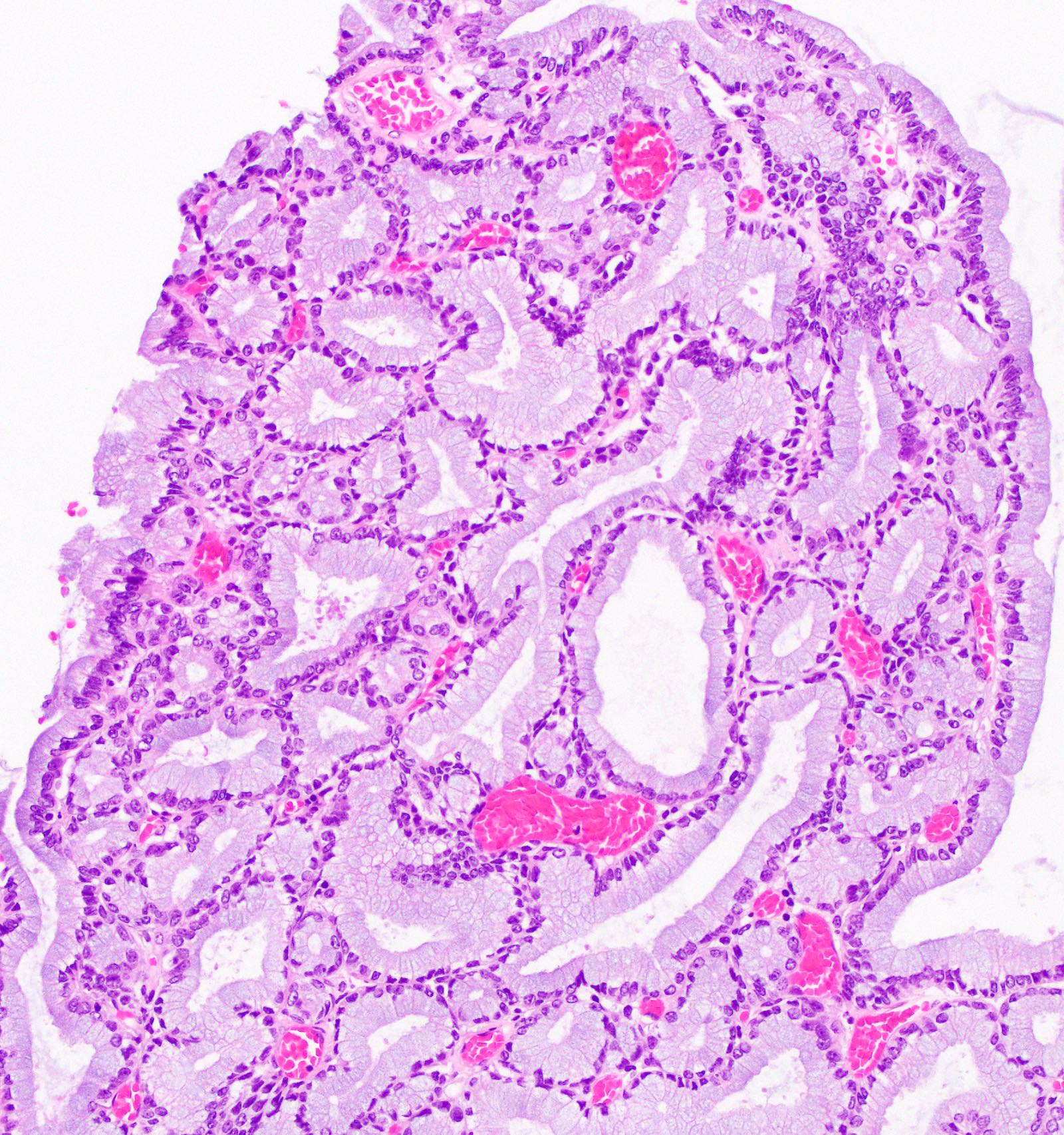
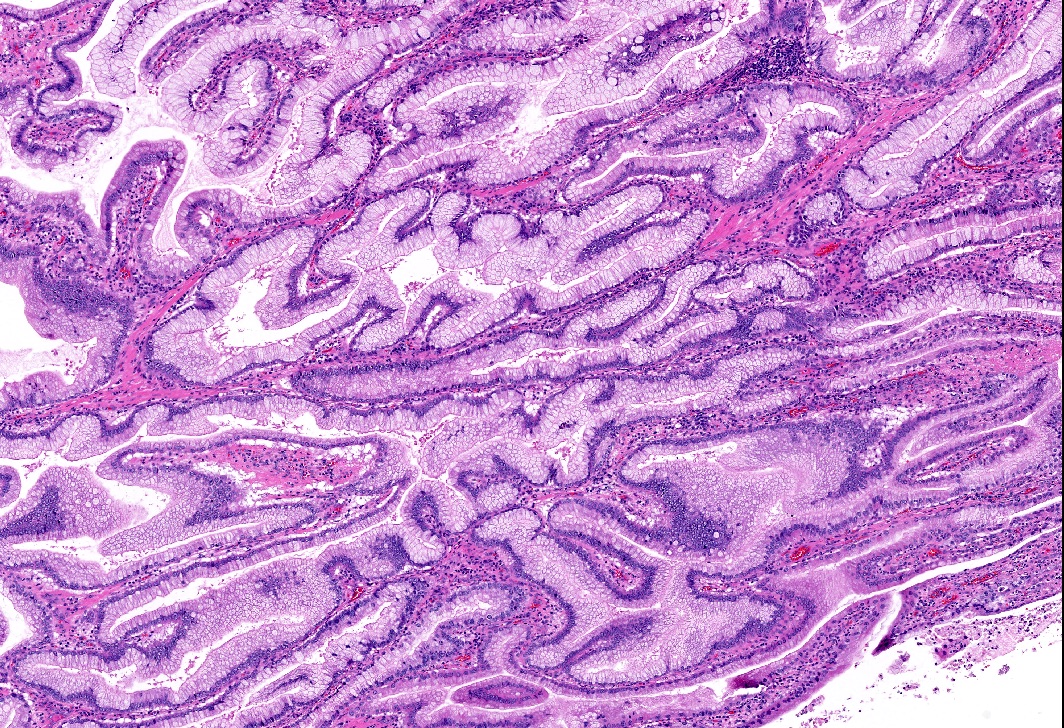
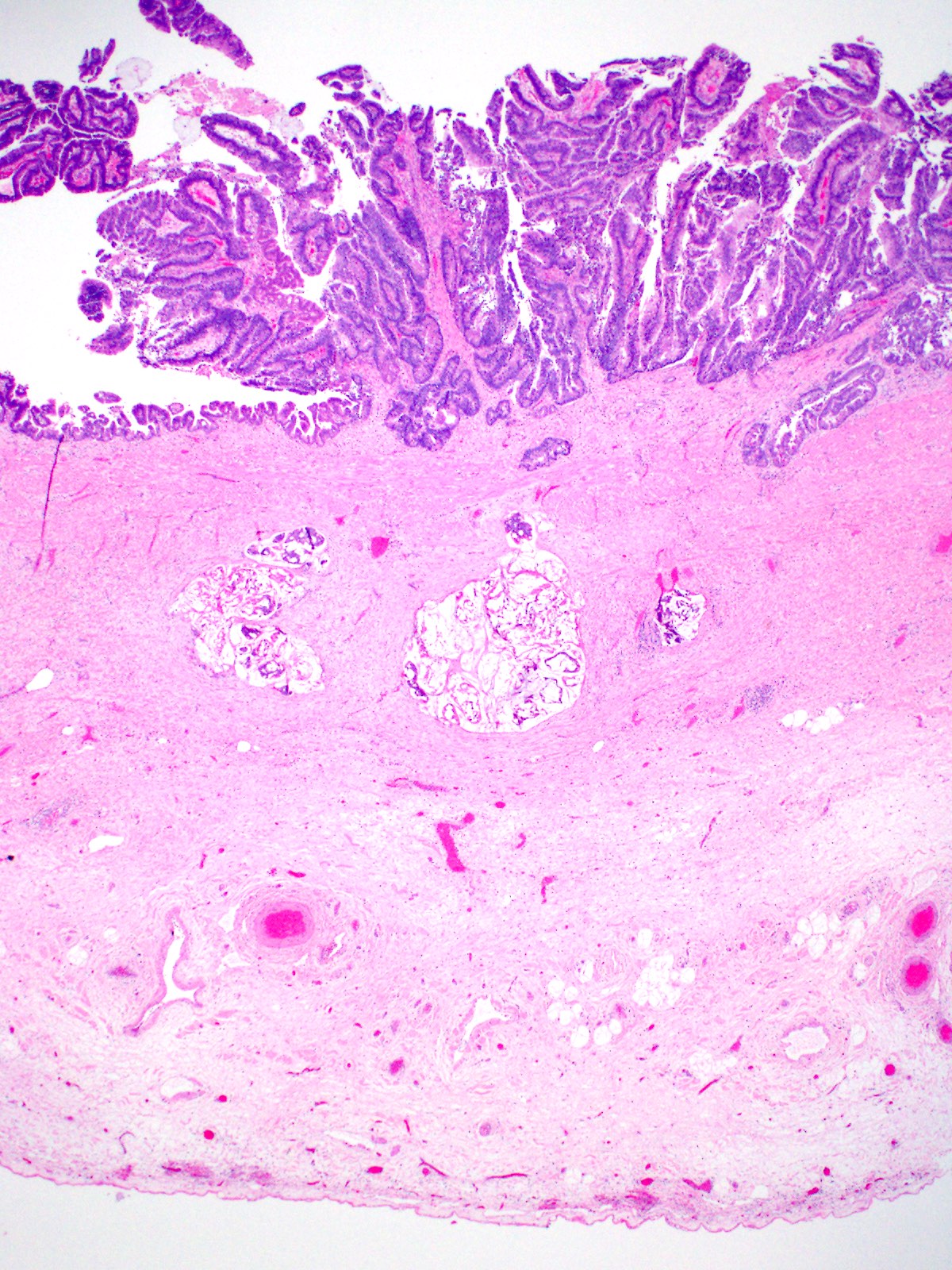
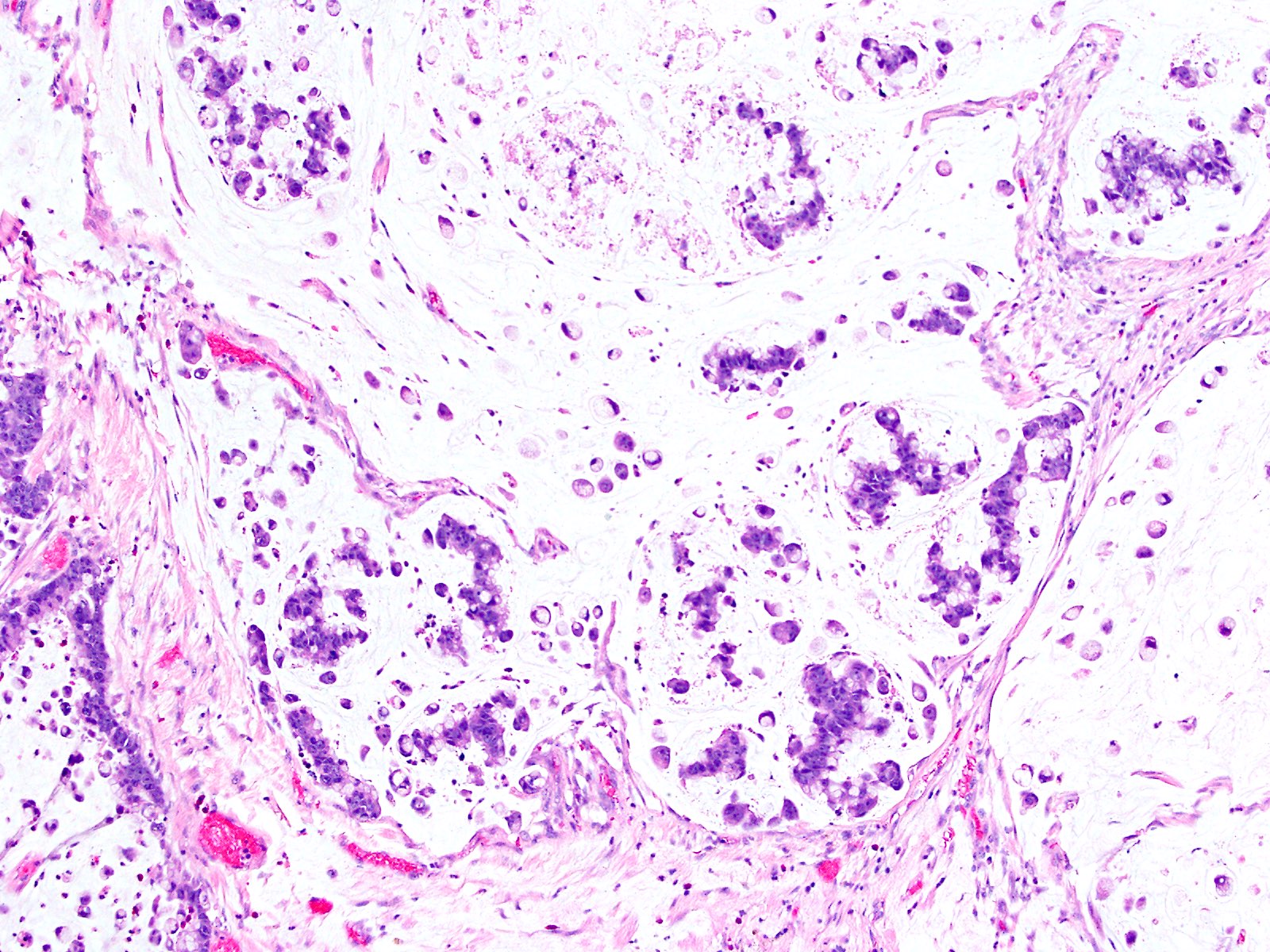
Microscopic (histologic) description
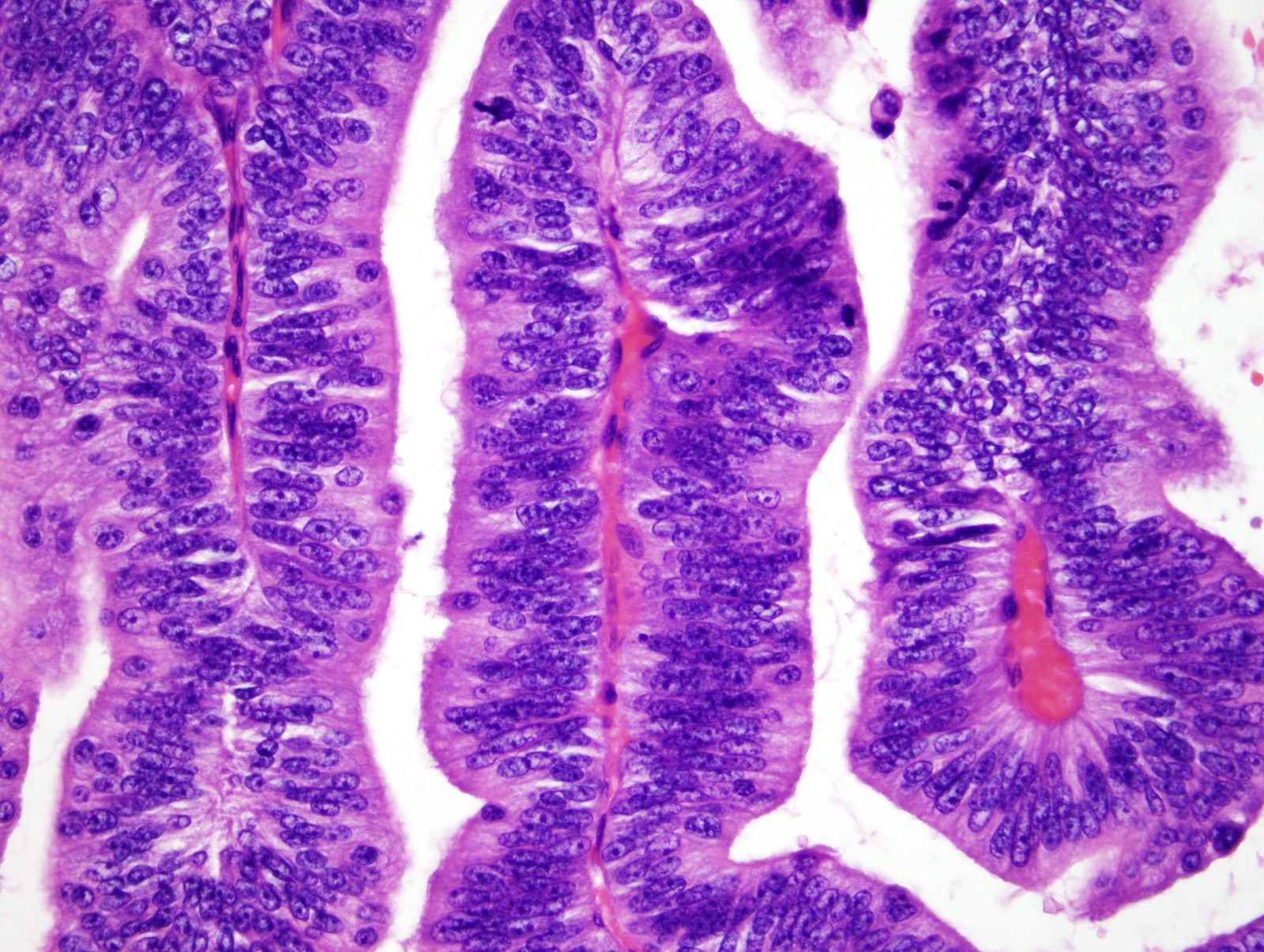
- Back to back epithelial units in papillary, tubular or tubulopapillary configuration with limited stroma (Am J Surg Pathol 2012;36:1279, Best Pract Res Clin Gastroenterol 2013;27:285)
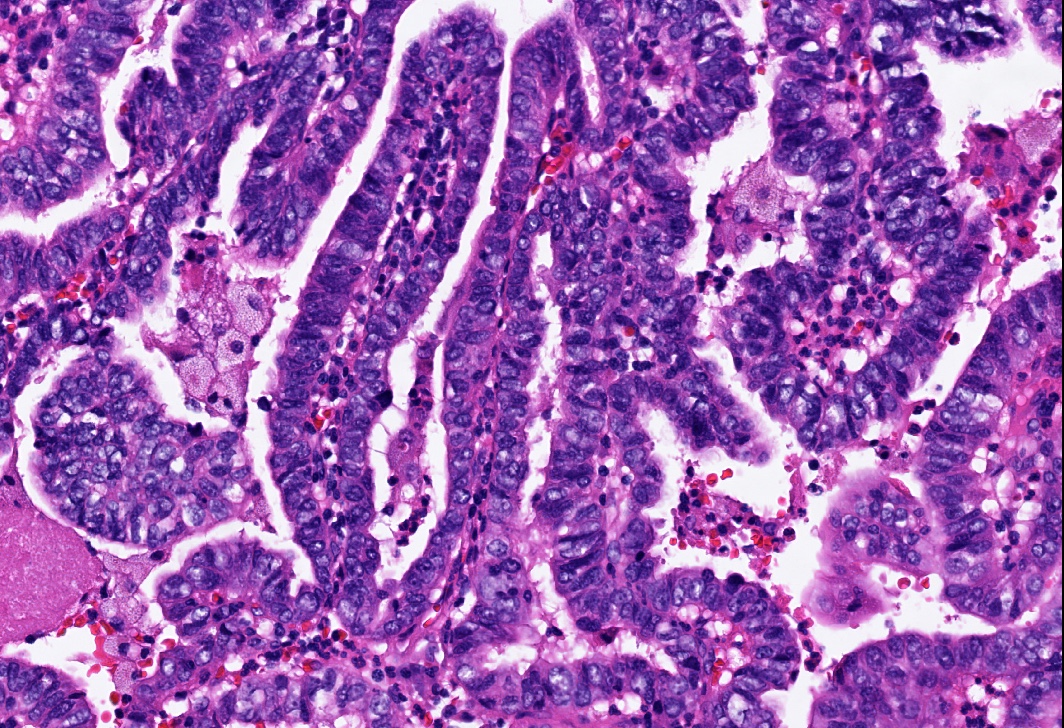
- 4 morphologic patterns are recognized (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57):
- Biliary phenotype: most common phenotype characterized by papillae lined by cuboidal cells with clear to eosinophilic cytoplasm and enlarged nuclei with distinct nucleoli; carries the highest risk for associated invasive carcinoma
- Gastric phenotype:
- Pyloric type:
- Intracholecystic neoplasms characterized by back to back mucinous glands with features characteristic of gastric pyloric glands were originally described as one of the subtypes of ICPN
- However, current (2019) WHO classifies these neoplasms as a distinct entity (i.e. pyloric gland adenoma)
- These carry the lowest risk for associated invasive carcinoma
- Foveolar type: large elongated glands lined by tall columnar mucinous epithelium with pale cytoplasm
- Pyloric type:
- Intestinal phenotype: morphologically similar to colonic adenoma showing pseudostratified cigar shaped nuclei and overall basophilia
- Oncocytic phenotype: least common subtype characterized by arborizing papillae that are lined by oncocytic cells (large, granular cytoplasm and prominent, large, eccentric nucleoli) with atypia
- 4 morphologic patterns are recognized (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57):
- Mixed phenotypes are common
- Lesions histologically characterized by abundant cytoplasm, small and uniform nuclei and distinct nucleoli are classified as low grade dysplasia; those with architectural complexity as well as nuclear atypia have high grade dysplasia (Am J Surg Pathol 2012;36:1279)
- For the noninvasive cases, it is important to assess the presence and amount of high grade dysplasia
- Associated invasive carcinoma is detected in more than half of the cases at the time of diagnosis, mostly in lesions with biliary phenotype and high grade dysplasia (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88)
- Associated invasive carcinoma is mostly pancreatobiliary type adenocarcinoma but other types of carcinomas, such as colloid or poorly differentiated neuroendocrine carcinoma, may also be seen (GE Port J Gastroenterol 2019;26:356, Surg Case Rep 2016;2:62)
- Invasive carcinoma may be grossly inapparent and may even occur away from the ICPN, therefore thorough sampling and careful microscopic evaluation are extremely important (Semin Diagn Pathol 2012;29:127)
Microscopic (histologic) images
Positive stains
Molecular / cytogenetics description
- KRAS mutation is common (Hum Pathol 1999;30:21, Appl Immunohistochem Mol Morphol 2011;19:133)
- STK11, CTNNB1 and APC mutations are identified (Am J Surg Pathol 2019;43:783)
- TP53 and GNAS mutations are rare
Sample pathology report
- Gallbladder, cholecystectomy:
- Intracholecystic papillary neoplasm of gallbladder (ICPN), biliary type, with extensive high grade dysplasia (> 75% of the tumor) (see comment)
- Comment: The gallbladder was submitted entirely for microscopic evaluation and no invasive carcinoma is identified. The ICPN measures 3.5 cm in greatest dimension. Cystic duct margin is free of ICPN.
- Gallbladder, cholecystectomy:
- Invasive adenocarcinoma, moderately differentiated, colloid type, arising in an intracholecystic papillary neoplasm (ICPN), intestinal type, with high grade dysplasia (see comment)
- Comment: The entire tumor is 5.3 cm in greatest dimension; the invasive carcinoma component is 1.5 cm in greatest dimension. The carcinoma invades through the muscularis layer (pT2). Cystic duct margin is free of invasive carcinoma but reveals high grade dysplasia.
Differential diagnosis
- Pyloric gland metaplasia:
- Not visible by gross examination or is smaller than 0.5 cm in greatest dimension
- Microscopically not well demarcated from surrounding mucosa
- Intracholecystic tubular nonmucinous neoplasms (ICTNs):
- Another type of preinvasive neoplasm of gallbladder, recently described by Pehlivanoglu et al. (Virchows Arch 2020 [Online ahead of print])
- Presents as a mass forming gallbladder neoplasm characterized by cauliflower-like architecture and is comprised of compact, back to back, small tubular units showing variable complexity
- Tubules are lined by low cuboidal, nonmucinous epithelium
- Nuclei are either round and have visible nucleoli or are more ovoid, overlapping and have optically clear chromatin, creating a picture highly reminiscent of papillary thyroid carcinoma
- Squamoid / meningothelial-like morules and neuroendocrine cell clusters are frequent
- Despite their cytoarchitectural complexity, they are not associated with invasive carcinoma
- Positive for MUC1 and MUC6 while negative for MUC2, CDX2 and MUC5AC
Board review style question #1
Which of the following is true about intracholecystic neoplasms of the gallbladder (ICPNs)?
- Jaundice is one of most common symptoms
- KRAS mutation is common
- Oncocytic phenotype is the most common subtype
- They are commonly seen in male patients
- They have a significantly worse prognosis compared with conventional gallbladder carcinomas
Board review style answer #1
Board review style question #2
Which one of the following stains is positive in intestinal phenotype of intracholecystic neoplasms (ICPNs) of the gallbladder?
- CK7
- MUC1
- MUC2
- MUC5AC
- MUC6
Board review style answer #2