Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Pehlivanoglu B, Adsay V. Intracholecystic tubular nonmucinous neoplasm (ICTN). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladderICTN.html. Accessed March 31st, 2025.
Definition / general
- Noninvasive epithelial neoplasm of the gallbladder that forms pedunculated polyps composed exclusively of small, nonmucinous tubules, often with squamoid morules (Virchows Arch 2021;478:435)
- Despite the cytoarchitectural complexity that warrants high grade dysplasia diagnosis, almost never associated with invasion (Virchows Arch 2021;478:435)
Essential features
- Pedunculated, typically solitary polyps with cauliflower architecture composed of lobules of back to back small acinar-like tubular units; possible association with cholesterol polyps
- Morules are common but can be subtle; they can be highlighted by beta catenin nuclear labeling
- Usually no dysplasia in the background gallbladder, uninvolved gallbladder is typically devoid of inflammation or chronic changes
- Virtually no association with invasive carcinoma (unlike other preinvasive neoplasia of the gallbladder) (Virchows Arch 2021;478:435)
- Does not appear to have field effect risk for biliary tract
Terminology
- Previously regarded as complex pyloric nonmucinous type of intracholecystic papillary tubular neoplasms (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Mod Pathol 2014;27:446A)
- Considered as a type of pyloric gland adenoma by some authors, along with pure and possibly hybrid (with both mucinous and nonmucinous components) pyloric gland adenomas (Am J Surg Pathol 2018;42:1237, Appl Immunohistochem Mol Morphol 2020;28:57, Virchows Arch 2008;453:521)
- Not defined as a distinct entity in WHO 2019; mentioned as intracholecystic papillary neoplasm showing gastric pyloric, nonmucinous morphology or presumably included in pyloric gland adenoma category
- Use of older terms, such as biliary adenoma, tubulopapillary adenoma or papillary carcinoma is not recommended
ICD coding
- No specific ICD code present; can be regarded under adenoma or intracholecystic papillary neoplasms
- ICD-O: 8503/2 - intracystic papillary neoplasm with high grade intraepithelial neoplasia
Epidemiology
- Mean age = 51 (Virchows Arch 2021;478:435)
- F:M = 0.9:1 (Virchows Arch 2021;478:435)
- Detected in < 1% of cholecystectomies (Ann Diagn Pathol 2019;40:88, Am J Surg Pathol 2012;36:1279)
Sites
- Specific to gallbladder; neoplasms with some similarities occur in the pancreatobiliary tract and are called intraductal tubulopapillary neoplasms (Mod Pathol 2015;28:1249, Am J Surg Pathol 2017;41:313)
Pathophysiology
- Considering the WNT / beta catenin alterations along with the common presence of morules, may be regarded as a part of the so called BROCN family tumors (morule forming with biotin rich optically clear nuclei, namely fetal type pulmonary adenocarcinoma, pancreatoblastoma, cribriform morular thyroid carcinomas and some endometrial adenocarcinomas) (Mod Pathol 2003;16:1124, Mod Pathol 2002;15:617, J Pathol 2001;194:59, Am J Pathol 2001;159:1619)
Etiology
- May be arising from cholesterol polyps (Virchows Arch 2021;478:435)
- No association with chronic cholecystitis or gallstones
Clinical features
- Discovered incidentally or may present with abdominal pain (Virchows Arch 2021;478:435)
Diagnosis
- Polyp identified on imaging studies; histology is confirmed after resection
Radiology description
- Features suggestive of a gallbladder polyp / mass or mimicking gallstones (Virchows Arch 2021;478:435)
Prognostic factors
- Excellent prognosis (Virchows Arch 2021;478:435)
- Hybrid lesions with both ICTN morphology and mucinous areas may be associated with invasive carcinoma (Am J Surg Pathol 2012;36:1279)
- Should be classified as intracholecystic papillary neoplasm
- Proper sampling to exclude associated lesions or invasive carcinoma is warranted regardless, although both are rare
Case reports
- 15 year old girl with recurrent right upper quadrant pain (J Pediatr Surg Case Rep 2017;25:46)
- 40 and 53 year old men presented with > 1 cm gallbladder polyps (J Gastrointest Oncol 2016;7:S81)
- 44 year old man with a polyp in the gallbladder (Gastroenterology 2011;141:e3)
- 61 year old woman with a pedunculated polyp in the gallbladder (Pathol Res Pract 1996;192:963)
Treatment
- Simple cholecystectomy is deemed adequate for this tumor, follow up may be appropriate (Virchows Arch 2021;478:435, Am J Surg Pathol 2012;36:1279)
- Radical cholecystectomy is not indicated (Virchows Arch 2021;478:435)
Gross description
- Most observed as detached intraluminal nodules or hemorrhagic debris / fibrin
- Typically present as pedunculated polyps with thin stalks
- Cauliflower architecture resembling cholesterol polyps
- Reference: Virchows Arch 2021;478:435
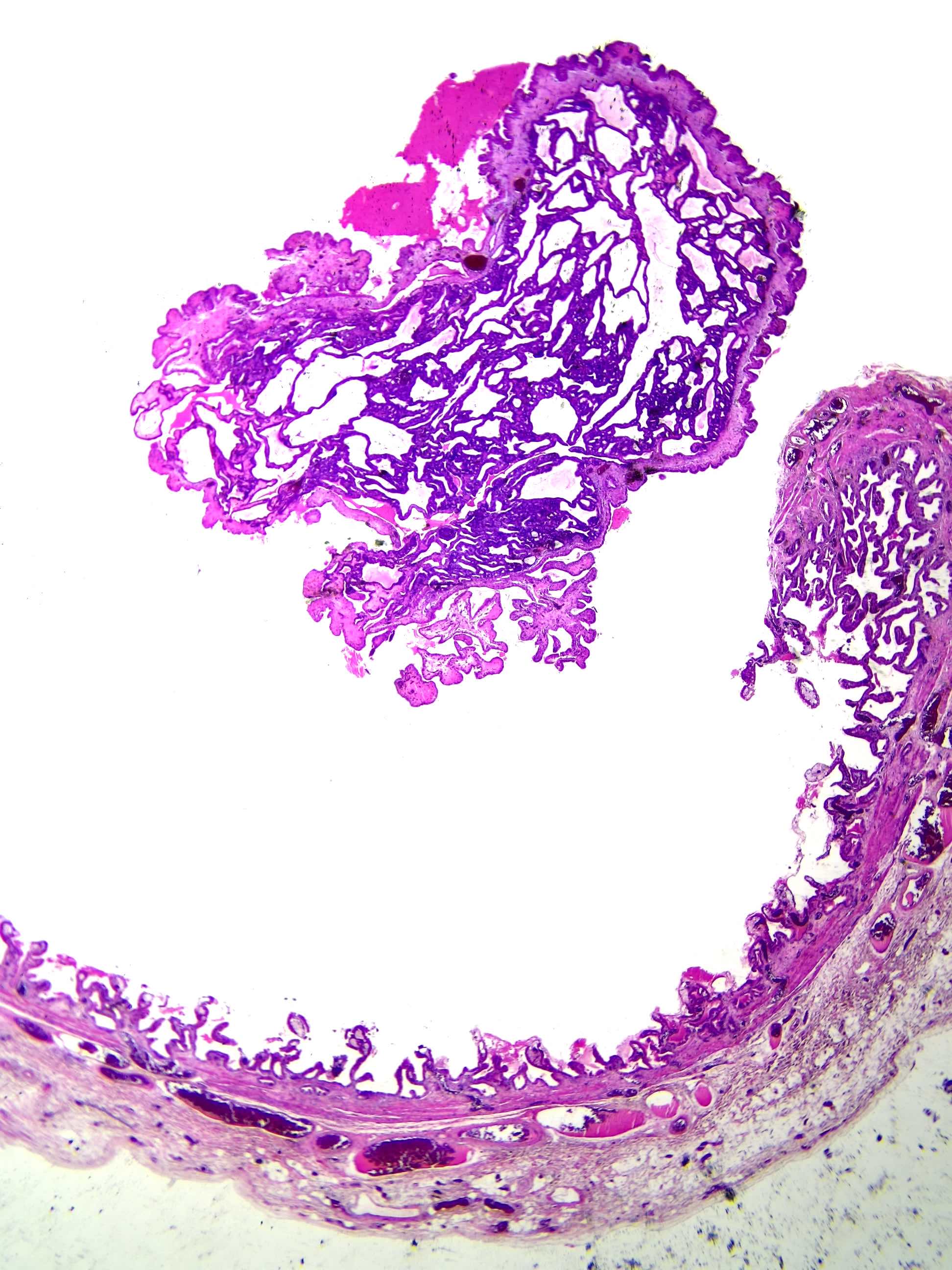
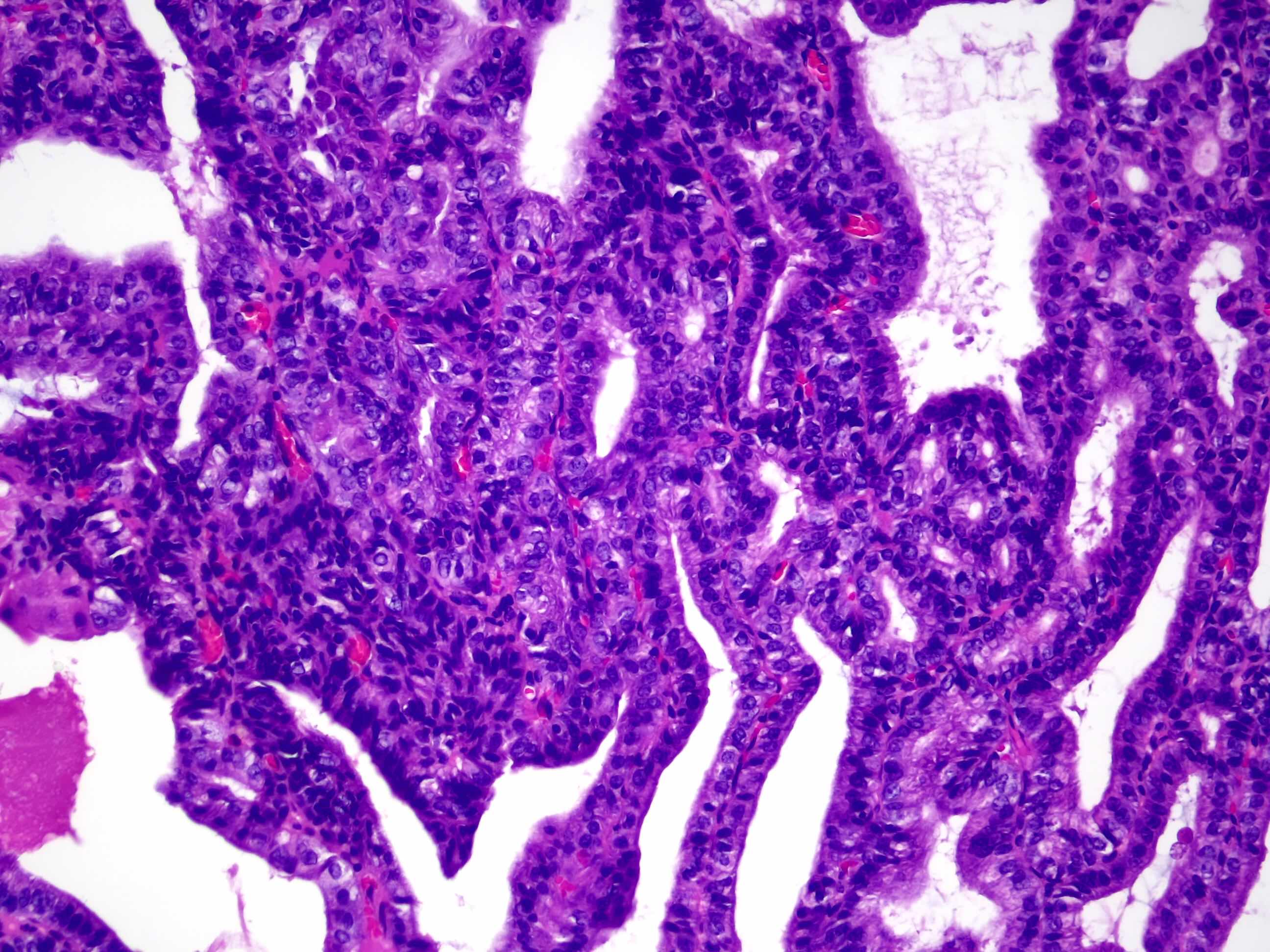
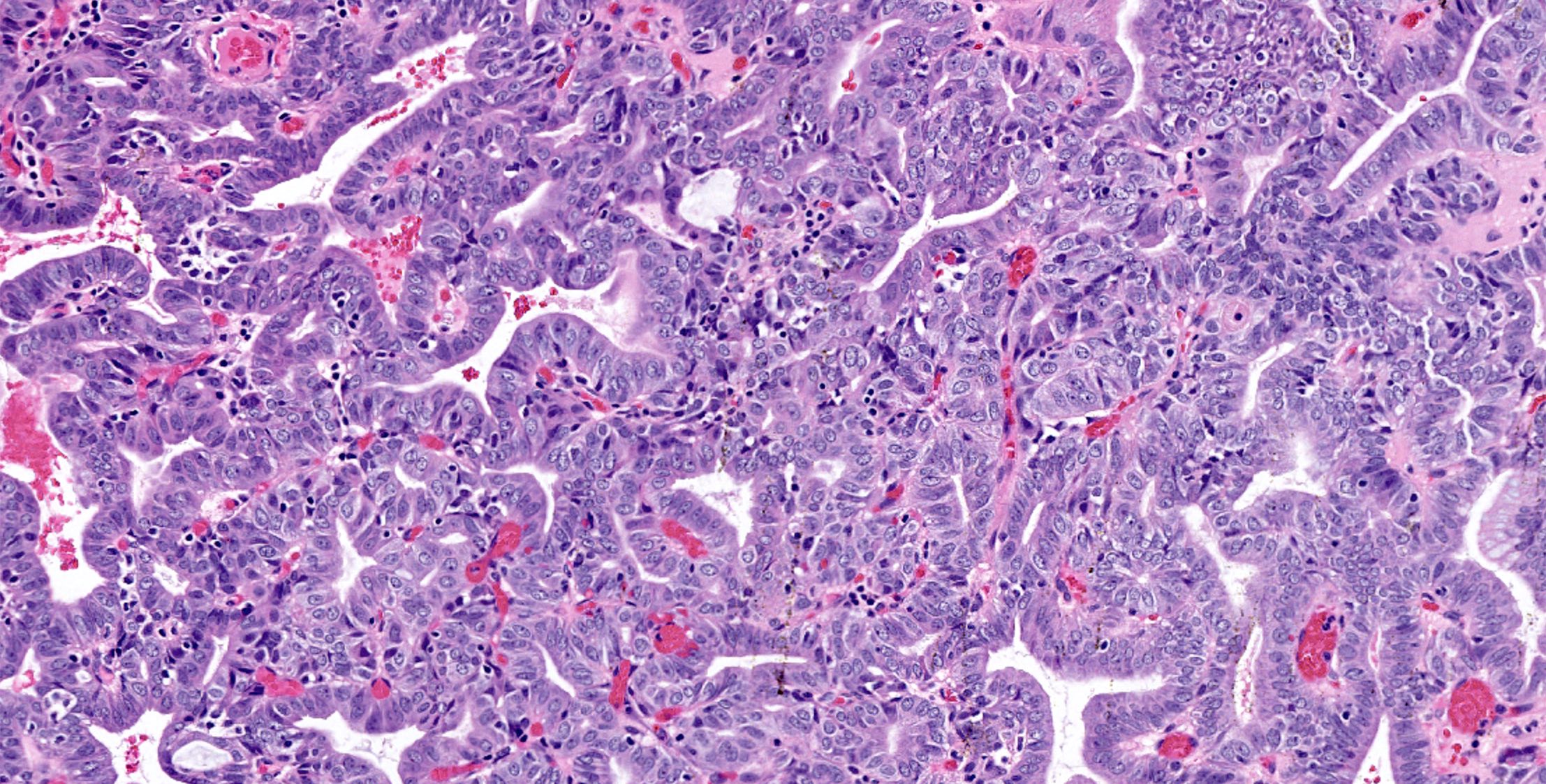
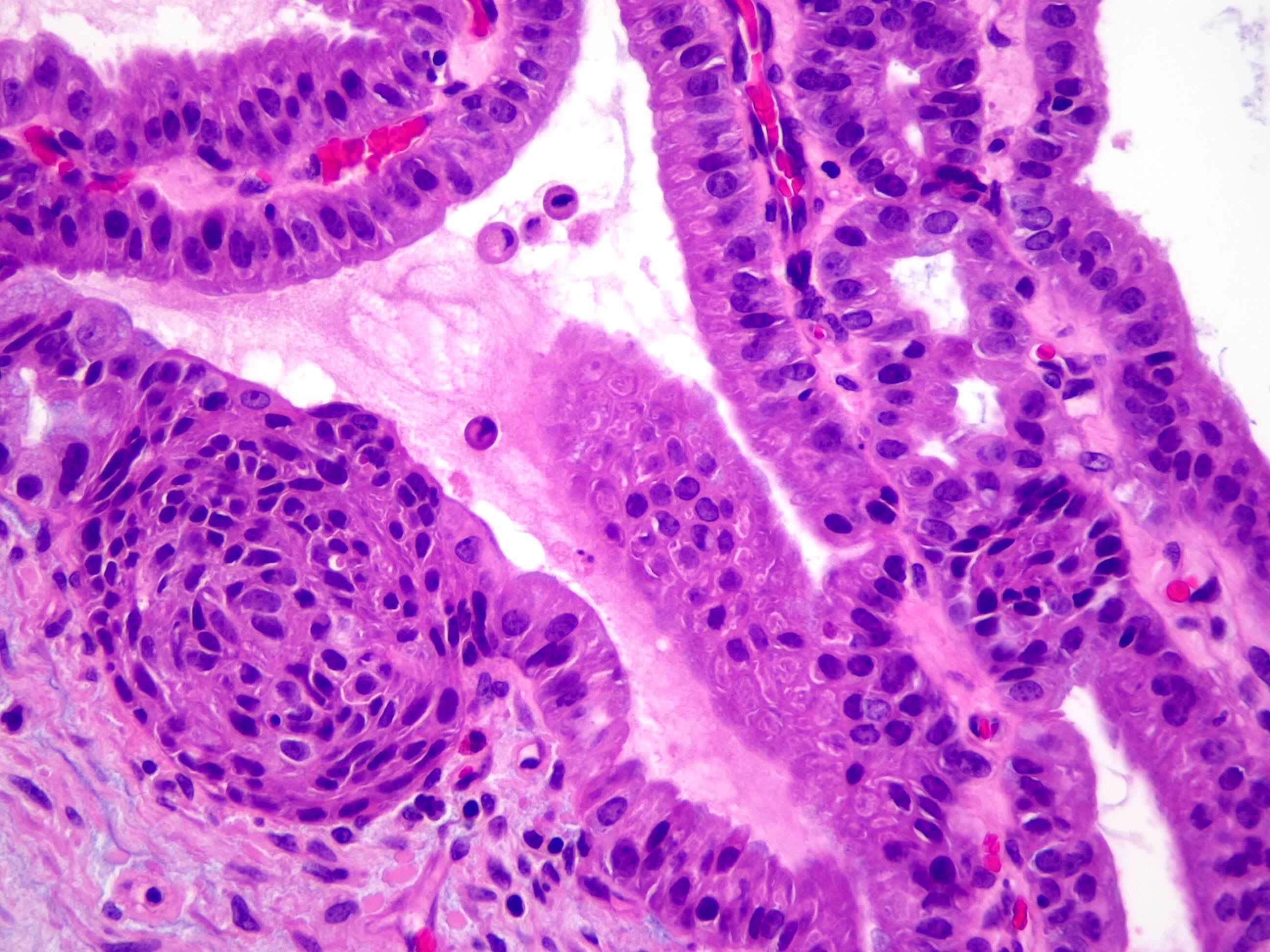
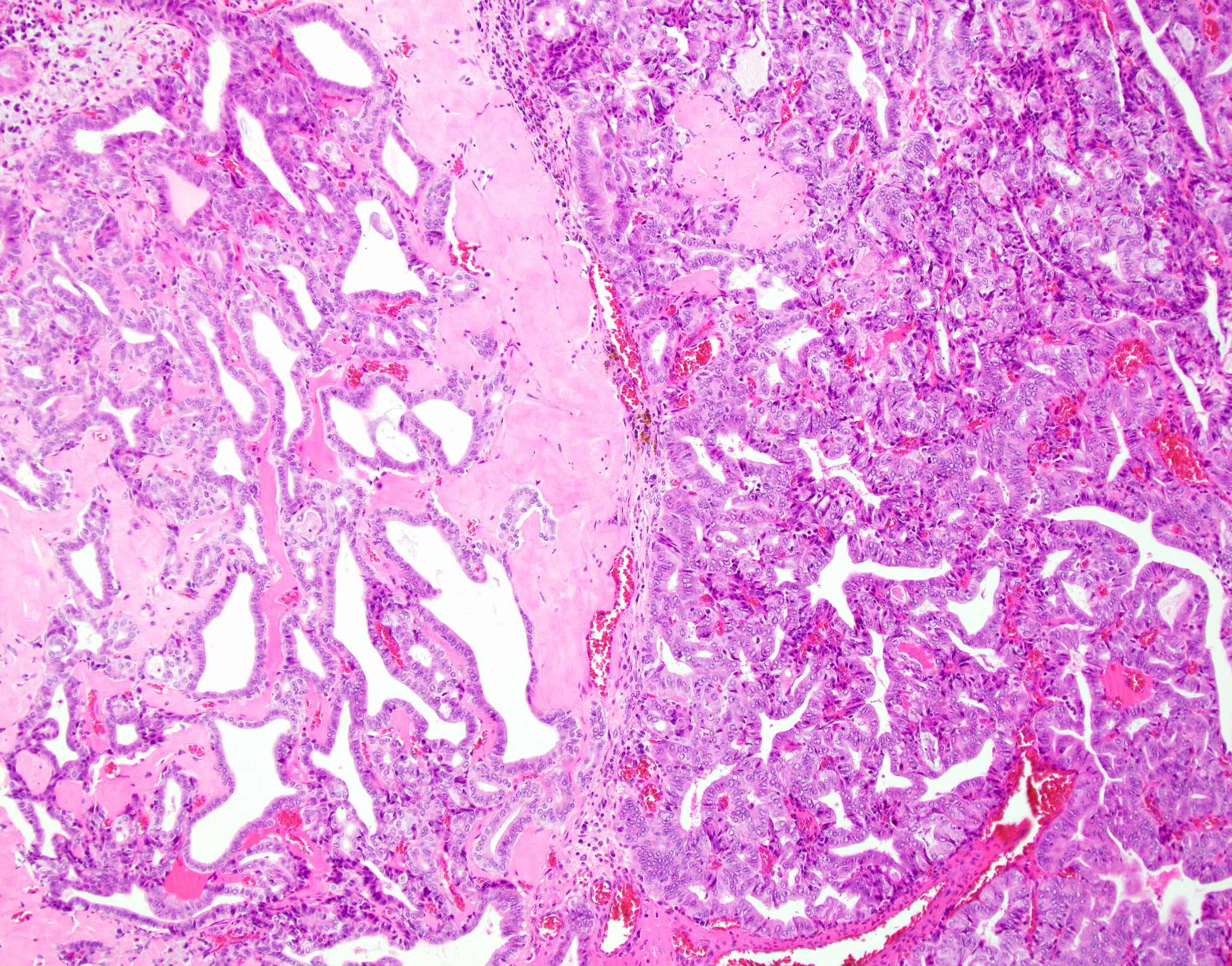
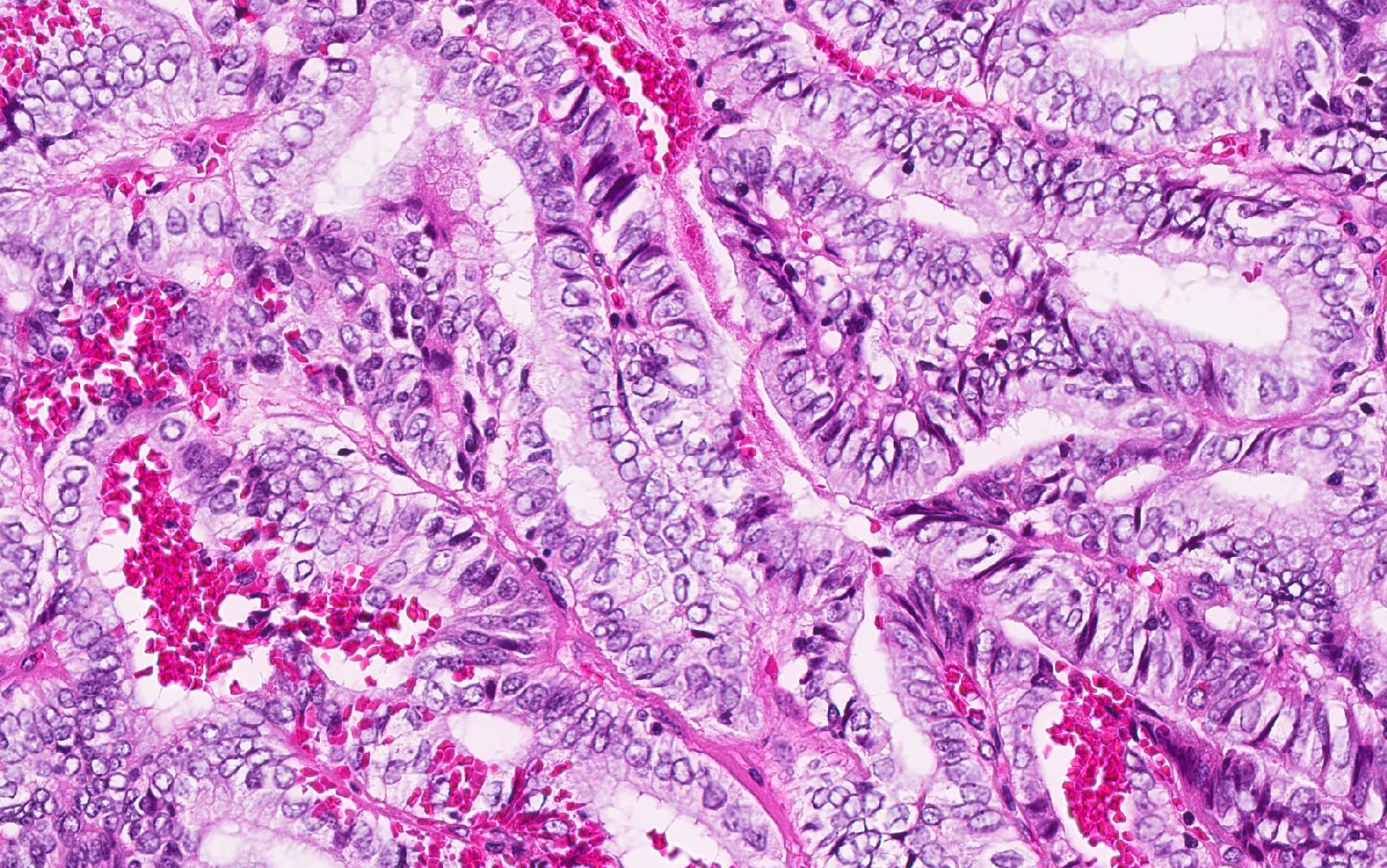
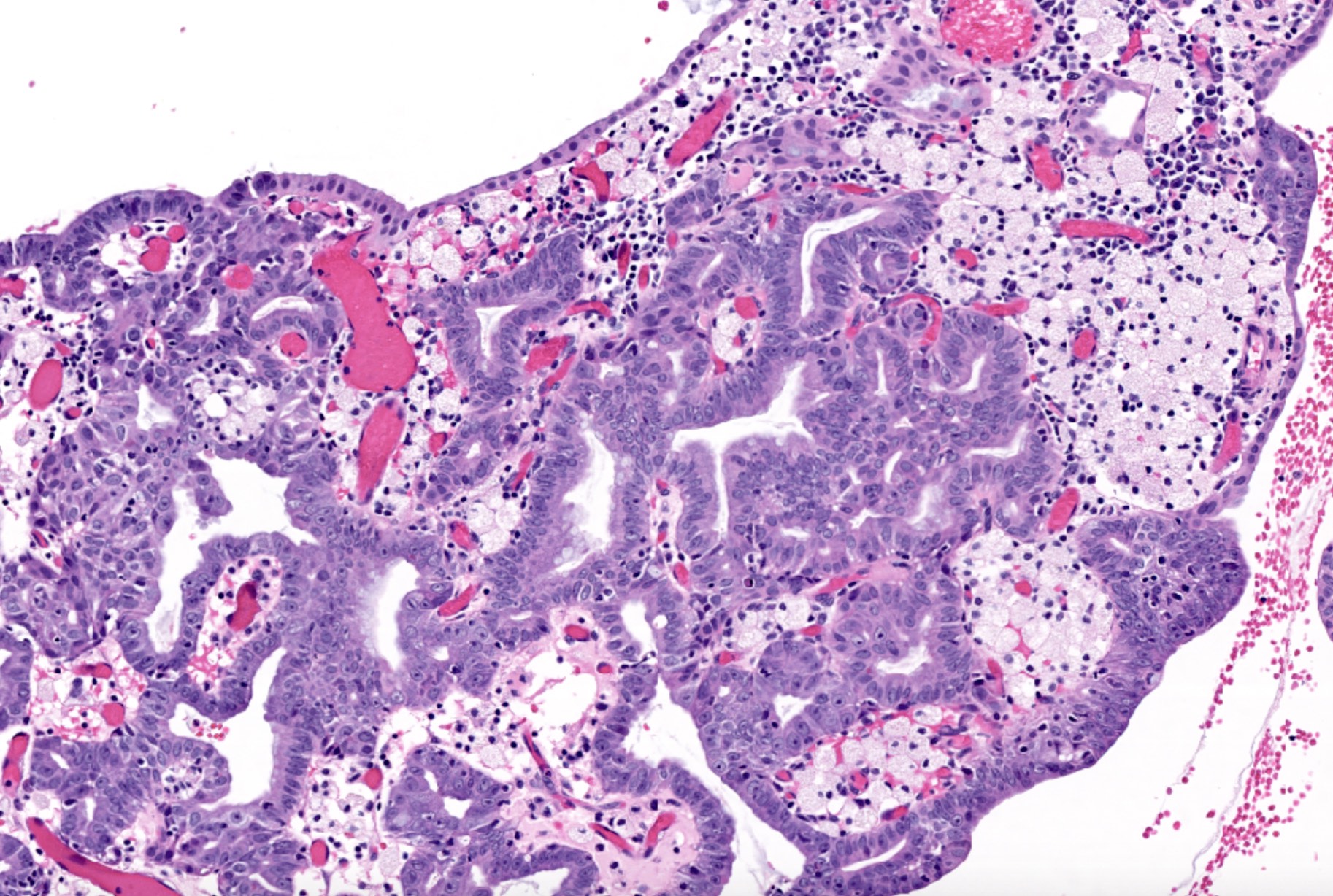
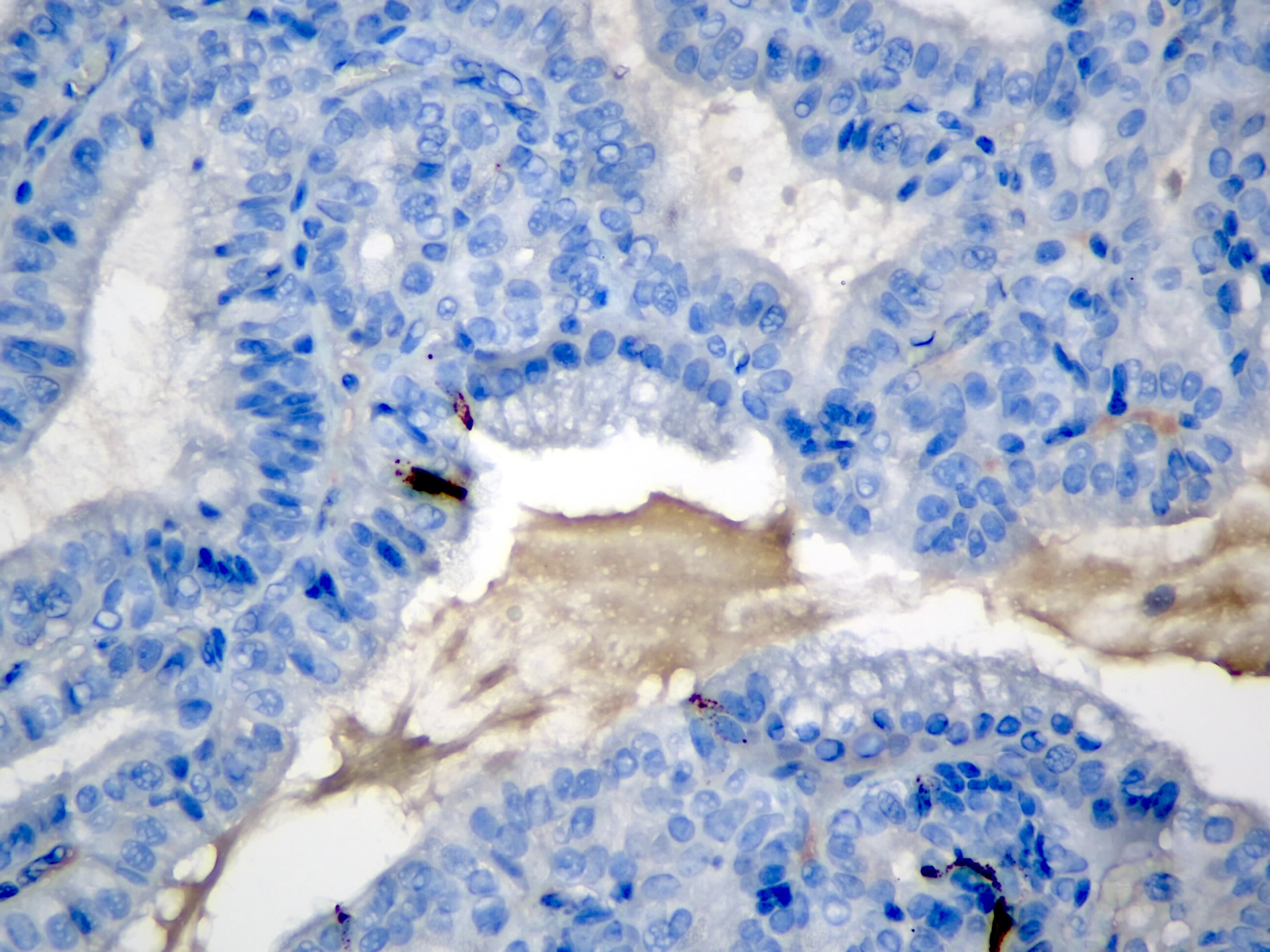
Microscopic (histologic) description
- Pedunculated polyps; nodular lesion in the lumen; the nodules often have normal epithelial covering
- Predominantly tubular, occasionally tubulopapillary architecture
- Compact, back to back small tubular units with minimal lumen
- Neoplastic cells have round nuclei with prominent nucleoli and scant cytoplasm
- Some show nuclei with washed out chromatin resembling papillary thyroid carcinoma
- Squamoid / meningothelial-like morules (> 60%)
- Amorphous amyloid-like hyalinization zones may be present in the stroma
- Cholesterolosis in the polyp and often in the uninvolved gallbladder
- Scattered neuroendocrine cells
- High grade dysplasia (HGD) by default of complexity but the background mucosa is typically devoid of any pathology, including dysplasia
- Usually no significant inflammation in the remaining gallbladder
- Lesions with a mucinous component should be evaluated separately
- Reference: Virchows Arch 2021;478:435
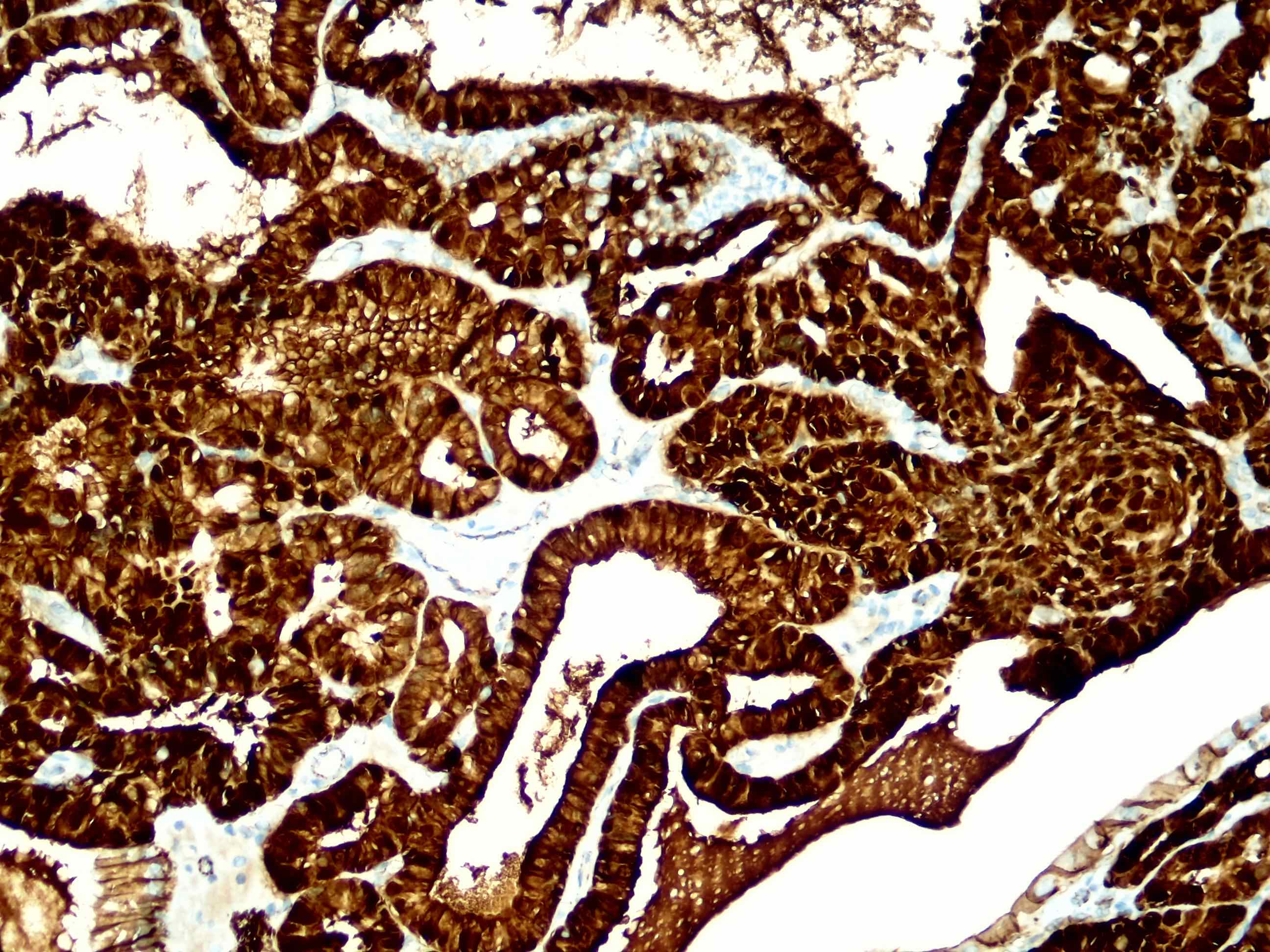
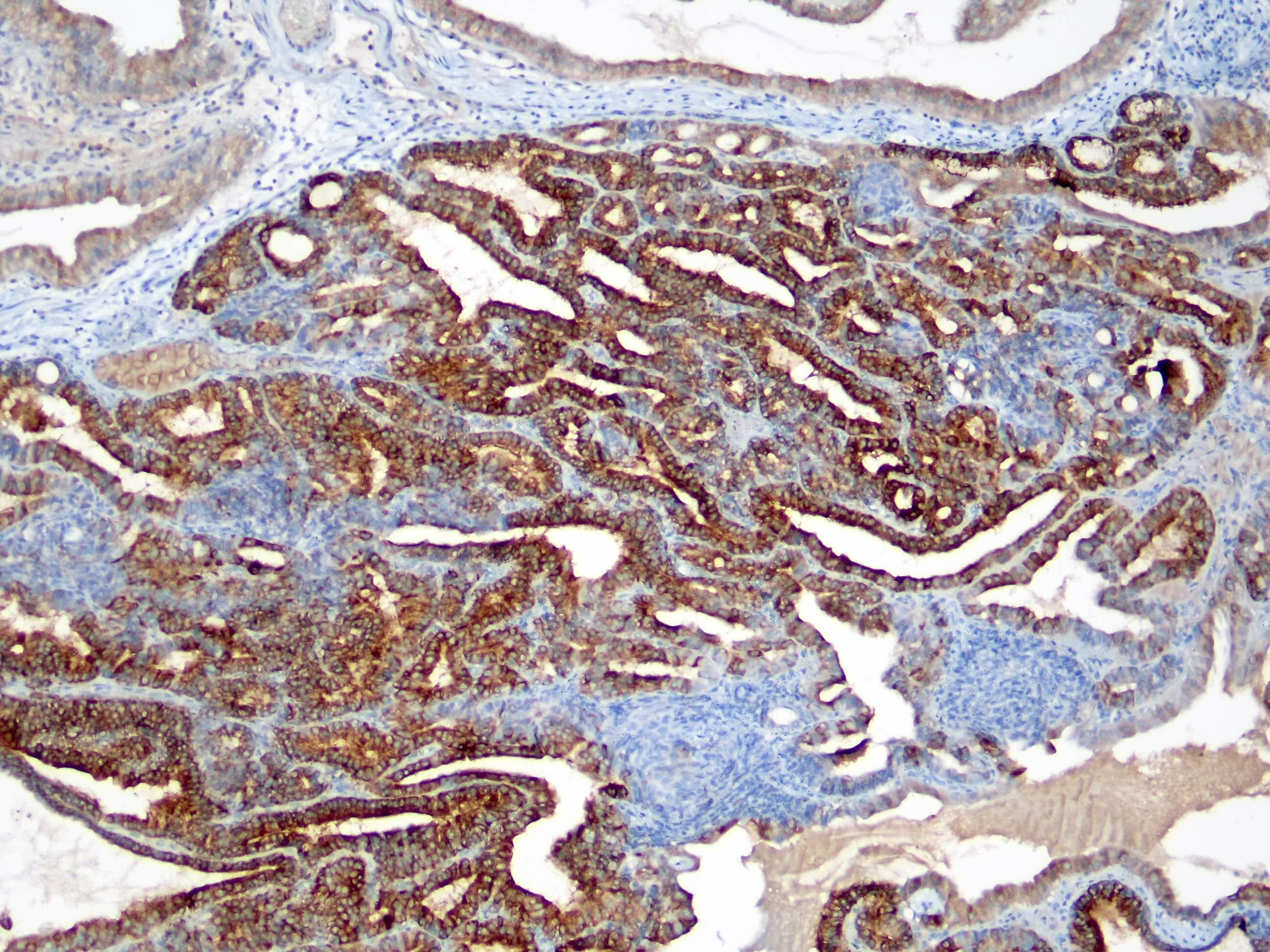
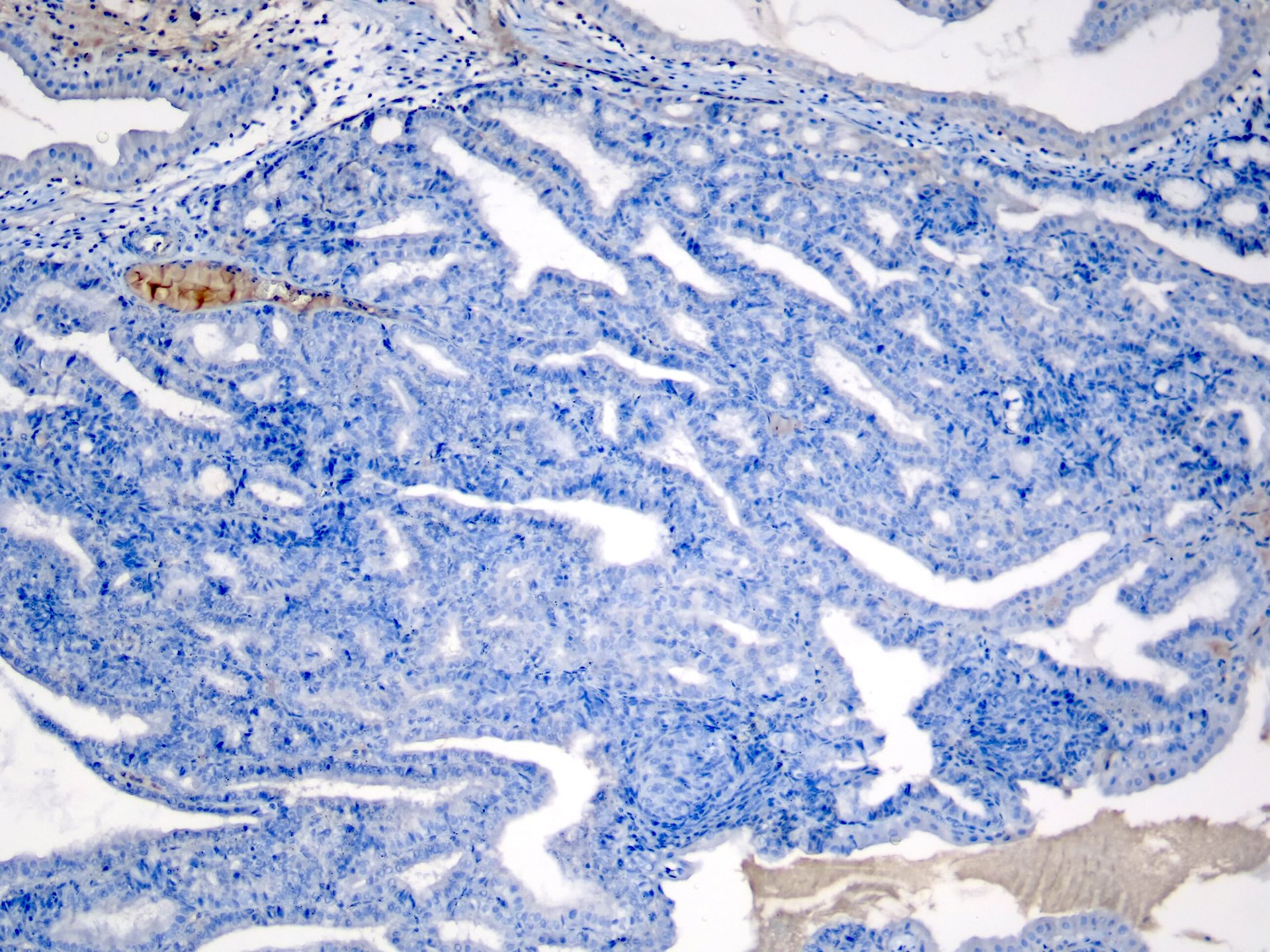
Microscopic (histologic) images
Contributed by Burcin Pehlivanoglu, M.D. and Volkan Adsay, M.D.
Positive stains
- MUC6: in virtually all cases and diffuse strong
- MUC1: variable, often focal
- Beta catenin: nuclear expression typically highlights squamoid morules and occasionally is diffuse in the lesional cells
- CDX2: occasionally positive, especially in squamoid morules (Virchows Arch 2021;478:435, Virchows Arch 2008;453:521)
Negative stains
- MUC5AC (rarely positive) (Virchows Arch 2021;478:435)
- MUC2
Molecular / cytogenetics description
- Remains to be fully elucidated but may be associated with CTNNB1 mutations or pathway (Lab Invest 2018;98:687, Mod Pathol 2019;32:44, Virchows Arch 2021;478:435)
Sample pathology report
- Gallbladder, cholecystectomy:
- Intracholecystic tubular nonmucinous neoplasm (ICTN) (see comment)
- No dysplasia identified in the remainder of the gallbladder
- No invasive carcinoma is identified
- Cholesterolosis (if present)
- Comment: Although there is high grade dysplasia within the lesion, intracholecystic tubular nonmucinous neoplasm (ICTN) typically has an innocuous behavior and does not seem to bear any risk for invasive carcinoma in the gallbladder or biliary tract.
Differential diagnosis
- Pyloric gland adenoma:
- Composed of mucinous cells forming glands, such as gastric pyloric type or Brunner-like mucinous glands
- Often multifocal and can be associated with invasive carcinoma
- Intracholecystic papillary neoplasm:
- Papillary configuration and in areas with tubule formation, which are common, either has mucinous characteristics or intestinal phenotype; cytologically different than ICTNs (Am J Surg Pathol 2012;36:1279, Best Pract Res Clin Gastroenterol 2013;27:285)
- May be of biliary, gastric, intestinal, oncocytic or mixed type (Am J Surg Pathol 2012;36:1279, Hum Pathol 2012;43:1506, Appl Immunohistochem Mol Morphol 2020;28:57)
- May show MUC5AC or MUC2 expression
- More than 50% have associated invasive carcinoma at the time of diagnosis (Am J Surg Pathol 2012;36:1279, Ann Diagn Pathol 2019;40:88, Int J Surg Pathol 2016;24:504)
Board review style question #1
Which of the following is true about intracholecystic tubular nonmucinous neoplasm (ICTN) of the gallbladder?
- Characterized by intestinal type neoplastic glands similar to colonic adenomas
- Commonly associated with diffuse high grade dysplasia in the background gallbladder; connotes high risk for entire biliary tract
- Squamoid morules that show beta catenin nuclear labeling are common
- Typically associated with invasive carcinoma
- Usually seen in gallbladders with severe chronic inflammation
Board review style answer #1
C. Squamoid morules that show beta catenin nuclear labeling are common
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)
Board review style question #2
Which of the following is characteristic for intracholecystic tubular nonmucinous neoplasm (ICTN) of the gallbladder?
- Intestinal differentiation
- Prominent papillary architecture
- Salt and pepper chromatin
- Squamoid or meningothelial-like morules
- Tubule forming cells with abundant mucin
Board review style answer #2
D. Squamoid or meningothelial-like morules
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)
Comment Here
Reference: Intracholecystic tubular nonmucinous neoplasm (ICTN)