Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chahar S, Garcia-Buitrago MT. Biliary intraepithelial neoplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/gallbladderBilIN.html. Accessed March 29th, 2025.
Definition / general
- Biliary intraepithelial neoplasia (BilIN) is a microscopic, premalignant, noninvasive neoplastic lesion of gallbladder or bile duct
- Classification is based on highest degree of cytologic atypia
- BilIN represents the biliary counterpart of pancreatic intraepithelial neoplasia (PanIN)
Essential features
- Non mass forming lesions
- Microscopically flat or micropapillary lesion with low or high grade dysplasia (Mod Pathol 2007;20:701)
- Commonly associated with lithiasis
- Mostly found incidentally in elective cholecystectomy specimens
- Favorable outcome as most high grade dysplasia can be cured by surgical resection
Terminology
- Biliary dysplasia or carcinoma in situ
ICD coding
Epidemiology
- Approximately 1 - 3.5% of cholecystectomies are found to have incidental BilIN
- No gender predilection
- Reference: J Surg Oncol 2006;93:615
Sites
- Gallbladder
- Intrahepatic and extrahepatic biliary tree
Pathophysiology
- Persistent chronic inflammation and cytokine stimulation to biliary epithelium induces neoplastic changes, with involvement of different molecular pathways (Histopathology 2011;59:867)
- KRAS mutations are an early event in biliary carcinogenesis and are present in almost 33% of BilINs, while TP53 mutations occur as a late molecular event (Cancer 2013;119:1669)
Etiology
- Risk factors: lithiasis, primary sclerosing cholangitis, choledochal cysts (Mod Pathol 2007;20:701)
- Anomalous arrangement of pancreaticobiliary ductal system (J Gastroenterol 2007;42:211)
Clinical features
- Does not manifest clinically
- These lesions are identified in mucosa that is adjacent to invasive carcinoma
Diagnosis
- Microscopic examination is required for diagnosis
- Cytology alone is not sufficient to distinguish between reactive changes, preinvasive and invasive lesions (J Gastroenterol 2014;49:64)
Radiology description
- Non mass forming lesions, not detectable by imaging studies (J Gastroenterol 2014;49:64)
Prognostic factors
- Extensive disease, involvement of Rokitansky-Aschoff sinuses and positive margin status increase the risk of recurrence (Virchows Arch 2013;463:651)
Case reports
- 21 year old woman with a giant choledochal cyst (Medicine (Baltimore) 2021;100:e24022)
- 64 year old man with abdominal pain and anorexia (World J Surg Oncol 2019;17:191)
- 70 year old woman with general weakness (Korean J Hepatol 2011;17:328)
- 72 year old man with obstructive jaundice (J Gastroenterol 2021;14:297)
- 84 year old man with epigastric pain and a short irregular stricture in the cystic duct (Intern Med 2021;60:47)
Treatment
- Most high grade BilIN of gallbladder can be cured by cholecystectomy
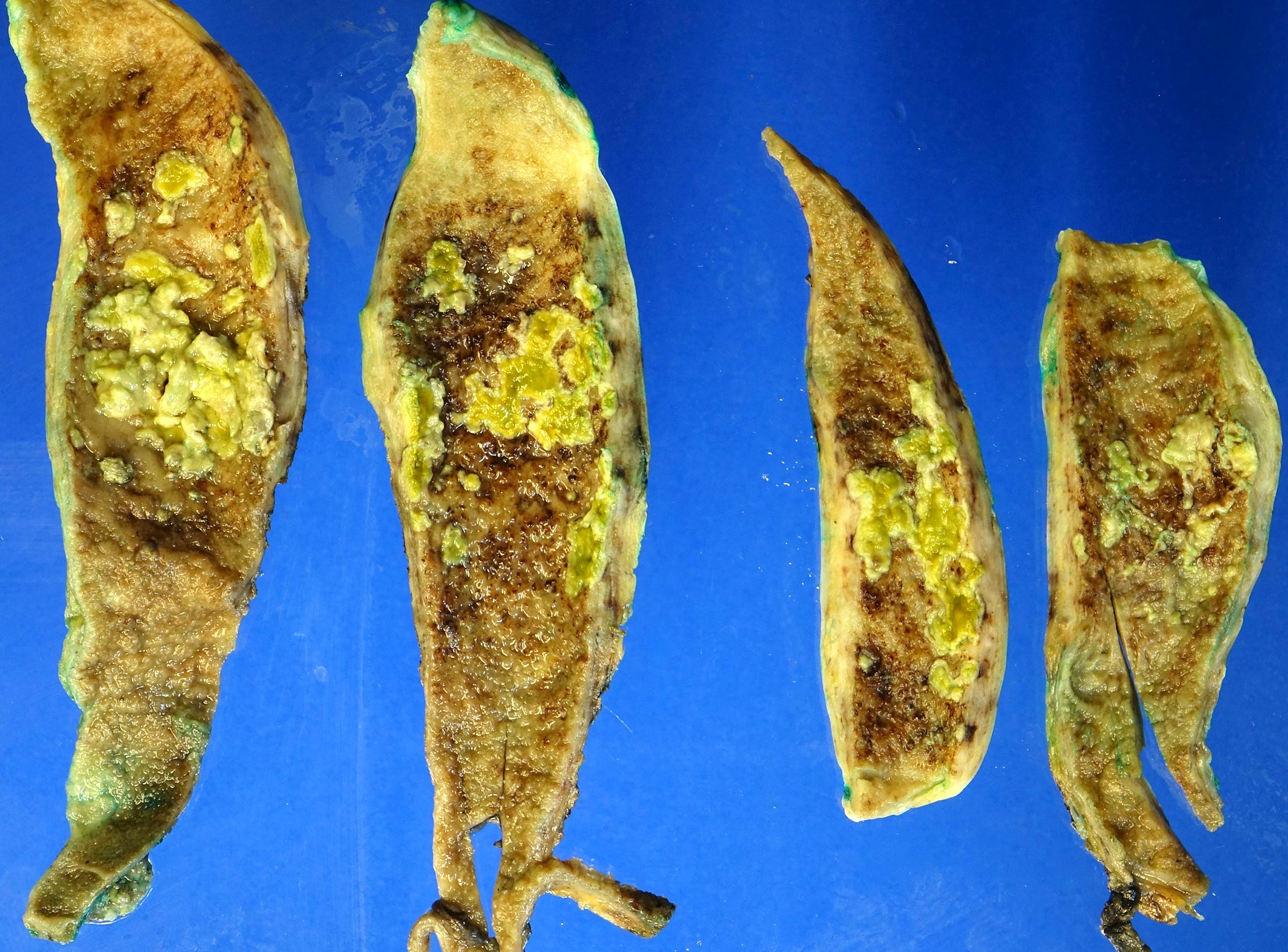
Gross description
- No grossly identifiable lesion
- Granular velvety mucosa
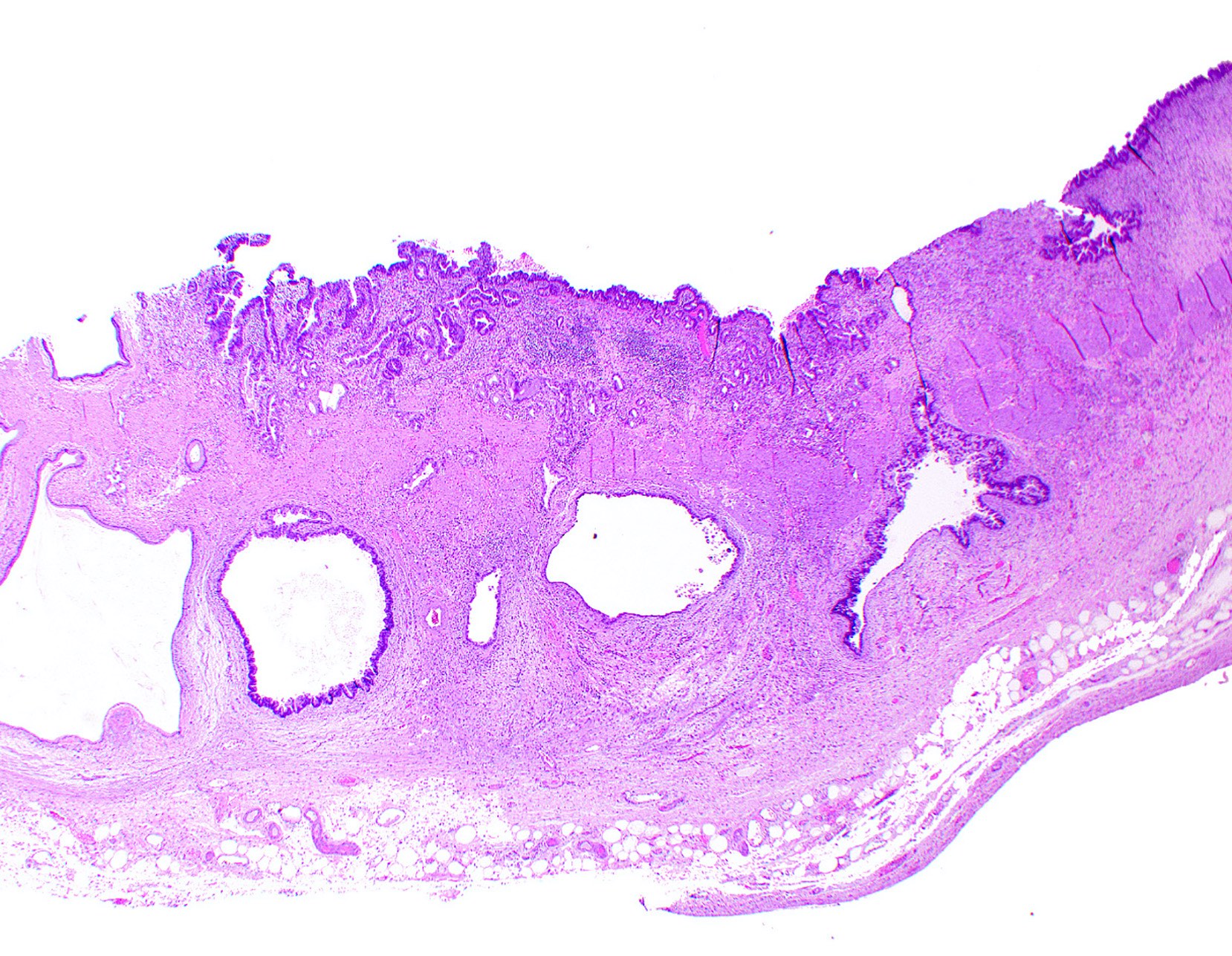
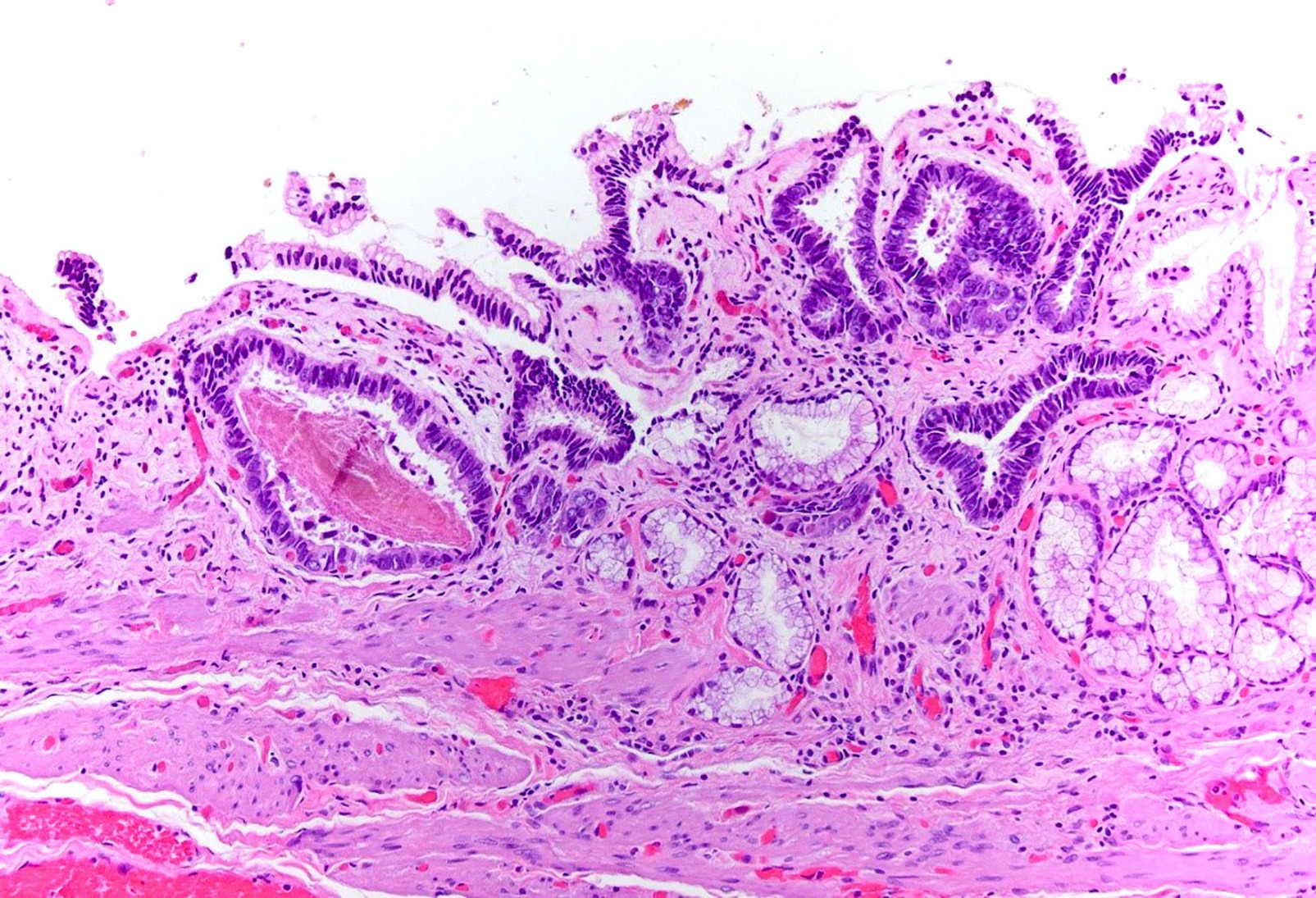
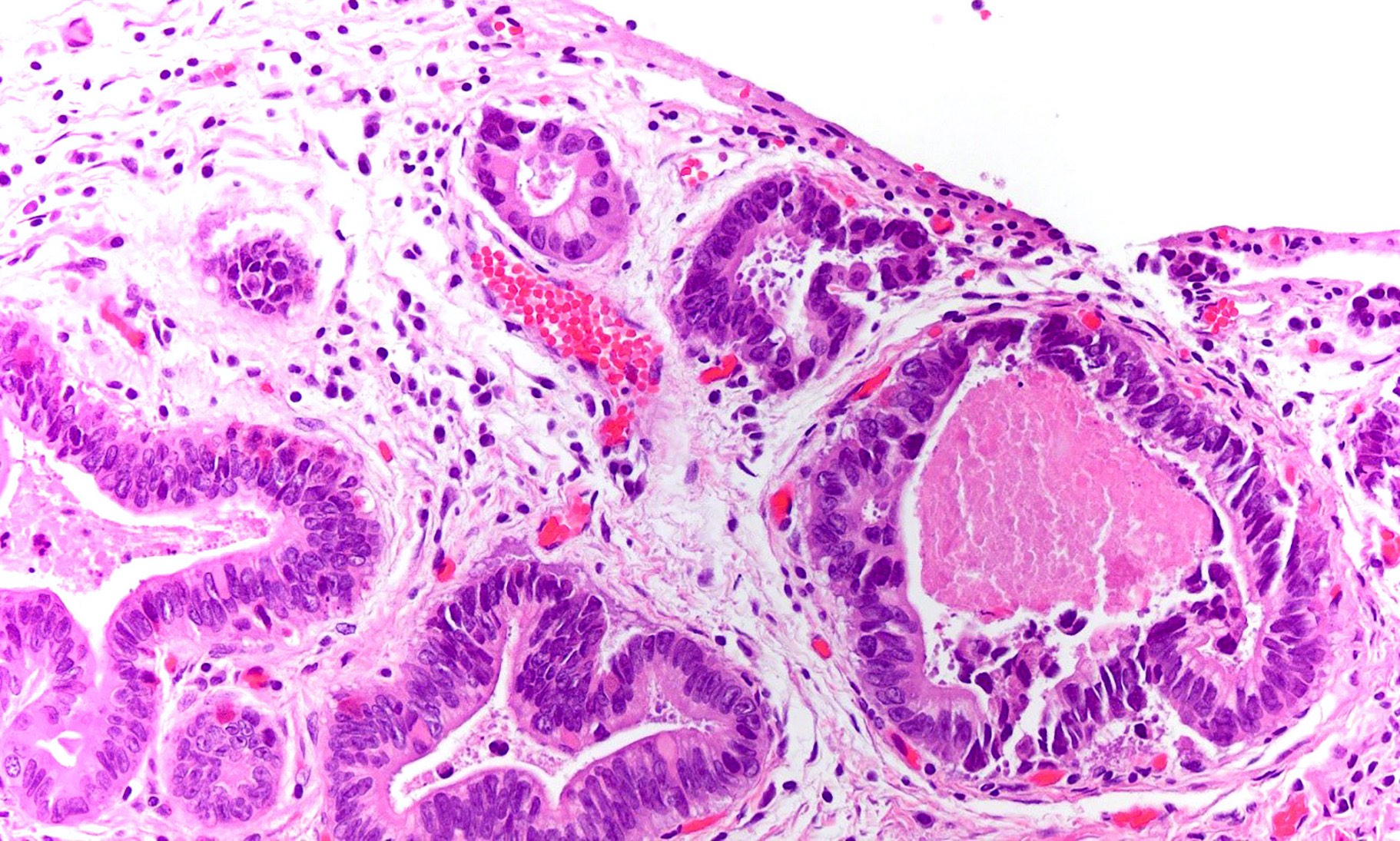
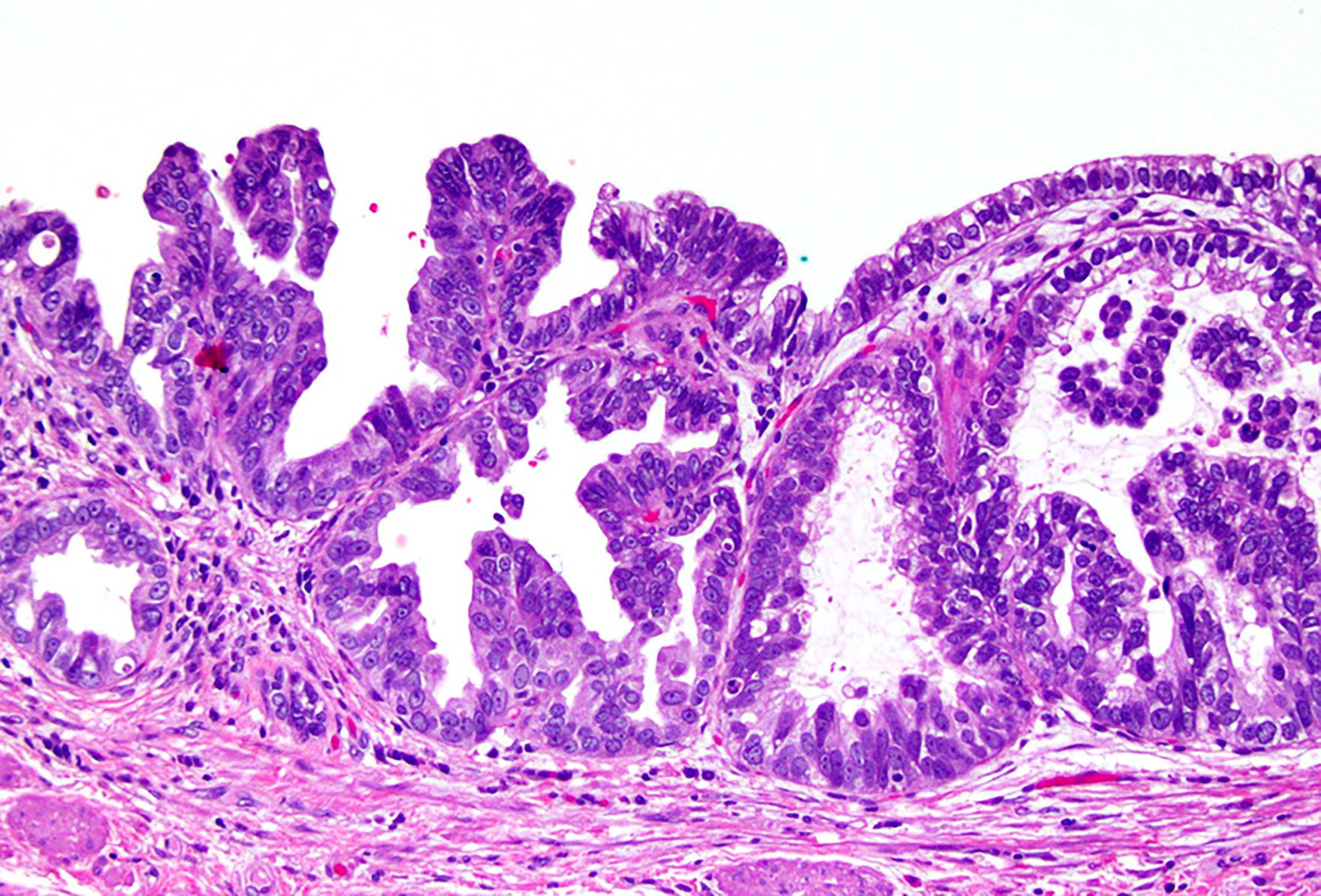
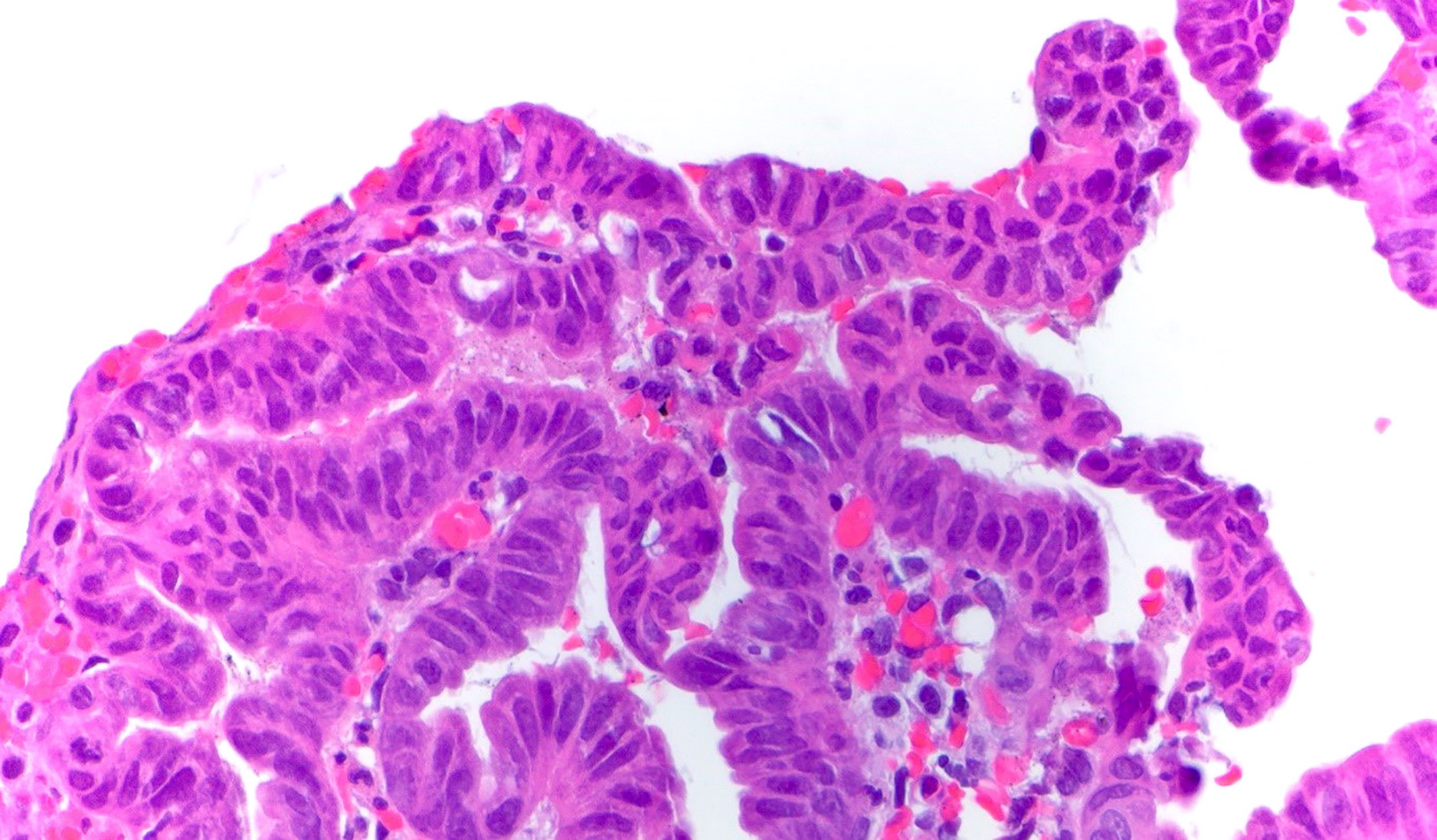
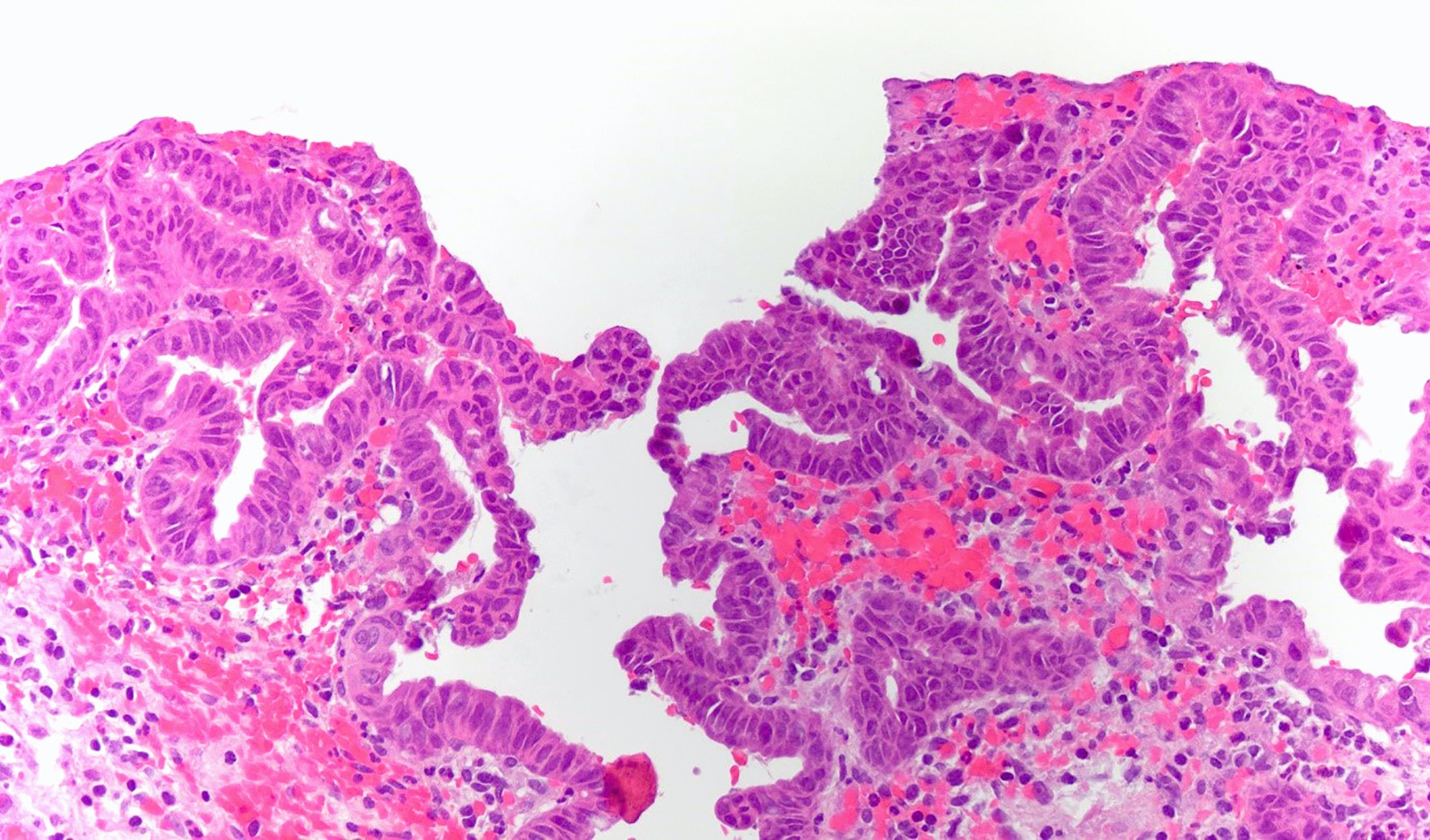
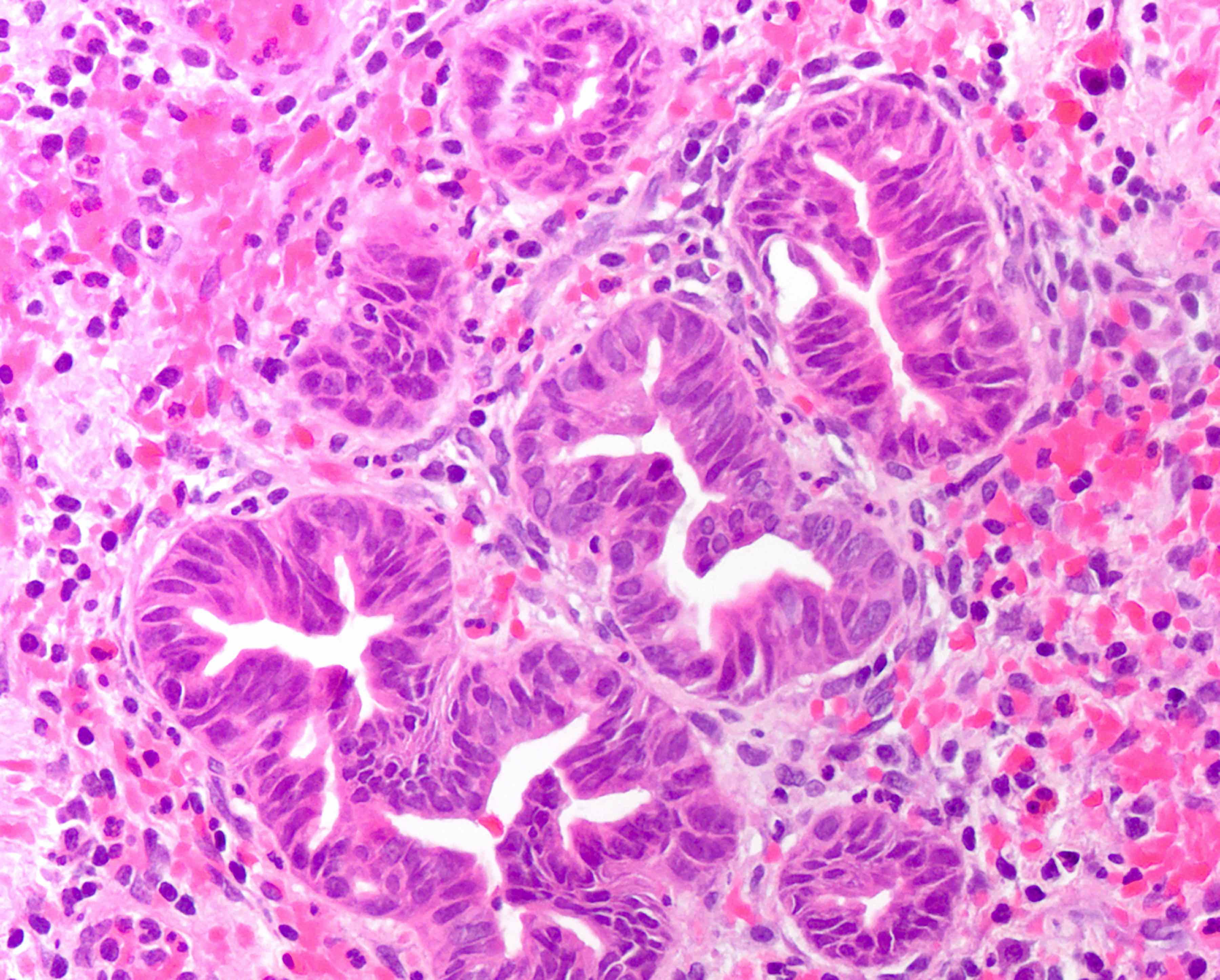
Microscopic (histologic) description
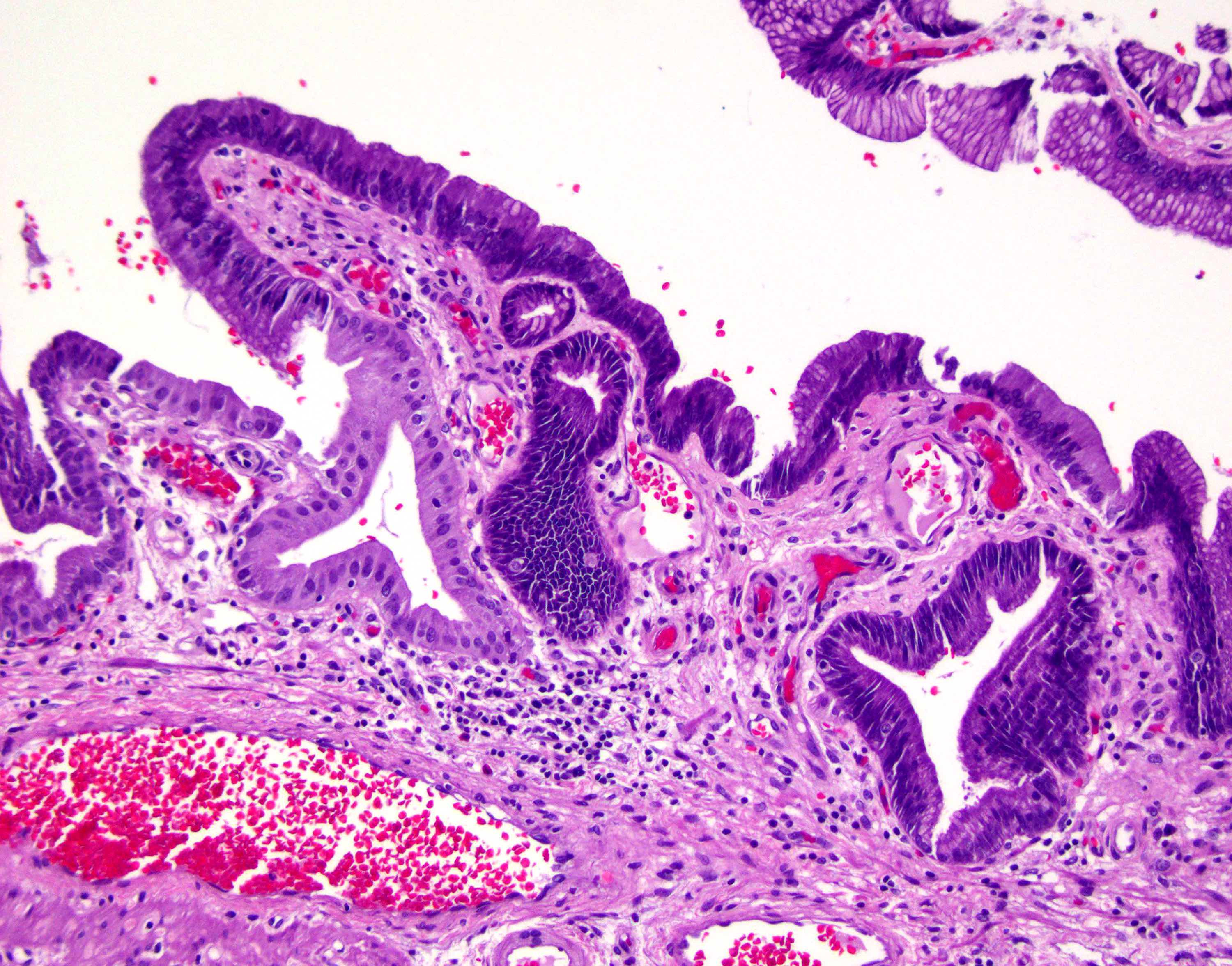
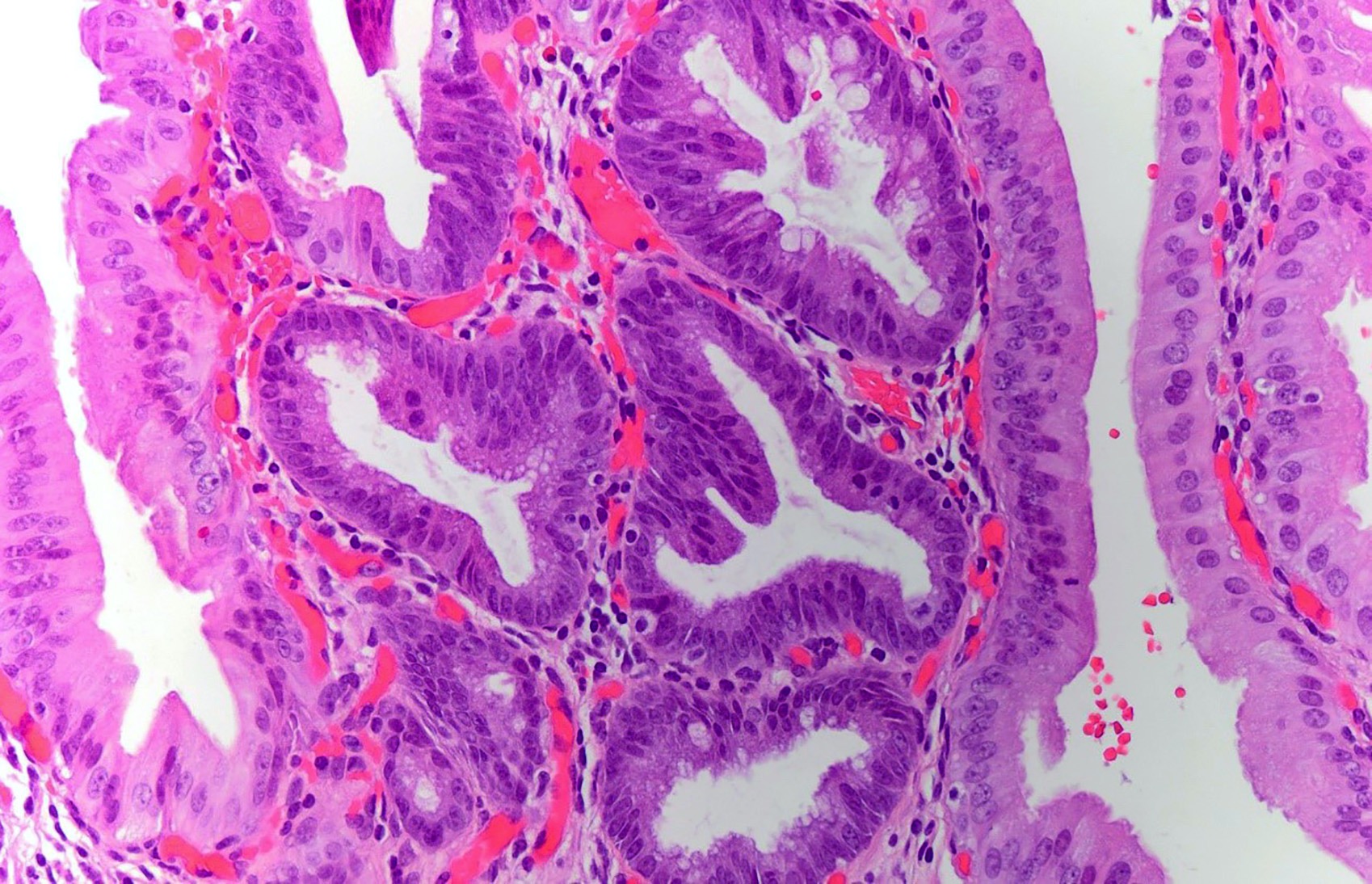
- Predominantly flat, micropapillary or pseudopapillary architecture
- Low grade BilIN
- Involves relatively small areas and does not involve peribiliary glands
- Hyperchromatic nucleus with relatively regular nuclear membrane
- Increased nuclear to cytoplasmic ratio
- Nuclear stratification
- Preserved nuclear polarity
- Mild to moderately increased Ki67 proliferative index
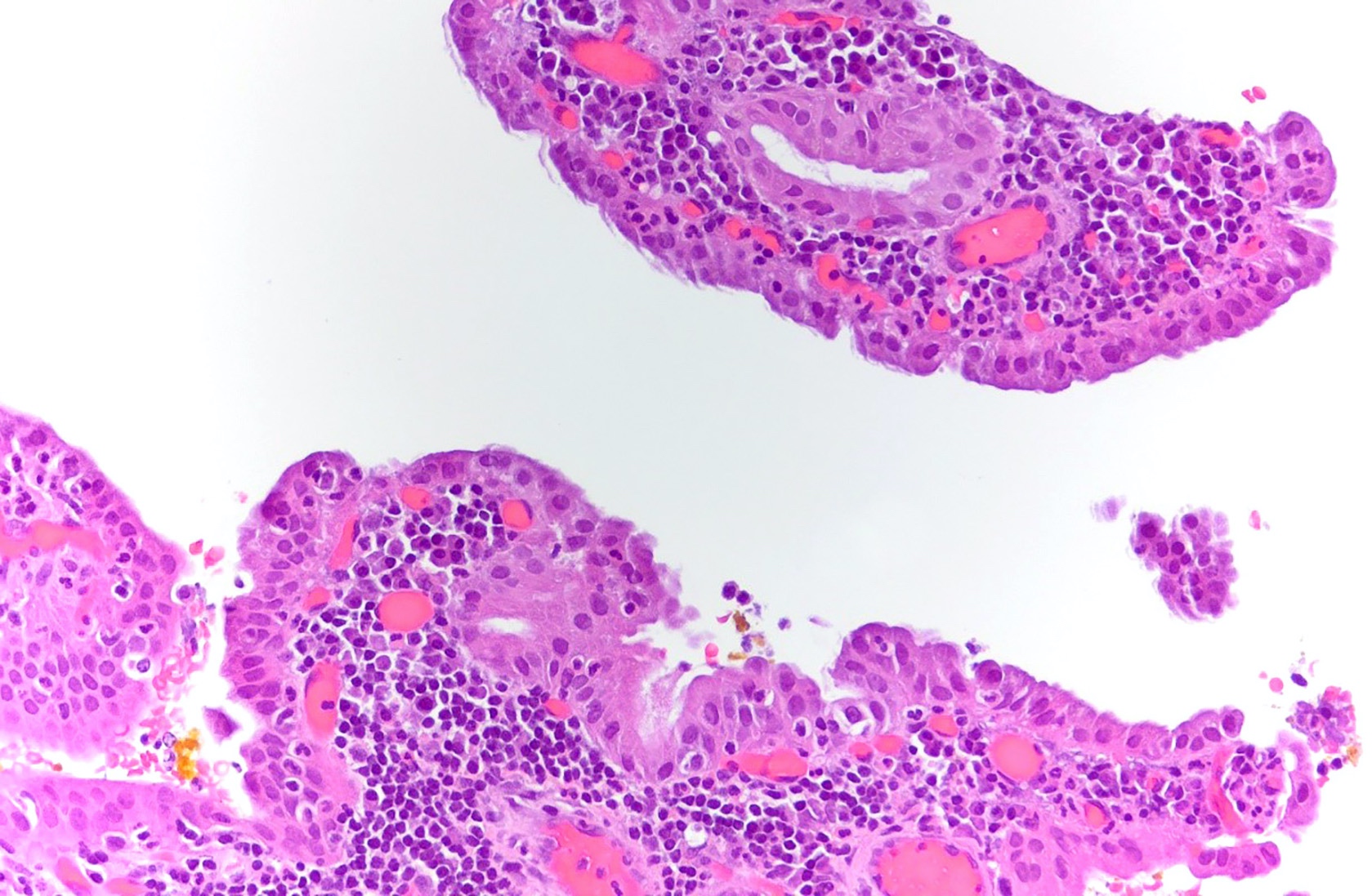
- High grade BilIN
- Involves extensive areas, including peribiliary glands
- Hyperchromatic nucleus with irregular nuclear membrane
- Very high nuclear to cytoplasmic ratio
- Relatively extensive degree of polymorphism and prominent nuclear atypia
- Complex nuclear stratification
- Loss of nuclear polarity
- Markedly increased Ki67 proliferative index
- Reference: Pathol Int 2005;55:180
Microscopic (histologic) images
Cytology description
- BilINs are microscopic, non mass forming lesions; not amenable to sampling via fine needle aspiration
- Bile duct brushing cytology: increased nuclear to cytoplasmic ratio, nucleomegaly, anisonucleosis, nuclear border irregularity, hyperchromasia, visible or prominent nucleoli are associated with next generation sequencing (NGS) positivity (clonal somatic mutations) (J Am Soc Cytopatol 2020;9:520)
Positive stains
Negative stains
Molecular / cytogenetics description
- Approximately 33% of BilIN lesions show KRAS mutations, which occur as an early molecular event during the progression of BilIN; p53 overexpression occurs as a late molecular event (Surg Oncol Clin N Am 2009;18:215)
- p21, p53, cyclin D1 and DPC4 are involved in BilIN carcinogenesis (Hum Pathol 2008;39:1153)
Sample pathology report
- Gallbladder, cholecystectomy:
- Multifocal high grade biliary intraepithelial lesion (BilIN3), extending to Rokitansky-Aschoff sinuses (see comment)
- Comment: The specimen is entirely submitted for microscopic examination. No invasive carcinoma is identified. Cystic duct margin is negative for dysplasia.
- Gallbladder, cholecystectomy:
- Chronic cholecystitis with cholelithiasis and focal low grade biliary intraepithelial lesion (BilIN) (see comment)
- Comment: The specimen is entirely submitted for microscopic examination. No invasive carcinoma is identified. Cystic duct margin is negative for dysplasia.
Differential diagnosis
- Reactive changes:
- Background acute and chronic inflammation present
- Gradual transition between benign epithelium and reactive epithelium
- Adenocarcinoma:
- Presence of invasive component
- Desmoplastic stroma
Additional references
Board review style question #1
Board review style answer #1
A. Associated cholelithiasis. Biliary intraepithelial neoplasia is a premalignant, non mass forming lesion and does not produce any clinical symptoms.
Comment Here
Reference: Biliary intraepithelial neoplasia
Comment Here
Reference: Biliary intraepithelial neoplasia
Board review style question #2
Biliary intraepithelial neoplasia is a preneoplastic lesion and is most commonly cured by cholecystectomy. Which feature is most suggestive of possible recurrence?
- Advanced age
- Extensive lesion with Rokitansky-Aschoff sinus involvement
- Female gender
- Granular velvety mucosa
- Radiologically identifiable mass
Board review style answer #2
B. Extensive lesion with Rokitansky-Aschoff sinus involvement
Comment Here
Reference: Biliary intraepithelial neoplasia
Comment Here
Reference: Biliary intraepithelial neoplasia