Table of Contents
Definition / general | Essential features | Complications of medications and medical solutions | Complications of medical device use | Complications of radiation therapy | Procedural and periprocedural deaths | Gross images | Undetermined causes | Medical misadventures | Comorbidities | Manner of death | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Giffen MA. Therapy related deaths. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/forensicsintrapostopdeaths.html. Accessed March 31st, 2025.
Definition / general
- Deaths which occur due to complications of medical treatment
- Not limited to people dying in a hospital setting
Essential features
- Medications and medically administered solutions are an important and significant source of morbidity and mortality
- If a medical device is used in patient care, it should be investigated as a cause or contributor to death
- Most procedure related deaths occur due to the underlying natural disease or injury which made the procedure necessary
- Comorbidities and social factors should be considered when determining the impact that medical treatment had on the cause and manner of death
- Manner of death classification with therapy related deaths is complex and should weigh a variety of factors, including what direct impacts (if any) the treatment had on morbidity and mortality
Complications of medications and medical solutions
- A variety of medications and medically prepared solutions can result in complications which may cause or contribute to death
- Likelihood of reactions or interactions between medications increases significantly with an increasing number of administered agents (Expert Opin Drug Saf 2014;13:57)
- Medication reactions can occur even at the recommended dosages and frequency:
- Hypotension (i.e. antihypertensives)
- Hyper / hypoglycemia (i.e. antidiabetics)
- Electrolyte abnormalities (i.e. antihypertensives, replacement supplements, overhydration)
- Dysrhythmias (i.e. digitalis)
- Idiopathic reactions (i.e. serotonin syndrome, neuroleptic malignant syndrome)
- Paradoxical reactions (i.e. antidepressants, benzodiazepines)
- Acute and delayed allergic reactions (i.e. monoclonal antibodies)
- Anaphylaxis (i.e. penicillin)
- Chronic systemic or organ specific toxicities:
- Most common with chemotherapeutic or immunomodulatory therapies
- Cardiac toxicity
- Hepatic toxicity
- Bone marrow suppression (i.e. ineffective hematopoiesis, infection)
- Secondary neoplasia
- Radiology contrast material:
- Most reactions occur with iodinated contrast
- Rare reactions have been reported with gadolinium contrast (CNS Drugs 2018;32:229)
- Barium and other orally introduced contrast material can lead to a variety of complications but these are rarely fatal on their own
- Blood products / apheresis:
- Blood products are not benign and can result in a variety of reactions that cause or contribute to death
- Any reaction believed to have caused or contributed to death must be reported to the FDA
- Acute / delayed hemolytic reactions
- Allergic / anaphylactic reactions
- Transfusion related acute lung injury (TRALI)
- Transfusion associated cardiac overload (TACO)
- Especially in persons with underlying cardiac / renal conditions
- Sepsis / transfusion associated infectious disease transmission
- Electrolyte abnormalities (i.e. hyperkalemia with massive transfusion protocols, hypocalcemia from citrate toxicity)
- Resuscitation fluids:
- Hyper / hypotonic fluids can lead to significant electrolyte abnormalities, especially in patients on NPO (nothing by mouth) diet
- Isotonic fluids, especially at large doses (such as intraoperative irrigation), can result in significant electrolyte and physiologic abnormalities
- Sudden corrections of electrolyte abnormalities can result in death (i.e. central pontine myelinolysis)
- Important measures to review include fluid inputs, urine outputs and antemortem / postmortem electrolyte measurements
- Medication and dosage errors:
- More common for patients residing in facilities (inpatient, long and short term) versus outpatients
- Medication administration logs can be helpful in determining under / overdosage
- If medications are available, check pill counts and descriptions against bottle
- Pill identifier websites are available at no cost to providers
- If a medication or dosage error is suspected and antemortem blood samples are available, obtain them for possible toxicology testing (the closest after the administration time preferred)
- Some genetic testing is available for persons believed to be hypermetabolizers or poor metabolizers
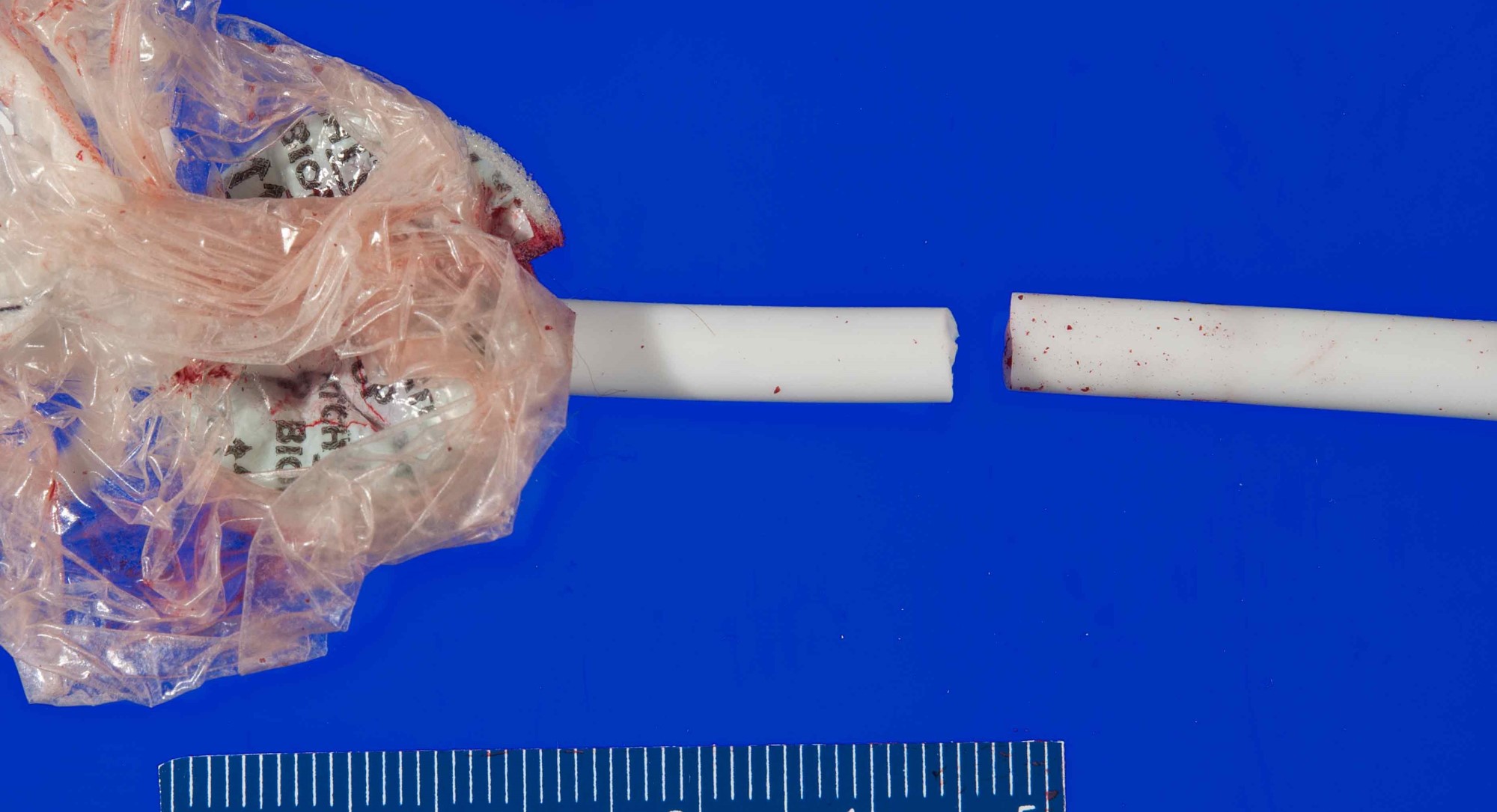
Complications of medical device use
- Both implanted and external medical devices may result in complications that cause or contribute to death
- Intubation / rescue airways / tracheostomy tube:
- Pneumothorax
- Laryngeal, tracheal or esophageal trauma
- Intubation of the esophagus / mainstem bronchus
- Attempted intubation with impaction of foreign body
- Dislodgement or occlusion
- Orogastric tubes
- Craniofacial trauma (i.e. malplacement into the cranial vault)
- Foley catheters
- Infection
- Bladder perforation
- Vascular catheters
- Hemorrhage
- Infection
- Thromboembolism
- Arteriovenous fistulization
- Implanted medical devices
- Orthopedic hardware: infection, bony fracture, hardware failure
- Pacemaker / implanted defibrillators: erroneous or repeated discharge, lead displacement, battery failure
- May require interrogation of the device
- Nerve stimulators: lead displacement
- External ventricular assist devices: pump failure, hemorrhage, thromboembolism
- Tissue expanders / implants: infection, chemical injury, foreign body reaction
- Medical synthetic implants (i.e. mesh): infection, scarring
- Device embolization (i.e. catheter tip embolization, IVC filter dislodgement)
- Catheter failure (i.e. hemorrhage, air embolism)
- External equipment failure
- Ventilators
- Medication administration pumps
- Cardiac bypass pumps
- Any medical equipment suspected to have been involved in a patient's injury or death should be removed from use and investigated
- Manufacturer or appropriate engineer may need to examine the device to determine safety prior to continued use (maintain the device as is until it can be examined)
Complications of radiation therapy
- Radiation can cause a variety of acute and delayed complications
- Radiation induced necrosis (i.e. wound dehiscence, infection)
- Radiation fibrosis / scarring (i.e. mediastinal fibrosis, bowel / bladder obstruction)
- Secondary malignancy (i.e. angiosarcoma)
Procedural and periprocedural deaths
- Vast majority of deaths during medical procedures occur as a direct result of the underlying natural disease process or injury which required the treatment
- Some state and local statutes require medicolegal investigation of all deaths occurring during medical procedures or under anesthesia; this does not always necessitate an autopsy
- Severe underlying natural disease is another common cause of death (i.e. myocardial infarction due to severe coronary artery disease during a surgical procedure)
- Procedural safety has greatly improved in recent years due to mandatory safety checklists and a time out process conducted just before the start of an invasive procedure (AORN J 2019;109:P5)
- All procedures carry inherent risks, which are often modified by the severity of disease or injury, underlying comorbidities (i.e. hypertension, diabetes mellitus) and social factors (i.e. tobacco, alcohol, drug use)
- Surgical procedures are commonly assigned a risk score which takes into account risk factors and the likelihood of significant morbidity or mortality due to the procedure
- Emergent procedures (conditions requiring treatment due to risk of severe morbidity and mortality)
- Consent is often implied or signed by a surrogate due to severity of illness / injury
- Risks of morbidity or mortality due to untreated injury / illness are greater than that of the procedure
- Traumatic injuries (i.e. gunshot wounds, stab wounds, blunt injuries, burns)
- Medical emergencies (ruptured vascular aneurysms, cerebrovascular events, gastrointestinal tract perforation)
- Consent is often implied or signed by a surrogate due to severity of illness / injury
- Nonemergent / elective procedures (conditions which require treatment but are typically stable)
- Require informed consent with understanding of known procedural risks
- Not all elective procedures are low risk and often carry an associated risk score
- Orthopedic joint replacements (i.e. bone marrow embolization, infection)
- Cancer resections
- Vascular surgeries (i.e. stable vascular aneurysms, asymptomatic endarterectomy)
- Routine maintenance procedures (tonsillectomy, cholecystectomy, skin excisions)
- Cosmetic procedures
- While generally considered to be low risk; individual tolerances and comorbidities vary
- Under normal circumstances death should not occur
- Nonreconstructive plastic surgical procedures
- Liposuction (i.e. adipose or air embolization, infection)
- Filler / dermal subcutaneous injections (i.e. filler embolization, infection)
- Botox injection (i.e. systemic botulinum toxicity via vascular injection)
- While generally considered to be low risk; individual tolerances and comorbidities vary
- Dental procedures
- Generally considered low risk but comorbidities can increase the risk of adverse events
- Anesthetic and medication overdoses have been reported (J Forensic Sci 1989;34:377)
- Bacteremia, sepsis and infective endocarditis can occur
- Deaths under anesthesia
- Type of anesthesia (general versus local)
- While local anesthetics are generally considered safer, their use can still result in death (i.e. vascular injection leading to dysrhythmia)
- Types of inhaled anesthetics (i.e. wrong type / dosage of gas, incorrectly filled tanks, pressure valve failure resulting in pneumothorax)
- Length of time under anesthesia (longer times significantly increase risk)
- Underlying genetic conditions predisposing to reactions (i.e. malignant hyperthermia)
- Type of anesthesia (general versus local)
- Remember that medication errors can also occur during procedures
Gross images
Undetermined causes
- Deaths which occur during the course of medical treatment or procedures without identifiable cause
- Extensive, thorough medical record review can be helpful in excluding potential causes of death
- If the survival interval between the inciting event and death is long, extensive review of medical records might be the only way to determine what occurred (or did not occur)
- Often require an autopsy to eliminate occult drug toxicity, injury or natural disease
- If no anatomic or toxicologic cause of death can be determined by autopsy, additional factors which should be considered / excluded:
- Electrolyte abnormalities (i.e. hyper / hypokalemia, hyper / hypocalcemia)
- Hyper / hypoglycemia
- Idiopathic medication reactions / interactions
- Physiologic reactions (i.e. vasospasm, vasovagal mediated bradycardia, idiopathic dysrhythmias, hyper / hypotension)
Medical misadventures
- Despite safeguards, a variety of medical errors can occur during treatment
- Some errors are harmless and have no effect on the subsequent treatment course
- Some errors are harmful and can result in varying degrees of morbidity or mortality
- In general, known and expected complications of a procedure are not considered medical misadventures (i.e. infection, expected hemorrhage)
- Physicians and literature originating in the specialty (or specialties) of question are the best sources of knowledge for appropriate evidence based treatments and expected outcomes
- Medical misadventures are those injuries or outcomes which are not expected (i.e. vascular injury unrelated to the anticipated procedure site, ligation of the incorrect vascular supply, incorrect line placement without verification, wrong patient / wrong procedure)
- They do not imply medical incompetence or negligence
- They do not imply negligence
- They do not imply an unavoidable error occurred
- Every effort should be made to identify the source of the unexpected outcome and complicating factors which may have contributed (i.e. atypical anatomy, distortion due to prior procedures)
- Report language should only reflect factual findings
- Judgment of error should be reserved for appropriate legal / review body
- Subject matter experts in the field of practice are better versed than the pathologist at determining what are / are not appropriate treatments or complications
- Do not use malpractice or similar terminology, which should be part of a legal / review body determination
Comorbidities
- Comorbidities often potentiate or adversely impact medical complications
- An increasing number of comorbidities significantly increases the risk that an individual will suffer complications during medical treatment and increases the likelihood of severe complications
- Chronic obstructive pulmonary disease / asthma / reactive airway disease (i.e. increased risk of pulmonary failure, prolonged intubation, pneumonia)
- Diabetes mellitus (i.e. poor wound healing, infection)
- Hypertensive and atherosclerotic cardiovascular diseases (i.e. poor wound healing, vascular complications)
- Dementia (i.e. aspiration)
Manner of death
- Some jurisdictions use a separate classification for most accidental or natural complications of medical treatment: therapeutic complication (J Forensic Sci 2006;51:1127)
- If death is directly related to underlying natural disease without contribution by medical treatment
- Manner is natural
- If death is related to the underlying injury without contribution by medical treatment
- Manner is determined by the cause of the injury: accident, homicide, suicide (and potentially undetermined)
- If death is due to a known and expected complication of therapy for a natural disease
- Manner is natural
- If death is due to use of inappropriate, defective or malfunctioning medical equipment / devices; and there is no evidence that the equipment was tampered with to result in malfunction
- Manner is accident
- If death is due to grossly negligent medical care without evidence of volitional act to cause harm or death
- Manner is accident
- This does not preclude the possibility of legal liability or actions by a medical board
- If death is due to a volitional act to cause harm or death (i.e. administration of large doses of opiate medications to cause cardiorespiratory arrest)
- Manner is homicide
- Law enforcement investigation will reveal additional information to support the manner in these cases
- Oftentimes caregivers that repeatedly cause harm to patients follow repeated patterns which may be revealed by thorough investigation (i.e. ICU nurse that has more cardiopulmonary arrests on their shifts than any other nurse due to smothering patients to create attention for themselves)
- If death is due to an undesirable or unexpected outcome of a diagnostic or therapeutic procedure and the circumstances are determined to be outside the realm of reasonably acceptable risk and expected outcome
- Manner is accident
- If death occurs in high risk surgical patients undergoing (or after) high risk procedures for natural disease (i.e. coronary bypass grafting due to coronary artery disease without procedural complications)
- Manner is natural
- If the death is due to undetermined causes (regardless of expected outcomes)
- Manner is undetermined
- There are a variety of gray zones and disagreements with some of the above classifications; however, these are the generally accepted classifications agreed upon by the National Association of Medical Examiners (NAME)
- For additional information about the nuances of death certification, please reference:
Additional references
- DiMaio: Forensic Pathology, 2nd Edition, 2001, Dolinak: Forensic Pathology - Principles and Practice, 1st Edition, 2005, Froede: Handbook of Forensic Pathology, 2nd Edition, 2003, Spitz: Spitz and Fisher's Medicolegal Investigation of Death - Guidelines for the Application of Pathology to Crime Investigation, 4th Edition, 2005
Board review style question #1
A 75 year old man is brought to the emergency department for increasing abdominal pain of 3 hours duration. His past medical history is significant for hypertension and 60 pack years tobacco use. Emergent CT scan reveals an abdominal aortic aneurysm with active extravasation for contrast into the abdomen. He is taken immediately from the scanner to surgery but dies within minutes of the procedure due to blood loss. What is the best classification for this manner of death?
- Accident
- Homicide
- Natural
- Suicide
- Undetermined
Board review style answer #1
C. Natural
Ruptured abdominal aortic aneurysms carry a high mortality rate regardless of operative treatment. There is no evidence to support that the surgical procedure caused or contributed to death and thus the underlying natural disease is the cause of death. Therefore, the manner of death is best classified as natural.
Comment Here
Reference: Therapy related deaths
Ruptured abdominal aortic aneurysms carry a high mortality rate regardless of operative treatment. There is no evidence to support that the surgical procedure caused or contributed to death and thus the underlying natural disease is the cause of death. Therefore, the manner of death is best classified as natural.
Comment Here
Reference: Therapy related deaths
Board review style question #2
An 82 year old woman is brought to the emergency department after sustaining multiple gunshot wounds in a domestic altercation. Her past medical history is significant for poorly controlled diabetes mellitus, atherosclerotic and hypertensive cardiovascular disease and hepatic cirrhosis. She is found to have 2 gunshot wounds of the face and 1 of the neck. A branch of the facial artery is embolized due to active bleeding but she is relatively stable immediately after the procedure. She subsequently requires a central venous line and develops sepsis due to a catheter associated infection. Due to coagulopathy related to the sepsis, she develops a significant hematoma requiring blood transfusion at the site of the central venous line. Despite aggressive treatment, she dies 2 days later. What is the best classification for this manner of death?
- Accident
- Homicide
- Natural
- Suicide
- Undetermined
Board review style answer #2
B. Homicide
This individual has a significant past medical history, develops sepsis and suffers a significant medical complication during treatment. Both the sepsis and medical complication are a result of needed treatment for the initial gunshot wounds. Therefore, the gunshot wounds (though not independently lethal) are the proximate cause of death. The manner of death is best classified as homicide. Her significant medical complications and natural disease would be appropriate to list under other significant contributing factors if they were felt to be contributory.
Comment Here
Reference: Therapy related deaths
This individual has a significant past medical history, develops sepsis and suffers a significant medical complication during treatment. Both the sepsis and medical complication are a result of needed treatment for the initial gunshot wounds. Therefore, the gunshot wounds (though not independently lethal) are the proximate cause of death. The manner of death is best classified as homicide. Her significant medical complications and natural disease would be appropriate to list under other significant contributing factors if they were felt to be contributory.
Comment Here
Reference: Therapy related deaths