Table of Contents
Definition / general | Essential features | Terminology | Physiology | Diagrams / tables | Clinical features | Laboratory | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Electron microscopy description | Electron microscopy images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Metcalf BD, Turashvili G. Anatomy, histology & embryology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/fallopiantubesnormal.html. Accessed December 28th, 2024.
Definition / general
- Fallopian tube is an anatomic bridge between the ovary and the uterus, in which fertilization of an egg by sperm may occur followed by delivery of the zygote to the uterus; it also provides the environment needed to sustain the gametes and prevent rejection of the zygote by the body
Essential features
- Fallopian tube is divided into several anatomic regions (i.e., intramural, isthmus, ampulla and infundibulum) and comprises mucosal, muscular and serosal layers
- Mucosa is composed of 4 cell types (ciliated columnar cells, secretory cells, peg [intercalated] cells and basal cells) that can be readily recognized on H&E staining; however, more cell subtypes can be identified immunohistochemically and molecularly
- Composition of these cell types varies based on location, phase of the menstrual cycle and menopausal status
- A complex immune system moderates tolerance to a fertilized egg, fights infection and plays a role in cancer surveillance
Terminology
- Other historically used names include tuba uteri, oviduct, uterine tube or tube (J Reprod Fertil 1988;82:843)
Physiology
- Ciliated cells move egg toward the ampulloisthmic junction
- Ampulloisthmic junction is the site of fertilization
- Growth is encouraged by estradiol
- Deciliation is encouraged by progesterone
- Prolonged exposure to progesterone or removal of estrogen causes epithelial atrophy (Mills: Histology for Pathologists, 5th Edition, 2019)
- Motile cilia beat to provide fluid flow (Int J Gynecol Cancer 2018;28:1535)
- Control gamete and embryo movement (Dev Cell 2022;57:914)
- Secretory cells
- Secrete oviduct fluid
- Complex mixture of materials derived from plasma and proteins specifically formed by the tubal epithelium
- Function of tubal fluid (J Reprod Fertil 1988;82:843)
- Moisturizes surface epithelium
- Bacteriostatic function
- Electrolyte balances may influence the development of embryos into blastocysts, the motility of sperm and the health of the ovum
- Contains nutrients for spermatozoa, oocytes and zygotes and promotes the capacitation of sperm by removing glycoproteins and other molecules from the plasma membrane
- Major constituents are calcium, sodium, chloride, glucose, proteins, bicarbonates, amylase, lactic acid (J Reprod Fertil 1988;82:843)
- Bicarbonates and lactic acid are vital to the sperm's use of oxygen; they also help with postfertilization egg development
- Tubal fluid flows against the action of cilia (i.e., toward the fimbriated end) (J Reprod Fertil 1988;82:843)
- Formation of fallopian tubal fluid (Reproduction 2001;121:339)
- Secrete oviduct fluid
- Intercalated cells are hypothesized to be stem / progenitor cells (J Reprod Immunol 2022;152:103646)
- Basal cells express epithelial and T cell markers, indicative of potential immune function (Dev Cell 2022;57:914)
- After menopause, the lining will contract and the epithelial cells will decrease in number, leading to blunting of the plica
- During pregnancy
- Inactive during gestation
- Mild decidual change in the endosalpingeal stroma during the later half of pregnancy
- Epithelial atrophy
- Birth control pills and tubal ligation can cause changes in morphology (Mills: Histology for Pathologists, 5th Edition, 2019)
- Molecular and transcriptional alterations occur throughout the menstrual cycle and after menopause (medRxiv 2023 Nov 23 [Preprint], Cell Rep 2022;41:111838)
- Immune system (Int J Gynecol Pathol 2014;33:581)
- Prevents infection
- Helps develop tolerance to the zygote
Diagrams / tables
Clinical features
- Fallopian tubes can be evaluated with hysterosalpingography (Fertil Steril 2022;118:19)
- Dye is injected into the uterus that can be visualized using Xray
- Flow of the dye is visualized to assess the patency of the fallopian tubes
Laboratory
- CA125 can be used to screen for ovarian / fallopian tube cancer (J Ovarian Res 2019;12:28)
- More useful in postmenopausal women
- False positive results are associated with endometriosis, pelvic inflammatory disease and uterine fibroids
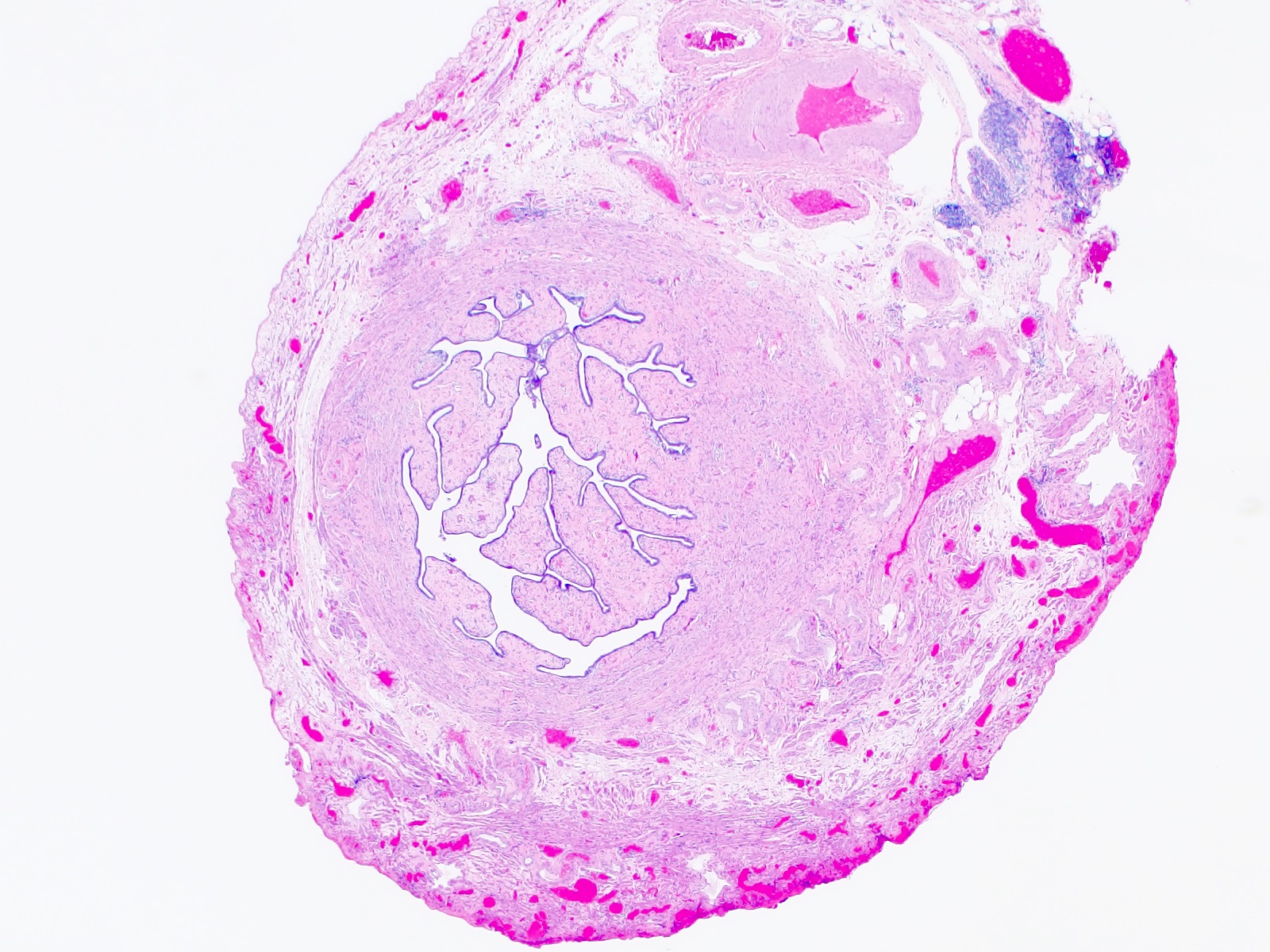
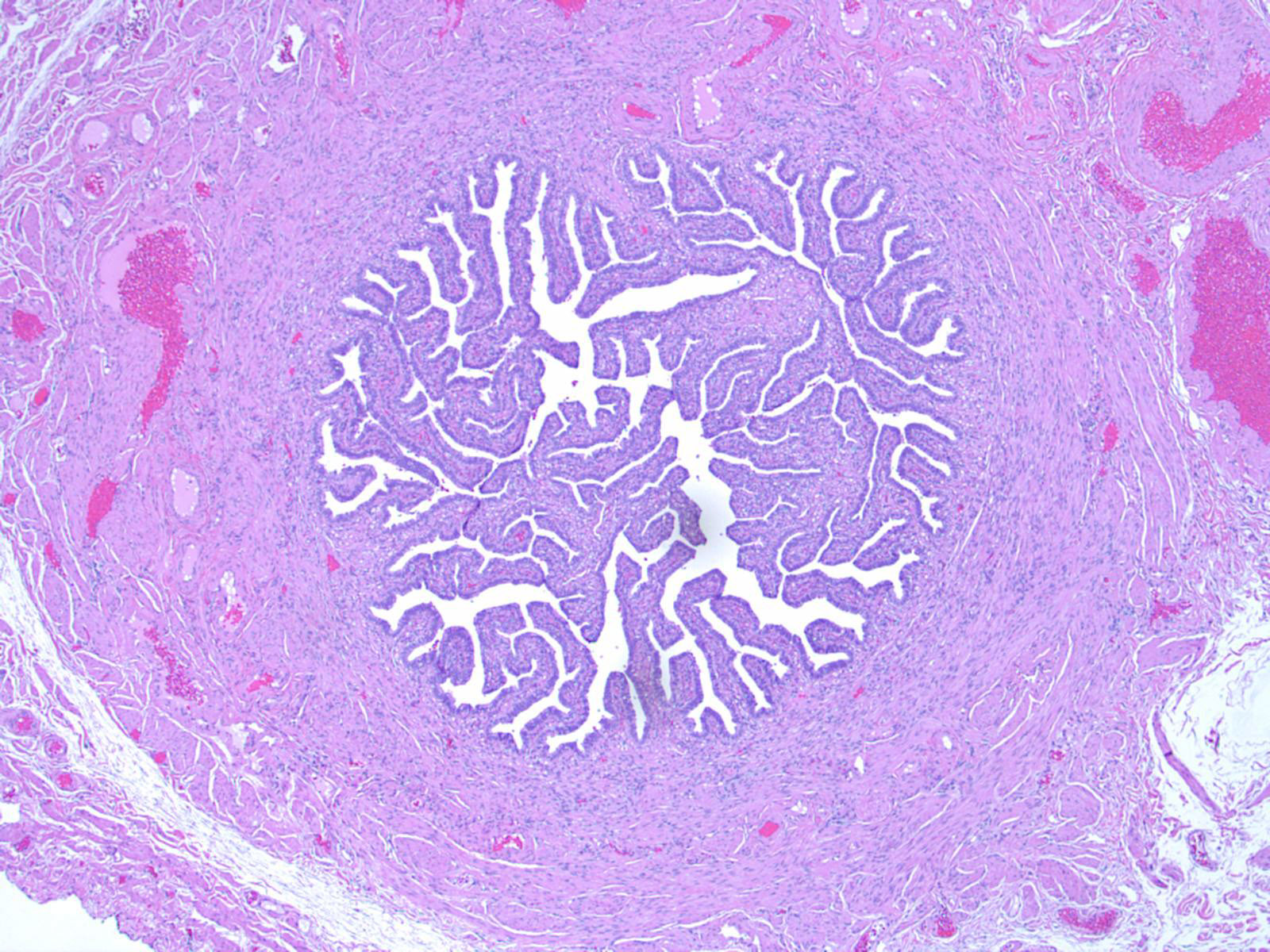
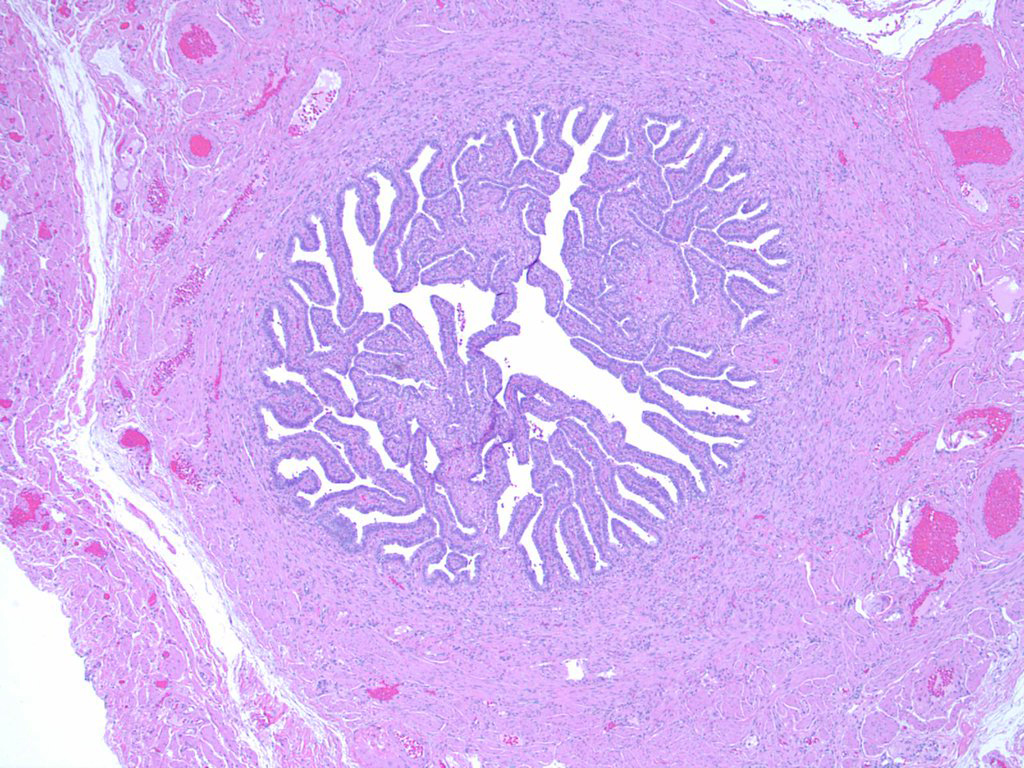
Gross description
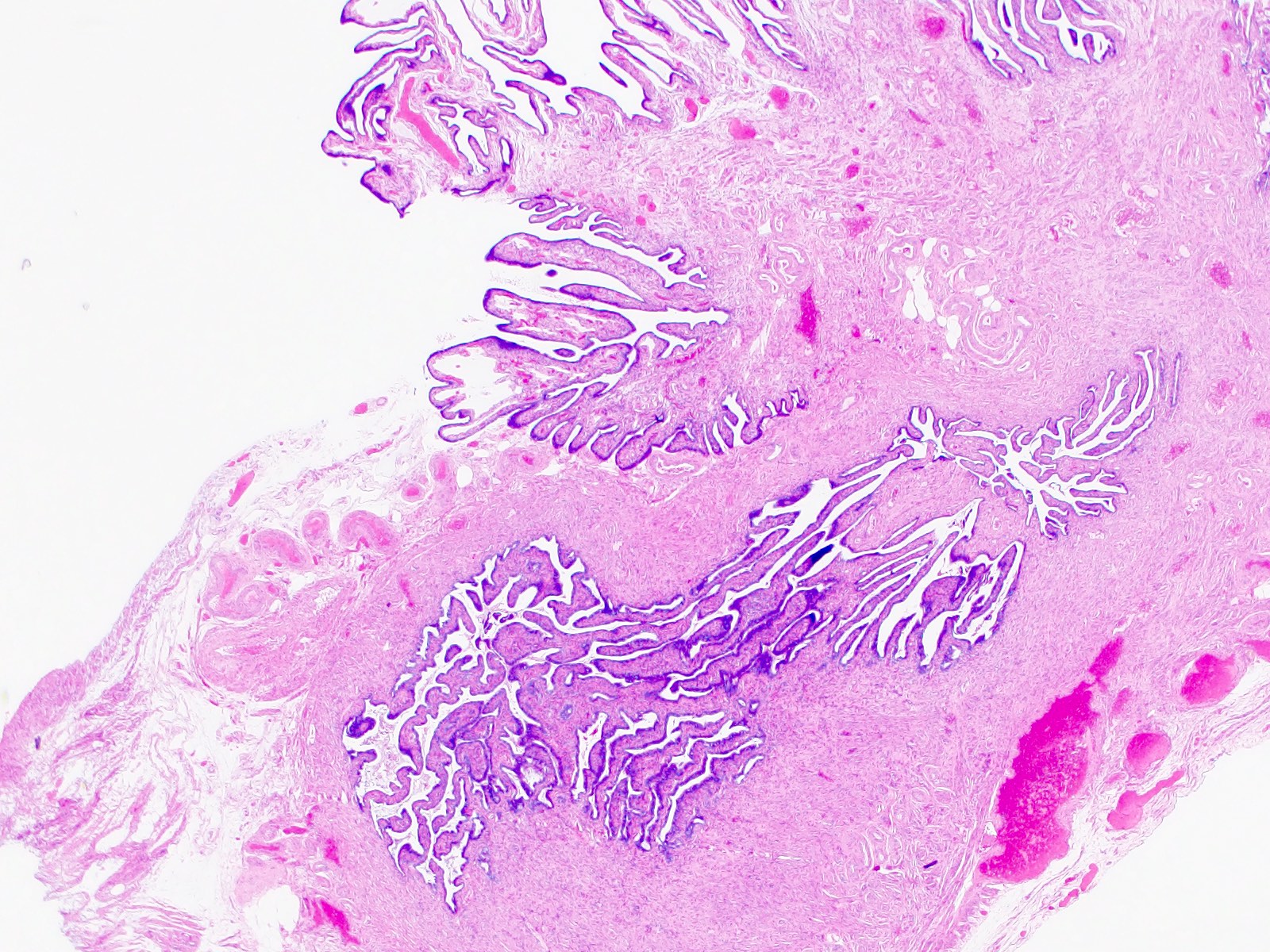
- Bilateral hollow, tubular structures, measuring 8 - 12 cm in length and 0.5 - 1.2 cm in diameter
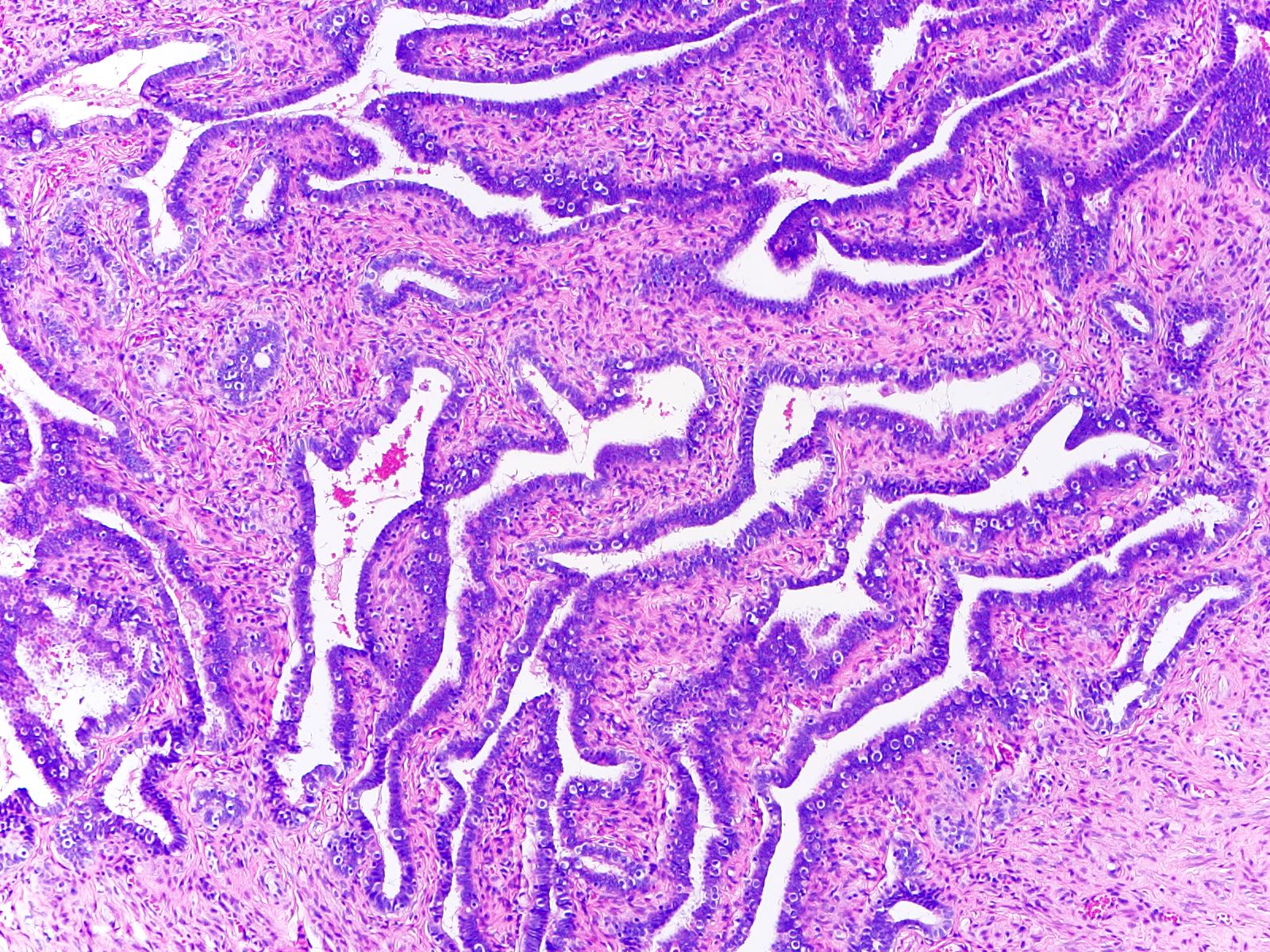
- Lined by a single layer of mucosal epithelium with many folds (plicae), which are most obvious in the ampulla where they subsequently merge with fimbriae
- Extend laterally from the posterior superior uterine fundus and lead to the ovaries
- Connected to broad ligament by mesosalpinx (double fold of peritoneum), to uterine cornu by utero-ovarian ligament and to lateral pelvic sidewall by infundibulopelvic (suspensory) ligament
- Arterial supply is from branches of uterine and ovarian arteries, located within mesosalpinx
- Nerve supply from both sympathetic and parasympathetic fibers
- Sensory fibers run from T11 - T12 and L1
- Lymphatic drainage to para-aortic, internal iliac, external iliac, common iliac and inguinal lymph nodes
- Segments
- Intramural (within wall of uterus)
- Isthmus (thick walled, narrower opening, ~2 cm in length)
- Ampulla (thin walled, major portion, typical site of fertilization)
- Infundibulum (trumpet shaped end lined by fimbriae, attaches to ovary)
- Tubal ostium is an opening to the peritoneal cavity
- Uterotubal junction is an entrance to the uterine cavity
- Reference: StatPearls: Anatomy, Abdomen and Pelvis - Fallopian Tube [Accessed 18 April 2024]
Frozen section description
- Fallopian tube specimen is most often received for frozen section as a part of a salpingo-oophorectomy specimen (Hui: Atlas of Intraoperative Frozen Section Diagnosis in Gynecologic Pathology, 1st Edition, 2015)
- Frozen section is not usually performed on grossly identifiable and unremarkable fallopian tubes; however, adherent fallopian tube tissue may occasionally be submitted for intraoperative consultation
- Morphologic features are consistent with normal fallopian tube as described below
Microscopic (histologic) description
Embryologic histology
Adult histology
- Third week
- Following migration of primordial germ cells from yolk sac, genital ridge forms from intermediate mesoderm and cloaca forms
- Fourth week
- Müllerian (paramesonephric) ducts form from coelomic epithelium invaginating ventrolaterally into Wolffian (mesonephric) duct and genital mesentery
- This site of invagination later becomes the tubal ostium in which the fimbriae develop and septation of the cloaca occurs
- Fifth to eighth weeks
- Unfused cephalic part of Müllerian ducts form fallopian tube
- Fused part forms uterus and upper vagina
- In a female fetus (or male without functioning testes) (Bhatnagar: Essentials of Human Embryology, 3rd Edition, 2000)
- Müllerian structures persist and Wolffian (mesonephric) duct regresses; vestiges may persist as epithelial inclusions
- Development is affected by clomiphene, tamoxifen and to a lesser extent, diethylstilbestrol (DES) (Hum Pathol 1987;18:1132, Hum Pathol 1982;13:190)
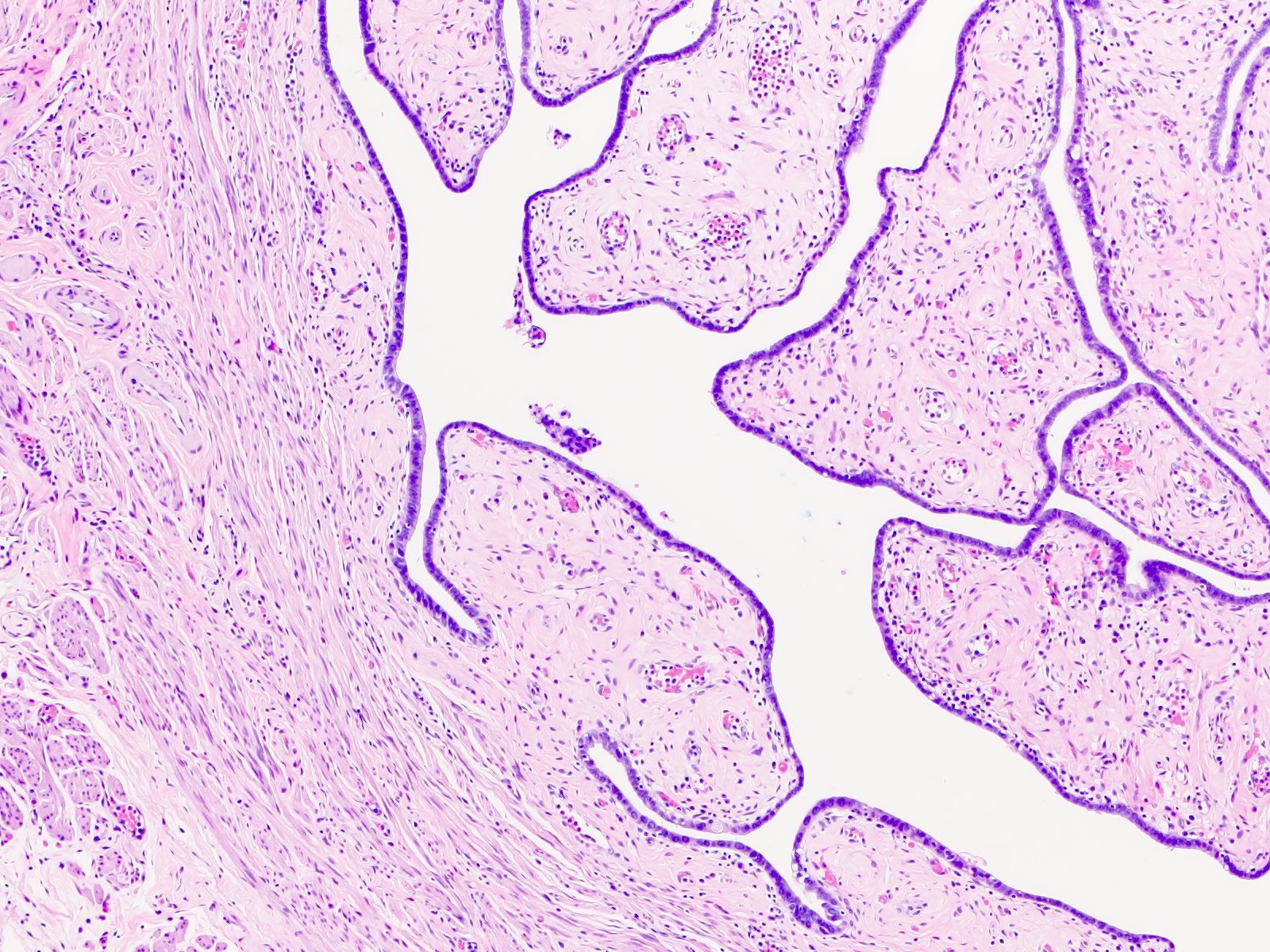
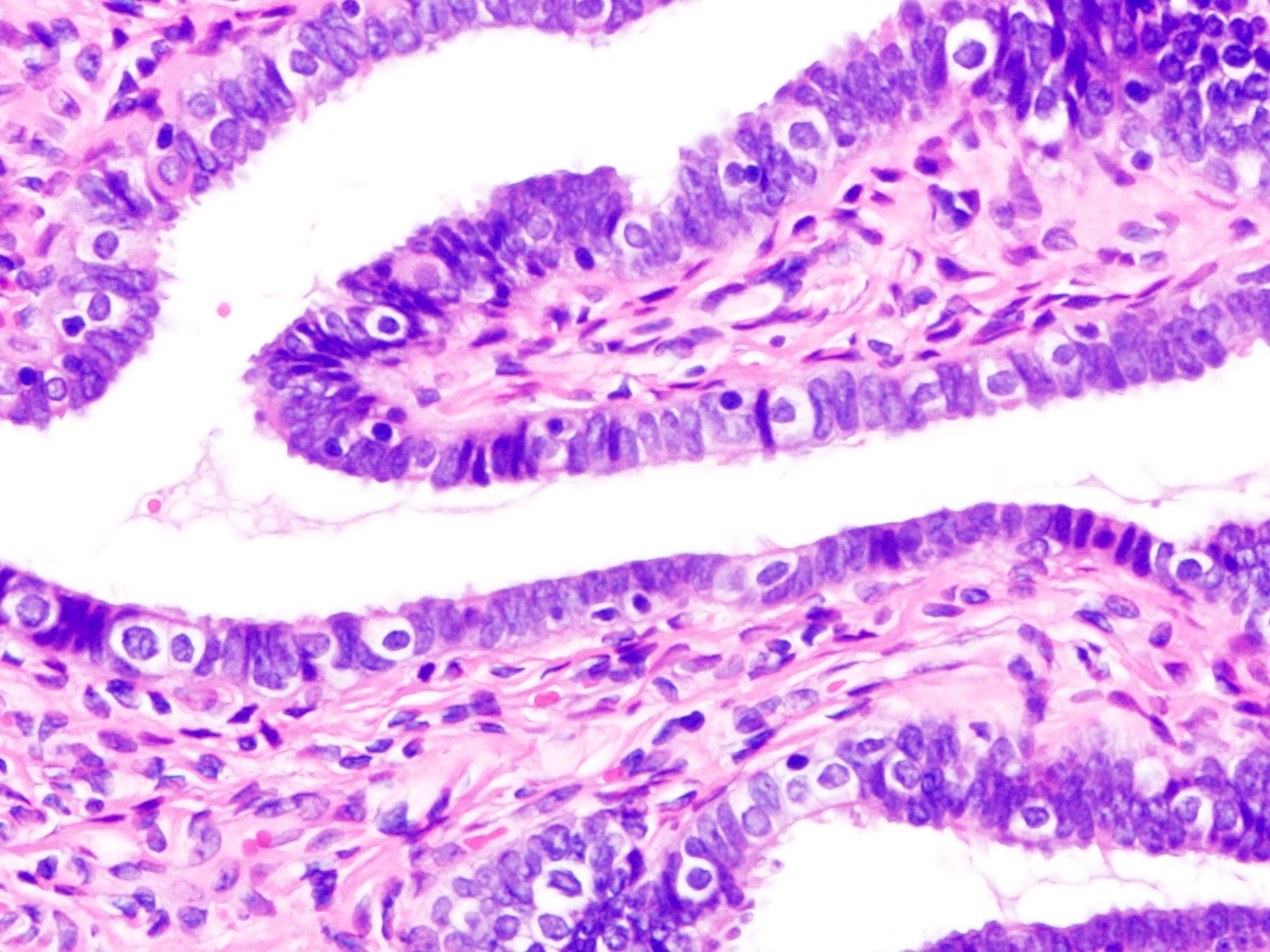
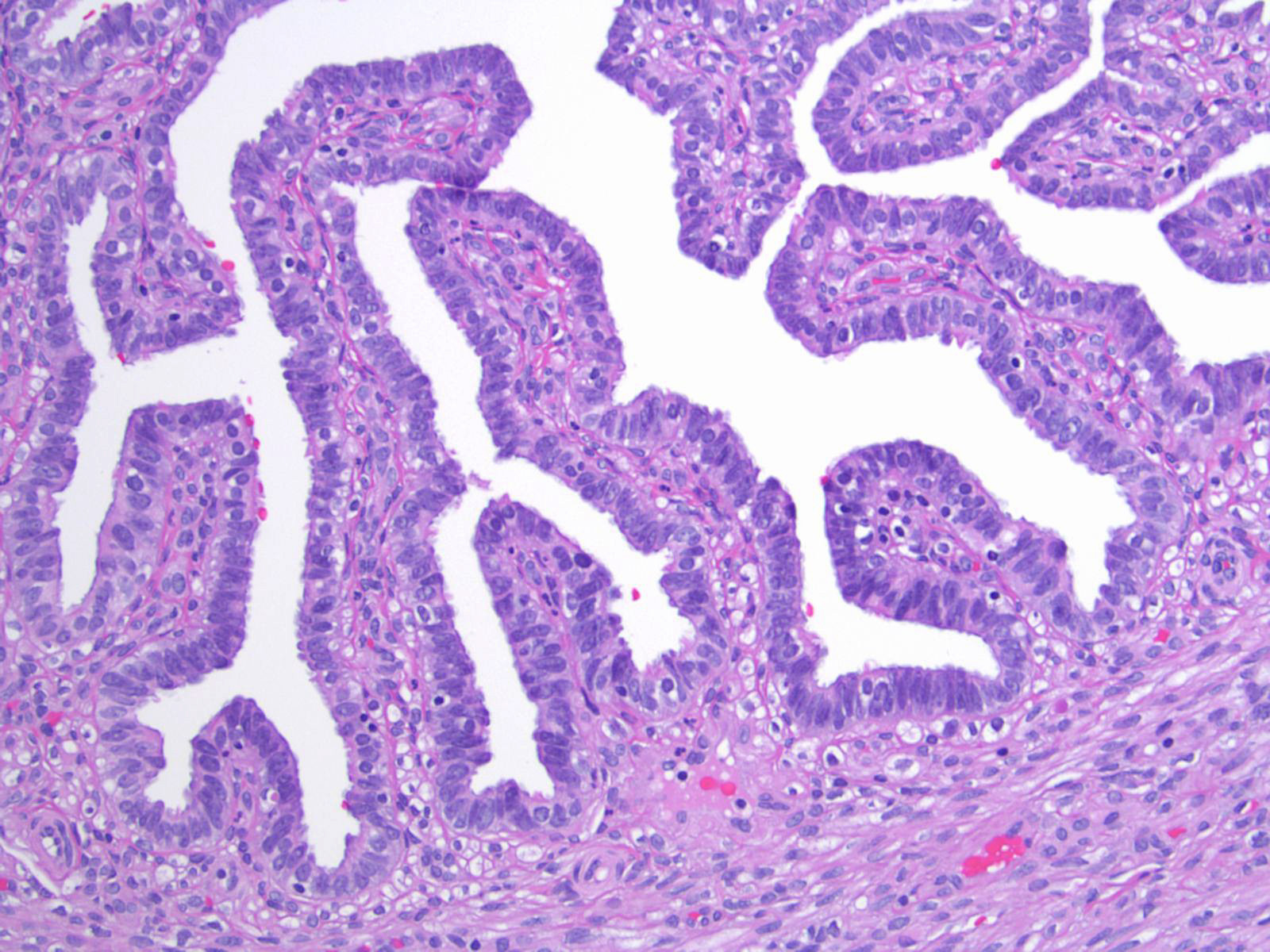
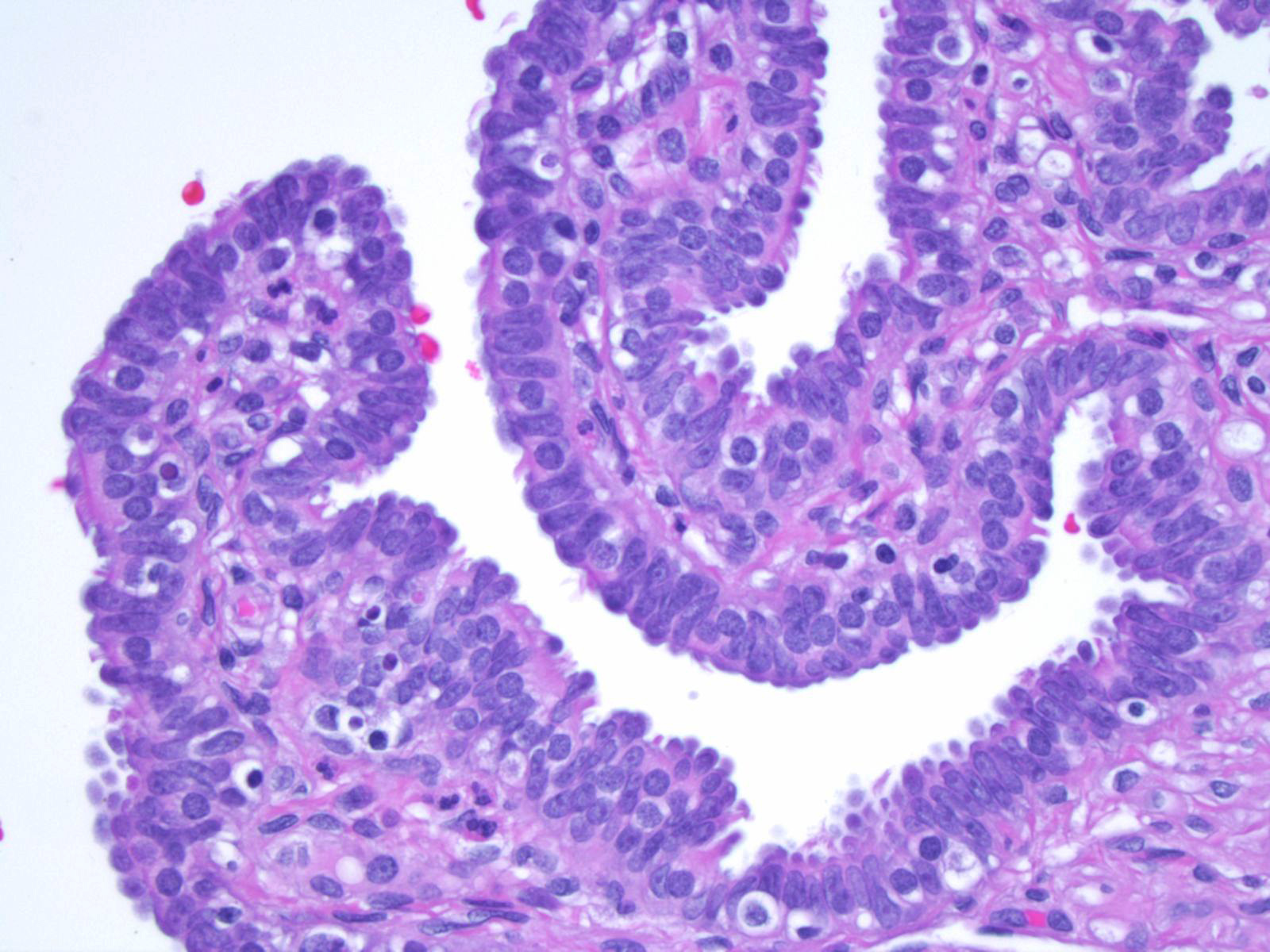
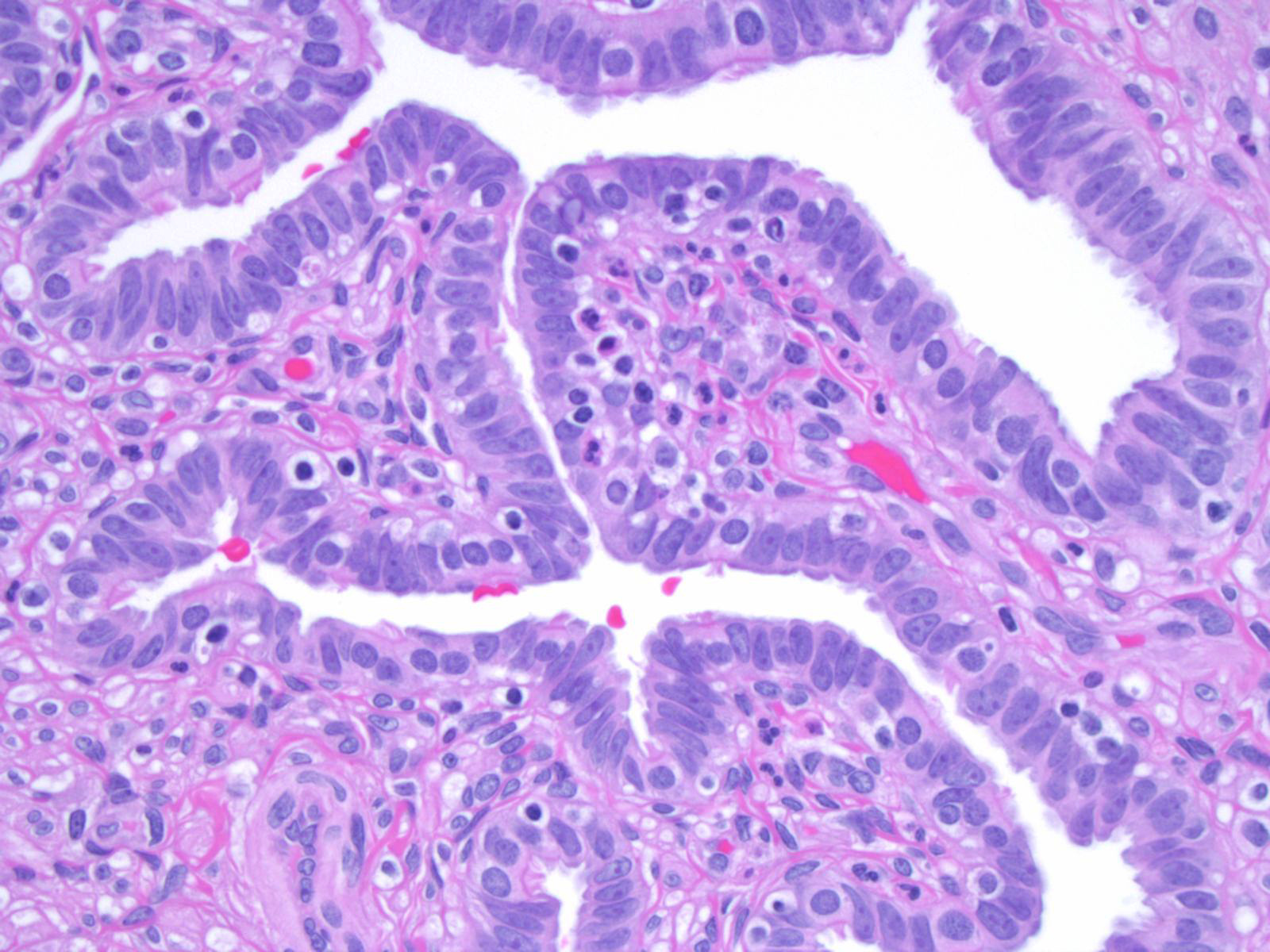
Adult histology
- Fallopian tube wall is composed of mucosal, muscular and serosal layers
- Mucosa comprises luminal epithelium and underlying lamina propria (stroma)
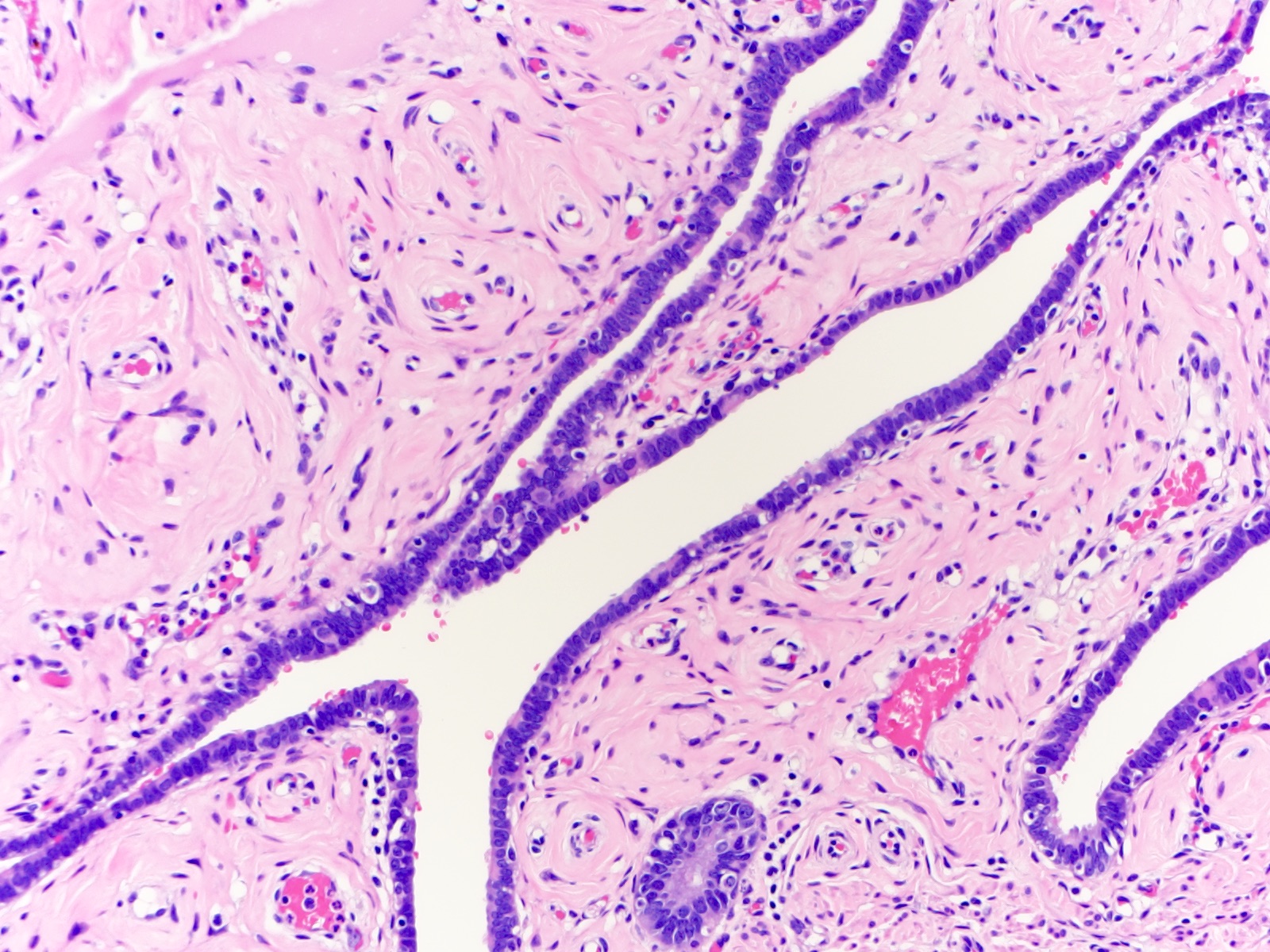
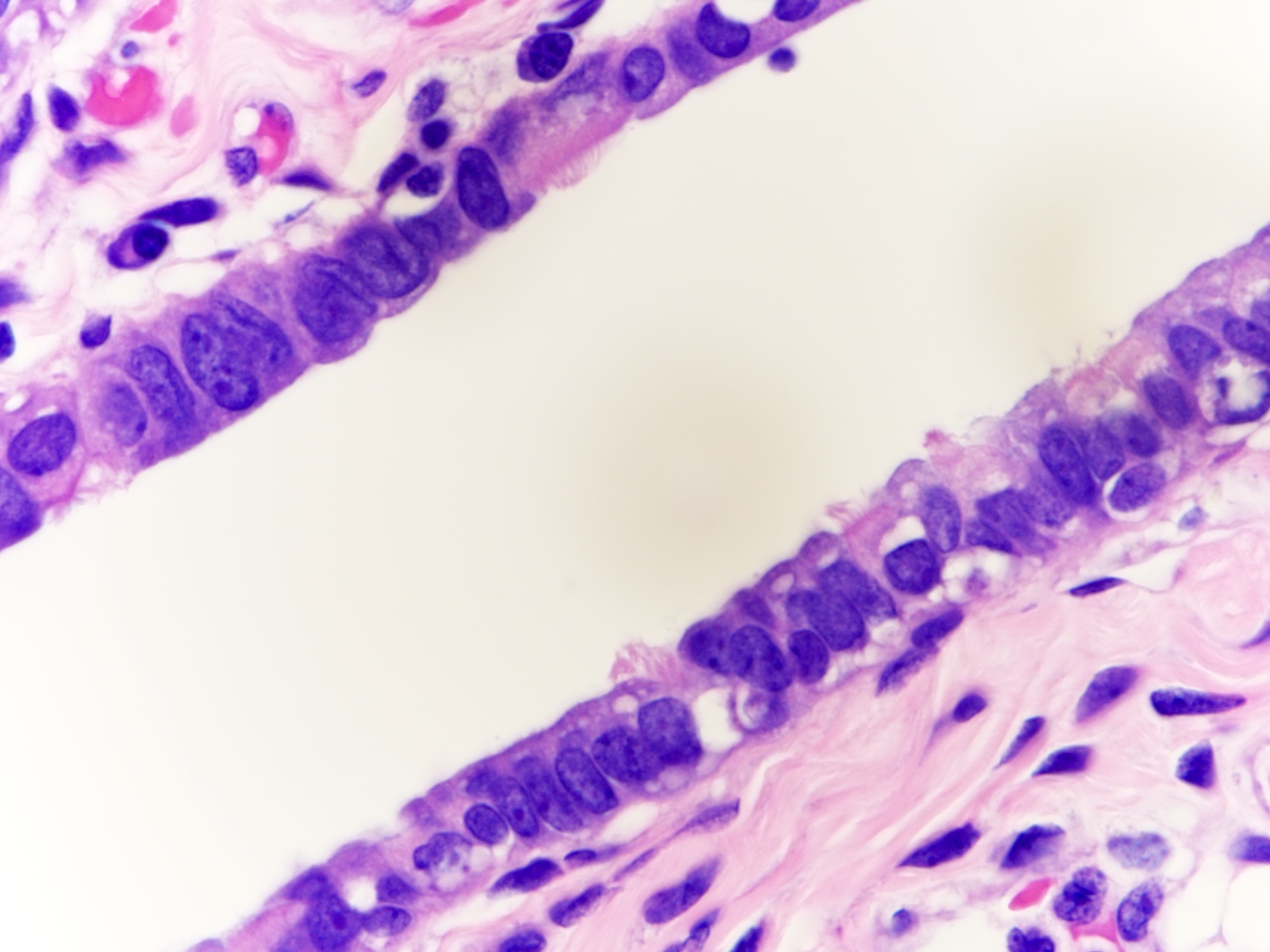
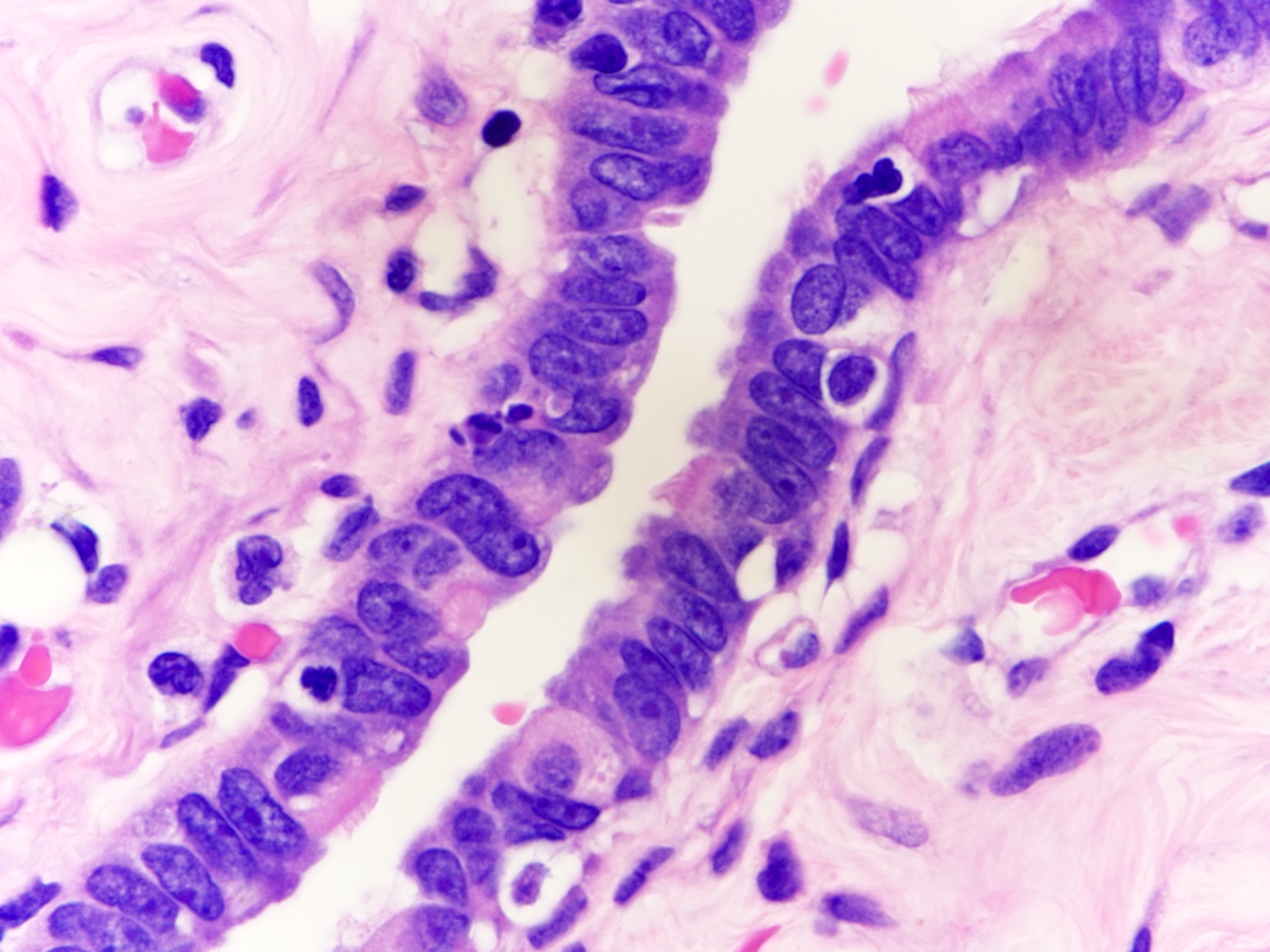
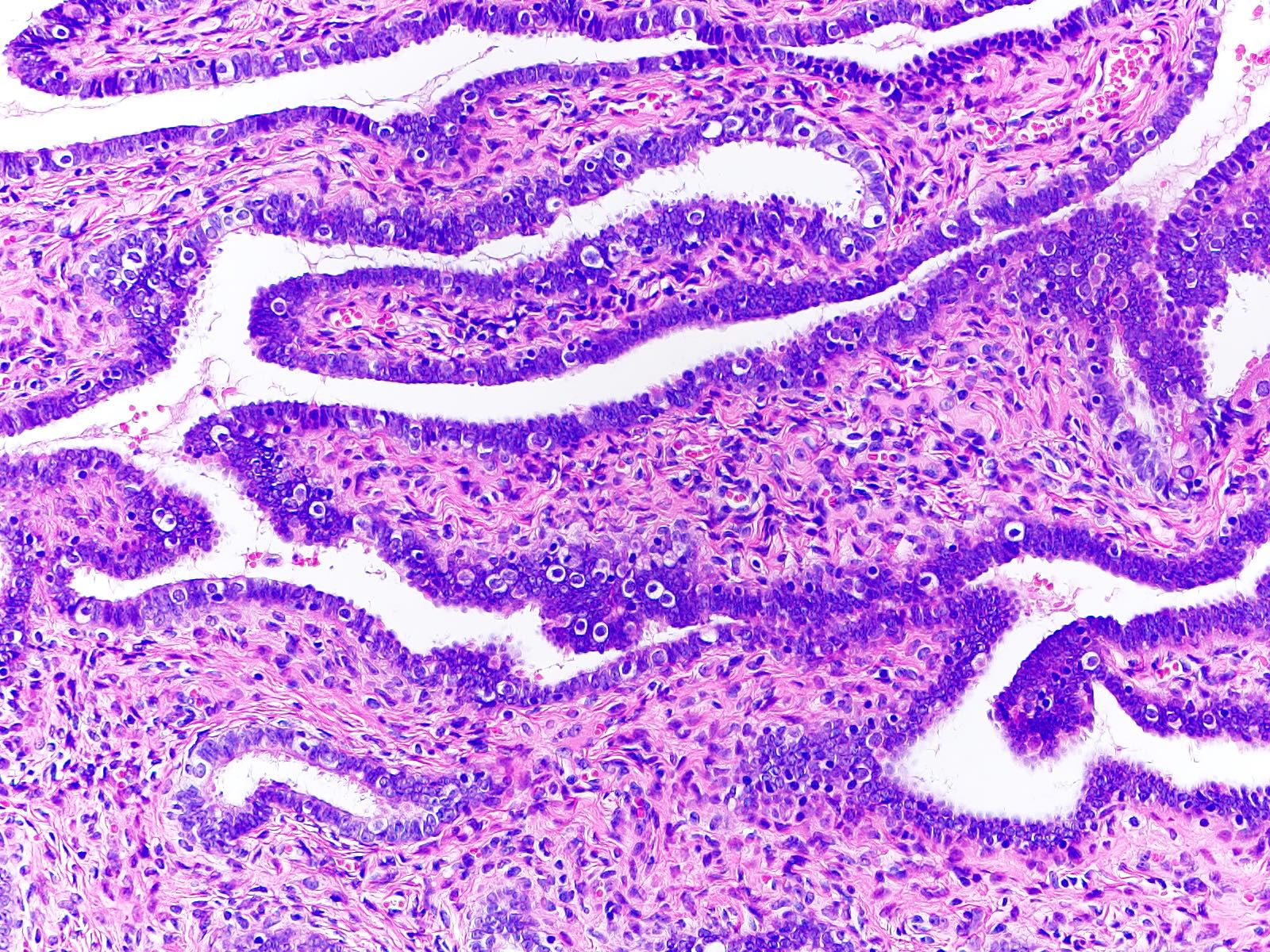
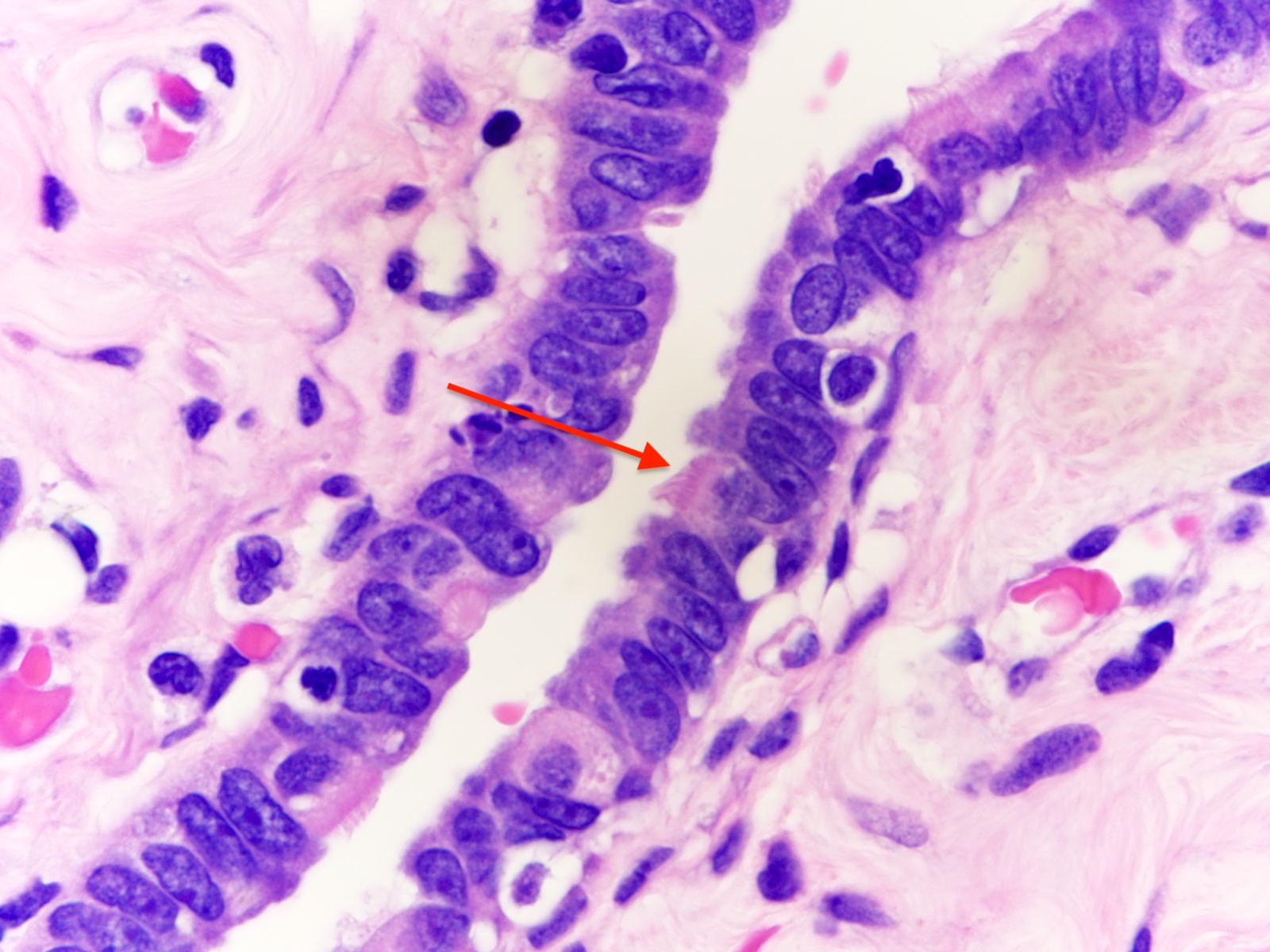
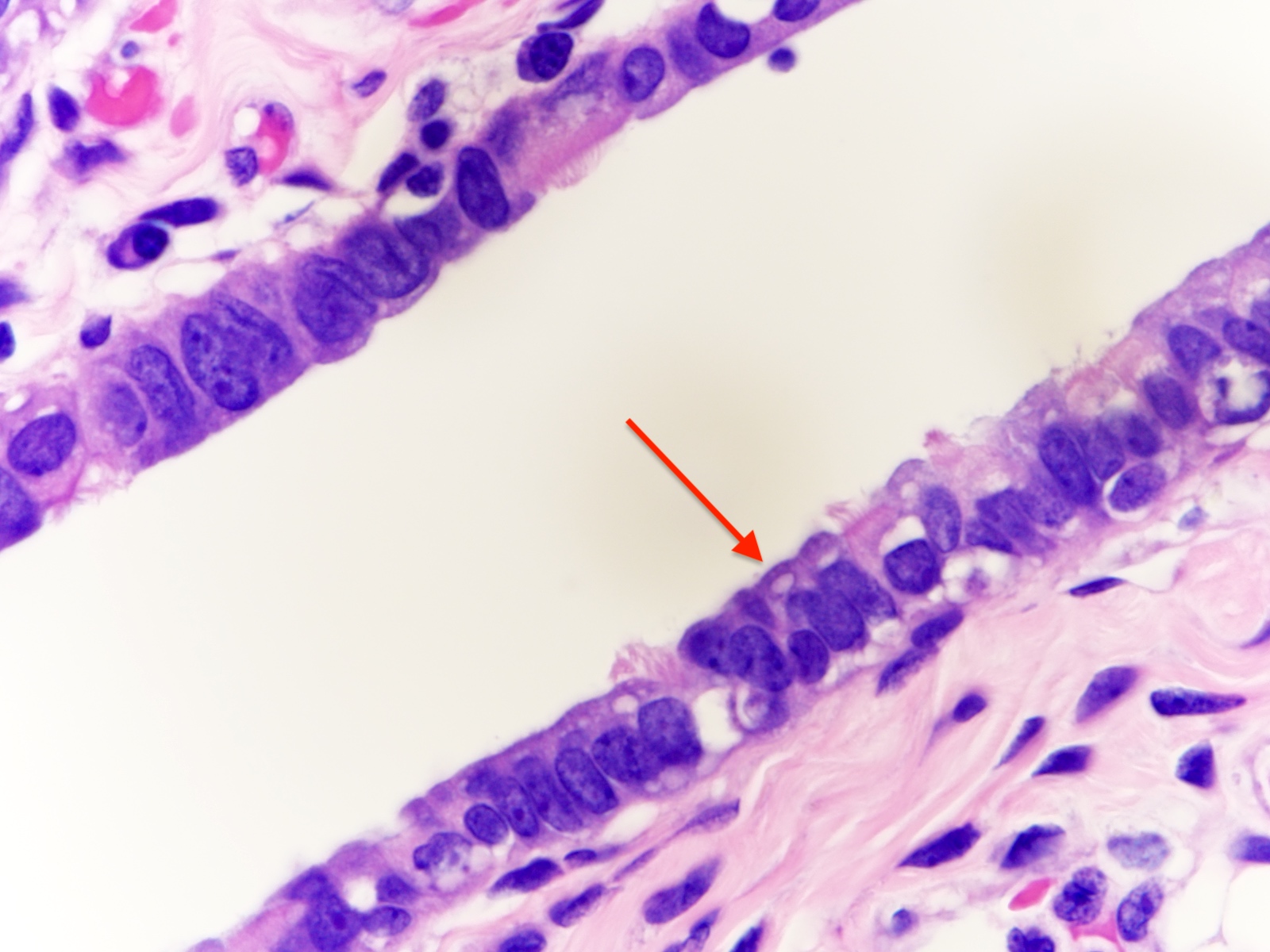
- Luminal epithelium consists of the following cells (Mills: Histology for Pathologists, 5th Edition, 2019)
- Ciliated columnar cells (~25%)
- Most abundant in infundibulum and ampulla
- Estrogen increases production of cilia
- Most often seen at the apex of mucosal folds
- Most common at the ovarian end of the tube, especially in fimbriae
- Most common during midcycle and decrease to the minimum number at menstruation
- Decrease during gestation
- Secretory cells (~60%)
- Nonciliated, containing apical granules and producing tubular fluid
- Exhibit ovoid, dense nuclei
- Most common at the proximal segment of the fallopian tube
- Increase in number in response to progesterone
- Height and secretory activity increase in response to estrogen
- Menstruation cycle changes cell height and appearance
- May exhibit nonmotile primary cilia
- Contain sensory organelles
- React to cilia mediated stimuli and are fully capable of affecting cilia mediated signaling pathways
- Lost in serous tubal intraepithelial carcinoma (Int J Gynecol Cancer 2018;28:1535)
- Peg (intercalated) cells (< 10%)
- Exhibit thin dense nuclei and little cytoplasm
- Stage in the cyclic variation during the menstrual cycle of the secretory cells
- Basal cells (Dev Cell 2022;57:914)
- Exhibit round nuclei and a cytoplasmic ring
- Ciliated columnar cells (~25%)
- Lamina propria (stroma) (Dev Cell 2022;57:914)
- Stromal cells resembling fibroblasts, surrounded by dense reticulin network
- Blood vessels
- Possibly Cajal-like cells (Dev Cell 2022;57:914)
- Muscle layer comprising 3 sublayers
- Innermost (obliquely arranged)
- Middle (circular)
- Outermost (longitudinal, extending into fimbriae)
- Serosal layer
- Lined by mesothelium of visceral peritoneum
- Often contains Walthard rests with transitional type epithelium
- Immune cells
- Lymphocytes may be observed in epithelium, lamina propria and muscular wall (Int J Gynecol Pathol 2014;33:581)
- Occasional lymphoid follicles may be seen
- Other immune cells include CD163+ macrophages, CD11c+ dendritic cells, CD8+ T cells and a minor populations CD56+ NK cells, CD4+ T helpers, CD20+ B cells, TCRγδ+ T cells, CD207+ (langerin) Langerhans cells, mast cells (Int J Gynecol Pathol 2014;33:581, Dev Cell 2022;57:914)
- Distribution varies according to menopausal status; T helper and B cells are more common in postmenopausal women, while macrophages are more abundant in premenopausal women (Int J Gynecol Pathol 2014;33:581)
- Play a role in cancer immune surveillance (Int J Gynecol Pathol 2014;33:581)
- Normal histologic variations
- Intramuscular edema in 12.5% of specimens, most frequently postpartum
- Plical fibrosis (35.5%), epithelial vacuolization (6.6%) and epithelial tufting / stratification (3.5%) correlated with increased patient age (Arch Pathol Lab Med 2002;126:951)
- Rare mitotic figures
- Metaplasia, including mucinous, endometrioid or transitional cell (Walthard rests)
Microscopic (histologic) images
Contributed by Brandon D. Metcalf, M.D. and Nicole D. Riddle, M.D.
Cytology description
- Ciliated cells in clustered arrangements with round or oval nuclei, hyperchromatic chromatin and mild nuclear membrane irregularity
- Honeycomb / monolayered sheets
- Spindled appearance is not characteristic (Cytojournal 2018;15:28)
- Utility of minimally invasive laparoscopic screening of fallopian tubes in patients at high risk for high grade serous carcinoma is being investigated (J Vis Exp 2017;125:55887, J Am Soc Cytopathol 2023;12:368)
Positive stains
- Ciliated cells (Dev Cell 2022;57:914, Stem Cells 2012;30:2487, Cancer Cell 2020;37:226)
- FOXJ1
- CAPS
- B tubulin
- TUBB4
- CCdC17
- CCDC78
- Secretory cells (Dev Cell 2022;57:914, Stem Cells 2012;30:2487)
- Peg cells (Dev Cell 2022;57:914)
- Basal cells (Dev Cell 2022;57:914)
- Stromal cells
- In postmenopausal fallopian tubes (Cell Rep 2022;41:111838)
- PAX8 in secretory cells
- FOXJ1, adiponectin, estrogen, insulin and oxytocin in ciliated cells (Cell Rep 2022;41:111838)
- EpCAM mainly in the ampulla and fimbriae (Cell Rep 2022;41:111838)
- AR, ER and PR in stromal cells (Cell Rep 2022;41:111838)
- Dual polyglut tubulin / DNAH5 stain
- Distinguishes motile cilia from primary cilia (Int J Gynecol Cancer 2018;28:1535)
Electron microscopy description
- Variations during menstrual cycle (Physiol Res 2022;71:S137)
- Postmenstrual
- Ciliation is separated by fields of nonciliated flat cells with indistinct cell borders
- Preovulatory epithelium
- Swelling of nonciliated polyhedral cells
- Still maintains overall distribution of ciliated and nonciliated cells.
- Clusters of nonciliated cells bulge up to the height of the cilia tips
- Imparts a more uniform appearance of the surface epithelium
- Ovulatory epithelium
- Nonciliated cells show disrupted membranes after releasing their secretions
- Premenstrual period
- Nonciliated cells
- Regress below the level of the ciliary tips
- Become flattened
- Regain their distinct boundaries
- Clear boundaries: classic feature for differentiating the premenstrual / luteal phase from the postmenstrual phase
- Ciliated cells
- May cluster in elongated fields called tracts
- May form small ciliated clumps
- Nonciliated cells
- Postmenstrual
- Menopausal (Physiol Res 2022;71:S137)
- Surface epithelium is similar to the luteal phase of premenopausal women
- Mucosal folds with tracts of ciliated cells alternate with stretched clumps of ciliated cells
- Postmenopausal (Physiol Res 2022;71:S137)
- More nonciliated cells
- Frequently turn into dome shaped giant cells
- Observe delicate microplicae-like structures (Histol Histopathol 2006;21:219)
- Gradual shortening of microvilli
- More nonciliated cells
Electron microscopy images
Videos
Shotgun histology: fallopian tube
UB medical: oviduct histology
Additional references
Board review style question #1
Board review style answer #1
B. Ciliated cell and movement of the egg. The ciliated cell contains motile cilia, which beat in a wave-like fashion to move the egg. Answer D is incorrect because secretory cells are not responsible for the movement of the egg. Answer A is incorrect because basal cells do not produce tubal fluid and are found at the basal aspect of the epithelium. Answer C is incorrect because ciliated cells do not produce tubal fluid.
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Board review style question #2
Board review style answer #2
D. PAX8 stains secretory cells. Answers A and B are incorrect because CD44 and EpCAM stain peg cells. Answer C is incorrect because FOXJ1 stains ciliated cells.
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report
Comment Here
Reference: Fallopian tubes & broad ligament - Anatomy, histology, embryology & features to report