Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zoroquiain P. Pterygium. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyepterygium.html. Accessed March 31st, 2025.
Definition / general
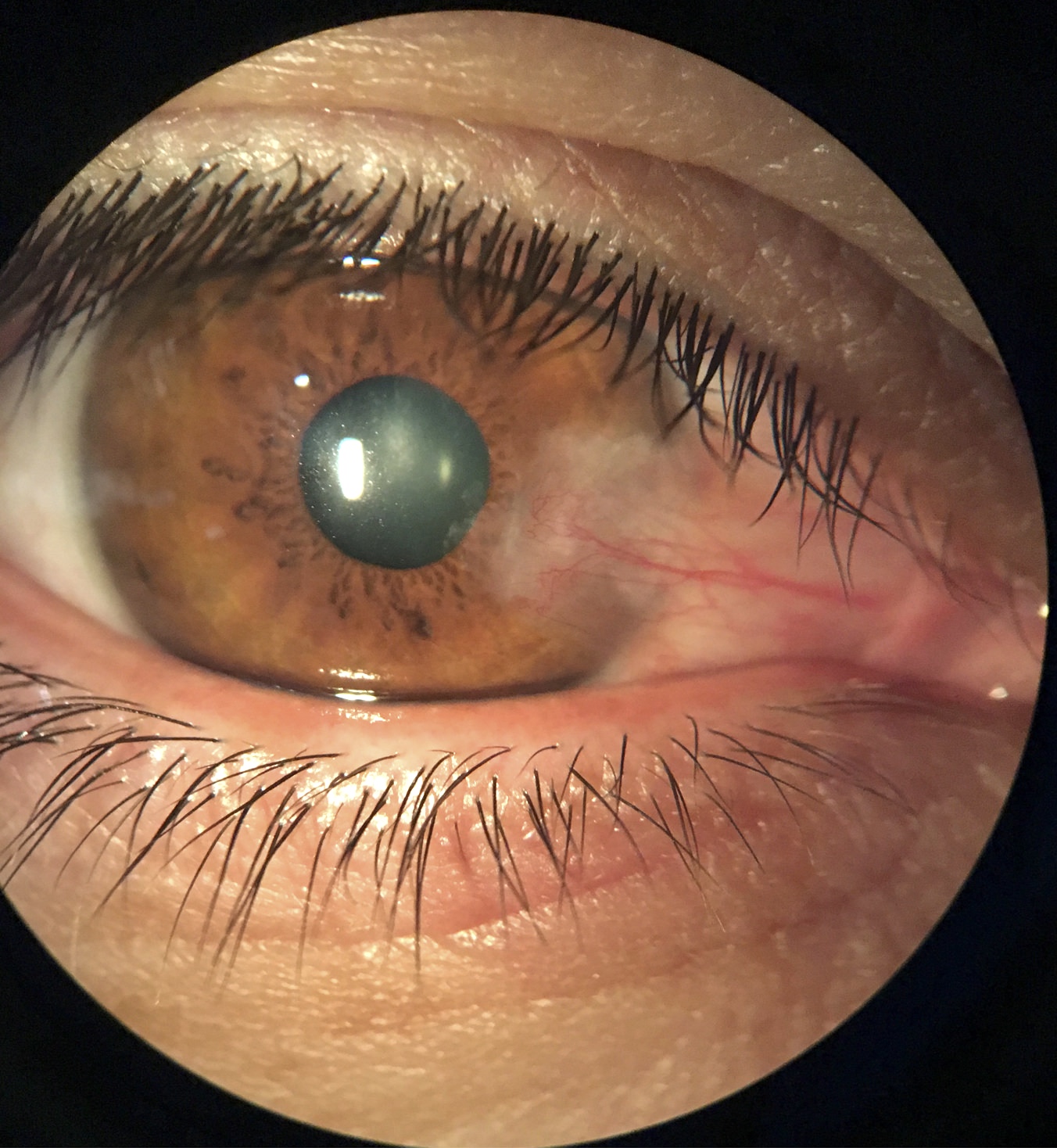
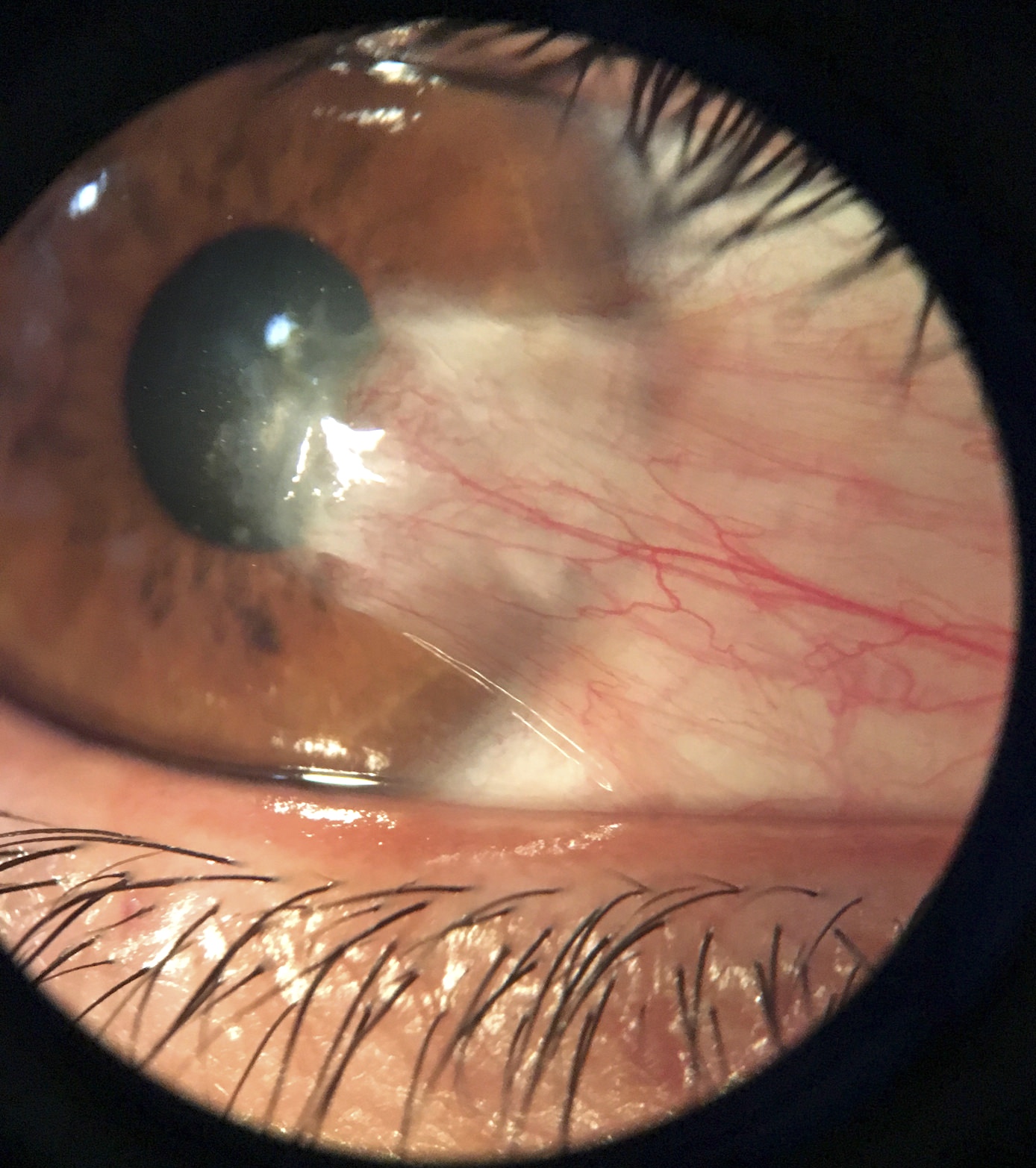
- Frequent, degenerative ocular surface lesion, characterized by invasion of the cornea by a fibrovascular tissue originating from the bulbar conjunctiva (Surv Ophthalmol 2018;63:719)
- Most frequent in the interpalpebral area, nasal side
- Thought to be UV light associated; not associated with human papillomavirus (HPV) (Br J Ophthalmol 200;91:1016)
- Develops from limbal epithelial progenitors; may be a stem cell disorder with possible premalignant features (Am J Pathol 2011;178:817)
Essential features
- Frequent, degenerative ocular surface lesion
- Similar to pinguecula but with corneal infiltration
- UV related
- Can masquerade as a neoplastic process
- Fibrovascular connective tissue that migrates to cornea
ICD coding
- ICD-10: H11.0 - pterygium of eye
Epidemiology
- Prevalence of 12%, with a geographic variation of 53% in China and 0.07% in Saudi Arabia (Surv Ophthalmol 2018;63:719)
Sites
- Corneoconjunctival limbus and cornea
Pathophysiology
- There are many hypotheses but its pathogenesis is still unknown
- Environmental factors have been suggested, due to high prevalence in hot and dry climates
- UV radiation has been proposed, due to the similarity with the histopathology of solar elastosis
- Other proposed hypotheses are corneal stem cell deficiency, inflammation, angiogenic disregulation, ultraviolet albedo (reflected, scattered light) in the anterior eye (Br J Ophthalmol 1993;77:734)
Etiology
- Older age, M > F, rurality, outdoor activities, prolonged exposure to UV light and alcohol consumption are known risk factors (Surv Ophthalmol 2018;63:719)
Clinical features
- Causes significant changes in corneal refractive status that increases with grade of pterygia (Indian J Ophthalmol 2007;55:383)
- High prevalence (18%) in those older than 40 living at high altitude in Mongolia (Eye (Lond) 2009;23:421)
- Clinically, may resemble ocular surface squamous neoplasia or melanoma
- Not related to multiple pterygium (webbing) syndrome (Am J Hum Genet 2006;79:390)
- Recurs in ~15% of patients and may masquerade as a neoplastic process
Diagnosis
- Diagnosis is performed when the typical clinical appearance is observed
Prognostic factors
- Recurrence rate is lower than 1/1,000 surgical procedures
Case reports
- 33 year old woman with growth in her eye (Am Fam Physician 2018;97:337)
- 40 year old man with mitomycin C excision and adjuvant extracellular matrix placement (Digit J Ophthalmol 2017;23:15)
- 60 year old man with corneal perforation associated with dellen after excision (BMJ Case Rep 2015;2015:bcr2015213319)
- 65 year old man with recurrent lesion treated with small incision lenticule extraction (J Int Med Res 2018;46:2474)
Treatment
- Treatment for cosmetic reasons, visual impairment, recurrent inflammation, mild irritation
- Medical therapy:
- Symptoms can be alleviated using over the counter vasoconstrictor drops and lubricating agents such as ointments or drops
- Corneal extension should be followed to determine the growth ratio to the visual axis
- Surgery:
- Excision with adjunctive therapies (radiotherapy, mitomycin C or fluorouracil [5FU]): low recurrence and fast but can have complication secondary to the use of the adjunctive agents
- Conjunctival flap or graft: considered the gold standard with recurrence as low as 1/1,000 with autografts; it is a lengthier procedure and technically more difficult
- References: Ther Adv Ophthalmol 2021;13:25158414211020152, J Curr Ophthalmol 2022;33:367
Clinical images
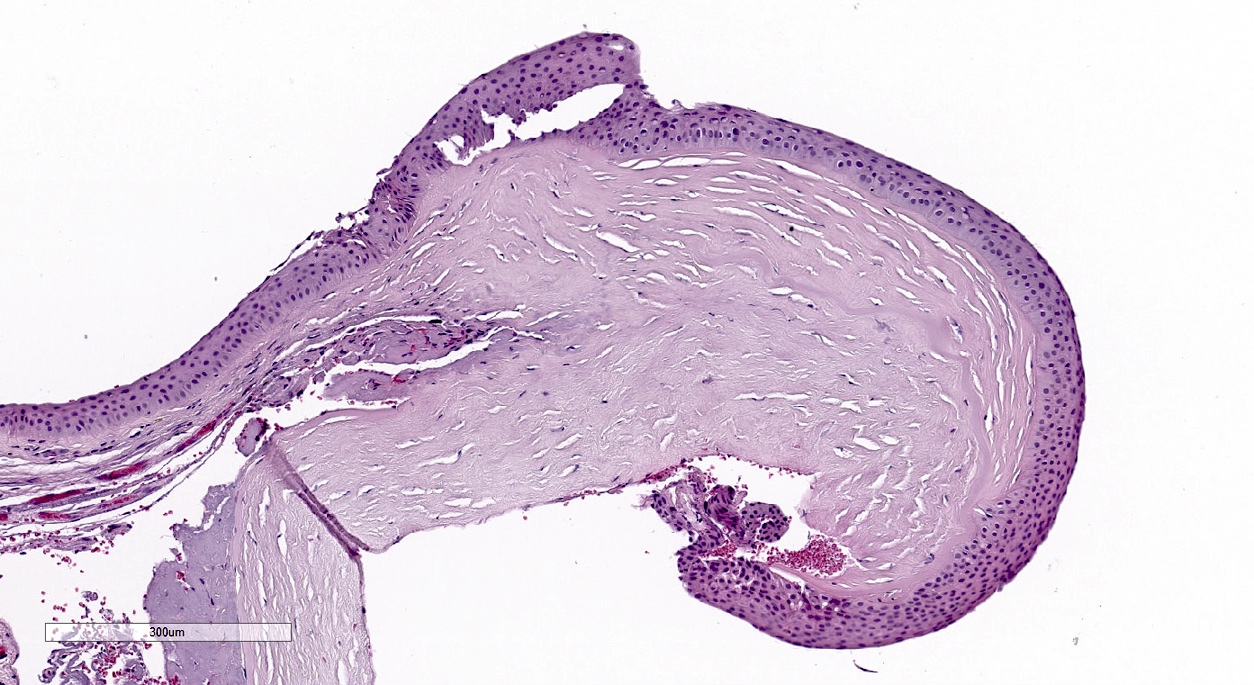
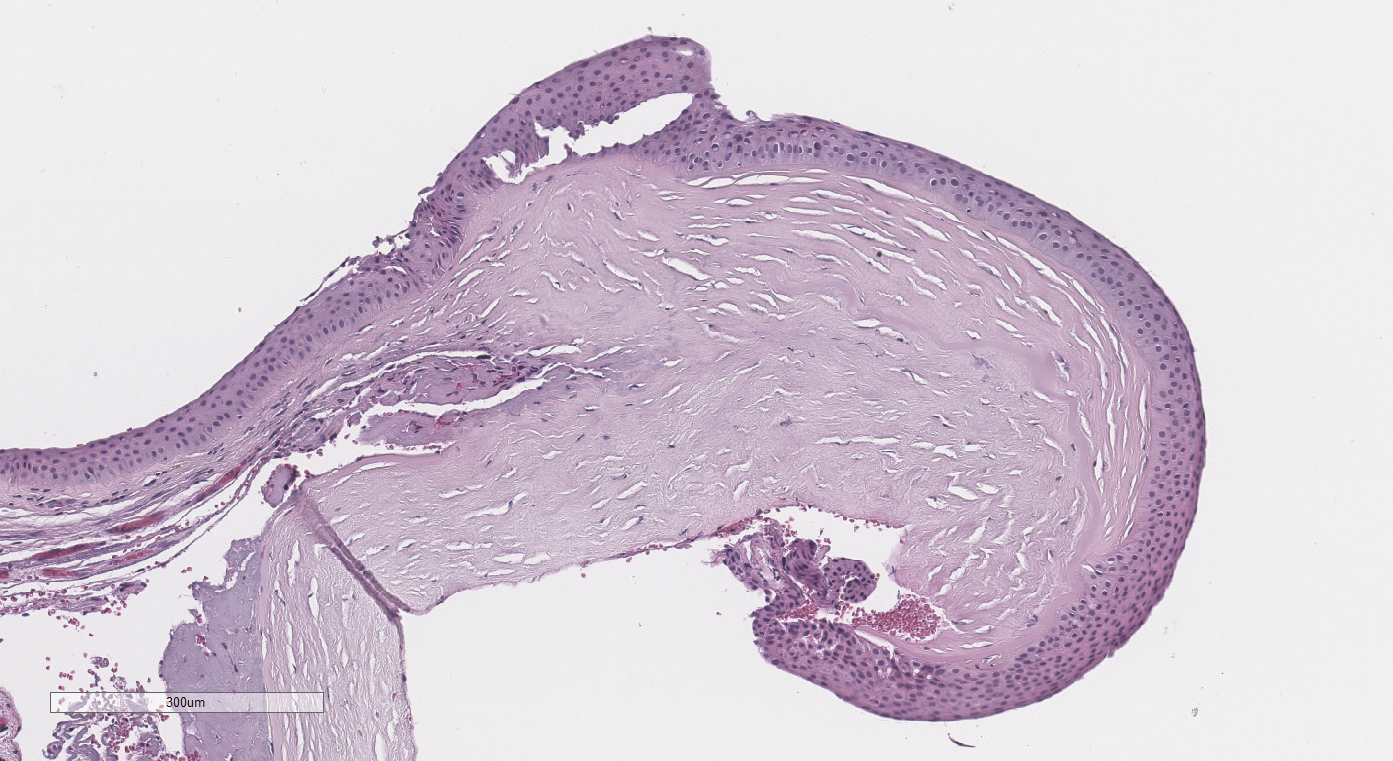
Gross description
- Fleshy
- Grossing tip: always bisect the tissue from the conjunctiva to the cornea
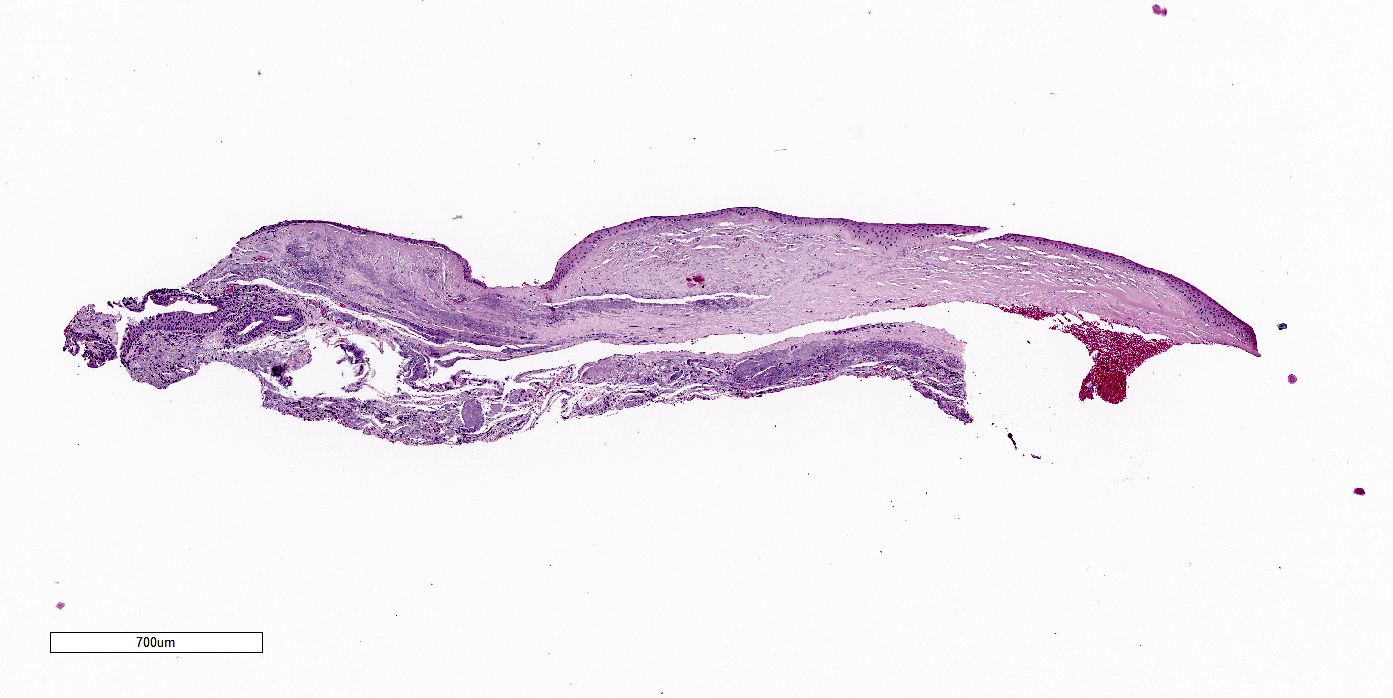
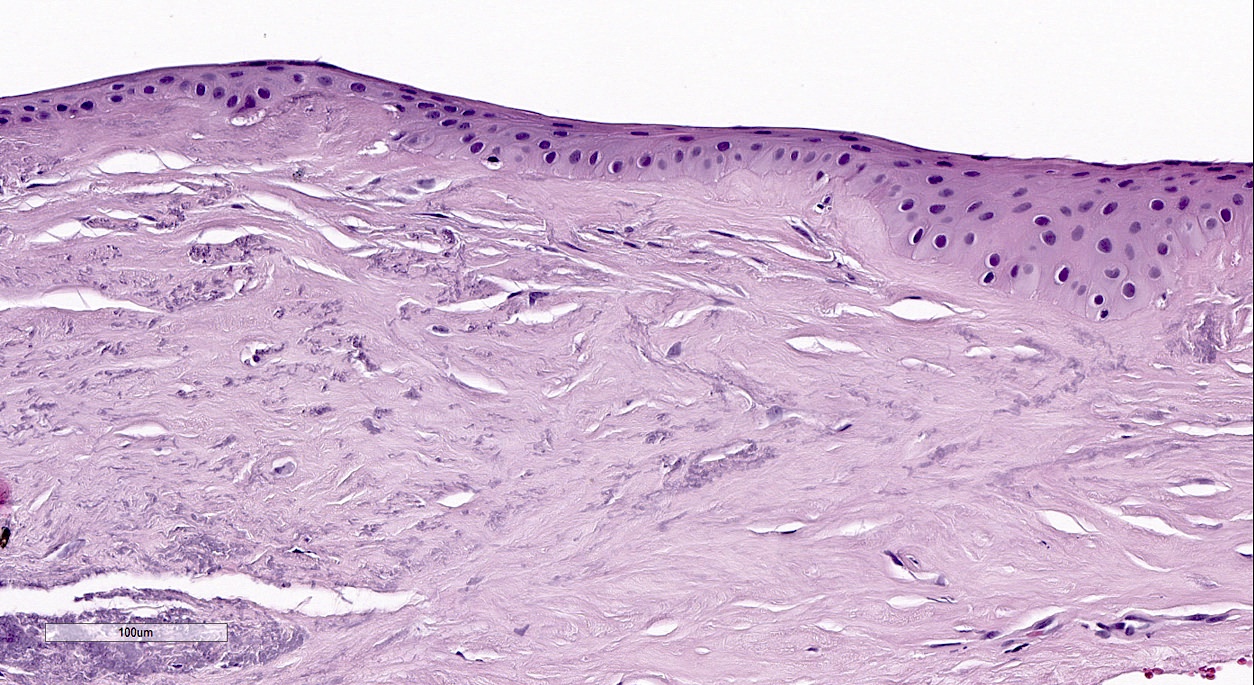
Microscopic (histologic) description
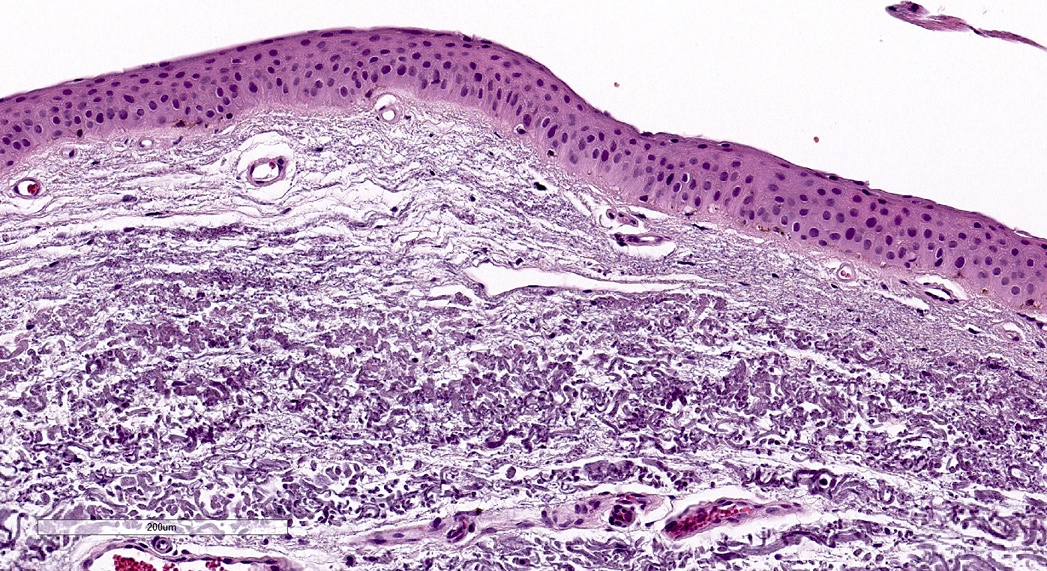
- Stromal changes:
- Fibrovascular connective tissue that migrates from the conjunctiva to cornea, dissecting into plane of Bowman layer, leading to fragmentation
- Fibrovascular core is composed of collagen mixed with basophilic fibrillar structures and blood vessels, all in variable amounts
- Variable acute and chronic inflammatory infiltrate
- Epithelial changes:
- May cause squamous metaplasia with goblet cell loss
- Acanthosis or atrophy
- Conjunctival intraepithelial neoplasia, primary acquired melanosis and nevus may coexist with pterygium (Saudi J Ophthalmol 2016;30:113, Histopathology 2006;48:387)
Microscopic (histologic) images
Positive stains
- Abnormal expression of HSP90 and Ki67 (Diagn Pathol 2013;8:32)
- Stromal plaques: E-cadherin and beta catenin (Br J Ophthalmol 2007;91:1209)
Negative stains
- HSP90 negativity may be useful to rule out ocular surface squamous neoplasia (Am J Clin Pathol 2016;145:385)
Sample pathology report
- Right eye, excision:
- Pterygium
Differential diagnosis
- Pinguecula:
- Histologically similar but there is no corneal invasion clinically or pathologically
- Superior limbic keratoconjunctivitis:
- Originates from the upper limbus
- Conjunctival intraepithelial neoplasia:
- Epithelial dysplasia; can coexist and be overlooked
Board review style question #1
Board review style answer #1
B. Elastosis of the lamina propria with corneal invasion. Elastosis is the key morphological finding in pterygia. The infiltration of the corneal stroma is important to be able to differentiate it from a pinguecula when there is no clinical information. Epithelial atrophy with goblet cell loss is nonspecific and can be seen in dry eye syndrome or superior limbic
keratoconjunctivitis. Neovascularization is present in most of pterygia but is also seen in many other
conjunctival inflammatory processes. Fragmentation of the Bowman layer may be present but is
also seen in keratoconus and other chronic keratitis.
Comment Here
Reference: Pterygium
Comment Here
Reference: Pterygium
Board review style question #2
Which of the following is the most important risk factor of pterygium?
- Chlamydia psittaci infection
- Human papillomavirus
- Sun exposure
- Tobacco and alcohol consumption
Board review style answer #2
C. Sun exposure is the most important risk factor. Human papillomavirus is not strongly associated with either pterygium or conjunctival intraepithelial neoplasia. Chlamydia psittaci has been associated with some MALT lymphomas but has not been associated with pterygium. Alcohol and tobacco have been listed as possible predisposing factors but are not as prevalent as sun exposure.
Comment Here
Reference: Pterygium
Comment Here
Reference: Pterygium