Table of Contents
Definition / general | Terminology | Conjunctival melanocytic intra-epithelial neoplasia (C-MIN) | Clinical features | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Differential diagnosisCite this page: Jain D. Conjunctival melanocytic intraepithelial lesions (CMIL). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyepamconj.html. Accessed December 4th, 2024.
Definition / general
- See also benign melanosis
- 11% of conjunctival melanocytic proliferations (Arch Pathol Lab Med 2010;134:1785)
- Called melanoma in situ by some, although cases without atypia don't progress (Mod Pathol 1991;4:253)
- Variable biologic behavior from benign to locally spreading to malignant
- Usually ages 40+ years, whites
- Presents as gradual appearance of golden brown pigmented lesion of bulbar conjunctiva
- May be associated with Addison disease
- May be contiguous with lentigo maligna (similar histology but with rete pegs) of adjacent eyelid skin
- May involve pseudoglands of Henle in palpebral conjunctiva and resemble invasive melanoma
Terminology
- Also called primary acquired melanosis (PAM)
Conjunctival melanocytic intra-epithelial neoplasia (C-MIN)
- Conjunctival melanosis now differentiated histologically into hypermelanosis and conjunctival melanocytic intra-epithelial neoplasia (C-MIN)
- Cases formerly classified as PAM are now classified as C-MIN:
- C-MIN score of 0 is melanosis only
- C-MIN score of 1 is PAM with mild atypia
- C-MIN score of 2 - 3 is PAM with moderate atypia
- C-MIN score of 4 is PAM with severe atypia
- C-MIN score of 5+ is Conjunctival melanoma in situ
- Scoring of C-MIN based on pattern of horizontal epithelial involvement, vertical depth of melanocytic infiltration, degree of cellular atypia (Eye (Lond) 2013;27:142, Clin Experiment Ophthalmol 2008;36:786)
Clinical features
- Unilateral, flat, acquired, brown pigmentation, rarely amelanotic, fair skinned individual
Prognostic factors
- Cases without atypia have no / minimal risk of progression to melanoma
- 46% with atypia do progress to melanoma (Hum Pathol 1985;16:129)
- Extent in clock hours is significant factor for recurrence and progression (Ophthalmology 2008;115:511)
- Was predisposing lesion in 13 - 75% cases of melanoma (Int J Surg Pathol 2010;18:60, Trans Am Ophthalmol Soc 2007;105:61)
Case reports
- 30 year old woman with conjunctival melanoma arising from diffuse primary acquired melanosis (Cornea 2005;24:352)
- Associated benign pigmented nodule (Orbit 2007;26:57)
Treatment
- Excision or cryotherapy
- Also topical mitomycin C (Clin Experiment Ophthalmol 2006;34:708, Graefes Arch Clin Exp Ophthalmol 2005;243:1108) or 5-FU
- Cases with atypia usually recur or develop new foci
Gross description
- Diffuse granular conjunctival pigmentation, usually in bulbar conjunctiva, also cornea, palpebral conjunctiva, eyelid skin
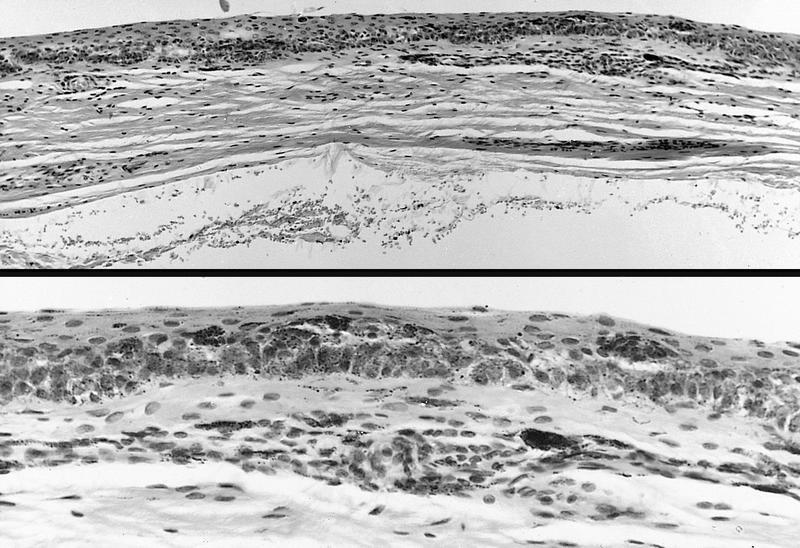
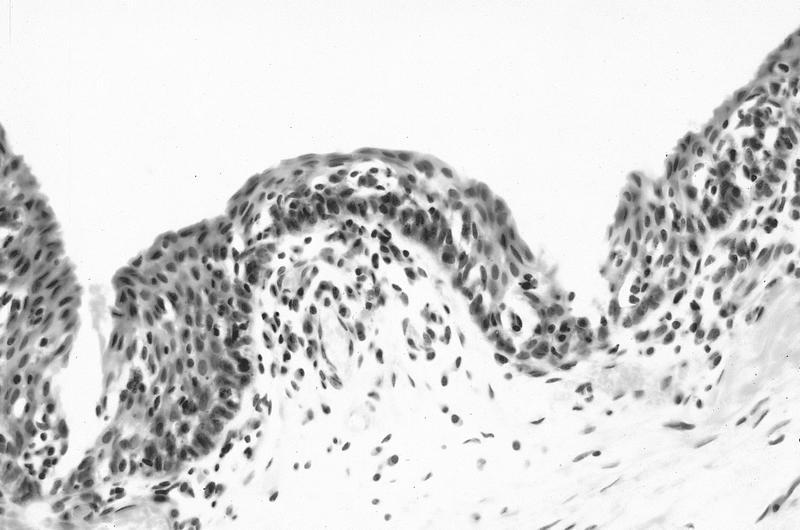
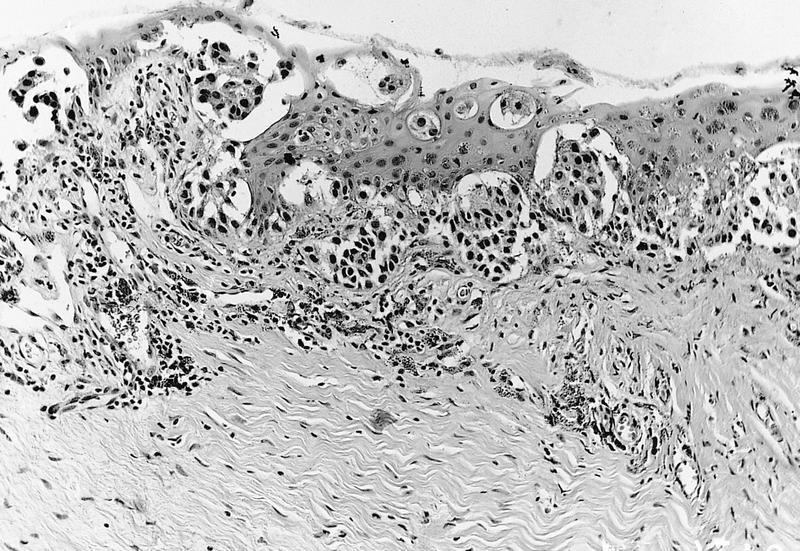
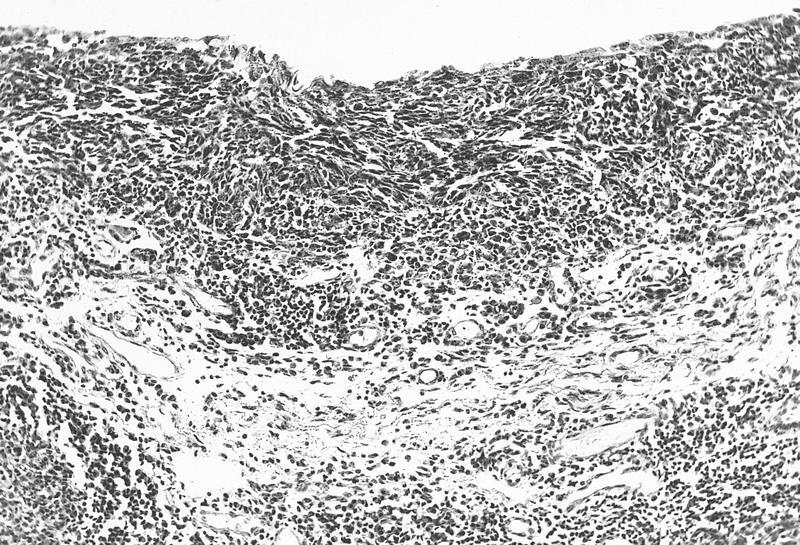
Microscopic (histologic) description
- See C-MIN scoring system above
- Intraepithelial proliferation of abnormal melanocytes with variable atypia
- Early: pigmentation of basilar epithelium only
- Later:
- Basilar melanocytic hyperplasia with nests, resembling Paget disease
- Cells have retracted cytoplasm, larger nuclei than neighboring cells, clumped chromatin and prominent basophilic nucleoli
- Cells may be small with scant cytoplasm and small round nuclei
- Classification: with or without atypia
- High risk of progression: atypia plus epithelioid features including abundant cytoplasm, vesicular nuclei, prominent nucleoli, may be mixed with low risk areas (almost all are associated with invasion, Am J Surg Pathol 2007;31:185)
- Low risk of progression: atypia plus primarily single cell lentinginous growth, small / medium size, high N/C ratio, small / medium hyperchromatic nuclei, no nucleoli, 15% risk of invasion
- Pitfalls: don't interpret melanophages as invasive tumor cells
- Sine pigmento: melanocytes without pigment
- Post-topical chemotherapy changes: epithelial atrophy, dyskeratosis, pyknosis, focal keratinization
Microscopic (histologic) images
Electron microscopy description
- Grade 1: melanocytes with dendritic processes and transferred melanin in epithelial cells
- Grade 2: melanocytes have short dendritic processes, incomplete melanin transfer and immature melanosomes, irregular nuclei with clumped chromatin and large nucleoli
- Grade 3: epithelioid cells, no cytoplasmic processes, large irregular nuclei with large prominent nucleoli and abnormal melanin transfer
Differential diagnosis
- Cystic benign melanosis:
- Epithelial lined cysts in substantia propria, goblet cells and secondary pigmentation of basilar keratinocytes (Cornea 2012;31:1273)
- Hypermelanosis:
- Freckle or complexion melanosis
- Bilateral, does not change over time
- Junctional nevus:
- Children, no irregular epithelial involvement, no melanocytic nests, no polygonal cells, no atypia
- Melanoma:
- Invasion
- Secondary melanosis:
- Due to Addison disease, pigmented squamous cell carcinoma
- Subconjunctival pigmentation:
- Congenital ocular melanocytosis