Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Peña JT, Zoroquiain P. Temporal arteritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyeorbittemporalarteritis.html. Accessed April 1st, 2025.
Definition / general
- Temporal (or giant cell) arteritis is a systemic and discontinuous nonnecrotizing, granulomatous vasculitis of elastic and muscular arteries
Essential features
- Presents in patients in the sixth decade of life or older with new onset headache
- Risk of permanent vision loss if left untreated
- Diagnosis requires morphologic confirmation (biopsy is the preferred modality)
- Classic findings include lymphocytes and macrophages arranged in concentric rings surrounding the external and internal elastic lamina as well as an association with intimal hyperplasia and loss / fragmentation of elastic fibers
- Useful stains: elastic stain, CD3 and CD68
Terminology
- Temporal arteritis
- Giant cell arteritis
- Horton disease
- Horton giant cell arteritis
- Cranial arteritis
ICD coding
Epidemiology
- Most common systemic / primary vasculitis (Semin Arthritis Rheum 2020;50:1040)
- Age: > 50 years; mean: 70 years; peak: 71 - 80 years
- Gender: F:M = 3:1
- Race / ethnicity: more common in Caucasians; rare in Asian and African American patients
- Incidence (ACR classification criteria)
- Northern Europe (Norway): 29 - 32.8 / 100,000 (J Rheumatol 1997;24:1739, J Rheumatol 2000;27:2624)
- U.S. (Minnesota): 19.8 / 100,000 (Scand J Rheumatol 2015;44:215)
- Southern Europe (Spain): 2.2 - 10.2 / 100,000 (Clin Exp Rheumatol 2015;33:S-11, Rheum Dis Clin North Am 2001;27:729)
- Seasonal variation: there is no seasonal influence (RMD Open 2017;3:e000531)
- Mortality (Rheumatology (Oxford) 2022;61:1195)
- All cause mortality
- 6.4% at 1 year (relative risk 1.49 ± 0.13); 45% at 10 years (relative risk 1.03 ± 0.02)
- Cause specific mortality
- Compared to the general population, there is increased mortality due to infectious, endocrine, cardiovascular and gastrointestinal diseases
- This increased mortality may be corticosteroid related (J Rheumatol 2017;44:84)
- All cause mortality
Sites
- Cranial arteries: temporal artery, occipital artery and intraorbital branches (ophthalmic and posterior ciliary)
- Extracranial arteries are compromised in 20 - 67% of cases (angiography) (Arthritis Care Res (Hoboken) 2020;72:1615)
- Most common sites: carotid, subclavian, axillary and thoracic aorta
- Bilateral axillary artery compromise is common
Pathophysiology
- Immunopathological model as described by Greigert et al. (J Clin Med 2022;11:2905)
- Phase 1: loss of tolerance and activation of the adventitia resident dendritic cells
- Dendritic cells acquire mature phenotype and produce IL12, IL23, IL6 and IL1β
- Phase 2: recruitment, activation and polarization of CD4+ T cells
- CD4+ T cells polarize to Th1 and Th17 phenotypes
- Phase 3: recruitment of CD8+ T cells and monocytes
- Phase 4: vascular remodeling
- Macrophages release several factors, such as reactive oxygen species and matrix metalloproteinases, which mediate internal elastic lamina destruction
- Vascular smooth muscle cells migrate to the intima and acquire a myofibroblast phenotype
- Myofibroblasts produce intimal hyperplasia, which then causes vessel occlusion and subsequent ischemia
- Phase 1: loss of tolerance and activation of the adventitia resident dendritic cells
Etiology
- Immune mediated disease of unknown etiology
- Postulated genetic predisposing factors (Sci Rep 2017;7:43953):
- Major histocompatibility class II genes (HLA-DRB1*04 alleles)
- IL12B locus
Clinical features
- Headache (73%)
- Tender temporal artery (31%)
- Scalp tenderness (44%)
- Jaw claudication (45%) (best predictor of positive biopsy)
- Can be elicited by the chewing gum test (N Engl J Med 2016;374:1794)
- Visual disturbances
- Blurred vision (18%)
- Transient vision loss (5%)
- Permanent vision loss (6%), due to ischemic optic neuropathy
- Fever (16%)
- Weight loss (25%)
- 25% of patients can be asymptomatic
- Comorbidities
- Polymyalgia rheumatica (PMR) (Rheumatology (Oxford) 2017;56:506)
- 40 - 60% of patients with giant cell arteritis have signs and symptoms of polymyalgia rheumatica
- 16 - 21% of patients with polymyalgia rheumatica develop giant cell arteritis
- Symptomatic thoracic aneurysm: 10 - 15% of giant cell arteritis patients develop symptomatic thoracic aneurysms
- Polymyalgia rheumatica (PMR) (Rheumatology (Oxford) 2017;56:506)
- Reference: Semin Arthritis Rheum 2021;51:1193
Diagnosis
- Diagnosis requires morphologic confirmation
- EULAR 2018: diagnostic confirmation can be performed by imaging or histology (Ann Rheum Dis 2020;79:19)
- ACR / Vasculitis Foundation 2021: temporal artery biopsy is the preferred modality for diagnostic confirmation (Arthritis Rheumatol 2021;73:1349)
- Ultrasonography: offers good sensitivity and specificity in treatment naive patients (up to 4 days of treatment)
- Temporal artery biopsy (TAB): offers good sensitivity and specificity within 2 - 4 weeks of glucocorticoid treatment (BMC Musculoskelet Disord 2016;17:363)
- Optimal length of biopsy: > 1 cm with at least 1.5 cm preferred by some groups (ANZ J Surg 2018;88:191)
- Unilateral temporal artery biopsy is the preferred modality as an initial approach over bilateral biopsies, though bilateral biopsies are recommended by some groups due to possible discordant findings (J Vasc Surg 2022;76:1704, Can J Ophthalmol 2014;49:157)
Laboratory
- Elevated erythrocyte sedimentation rate
- Elevated C reactive protein
Radiology description
- High frequency Doppler ultrasound
- Halo sign (sensitivity 80%, specificity 80%): hypoechoic halo surrounding temporal artery lumen (J Ultrasound 2022;25:837)
- Compression sign (sensitivity 85%, specificity 65%): compression of the temporal artery produces contrasting echogenicity in the surrounding tissue (Clin Exp Rheumatol 2015;33:S-113)
Prognostic factors
- Predictors associated with reduced risk of permanent visual loss
- Fever
- Rheumatic symptoms
- Predictors associated with increased risk of permanent visual loss
- Age
- History of transient visual ischemic symptoms
- Jaw claudication
- Reference: J Rheumatol 2016;43:1393
Case reports
- 68 year old woman with tongue necrosis (Case Rep Med 2017;2017:6327437)
- 71 year old woman with headache and normal inflammatory markers (Clin Med (Lond) 2020;20:224)
- 72 year old man with an aortic aneurysm (Radiol Case Rep 2021;16:3734)
- 79 year old man with vision loss (Rheumatol Int 2022;42:1855)
- 81 year old woman with scalp ulceration (BMJ Case Rep 2019;12:e230795)
Treatment
- High dose glucocorticoids
Gross description
- Segment of muscular artery with thickened, nodular and rubbery wall
- Grossing and processing differ between institutions but should be thorough and account for the possibility of skip lesions or the uneven distribution of pathologic changes
- Serially section vessel at 3 mm intervals
- Embed in cross section (ink may be used to indicate which surface should be embedded to ensure uniform examination along the entire length of the artery)
- Some prefer cutting 30 levels with 1 H&E slide performed every third level, leaving intervening unstained slides for additional stains as needed
- Others recommend cutting 4 leveled groups with 1 H&E, 1 elastin stain and 1 unstained slide per group (Westra: Surgical Pathology Dissection - An Illustrated Guide, 2nd Edition, 2003, J Clin Pathol 2000;53:137)
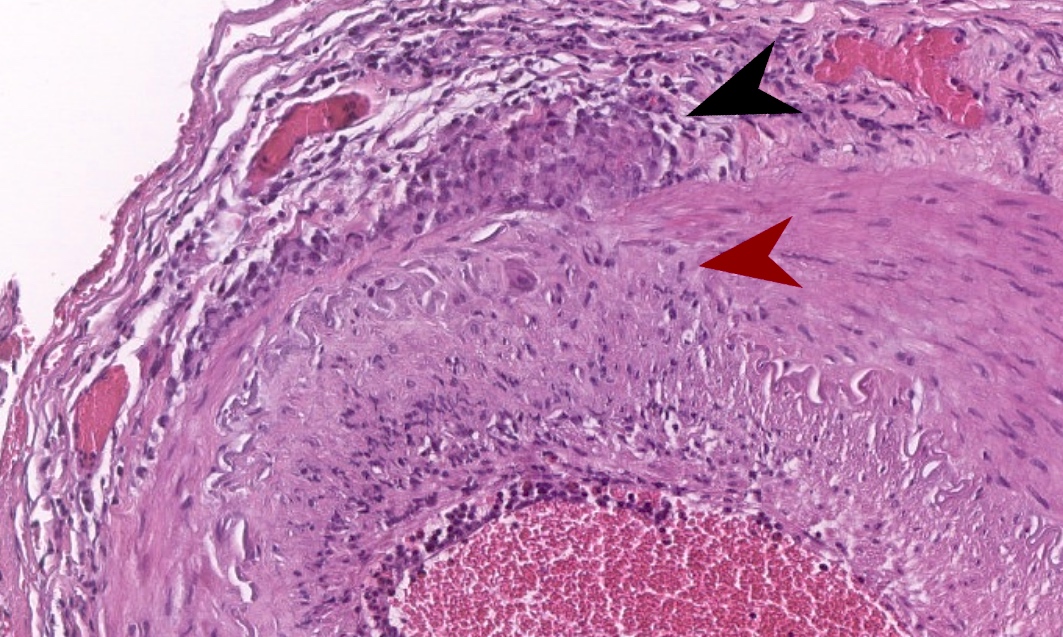
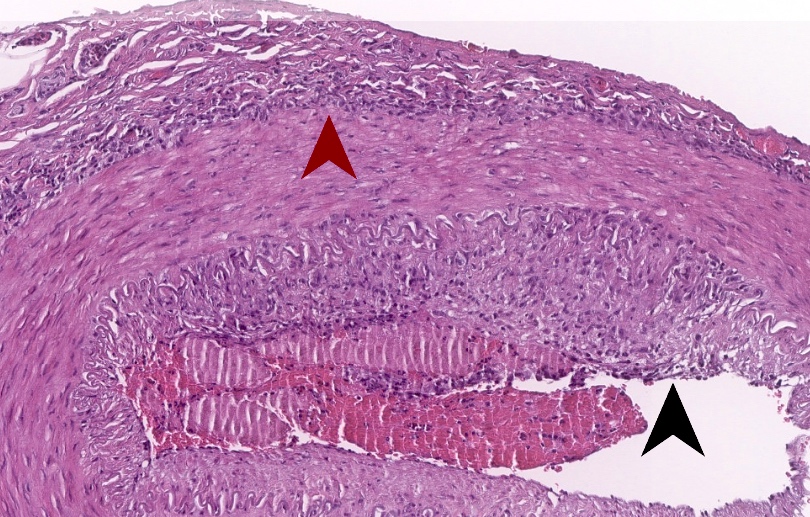
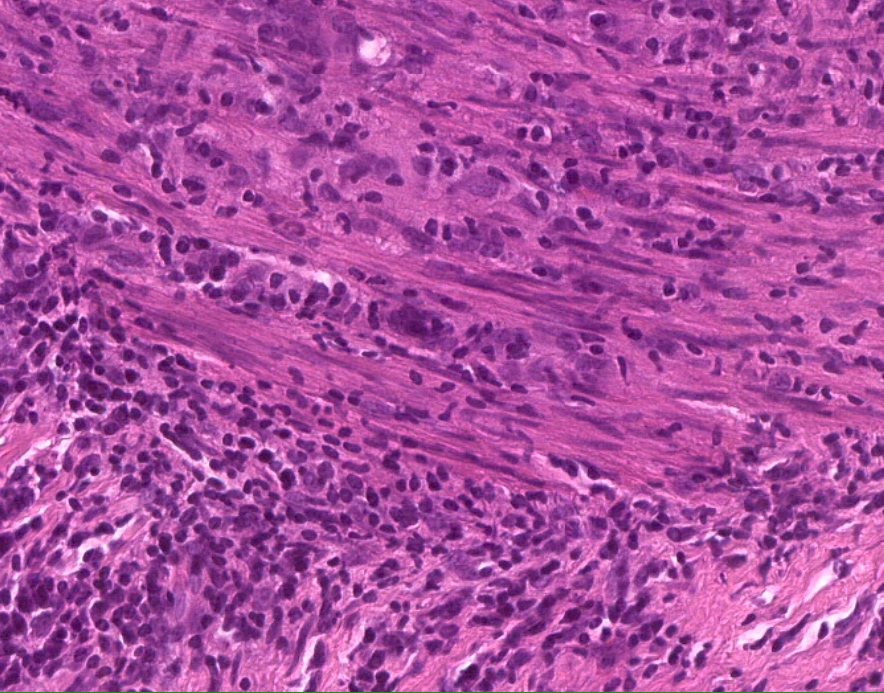
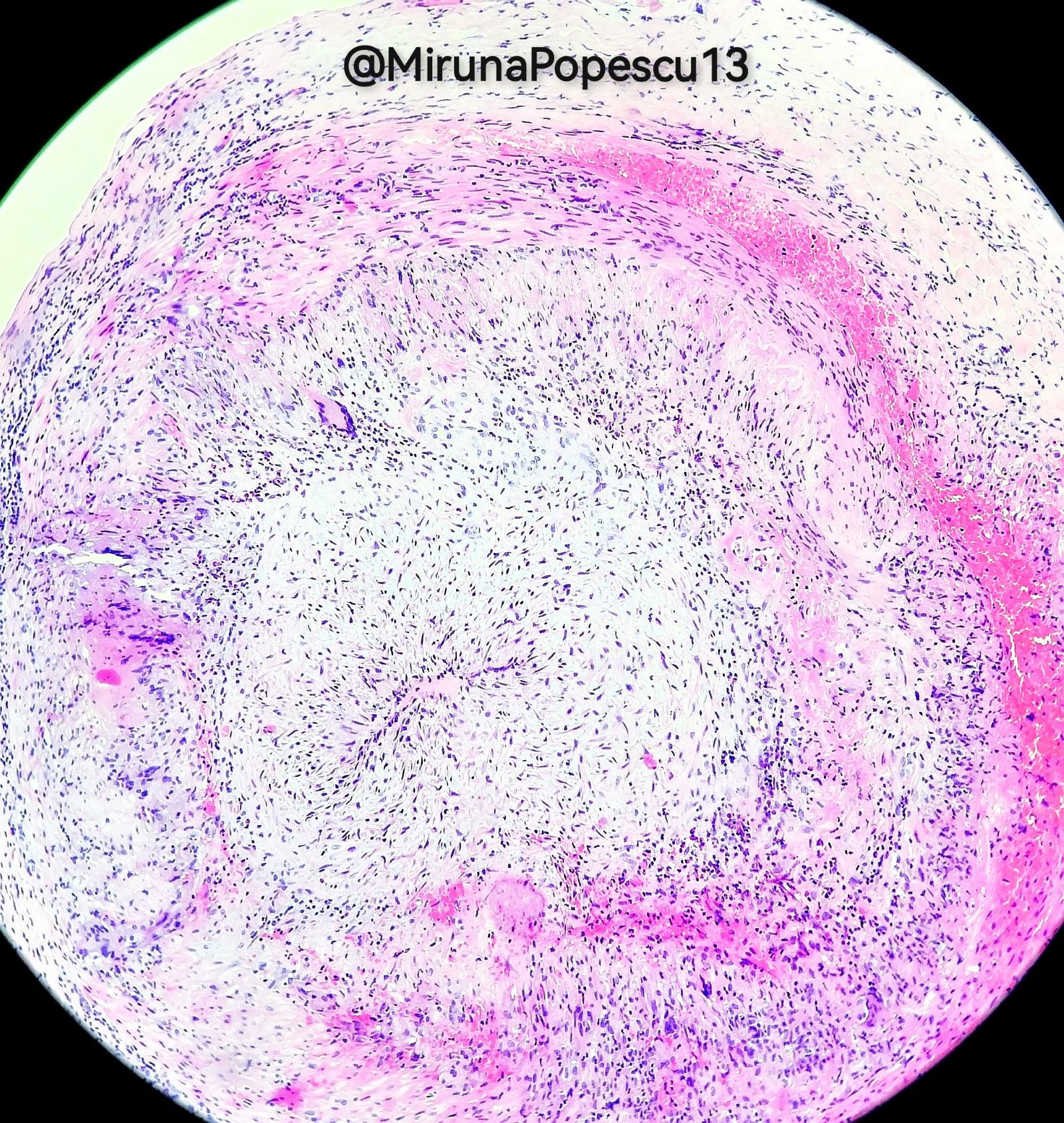
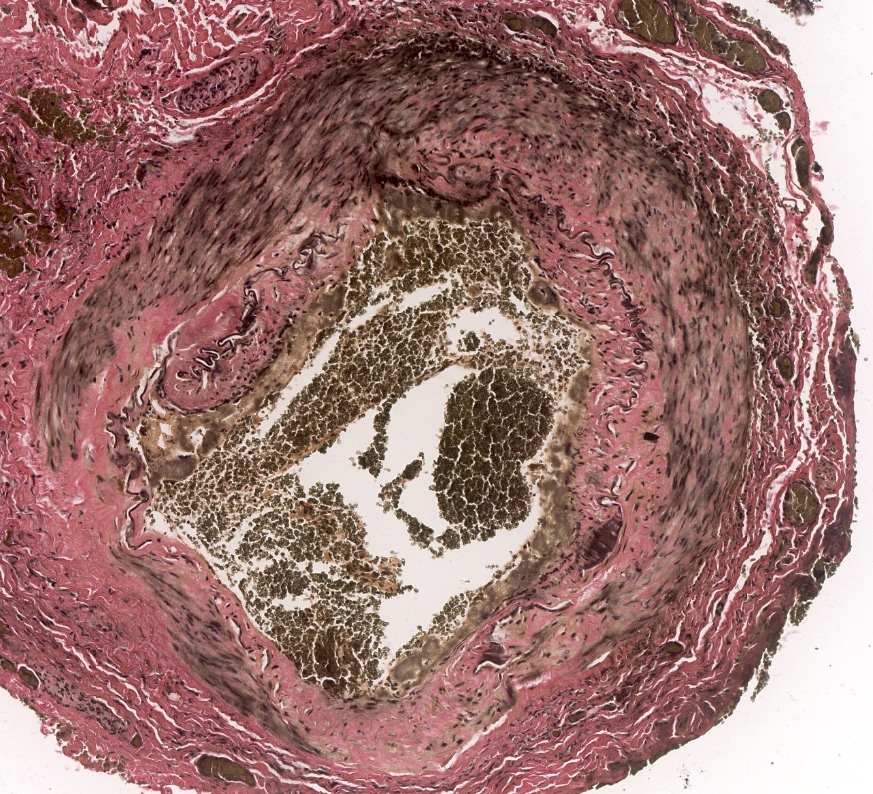
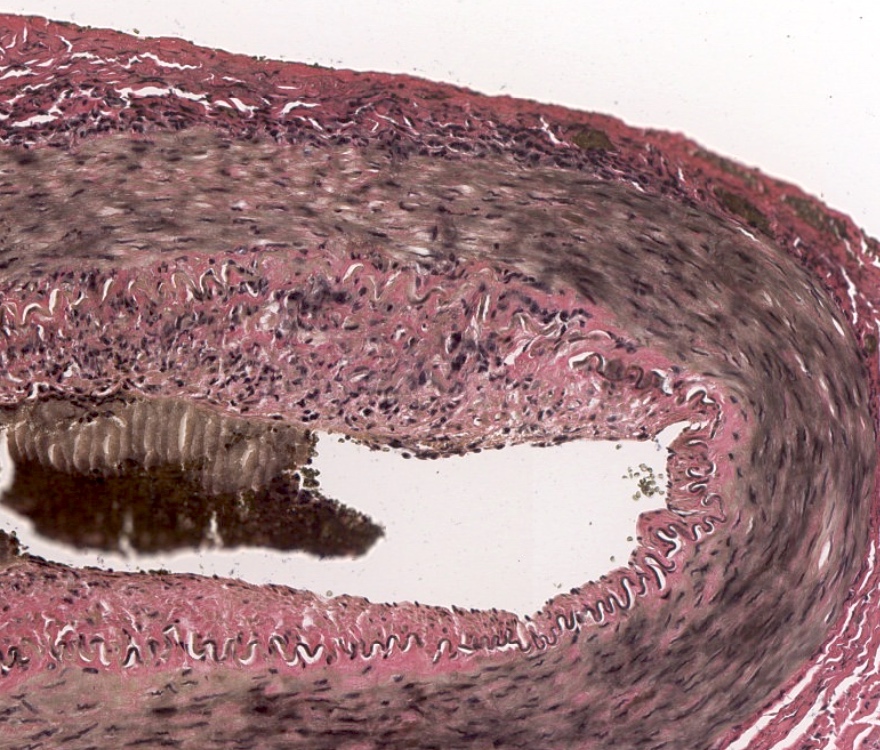
Microscopic (histologic) description
- Classic giant cell arteritis (77% of cases) (Am J Surg Pathol 2014;38:1360)
- Transmural inflammation pattern with lymphocytes and macrophages arranged in concentric rings, surrounding the external and internal elastic lamina and associated with intimal hyperplasia and loss of elastic fibers
- 50 - 70% of cases exhibit giant cells but giant cells are not required for the diagnosis
- Neutrophils are uncommon (1.8%)
- Unusual findings include necrosis, well formed granulomas and thrombosis
- Transmural inflammation pattern with lymphocytes and macrophages arranged in concentric rings, surrounding the external and internal elastic lamina and associated with intimal hyperplasia and loss of elastic fibers
- Borderline arteritis - lymphocytic and histiocytic infiltrate restricted to the following localizations
- Vasa vasorum vasculitis (6.5% of cases): inflammation of vasa vasorum in the absence of medial inflammation
- Inflammation limited to the adventitia (7% of cases): crescent shaped configuration limited to the adventitia and external elastic lamina, with sparing of the media
- Small vessel vasculitis (9% of cases): inflammatory lymphocytic infiltrate surrounding (cuffing) small periadventitial vessels
- Healed arteritis - fibrotic changes without inflammatory lymphocytic infiltrate
- Marked intimal thickening
- Intimal, medial and adventitial fibrosis and scarring, with neovascularization
- Loss of elastic fibers
Microscopic (histologic) images
Virtual slides
Positive stains
Videos
Vasculitis Foundation giant cell arteritis webinar
Giant cell arteritis
by Nicholas J. Volpe,
European Society of Ophthalmology
Temporal artery biopsy technique
Giant cell arteritis (temporal arteritis) pathology by Jerad Gardner, M.D.
Sample pathology report
- Right temporal artery, biopsy:
- Morphological findings consistent with temporal arteritis (see comment)
- Comment: There is lymphocytic and macrophagic infiltration within the vascular wall. Multinucleated giant cell phagocytizing elastic fibers (elastic stain) are observed, supporting the diagnosis.
- Gross description: Specimen A is received in formalin in a container and labeled with the patient’s name and specimen number and designated right temporal artery. The specimen consists of a tan, tubular structure, consistent with a muscular artery, that measures 1.5 cm in length and is notable for nodularity and thickening. The specimen is serially cross sectioned at 3 mm intervals, placed between sponges and submitted entirely in a cassette.
Differential diagnosis
- Age related changes:
- Intimal hyperplasia, duplication of the elastic inner lamina, adventitial fibrosis
- Absence of mononuclear infiltration of the arterial wall
- Another vasculitis (up to 5% of cases):
- Neutrophil infiltration, abundant fibrinoid necrosis, microthrombi and leukocytoclasis
- AL amyloidosis (< 1%) (Mod Rheumatol Case Rep 2020;4:90):
- Intramural amorphous eosinophilic material deposits
- Light chain immunofixation in urine
- Congo red+ with green dichroism
- Calciphylaxis (< 1%) (J Neuroophthalmol 2022;42:e362):
- Calcium deposition in vessels
- Numerous thrombi
- Necrosis of distal territories
- Atherosclerosis (< 1%) (J Neuroophthalmol 2022;42:e359):
- Intimal hyperplasia, foamy macrophages (early)
- Intimal fibrosis, cholesterol cleft and variable inflammatory cell infiltration within the intima (chronic)
- No medial inflammation, no phagocytosis of elastic fibers
- Mönckeberg medial calcific sclerosis of the temporal artery (< 1%) (Cureus 2020;12:e9210):
- Annular calcification within media
- No thrombus
- No inflammatory infiltrate
Additional references
Board review style question #1
In addition to special staining to evaluate elastic fibers, which of the following antibody panels is most useful for evaluating temporal arteritis?
- CD3 / CD68
- CD4 / CD8
- CD20 / CD138
- CD34 / CD68
Board review style answer #1
A. CD3 / CD68. The hallmark of temporal arteritis is a transmural lymphocytic (T cells) and macrophagic infiltrate, which can be demonstrated with antibodies against CD3 and CD68, respectively. Answer C is incorrect because B cells (CD20+) and plasma cells (CD138+) are not diagnostic findings. Answer D is incorrect because the combination of CD34 and CD68 highlights histiocytes, myofibroblasts and small blood vessels but excludes T cells. Answer B is incorrect because although CD4+ and CD8+ are T cell markers, this panel does not stain macrophages.
Comment Here
Reference: Temporal arteritis
Comment Here
Reference: Temporal arteritis
Board review style question #2
Board review style answer #2
B. Loss of elastic fibers. The Verhoeff-Van Gieson stain is a special stain used to demonstrate elastic fibers. In the setting of temporal arteritis, it can be used to evaluate areas of loss and disorganization of elastic fibers. Answer A is incorrect because intimal hyperplasia is visible with H&E and does not require special stains. Answer D is incorrect because tunica media fibrosis is a nonspecific finding and can be observed in the scenario of healed arteritis. Answer C is incorrect because myxoid degeneration is not a characteristic finding of temporal arteritis.
Comment Here
Reference: Temporal arteritis
Comment Here
Reference: Temporal arteritis