Table of Contents
Globe | Lacrimal duct & gland | Lens | Orbit & optic nerve | Radiology images | Drawings | Microscopic (histologic) description | Microscopic (histologic) imagesCite this page: Pernick N. Anatomy & histology-other. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyeanatomyother.html. Accessed April 3rd, 2025.
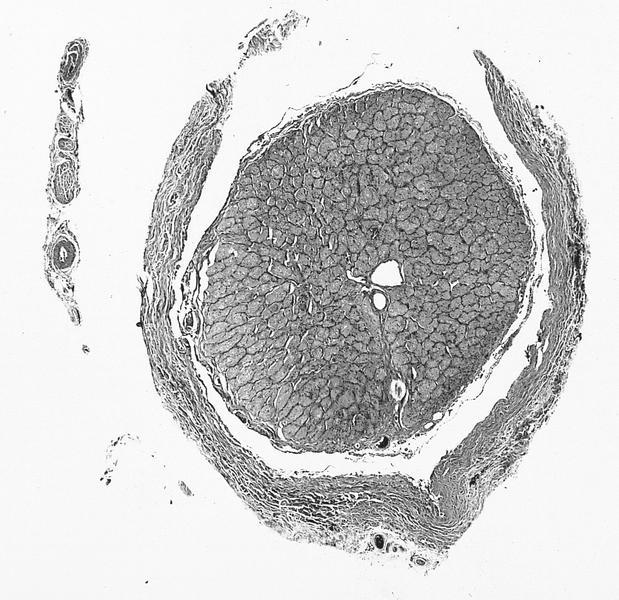
Globe
- Defined as eyeball itself plus intraocular tissues, or eye proper without its appendages
- Dimensions: anterior-posterior 24 mm, vertical and horizontal dimensions are both 23 to 23.5 mm
- Six extraocular muscles:
- 4 rectus and 2 oblique muscles
- Arise in posterior orbit from fibrous ring called annulus of Zinn, and insert into sclera
- Muscles are surrounded by fascia
- Inferior oblique inserts on sclera, other muscles insert on tendons
- Equator: midway between anterior and posterior poles
- Specimen is the result of enucleation, performed because eye is nonfunctional, painful, unsightly, infectious, contains neoplasm, post-trauma (may be removed to prevent sympathetic uveitis) or has chronic glaucoma
- Globe usually intact but free of extraocular muscles and orbital fat
- Globe may be eviscerated, with only fragments available for microscopic study
- Initial pathologic processes may be obscured by subsequent pathologic processes
- Enucleation: due to tumor (48%, usually melanoma), glaucoma (13%), phthisis bulbi (12%), recent trauma (11%)
- Specimens also received after evisceration (10%) or exenteration (9%) to manage malignant orbital tumors (Am J Clin Pathol 2003;119:594)
- During 1990 to 2000, decrease in percentages due to neoplasms, increase due to glaucoma and phthisis bulbi
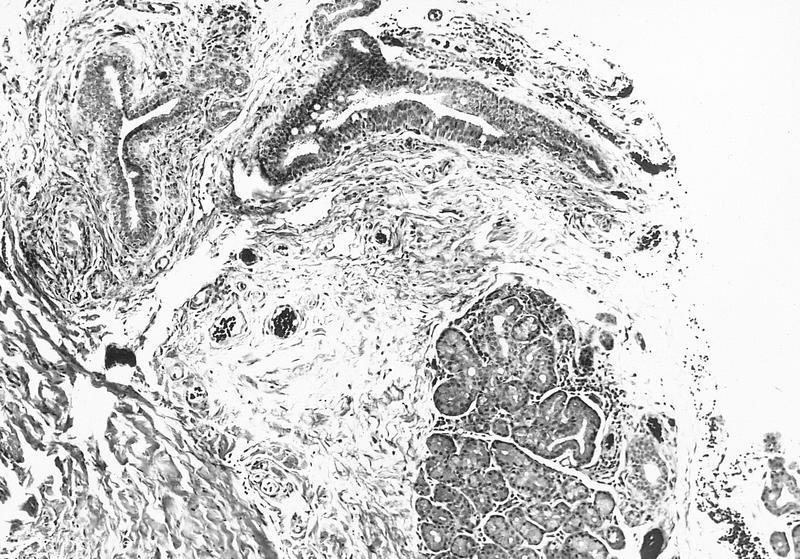
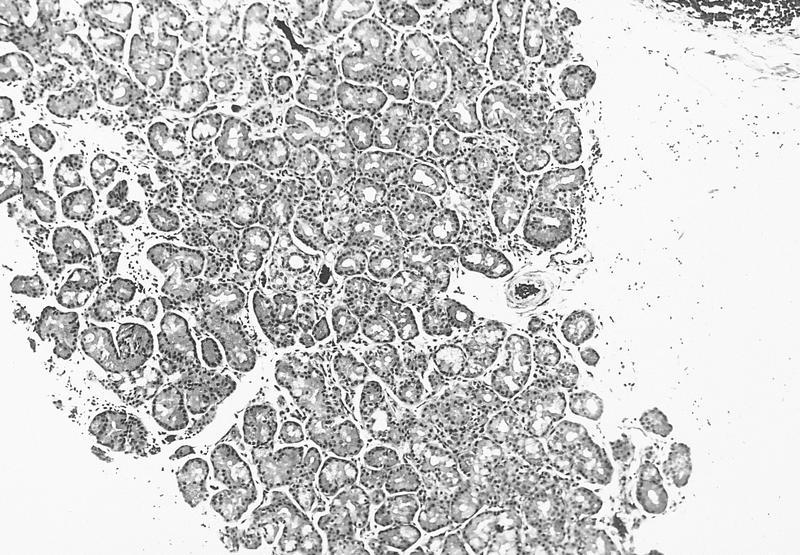
Lacrimal duct & gland
- Lacrimal gland located in superiotemporal aspect of orbit, not palpable
- Contributes secretions to tear film including IgA
- Accessory lacrimal glands are embedded above fibrous tarsus of eyelid and in conjunctival fornix
- Serous with minor mucinous component
- Larger ducts have myoepithelial layer
- Normally may have lymphocytes and plasma cells
- Drainage apparatus is composed of puncta, canaliculi, lacrimal sac and nasolacrimal duct
- Tears drain toward medial canthus, then through lacrimal punctum into lacrimal canaliculi, then nasolacrimal sac, then nasolacrimal duct, then nose
- Puncta:
- Opening in medial aspect of eyelid where tear fluid drains
- Canaliculi (lacrimal duct):
- Tubular structures 0.5 mm in diameter where puncta drains
- Nonkeratinizing squamous epithelium surrounded by fibrous tissue
- Lacrimal sac:
- Merging of canaliculi, encased by bones of orbit
- Stratified columnar epithelium with goblet cells
- Nasolacrimal duct:
- Drains lacrimal sac, 1 cm long, connects to inferior meatus of nose
- Stratified columnar epithelium with goblet cells
- Lacrimal duct disorders often cause epiphora (tears flow over lid margin onto cheek), induration, inflammation of lower eyelid
- Tumors tend to displace eye downward because adjacent orbit restricts growth
- Tumors are difficult to resect completely leading to high recurrence rate
- Lacrimal gland is considered a minor salivary gland for tumor reporting
- Regional lymph nodes are preauricular (parotid), submandibular and cervical
Lens
- Most surgical specimens are cataracts or prosthetic intraocular lens
- Normal lens is biconvex, behind pupil / iris, in front of vitreous, in posterior chamber
- 10 mm in diameter by 4 - 5 mm in width
- Usually Gross Examination Only (report as transparent - Yes or No), don't section
- Anterior lens capsule is eosinophilic acellular band overlying single layer of epithelial cells
- Lens capsule is strongly PAS+, holds lens in place
- Lens has thinner capsule posteriorly, without epithelial cells
- Lens in held in place by zonules that connect to pars plicata of ciliary body
- Lens normally opacifies with age due to globules of degenerate lens fibers
- Is a closed epithelial system with lens capsule (epithelium) that totally envelops the lens
- Vitreous humor:
- Avascular
- Extends from lens to sensory retina
- Contains gel-like material composed of water, protein, hyaluronic acid and "hyalocytes"
- Gel consistency is due to randomly oriented collagen fibrils
- May appear as amorphous material on H&E
Orbit & optic nerve
- Orbit contains globe and its fibrous covering (Tenon capsule), lacrimal gland, optic nerve and its meningeal covering, extraocular muscles, cartilaginous trochlea, blood vessels and delicate fibroadipose connective tissue
- Floor of orbit is roof of maxillary sinus
- Medial wall of orbit (lamina papyracea) separates orbit from ethmoidal sinuses
- Proptosis: forward displacement of eyeball (or other organs), due to any disease that increases orbital contents, since orbit is closed medially, laterally and posteriorly
- Exophthalmos: abnormal protrusion of eyeball
- Common symptom of orbital disease, although often due to thyroid disease and not biopsied
- Other common causes of exophthalmos are mucocele from paranasal sinus, hemangioma, inflammatory pseudotumor
- Optic nerve:
- Surrounded by meninges; part of central nervous system
- Not usually biopsied
- Often has psammoma bodies or drusen (calcified acellular globular concretions of nerve fibers)
- Site of convergence of one million axons from retinal nerve fiber layer
- Nerve head accounts for physiologic blind spot in normal visual field
- Receives blood supply from branches of ophthalmic artery
- Surrounded on both sides by short posterior ciliary arteries
- Lamina cribrosa:
- Site of myelination of optic nerve axons
- Highlighted with Luxol fast blue or other myelin stains
- Trochlea:
- Arc shaped structure through which tendon of superior oblique muscle passes before insertion upon eyeball
- The only cartilaginous structure in normal orbit
- Tumors should be reported using formats published for their counterparts elsewhere in body
- Drainage through submandibular, parotid and cervical lymph nodes through vascular anastomosis
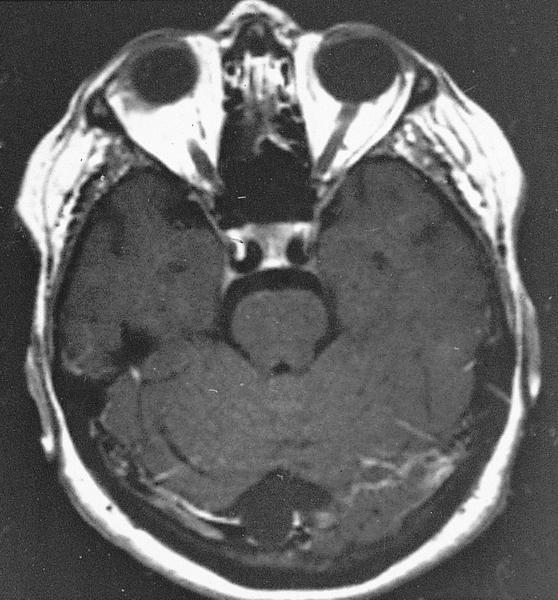
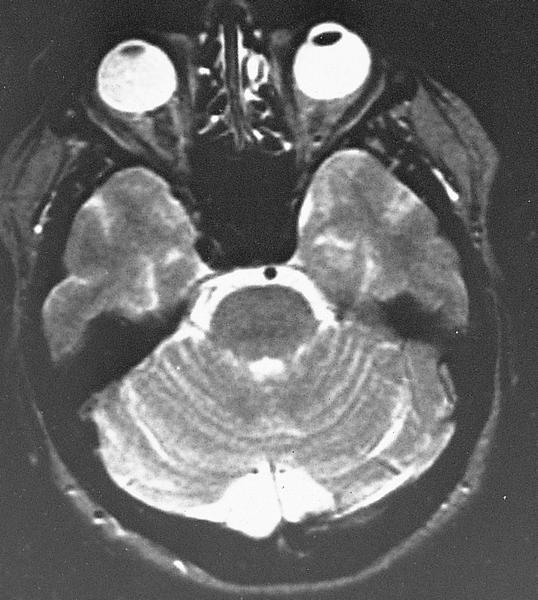
Radiology images
Drawings
Microscopic (histologic) description
- Anterior but not posterior lens has single epithelial layer