Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nazli S, Hagen CE. Squamous dysplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagussquamousdysplasia.html. Accessed April 2nd, 2025.
Definition / general
- Neoplastic alteration of squamous esophageal mucosa without invasion
- Precursor lesion to squamous cell carcinoma (SCC)
- Low grade dysplasia is characterized by atypia limited to the lower half of the epithelium while high grade dysplasia is characterized by atypia involving greater than half of the epithelium
Essential features
- Precursor lesion to squamous cell carcinoma
- Occurs predominantly in the middle third of the esophagus
- Often encountered at the periphery of invasive squamous cell carcinoma
- Comprises both architectural and cytologic abnormalities
Terminology
- Squamous intraepithelial neoplasia, squamous carcinoma in situ
ICD coding
- ICD-O
- ICD-11
- 2E92.0 & XH3Y37 - benign neoplasm of esophagus & esophageal squamous intraepithelial neoplasia (dysplasia), low grade
- 2E60.1 & XH9ND8 - carcinoma in situ of esophagus & esophageal squamous intraepithelial neoplasia (dysplasia), high grade
Epidemiology
- More prevalent in certain geographic regions, with a higher incidence in parts of Asia (including China and Iran) and parts of Africa
- Risk is highest in North Central China where 25% of adults ≥ 35 years of age are found to have the lesion (Cancer Epidemiol Biomarkers Prev 2013;22:540)
- Diets rich in nitrates and nitrosamines may be predisposing factor
- U.S. is a low risk area for both squamous dysplasia and SCC
- In the U.S., squamous dysplasia is more common in Black patients than in White patients
- Mostly seen in heavy alcohol users and smokers (Int J Clin Oncol 2010;15:135)
Sites
- Can occur anywhere in the esophagus but more common in mid esophagus (Gastroenterol Rep 2017;5:247)
Etiology
- Environmental exposures, predisposing conditions and genetic factors interplay in the pathogenesis of squamous dysplasia; risk factors are similar to those of SCC (Gastroenterology 2018;154:360)
- Substantial alcohol use and smoking
- Chronic esophageal irritation associated with conditions such as achalasia, esophageal diverticula, gastroesophageal reflux disease (GERD), Plummer-Vinson syndrome and chronic strictures
- Low socioeconomic status
- Dietary factors and drinking very hot beverages
- Increased body mass index
- Male sex
- Genetic conditions
- Nonepidermolytic palmoplantar keratoderma (tylosis), a rare autosomal dominant disorder with hyperkeratosis of palms and soles, confers a > 90% risk of development of SCC (Orphanet J Rare Dis 2015;10:126)
- Epidermoid metaplasia, also termed esophageal leukoplakia, is thought to represent a precursor lesion to squamous dysplasia
- Magnitude of risk is not known, although targeted next generation sequencing supports that epidermoid metaplasia shares molecular signatures with squamous dysplasia and squamous cell carcinoma (Mod Pathol 2017;30:1613)
- Current consensus is that human papillomavirus (HPV) is unlikely to be a substantial risk factor (Gastroenterology 2018;154:360)
Clinical features
- Patients may present with dysphagia or be asymptomatic
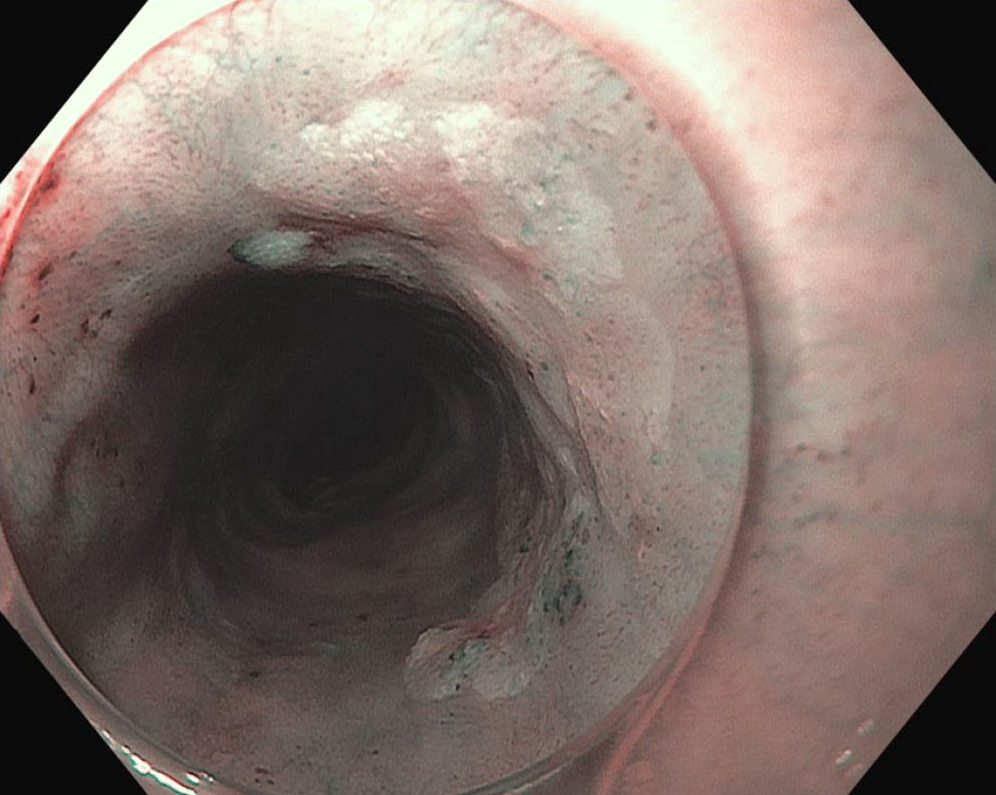
- Endoscopically, dysplasia is usually flat and requires enhancing techniques such as methylene blue or Lugol iodine with chromoendoscopy or narrow band imaging (Ann Gastroenterol 2015;28:41)
Diagnosis
- Endoscopic biopsy with histologic examination
Prognostic factors
- Patients with high grade dysplasia have a greater risk of progressing to SCC
- In a study of Chinese patients over a period of 3.5 years, 5% of patients with mild dysplasia progressed to SCC versus 65% with severe dysplasia (Cancer 1994;74:1686)
Case reports
- 62 year old man with liver cirrhosis (Transl Cancer Res 2022;11:2433)
- 62 year old man with upper gastrointestinal (GI) bleed (Rev Esp Enferm Dig 2023;115:194)
- 76 year old woman with a past medical history of GERD with esophagitis (Am J Gastroenterol 2020;115:S962)
- 77 year old woman with history of achalasia (Cureus 2022;14:e23735)
Treatment
- Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) is the definitive treatment with endoscopic surveillance for recurrence or progression
- Alternatively, for superficial dysplasia, radiofrequency ablation can be performed (Gastrointest Endosc 2017;85:322, Gastrointest Endosc 2017;85:330)
Clinical images
Gross description
- Erythema, nodular or irregular mucosa, erosive appearance or plaque-like white patches
- Discolored, granular mucosa
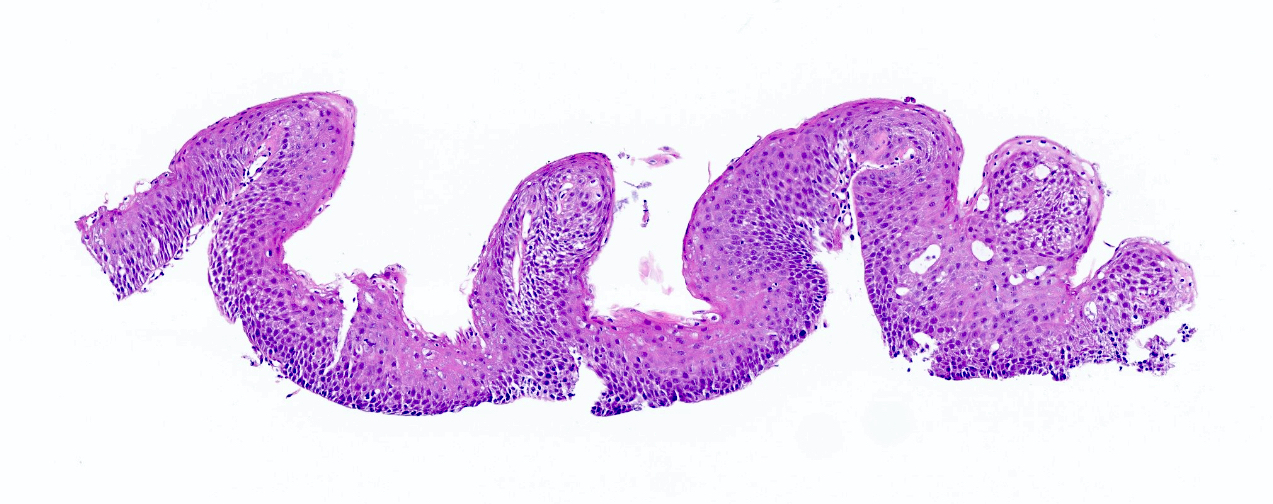
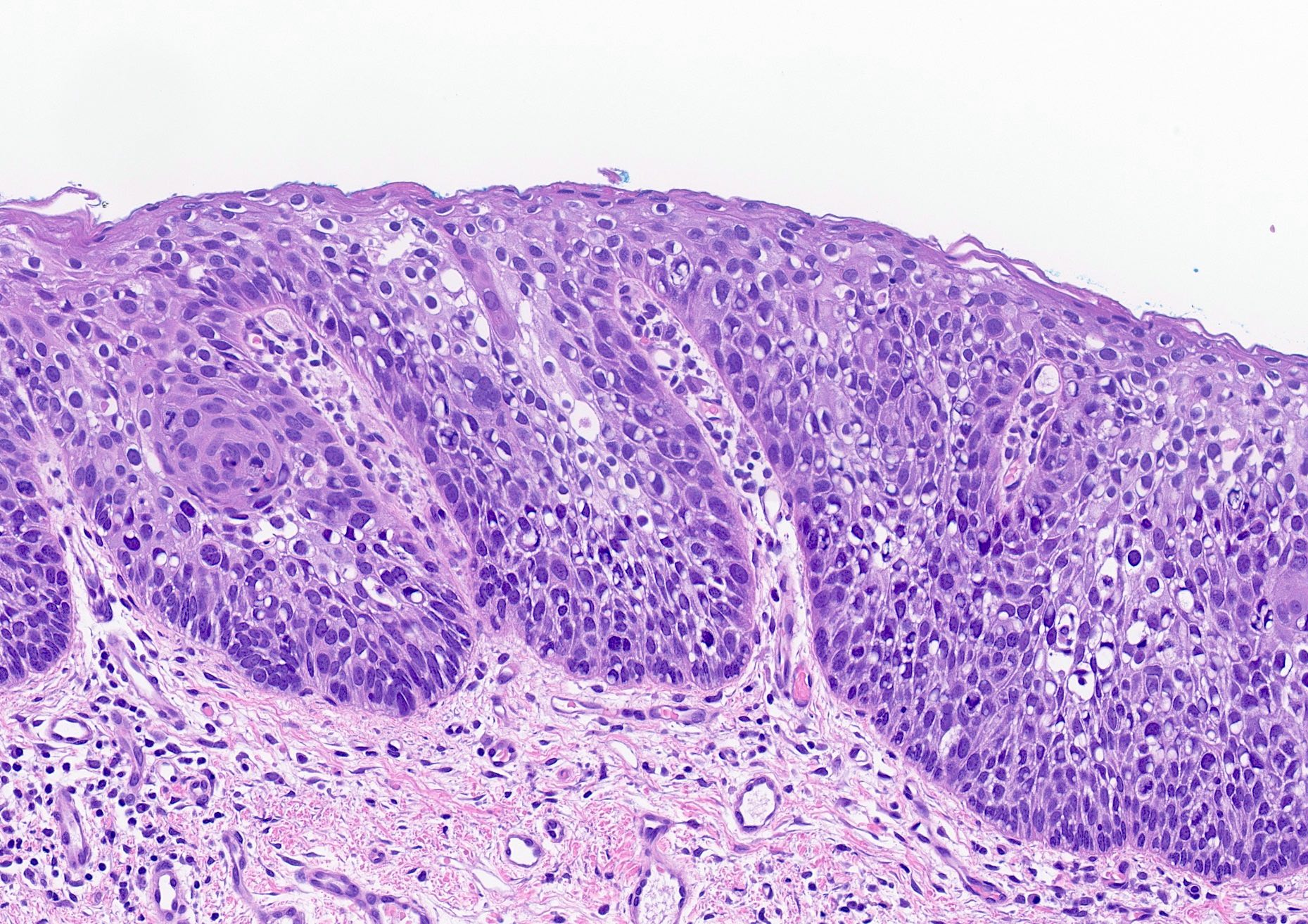
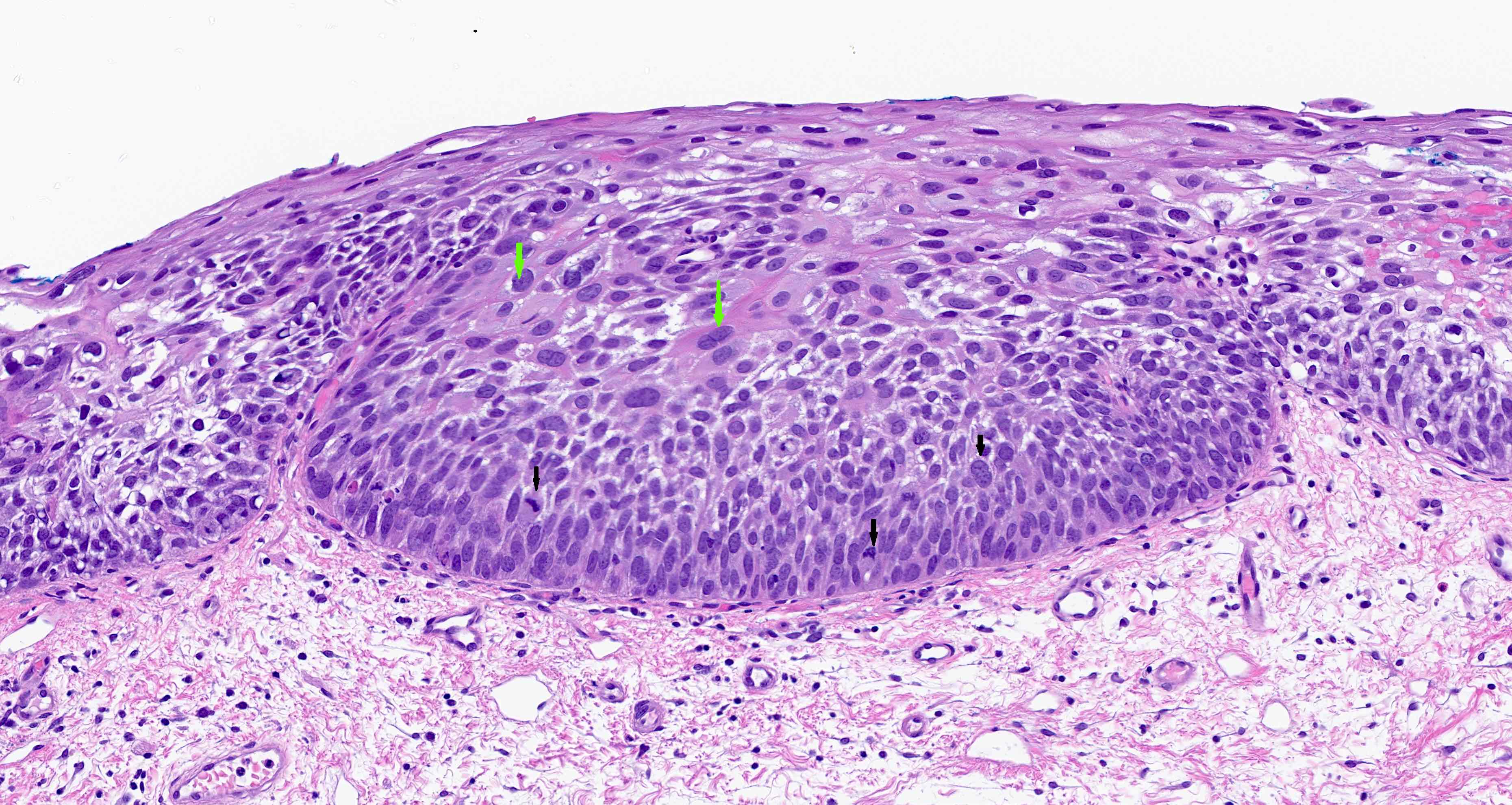
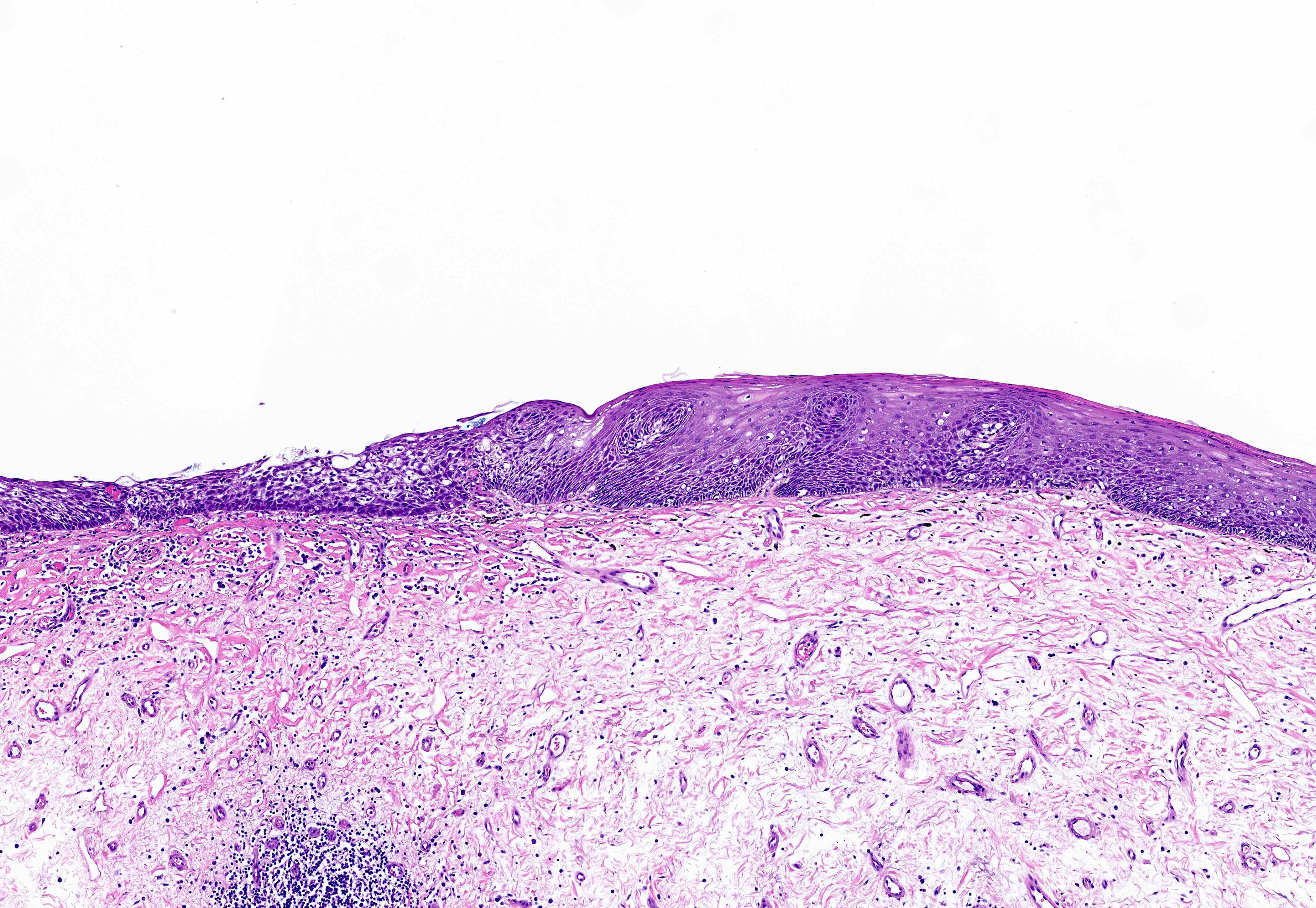
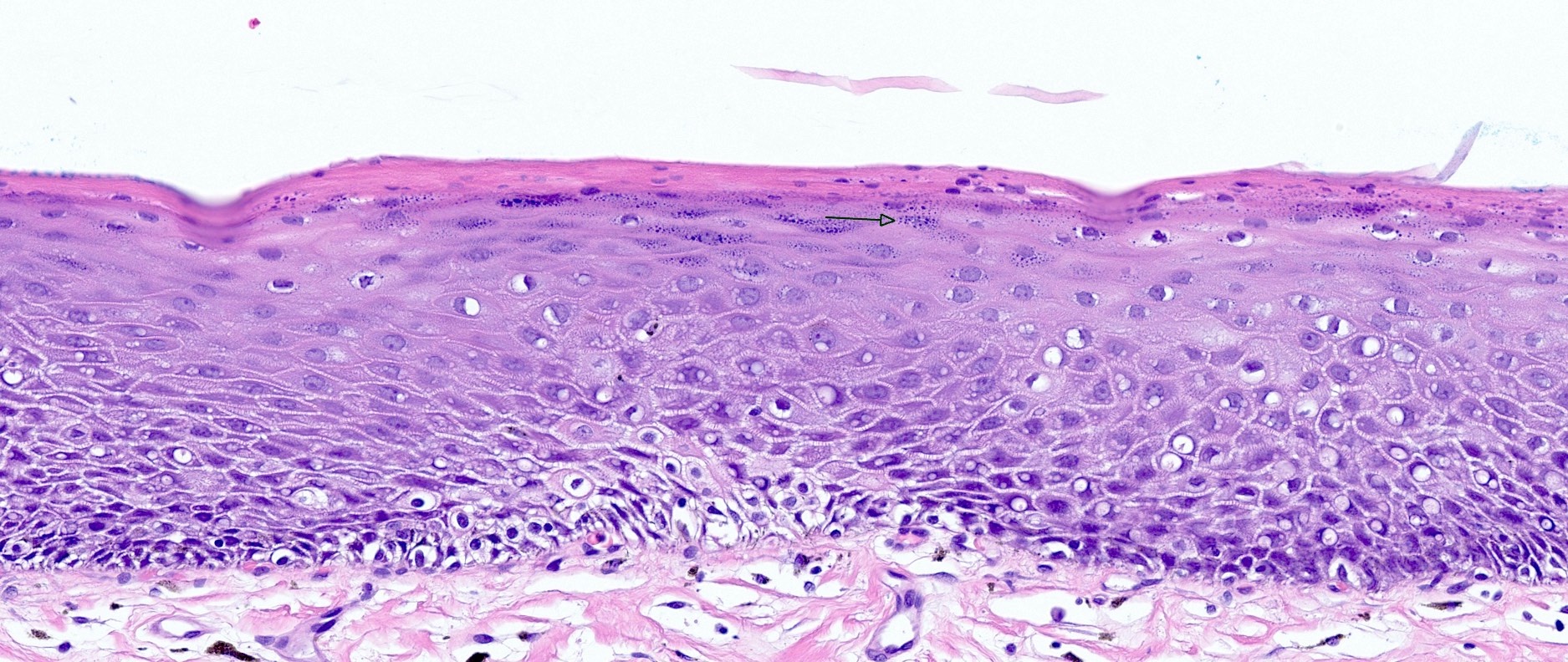
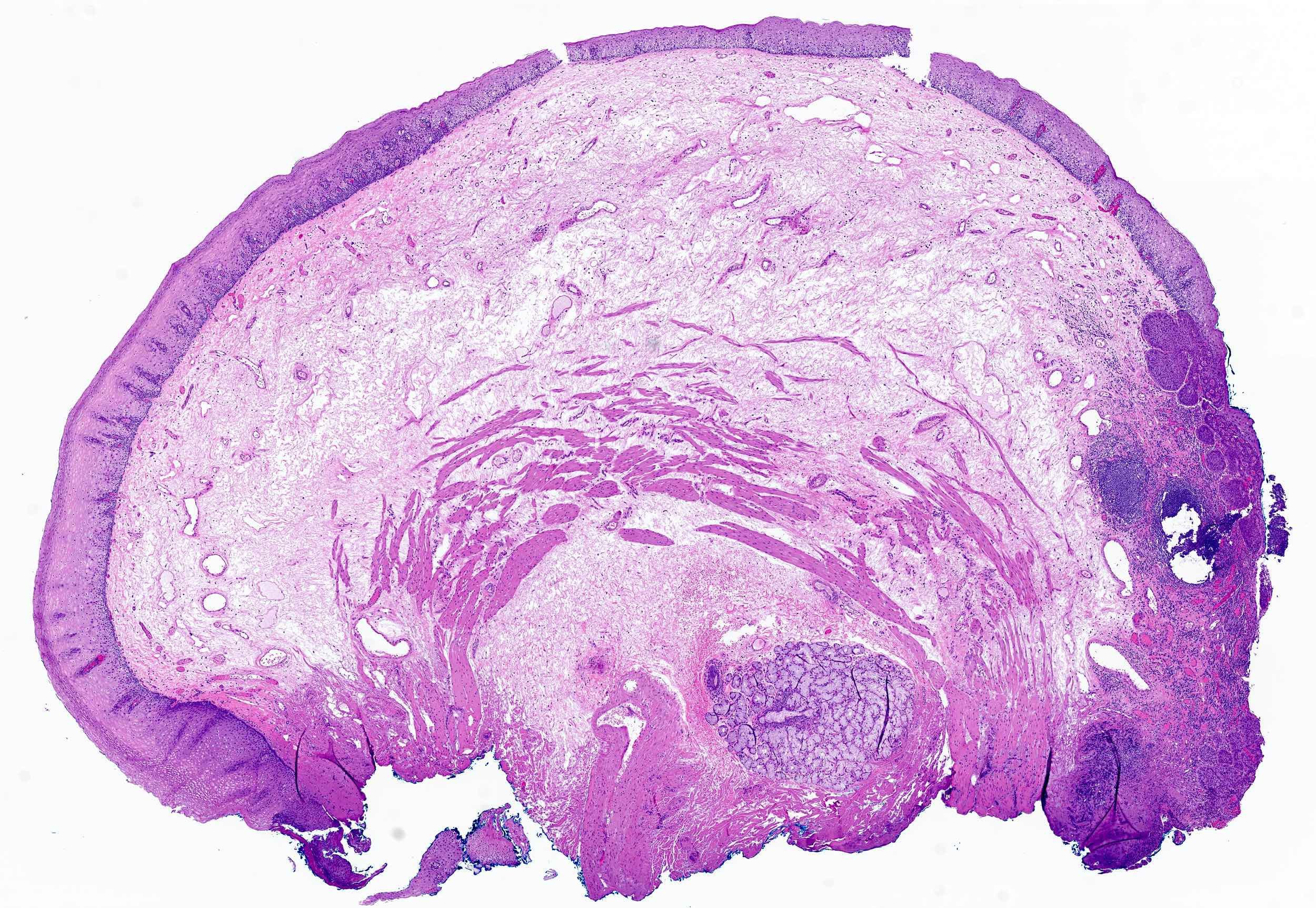
Microscopic (histologic) description
- Nuclear enlargement and irregularity, anisonucleosis and nuclear pleomorphism
- Hyperchromasia with irregular nuclear contours
- Increased N:C ratio
- Increased mitotic activity
- Abnormal epithelial maturation with increased cellularity of superficial mucosa
- 2 tiered microscopic grading system
- Low grade: involvement of the lower half of the epithelium only, with mild atypia
- High grade: neoplastic cells occupy > 50% of epithelial thickness or severe cytologic atypia
- Reference: Mod Pathol 2017;30:S112
Microscopic (histologic) images
Positive stains
- p53 mutant pattern, especially in cases of high grade dysplasia (77 - 93% of high grade dysplasia cases) (Dig Dis 2023;41:685, Hum Pathol 2011;42:1430)
- Increased Ki67 proliferation (Hum Pathol 2011;42:1430)
Molecular / cytogenetics description
- Overexpression of p53 and hypermethylation of CDKN2A (Cancer Epidemiol Biomarkers Prev 2013;22:540)
Videos
Squamous dysplasia screening and treatment
Sample pathology report
- Esophagus, endoscopic biopsy:
- High grade squamous dysplasia
- Esophagus, endoscopic mucosal resection:
- High grade squamous dysplasia
- Margins are negative for dysplasia
Differential diagnosis
- Reparative epithelial changes or pseudoepitheliomatous hyperplasia:
- Prominent nucleoli and accompanying inflammatory process suggests a reactive process
- Benign hyperplasia of the epithelial rete ridges that mimics dysplasia but lacks cytological atypia
- Squamous papilloma:
- Endoscopically present as a papillary wart-like growth
- Histologically characterized by papillary hyperplasia of the squamous layer without dysplasia
- Microinvasive squamous cell carcinoma:
- More atypia and pleomorphism
- Invasion beyond basement membrane
Additional references
Board review style question #1
Board review style answer #1
A. Epidermoid metaplasia. Epidermoid metaplasia (leukoplakia) is thought to represent a precursor lesion to esophageal squamous dysplasia, although the magnitude of risk is unknown. Answer B is incorrect because intestinal metaplasia (i.e., Barrett esophagus) is a precursor for glandular dysplasia in the esophagus. Answer C is incorrect because pancreatic acinar metaplasia is usually an incidental finding seen at the gastroesophageal (GE) junction with no known neoplastic risk. Answer D is incorrect pyloric gland metaplasia is usually seen in the intestine and not in the esophagus.
Comment Here
Reference: Squamous dysplasia
Comment Here
Reference: Squamous dysplasia
Board review style question #2
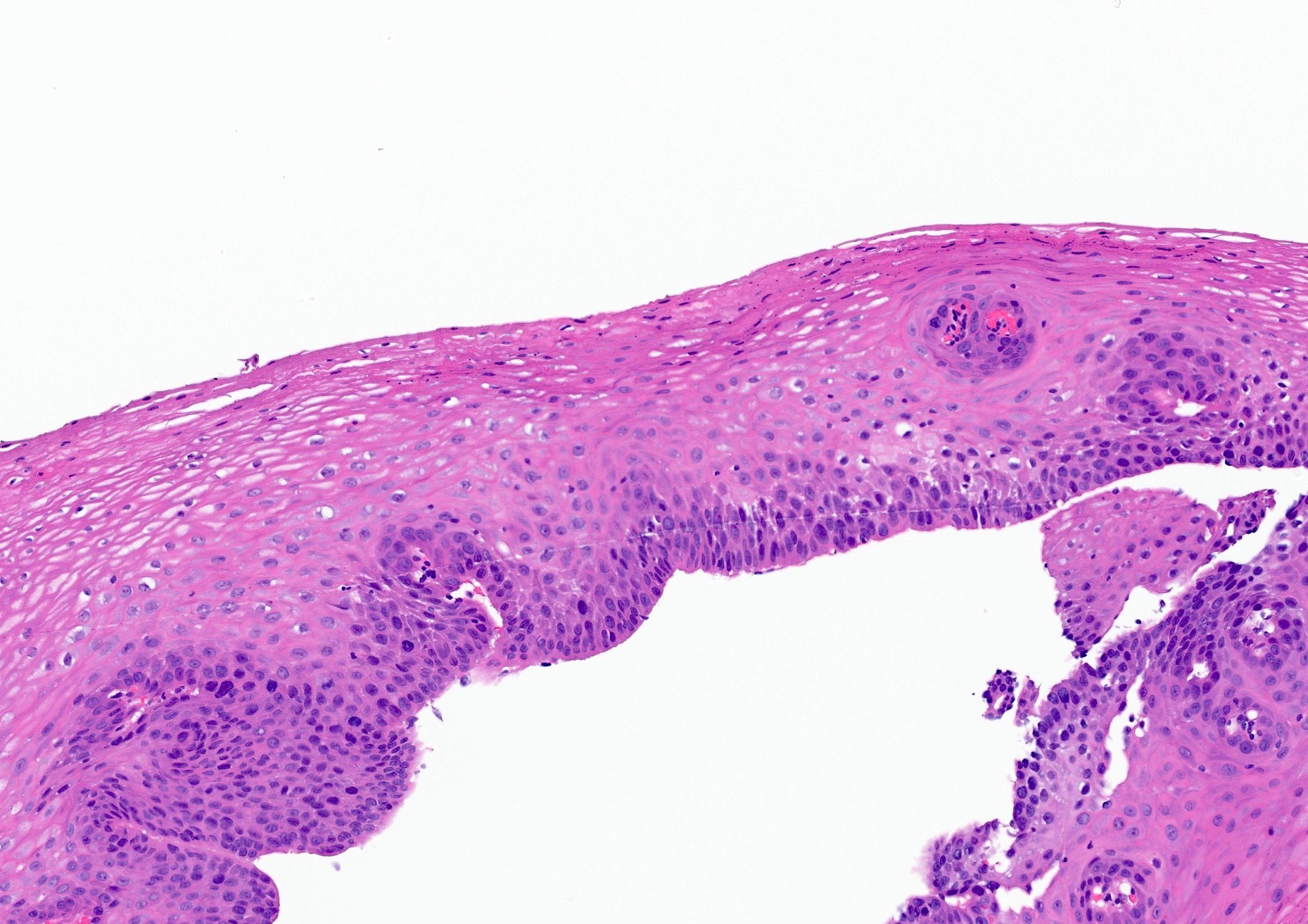
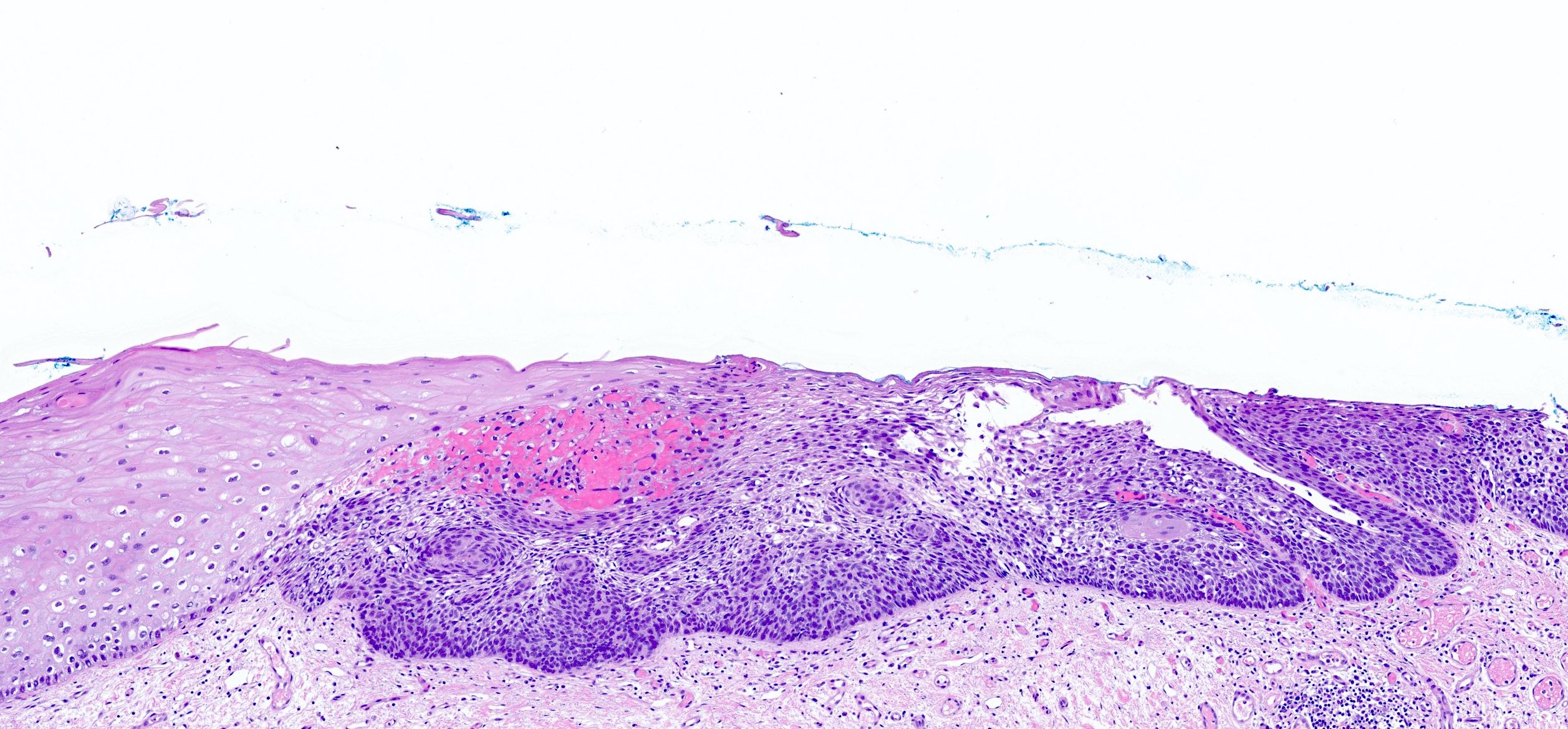
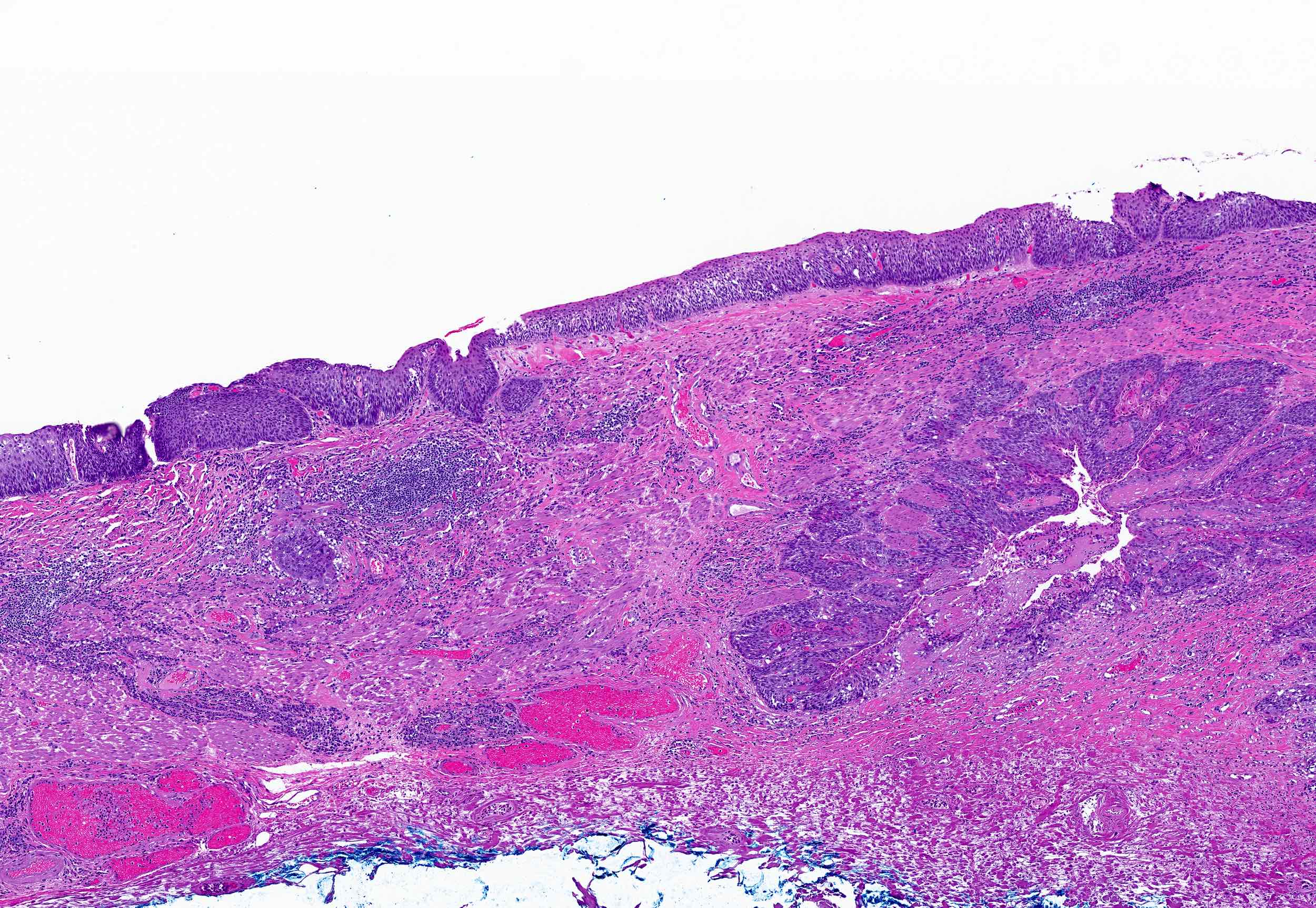
The image above shows an endoscopic biopsy of a lesion noted as a white plaque that did not stain with Lugol iodine in the middle third of the esophagus. What is your diagnosis?
- Barrett esophagus with dysplasia
- High grade squamous dysplasia
- Low grade squamous dysplasia
- Reactive atypia, negative for dysplasia
Board review style answer #2
B. High grade squamous dysplasia. A full thickness high grade squamous esophageal dysplasia with cytologic atypia is seen on the right side of the image with sharp demarcation from the normal nondysplastic squamous epithelium on the left. Answer C is incorrect because low grade dysplasia encompasses less than half of the mucosa. Answer A is incorrect because Barrett esophagus or intestinal metaplasia, which by definition is columnar epithelium with or without goblet cells that extends ≥ 1 cm proximal to the gastroesophageal junction, is commonly seen in distal esophagus and gastroesophageal (GE) junction. Answer D is incorrect because the full thickness atypia present exceeds what would be expected for reactive atypia.
Comment Here
Reference: Squamous dysplasia
Comment Here
Reference: Squamous dysplasia