Table of Contents
Definition / general | Essential features | Terminology | Anatomy | Embryology | Diagrams / tables | Clinical features | Laboratory | Radiology images | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Stringham N. Anatomy, embryology & histology. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagusnormalhistology.html. Accessed April 1st, 2025.
Definition / general
- Esophagus is a muscular tube that extends from the pharynx to the gastroesophageal junction; it has typical gastrointestinal (GI) tract layering (mucosa, submucosa, muscularis propria / externa, adventitia) around a central lumen as well as 2 muscular sphincters (upper and lower)
Essential features
- Esophageal tissue is arranged in 4 concentric layers following typical GI layering: mucosa, submucosa, muscularis propria / externa, adventitia
- Mucosa lines the lumen of the esophagus and is composed of epithelium (nonkeratinized stratified squamous), lamina propria and muscularis mucosae
- Submucosa lies just deep to the mucosa and comprises connective tissue, nerves, Meissner plexus, lymph and blood vessels and submucosal glands
- Muscularis propria / externa is composed of 2 concentric layers of muscle cells; these muscle cells are a variable mixture of skeletal and smooth muscle with a greater proportion of skeletal muscle at the proximal end of the esophagus transitioning to solely smooth muscle at the distal end
- Esophagus is primarily retroperitoneal and is covered in a connective tissue adventitia and fascia
Terminology
- Oesophagus
- Gullet
Anatomy
- Esophagus is a muscular tube that extends from the oral cavity / pharynx to the stomach; in an adult it is ~25 cm in length (Richter: The Esophagus, 6th Edition, 2021)
- Esophagus has cervical, thoracic and abdominal portions; it transitions from the cervical to thoracic region at the suprasternal notch and then passes from the thorax to the abdomen through the diaphragmatic hiatus
- In axial cross section, esophagus is located posterior to the trachea and anterior to the vertebral column
- Esophagus extends from cricopharyngeus muscle in pharynx (level of C6) to lower esophageal sphincter at gastroesophageal junction (T11 / T12)
- Gastroesophageal / esophagogastric (EGJ) junction
- Macroscopically: the point of flaring of tubular esophagus or proximal limit of gastric rugal folds
- Endoscopically: the Z (zigzag) line at the irregular boundary of squamous and columnar mucosa in distal esophagus; usually 2 - 3 cm
- Main function of esophagus is to move food from pharynx to stomach via peristalsis
- Submucosal glands secrete HCO3 and mucin to maintain esophageal moisture and to protect against refluxed gastric acid (Am J Physiol Gastrointest Liver Physiol 2005;288:G736)
- No other significant secretory or absorptive functions
- Arterial blood supply of the esophagus is generally arranged in segments with the inferior thyroid artery supplying the upper esophageal sphincter and cervical esophagus, the aortic esophageal arteries supplying the thoracic esophagus and the left gastric artery and a branch of the left phrenic artery supplying the distal esophagus and lower esophageal sphincter
- Esophageal infarction is rare due to the abundant blood supply
- Venous drainage depends on esophageal region but initially is into the periesophageal venous plexus
- Upper third (periesophageal venous plexus) → inferior thyroid vein → superior vena cava (via subclavian / brachiocephalic)
- Middle third (periesophageal venous plexus) → azygous vein → superior vena cava
- Lower third (periesophageal venous plexus) → gastric veins → portal system
- Connection between caval and portal venous systems can explain esophageal varices due to portal hypertension
- Lymphatic drainage is via freely anastomosing networks in submucosa, muscularis propria and occasionally lamina propria
- Upper third drains into paratracheal and internal jugular nodes
- Middle third to mediastinal nodes
- Lower third to nodes around aorta and celiac axis
- Can facilitate lengthwise tumor dissemination
- Parasympathetic and sympathetic innervation of the esophagus is via the vagus and spinal nerves (sympathetic chain) (J Clin Gastroenterol 2008;42:610)
- Auerbach plexus (that lies between the longitudinal and circular layers of the muscularis propria) regulates contraction of the outer muscular layers of the esophagus
- Meissner plexus (submucosa) regulates contraction of the muscularis mucosae as well as glandular secretion
Embryology
- Embryologically, esophagus develops from foregut at ~10 weeks; upper esophagus is derived from branchial arches 4 - 6 (StatPearls: Embryology, Esophagus [Accessed 10 July 2024])
- ~4 weeks: gut tube precursor is formed from the resulting innermost layer of the folding trilaminar disc
- Foregut component that gives rise to esophagus also gives rise to trachea and lungs
- Foregut endoderm gives rise to esophageal epithelium and mucosal glands
- Mesoderm surrounding foregut gives rise to smooth and skeletal muscle of esophagus
- ~6 weeks: circular and longitudinal muscle layers begin to form and myenteric plexus develops; cells of neural crest migrate to give rise to submucosal plexus
- ~7 weeks: blood supply begins to form via proliferation of mesodermal cells into submucosa
- ~9 weeks muscle layers are complete; cranial to caudal distinction of muscle types
- At 4 months, submucosal glands appear due to downward growth of columnar cells; columnar epithelium of the foregut begins to transition into squamous epithelium (continues into third trimester)
Diagrams / tables
Clinical features
- Esophageal tumors spread to involve local organs more easily than in other areas of the GI tract because the esophagus is not covered in a serosa; this also makes these tumors harder to treat surgically (Silverman: Oncologic Imaging - A Multidisciplinary Approach, 2nd Edition, 2022)
- Gastroesophageal reflux disease (GERD) can cause chronic esophageal irritation that induces epithelial metaplasia (i.e., Barrett esophagus); this induces an epithelial replacement of cells from the normal stratified squamous to intestinal columnar epithelium with goblet cells (Gastrointest Endosc 2017;85:889)
- AJCC regions: location of esophageal cancer primary site with approximate endoscopic measurements (distance listed in cm from incisors)
- Cervical: lower border of cricoid cartilage (~15 cm) to suprasternal notch / thoracic inlet (~20 cm), contains striated muscle
- Upper thoracic: suprasternal notch (~20 cm) to tracheal bifurcation (~25 cm), contains striated and smooth muscle
- Middle thoracic: tracheal bifurcation (~25 cm) to diaphragmatic hiatus (~30 cm), contains striated and smooth muscle
- Lower thoracic and esophagogastric junction (EGJ): diaphragmatic hiatus (~30 cm) and extending past diaphragm and including lower esophageal sphincter and EGJ (~42 cm); contains smooth muscle only
- Cancers involving EGJ with epicenter within the proximal 2 cm of cardia are staged as esophageal cancer; whereas epicenters > 2 cm distal to EGJ are staged as gastric cancer
- Reference: J Thorac Oncol 2017;12:36
Laboratory
- Biopsy is performed via endoscopy for evaluation of esophageal tissue; diagnostic accuracy is high for identification of malignant versus infectious diseases, as well as in evaluation for dysplasia (Gastrointest Endosc Clin N Am 2000;10:713)
Gross description
- Esophagus is a muscular tube that extends from the oral cavity / pharynx to the stomach; in an adult, it is ~25 cm in length (Richter: The Esophagus, 6th Edition, 2021)
- Esophagus has typical GI layering: mucosa, submucosa, muscularis propria / externa, adventitia
- 2 muscular sphincters are present: upper and lower esophageal sphincters
- Primarily retroperitoneal and is therefore covered in a connective tissue adventitia and fascia
- In axial cross section, esophagus is located posterior to trachea and anterior to the vertebral column
Microscopic (histologic) description
- Esophagus is arranged in 4 concentric layers following a typical GI layering scheme; listed from the lumen outward, these layers are mucosa, submucosa, muscularis propria / externa, adventitia
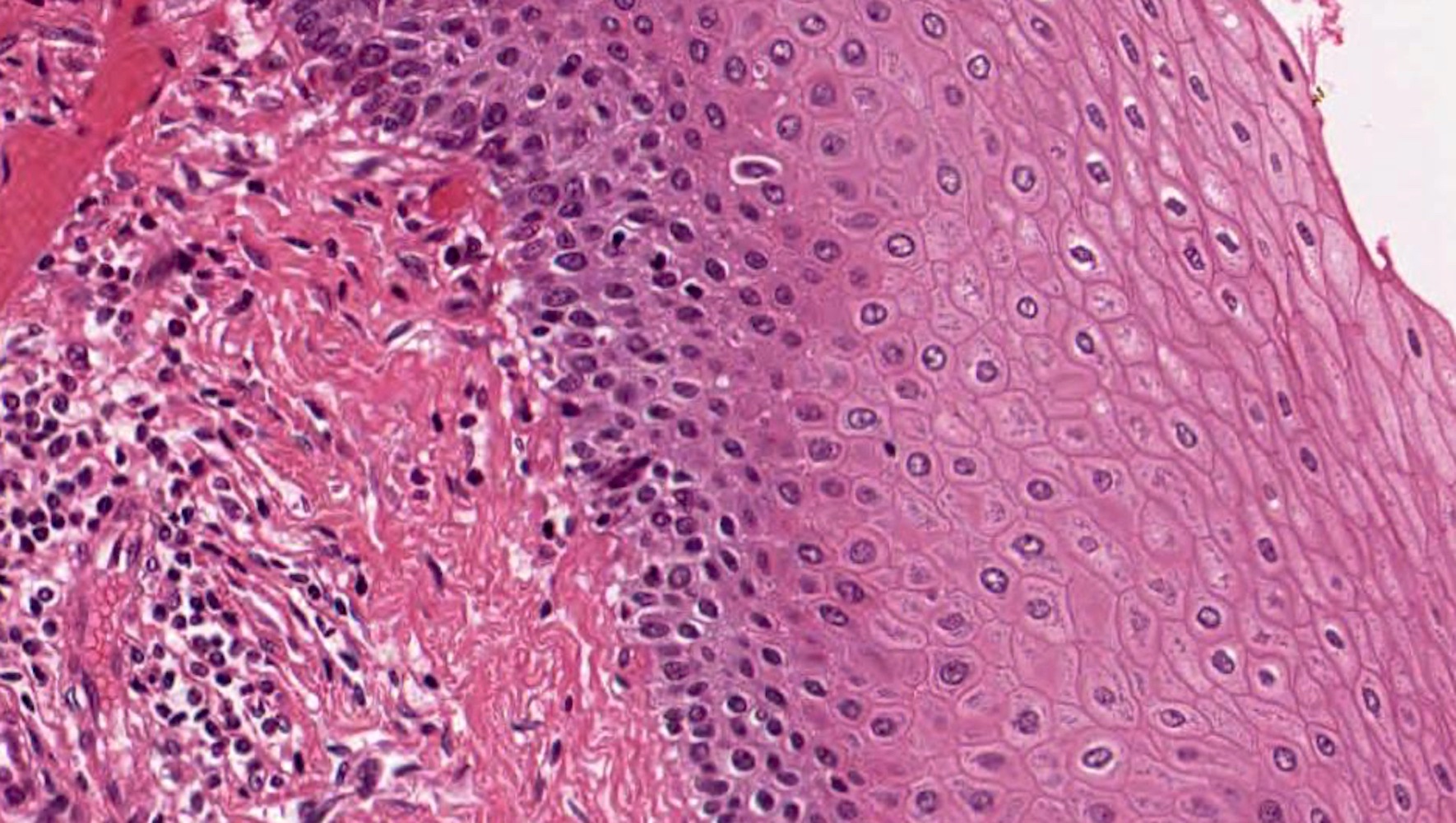
- Esophageal mucosa
- Epithelium: nonkeratinized stratified squamous epithelium
- Innermost layer of the esophageal mucosa, lining the lumen
- Other cells present: melanocytes, endocrine cells, Langerhans cells, Merkel cells, T cells
- Basement membrane separates the epithelium from the underlying lamina propria
- Basal layer: < 15% of the mucosal thickness, usually 2 - 3 cells thick, comprised of basophilic proliferative cells with minimal cytoplasm, mitotic figures are found only here (under normal conditions) (Richter: The Esophagus, 6th Edition, 2021)
- Intermediate layer: these glycogen rich squamous cells have more cytoplasm than those of the basal layer (i.e., decreased N:C ratio)
- Superficial layer: cells appear more flattened as they mature and approach the lumen, many cells are anucleate
- Lamina propria: composed of loose fibrovascular connective tissue
- Situated between the epithelium and muscularis mucosae
- Folds form papillae; these usually extend ~33 - 50% of epithelial thickness (Richter: The Esophagus, 6th Edition, 2021)
- Scattered inflammatory cells may be present
- Muscularis mucosae: composed of smooth muscle
- Begins proximally at the cricoid cartilage and becomes thickened distally
- In the lower esophagus, it may play a protective role against stomach acid erosion (Ann N Y Acad Sci 2013;1300:261)
- May resemble muscularis propria / externa, which is important for accurate American Joint Committee on Cancer (AJCC) staging of adenocarcinoma in this region (J Thorac Dis 2014;6:S289)
- Epithelium: nonkeratinized stratified squamous epithelium
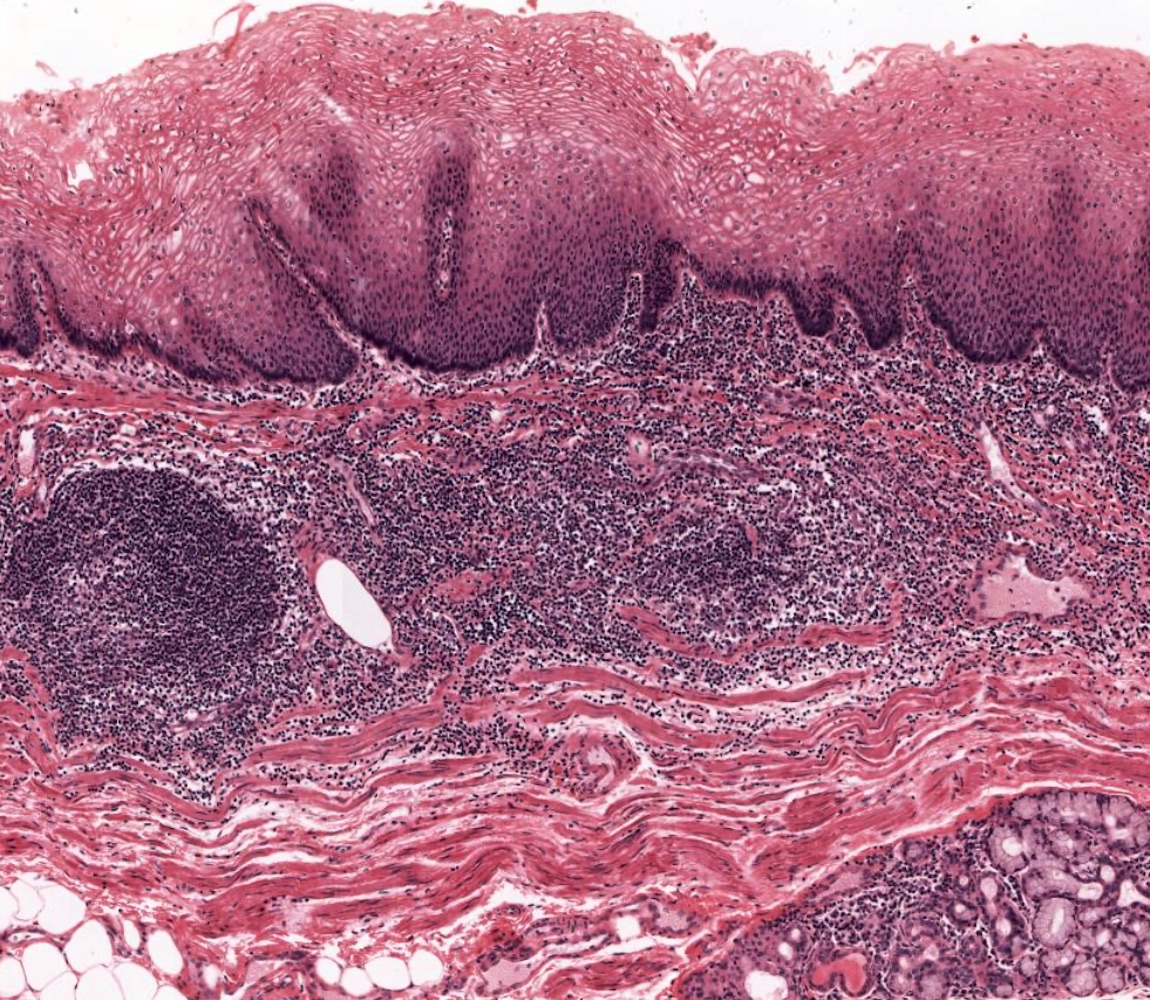
- Submucosa: connective tissue
- Contains fibroblasts / collagen, nerves, sparse ganglia (Meissner plexus), lymphatic channels, blood vessels and submucosal (seromucous) glands
- Submucosal glands are comprised of mucinous cells surrounding a central lumen that produce acid mucin and empty into the esophagus via squamous lined ducts
- Submucosal glands are a significant identifying landmark of esophagus on biopsy or resection specimen (Richter: The Esophagus, 6th Edition, 2021)
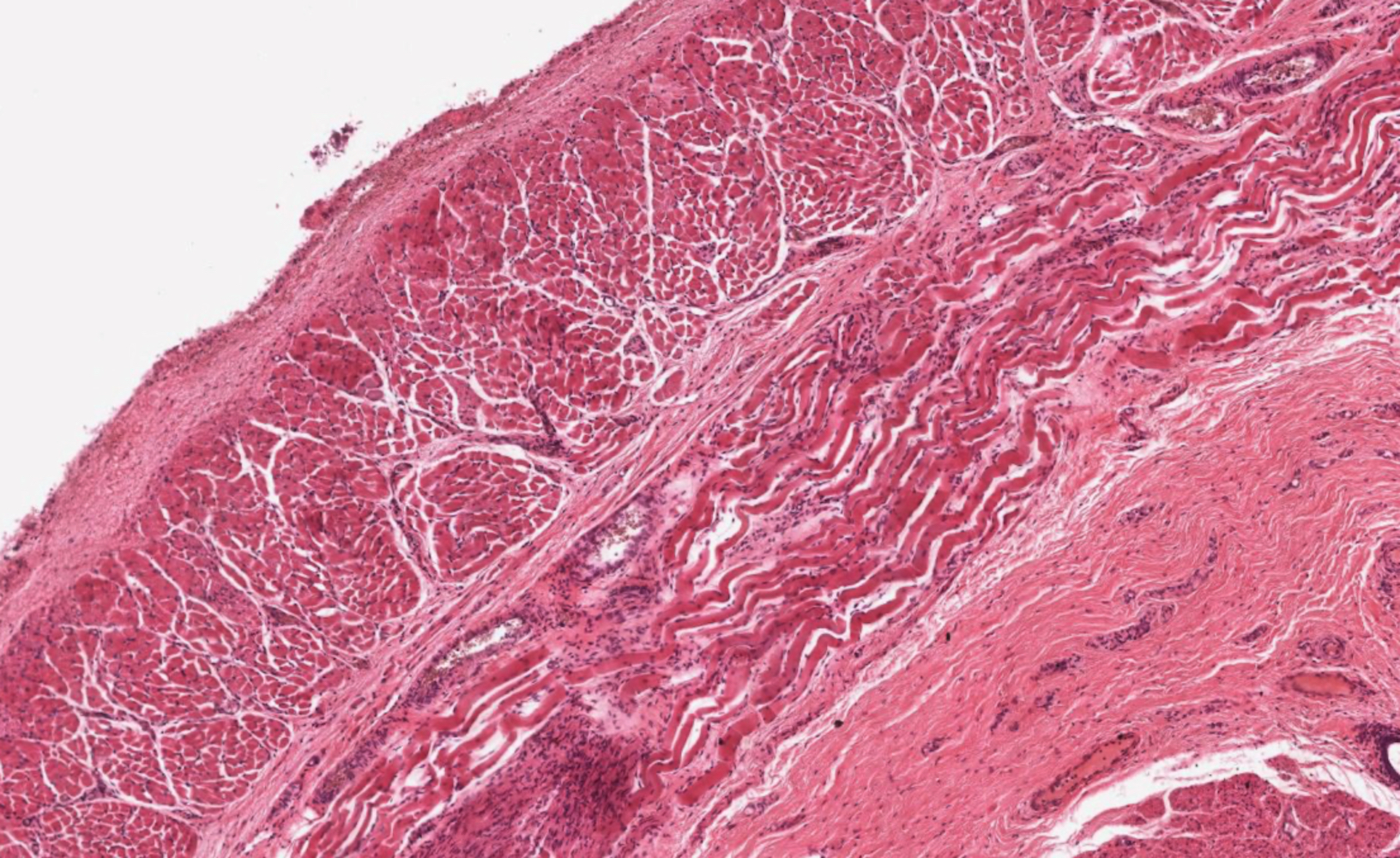
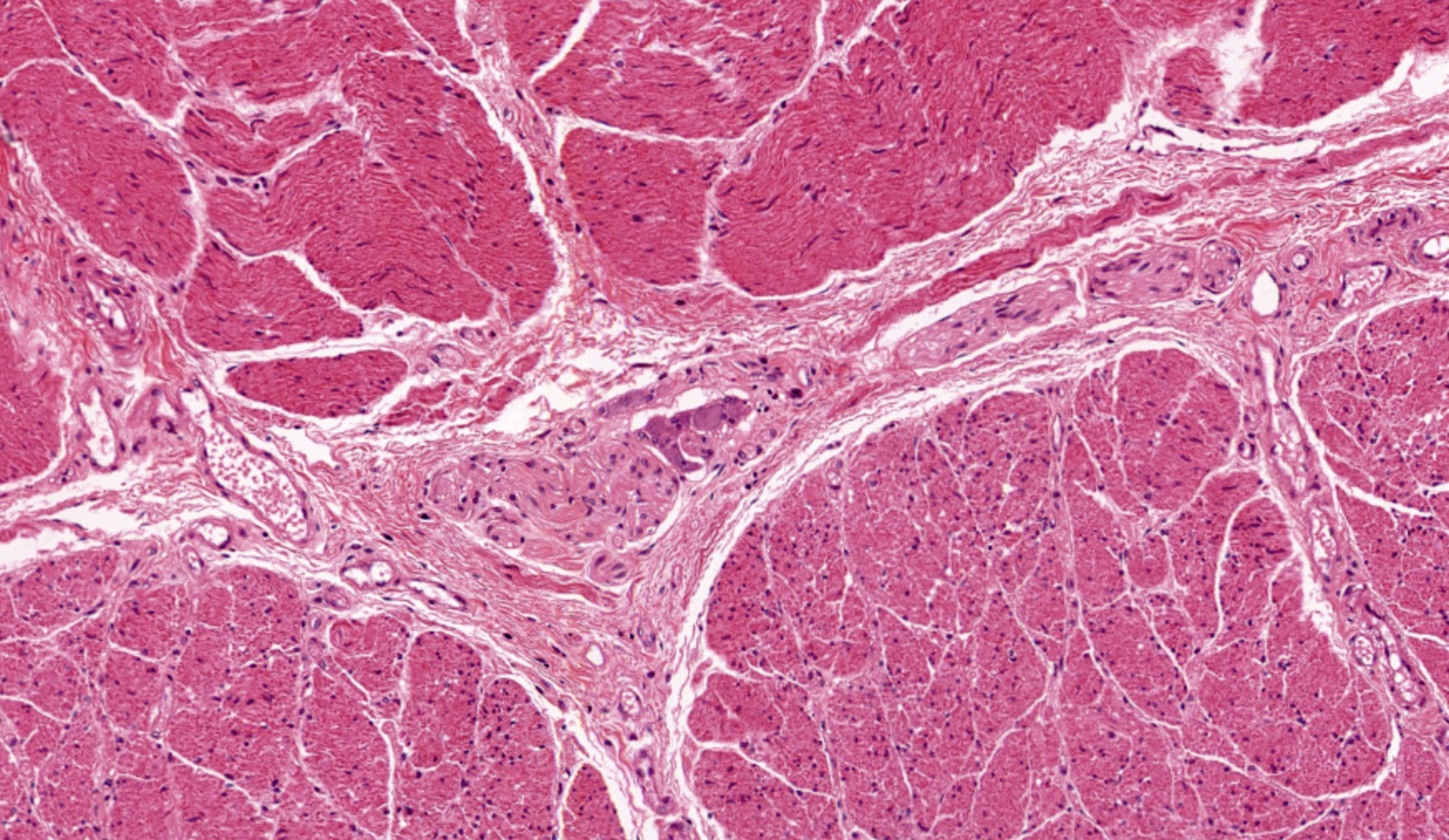
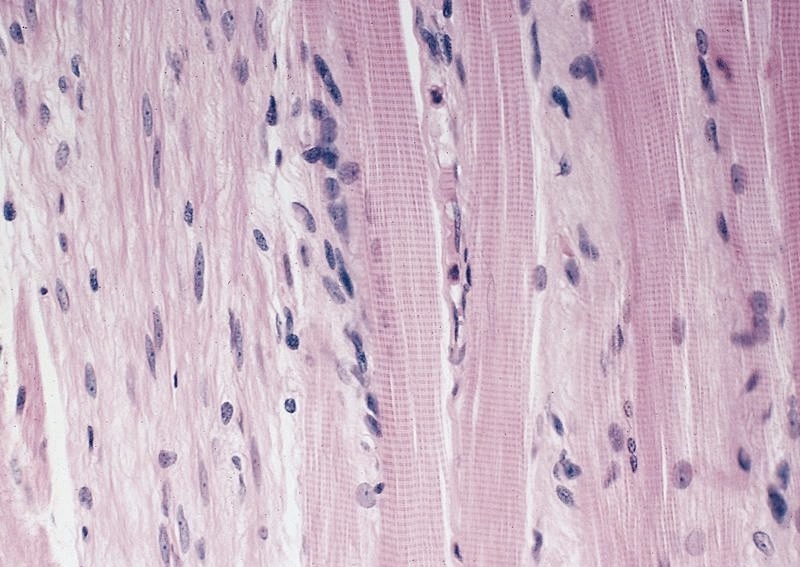
- Muscularis propria (i.e., muscularis externa)
- Composed of striated skeletal muscle in the proximal third of the esophagus, smooth muscle in the distal third and a mixture of both skeletal and smooth muscle in the middle third
- Inner layer is oriented circumferentially while the outer layer is oriented longitudinally; this allows for both segmental contraction and peristalsis
- Myenteric plexuses (nerves and ganglia) are found between the inner and outer layer
- Adventitia: composed of loose irregular connective tissue
- Esophagus is primarily retroperitoneal and the majority is surrounded by fascia
Microscopic (histologic) images
Contributed by Nicole Stringham, Ph.D. (sources: University of Michigan virtual slide box and Duke University virtual slide collection) and AFIP
Virtual slides
Cytology description
- Esophageal brushing specimens are usually composed of mature superficial type and intermediate type squamous cells with abundant cytoplasm and small, round, regular nuclei
- Superficial type nuclei are dense and pyknotic; intermediate type contain finely granular chromatin and inconspicuous nucleoli
- Cells present as loosely cohesive aggregates, individual cells, large sheets
- Brush cytology may be helpful in the diagnosis of Barrett esophagus (Diagn Cytopathol 2011;39:60)
Positive stains
- PASD and Alcian blue (at pH 2.5) are positive in submucosal glands
- CK7, CK8/18, CK14 and CK19 are positive in ducts
- CK10 and CK13 are positive in normal stratified squamous epithelium (Prz Gastroenterol 2015;10:61)
Negative stains
- Methylene blue is helpful for distinguishing areas of dysplastic columnar epithelium associated with Barrett esophagus (95% accuracy) (Gastrointest Endosc 1996;44:1)
- CDX2 negative in normal stratified epithelium (positive in 87.5% of Barrett esophagus) (Prz Gastroenterol 2015;10:61)
Electron microscopy description
- Cytoarchitecture of the muscularis mucosae and distribution of lymphatic vessels varies between regions of the esophagus (i.e., cervical, thoracic, abdominal); this may affect esophageal cancer infiltration and lymph node metastasis (Esophagus 2019;16:44)
Electron microscopy images
Videos
Normal esophagus histology
Additional references
Board review style question #1
Which of the following cell types comprise the innermost lumen lining layer of a normal esophagus?
- Columnar epithelium with goblet cells
- Keratinized stratified squamous epithelium
- Low columnar epithelium
- Nonkeratinized stratified squamous epithelium
- Simple columnar epithelium
Board review style answer #1
D. Nonkeratinized stratified squamous epithelium. The innermost layer of the esophageal mucosa, lining the lumen, is made up of nonkeratinized stratified squamous epithelium. Answer A is incorrect because columnar epithelium is normally found in the small intestine but can be found in the esophagus in cases of dysplasia (Barrett esophagus). Answer B is incorrect because keratinized epithelium is generally associated with skin (epithelium on outward facing surfaces of the body). Answer C is incorrect because low columnar epithelium is a type of simple columnar epithelium and is typical of the stomach and intestines, not the esophagus. Answer E is incorrect because simple columnar epithelium is usually found in other areas of the gastrointestinal (GI) tract.
Comment Here
Reference: Esophagus - Anatomy, embryology & histology
Comment Here
Reference: Esophagus - Anatomy, embryology & histology
Board review style question #2
The image shown above is in need of evaluation. Features that are present, both in the image and in subjacent areas, include gastrointestinal (GI) layering, Auerbach plexus, submucosal glands and 2 distinct layers of muscularis propria made of smooth and skeletal muscle. What is the anatomical origin of this sample?
- Anus
- Duodenum
- Large intestine
- Pylorus
- Upper esophagus
Board review style answer #2
E. Upper esophagus. The upper esophagus is the only listed option that has nonkeratinized stratified squamous epithelium (shown in the image) in addition to all of the other listed features. Answer A is incorrect because the anus does not have submucosal glands. Answer B is incorrect because although the duodenum has many of these features, including submucosal glands, it does not have skeletal muscle and is lined by simple columnar (enterocytes) and goblet epithelial cells. Answer C is incorrect because the large intestine is lined by enterocytes with goblet cells and has mucosal rather than submucosal glands. Answer D is incorrect because the pylorus does not have 2 layered muscularized propria with skeletal muscle and the epithelium is simple columnar, not squamous.
Comment Here
Reference: Esophagus - Anatomy, embryology & histology
Comment Here
Reference: Esophagus - Anatomy, embryology & histology