Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: George GV, Huber AR. Glycogenic acanthosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagusglycogenic.html. Accessed April 1st, 2025.
Definition / general
- Glycogenic acanthosis (GA) is a benign hyperplasia of the esophageal squamous epithelium due to accumulation of intracytoplasmic glycogen of unknown etiology
- Endoscopically, affected areas display white plaques or nodular areas (usually 2 - 10 mm in diameter), which may be solitary, multiple or coalesced
- Diffuse glycogenic acanthosis may be a manifestation of PTEN hamartoma tumor syndrome (Cowden syndrome) in 20 - 80% of affected adults (Best Pract Res Clin Gastroenterol 2022;58:101792)
Essential features
- First described by Rywlin and Ortega in 1970, glycogenic acanthosis of the esophagus is a common benign lesion seen during upper gastrointestinal endoscopy
- Characterized histologically by squamous hyperplasia and intracellular glycogen accumulation
- Manifestation of PTEN hamartoma tumor syndrome (Cowden syndrome)
- References: Am J Med Genet A 2003;122A:315, Am J Gastroenterol 2003;98:1429, Am J Gastroenterol 1997;92:1038, Arch Pathol 1970;90:439, Gastrointest Radiol 1984;9:93
Terminology
- Pachyderma nodosa, esophageal leukoplakia
ICD coding
- ICD-10: K22.9 - disease of esophagus, unspecified
Epidemiology
- Most common in adults with a mean age of 52 years (range: 45 - 79 years)
- Common incidental endoscopic finding seen in up to 3.5% of upper endoscopies
- Diffuse involvement of the esophagus is associated with PTEN hamartoma tumor syndrome (Cowden syndrome) and highly predictive of PTEN mutation (80 - 90% of patients)
- PTEN hamartoma tumor syndrome (Cowden syndrome) is an autosomal dominant multiple hamartoma syndrome with increased risk of malignant tumors (breast, thyroid and endometrial) due to germline mutations in the tumor suppressor gene PTEN on 10q23
- There are rare reported cases in patients with tuberous sclerosis complex (J Clin Gastroenterol 1994;19:46)
- Reported associations with reflux esophagitis (GERD), increasing age, eosinophilic esophagitis and celiac disease
- References: World J Gastroenterol 2015;21:1091, Prz Gastroenterol 2020;15:39, Acta Paediatr 2004;93:568, J Pediatr Gastroenterol Nutr 2021;72:e161
Sites
- Esophagus, primarily in the mid esophagus (AJR Am J Roentgenol 1995;164:96)
- Rare reports of laryngeal involvement (Laryngoscope 2022;132:1641, Arch Otolaryngol Head Neck Surg 1998;124:1029, Otolaryngol Head Neck Surg 2021;164:1153)
Pathophysiology
- Unknown (see Etiology)
Etiology
- Although the etiology of glycogenic acanthosis is unknown, it is strongly associated with PTEN hamartoma tumor syndrome (Cowden) syndrome
- Glycogenic acanthosis has also been associated with tuberous sclerosis, hiatal hernia, reflux esophagitis (GERD) and increased age
- Rare reports have noted a possible association with eosinophilic esophagitis or celiac disease
- Glycogenic acanthosis has not been found to be associated with disorders of glucose metabolism (diabetes) or skin disorders (psoriasis or acanthosis nigricans)
- Given an association with GERD, a postinflammatory hypothesis was raised but has not been proven
- References: Prz Gastroenterol 2020;15:39, Am J Med Genet A 2003;122A:315, Acta Paediatr 2004;93:568, J Pediatr Gastroenterol Nutr 2021;72:e161, AJR Am J Roentgenol 1995;164:96
Clinical features
- See Etiology and Epidemiology
Diagnosis
- Ultimately, the diagnosis is based on the characteristic histologic findings in endoscopic biopsies (see Microscopic (histologic) description)
Radiology description
- May be seen in ~30% of patients undergoing double contrast radiography
- Mucosal nodules or plaques ranging from 2 to 15 mm in diameter
- Some have sharp edges that are demarcated by the barium, while others have ill defined borders that blend into the surrounding mucosa
- References: AJR Am J Roentgenol 1982;139:683, AJR Am J Roentgenol 1995;164:96
Prognostic factors
- Nonneoplastic and benign
- Solitary lesions have no clinical significance
- Prognosis of glycogenic acanthosis with PTEN hamartoma tumor syndrome (Cowden syndrome) is determined by the risk of various malignant tumors (breast, thyroid, kidney, endometrium or colorectal)
- Reference: Yantiss: Diagnostic Pathology - GI Endoscopic Correlation, 1st Edition, 2014
Case reports
- 6 year old boy and 8 year old girl with anemia and failure to thrive (Acta Paediatr 2004;93:568)
- 14 year old boy with eosinophilic esophagitis diagnosed with glycogenic acanthosis (J Pediatr Gastroenterol Nutr 2021;72:e161)
- 36 year old man with a history of gastrointestinal polyps (Eur J Gastroenterol Hepatol 2007;19:513)
- 45 year old man with a history of Cowden syndrome (Clin Gastroenterol Hepatol 2017;15:e131)
- 62 year old man with gastrointestinal polyposis (Am J Gastroenterol 2003;98:1429)
Treatment
- No treatment is required as it is a benign condition
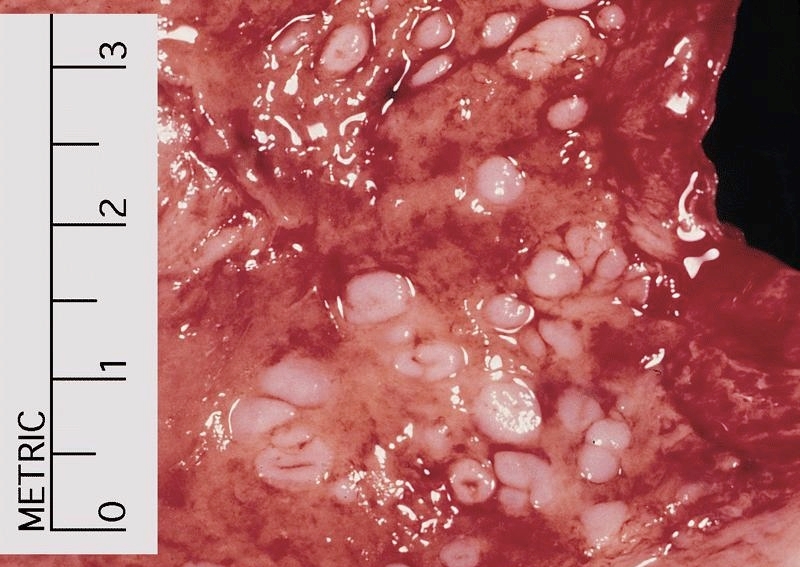
Gross description
- Endoscopically and grossly, glycogenic acanthosis is described as raised white plaques or nodular areas (typically 2 - 10 mm in diameter), which may be single, multiple or coalesced (Gastrointest Radiol 1984;9:93)
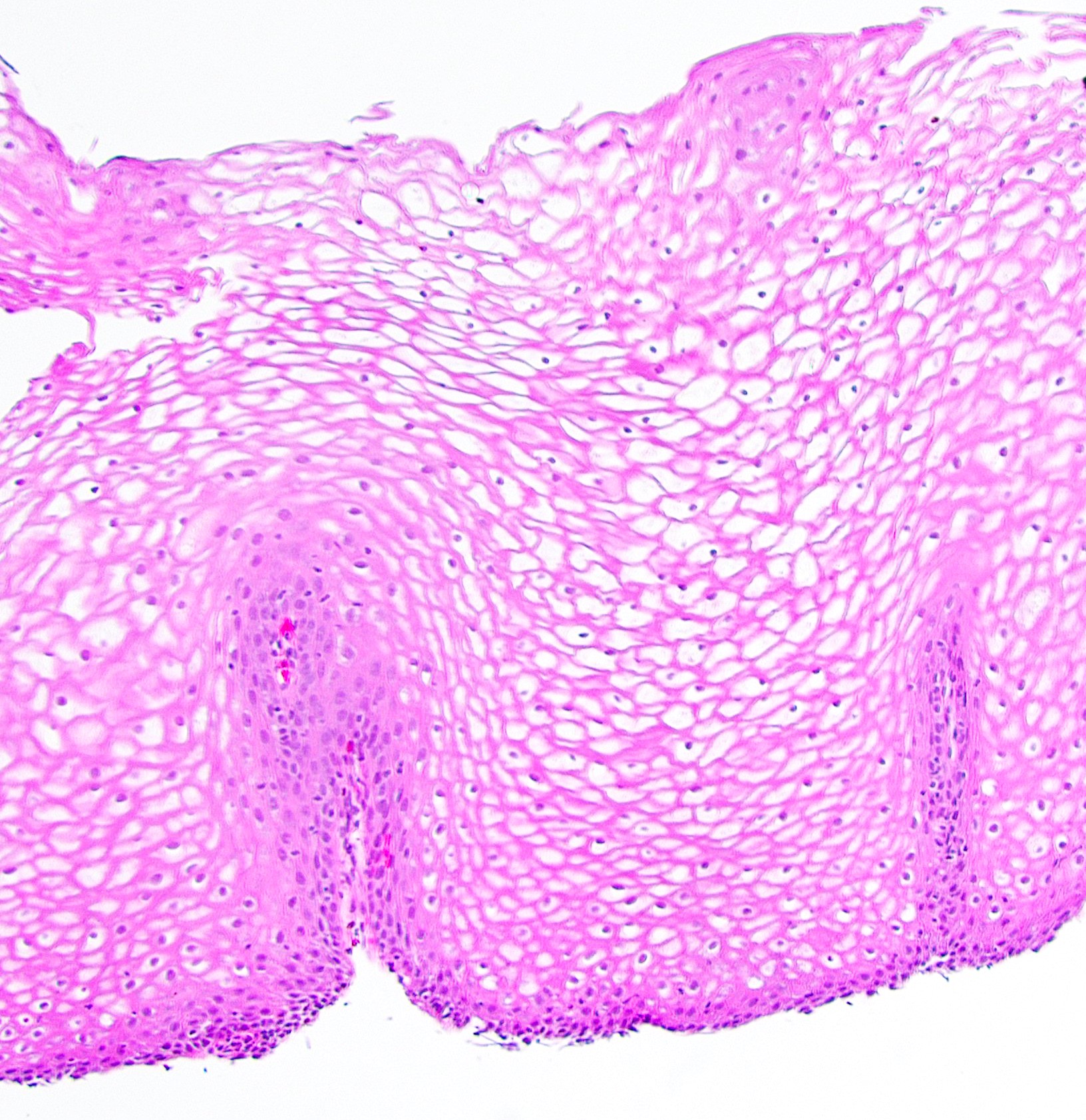
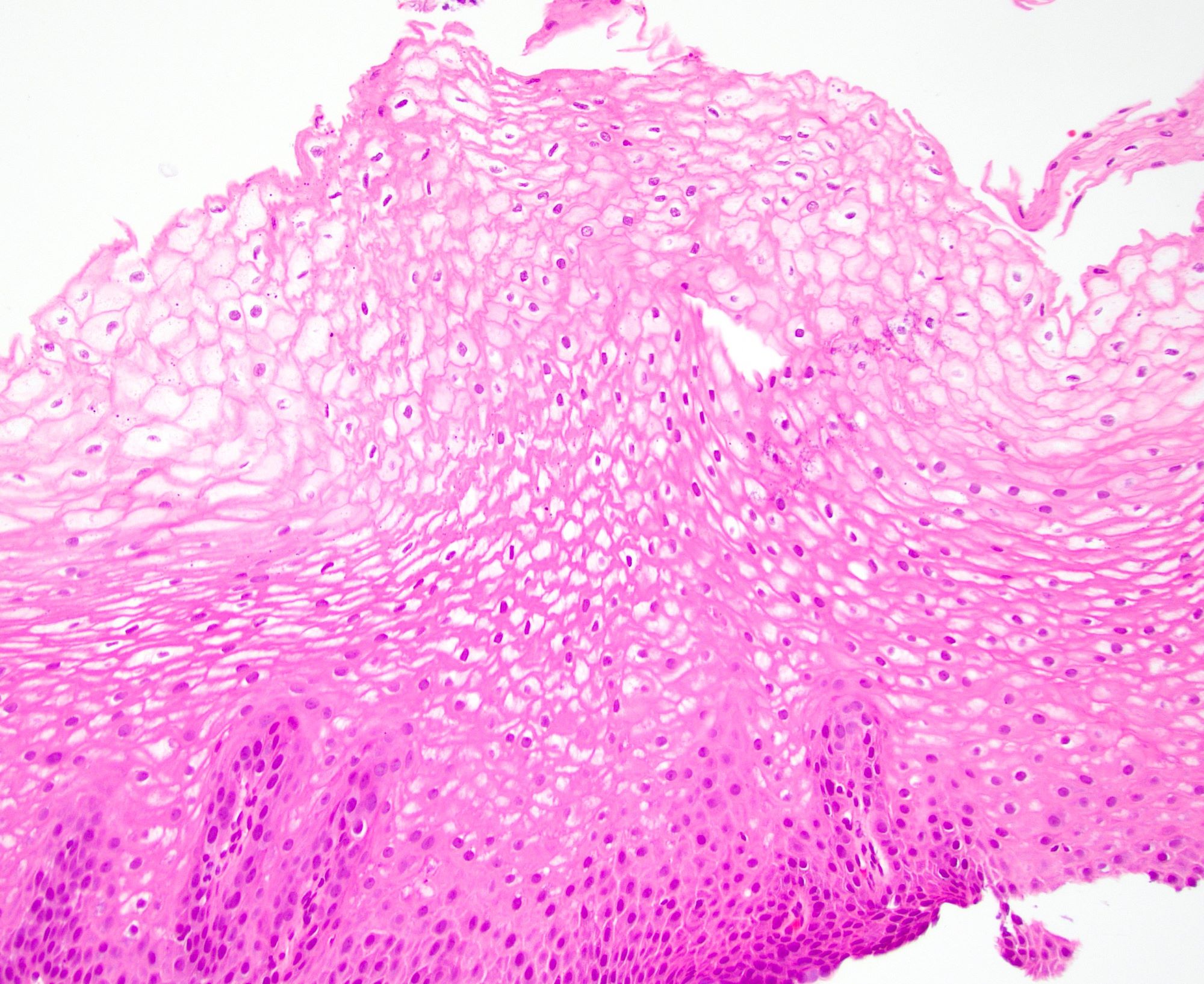
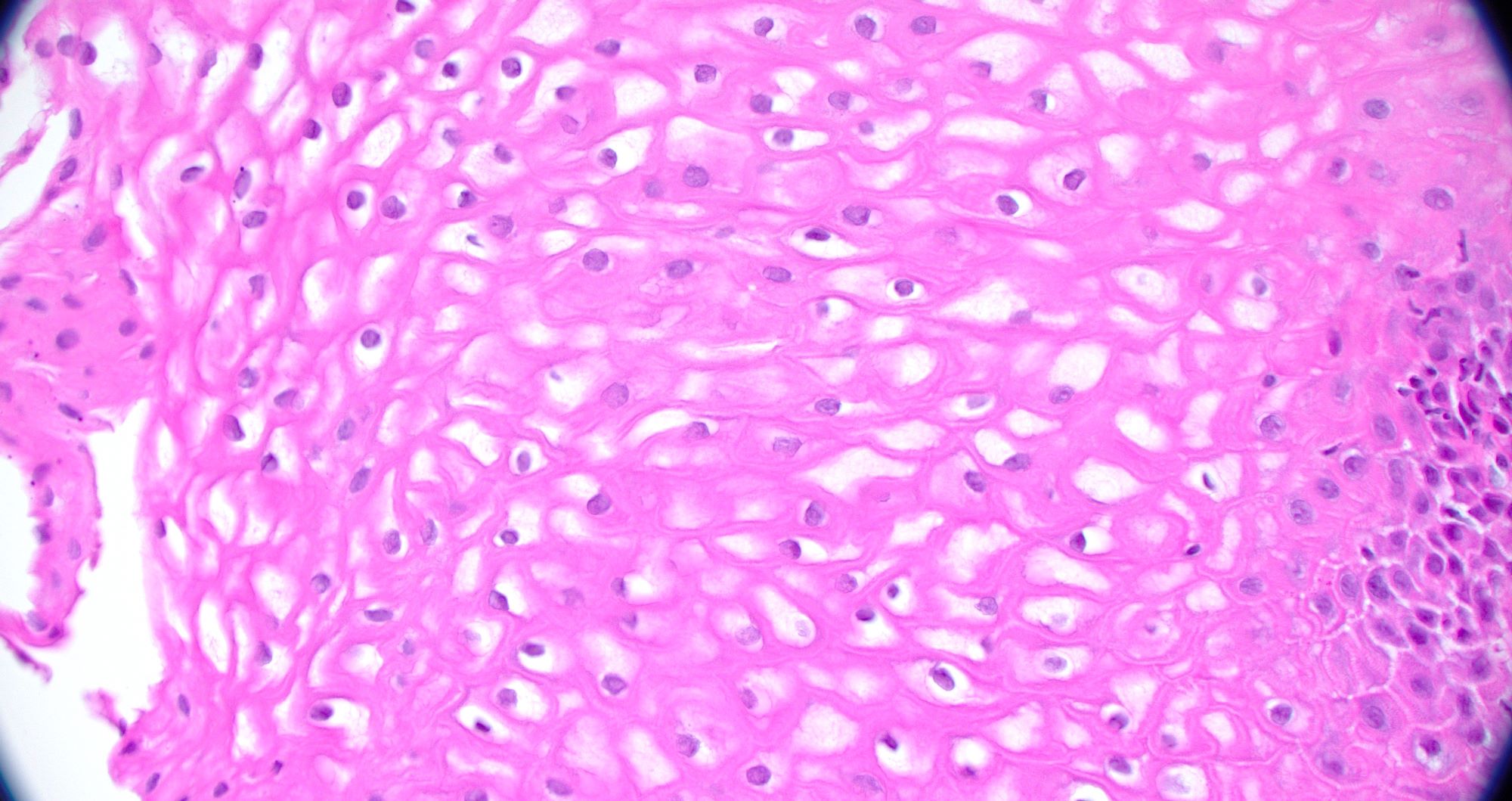
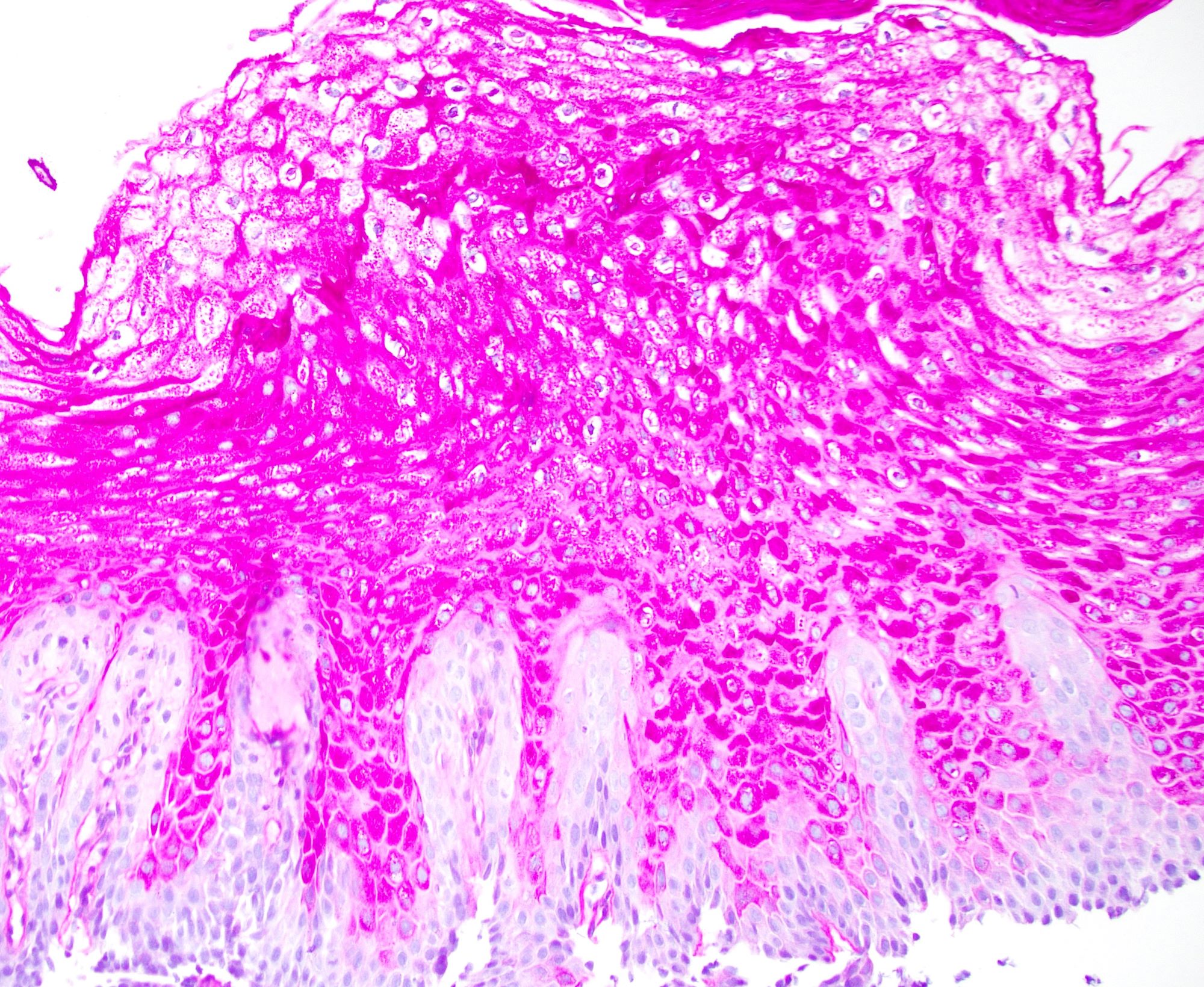
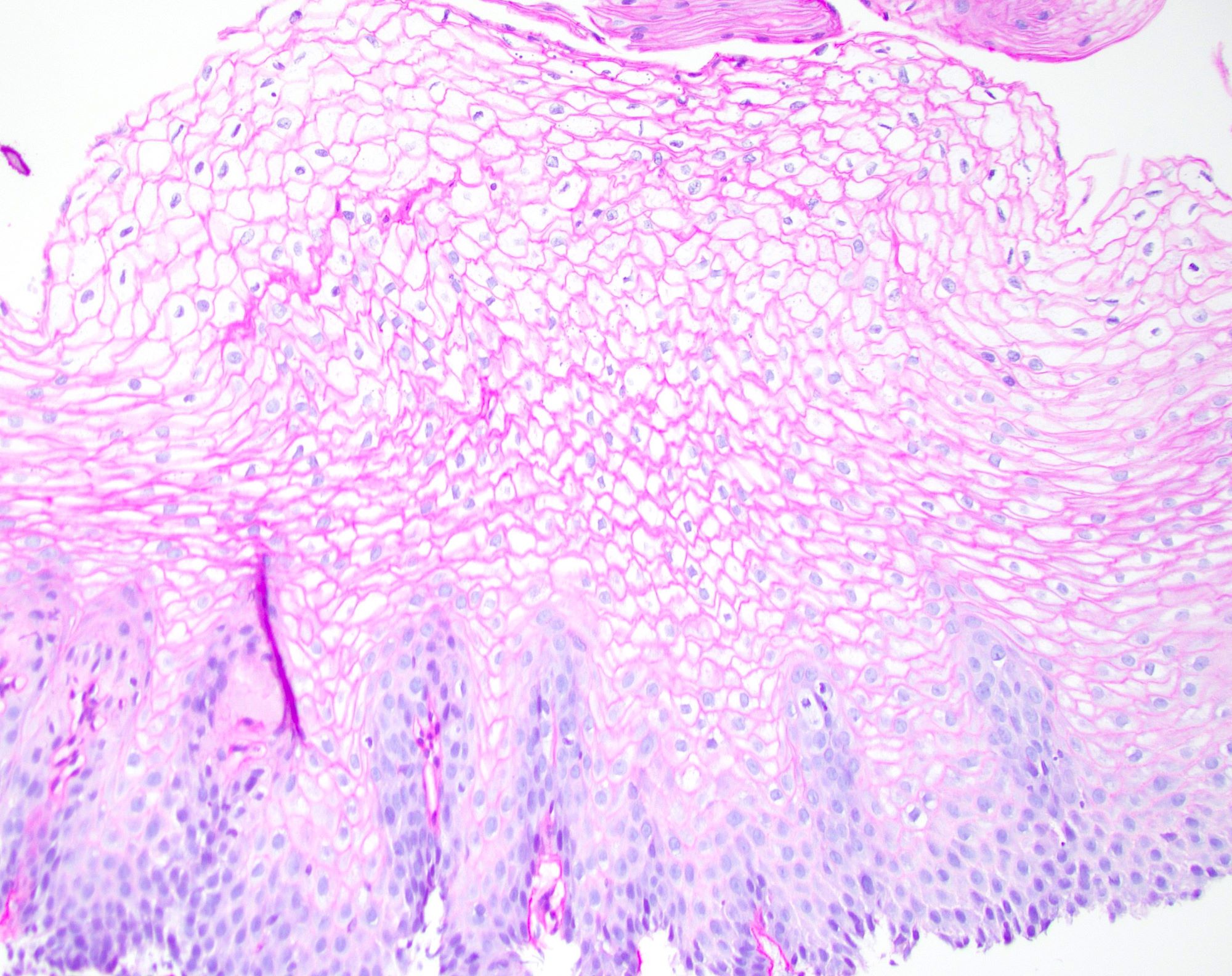
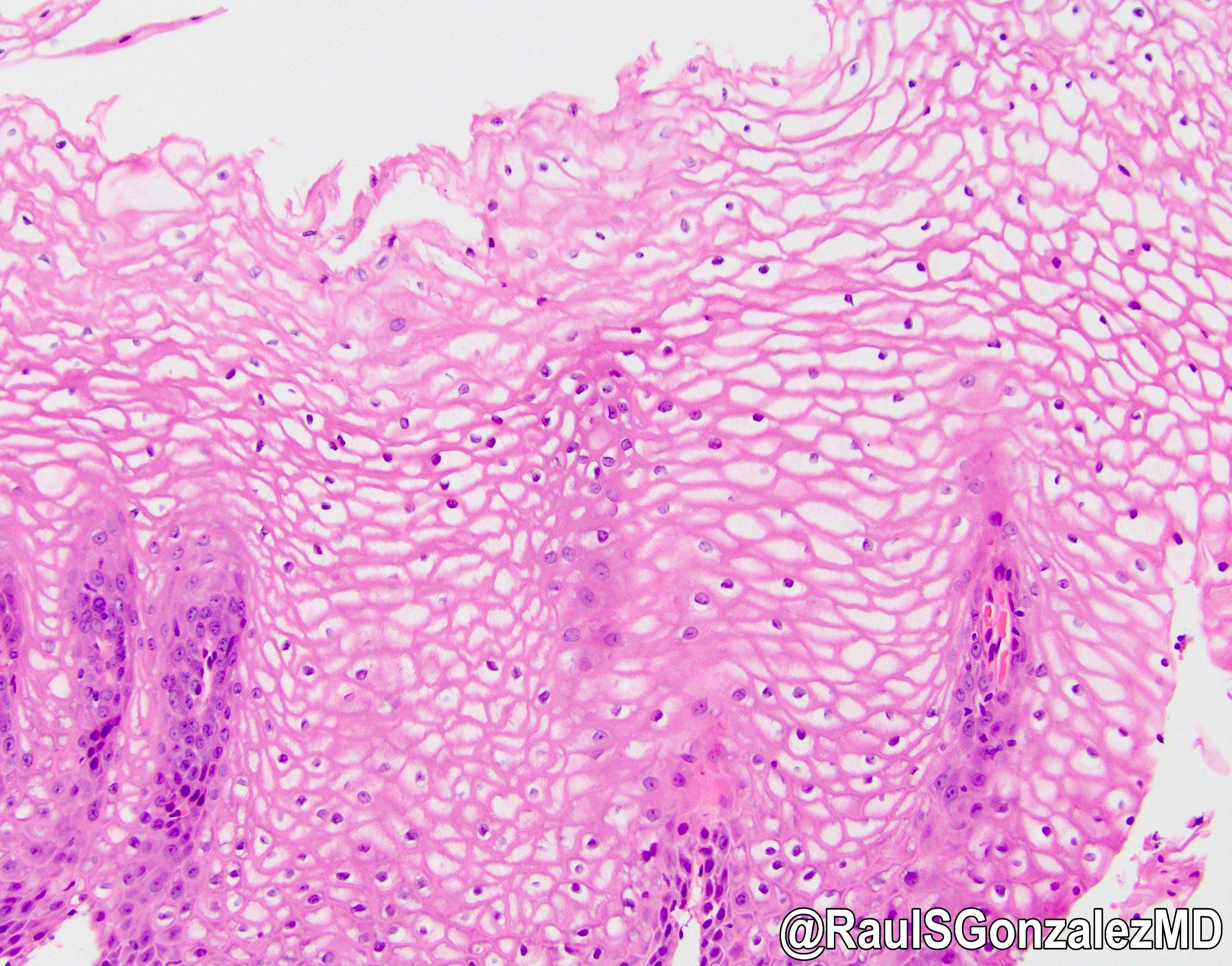
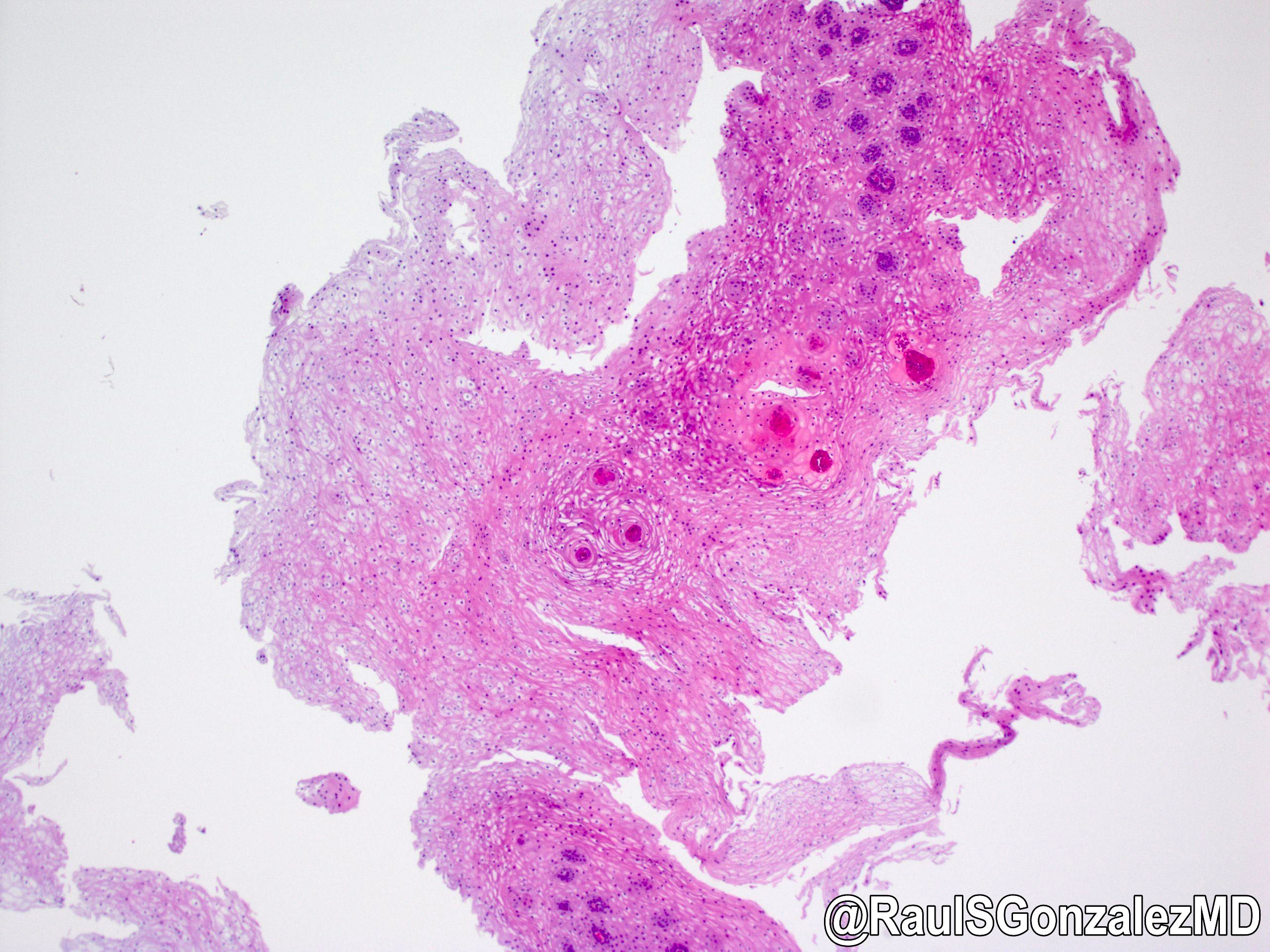
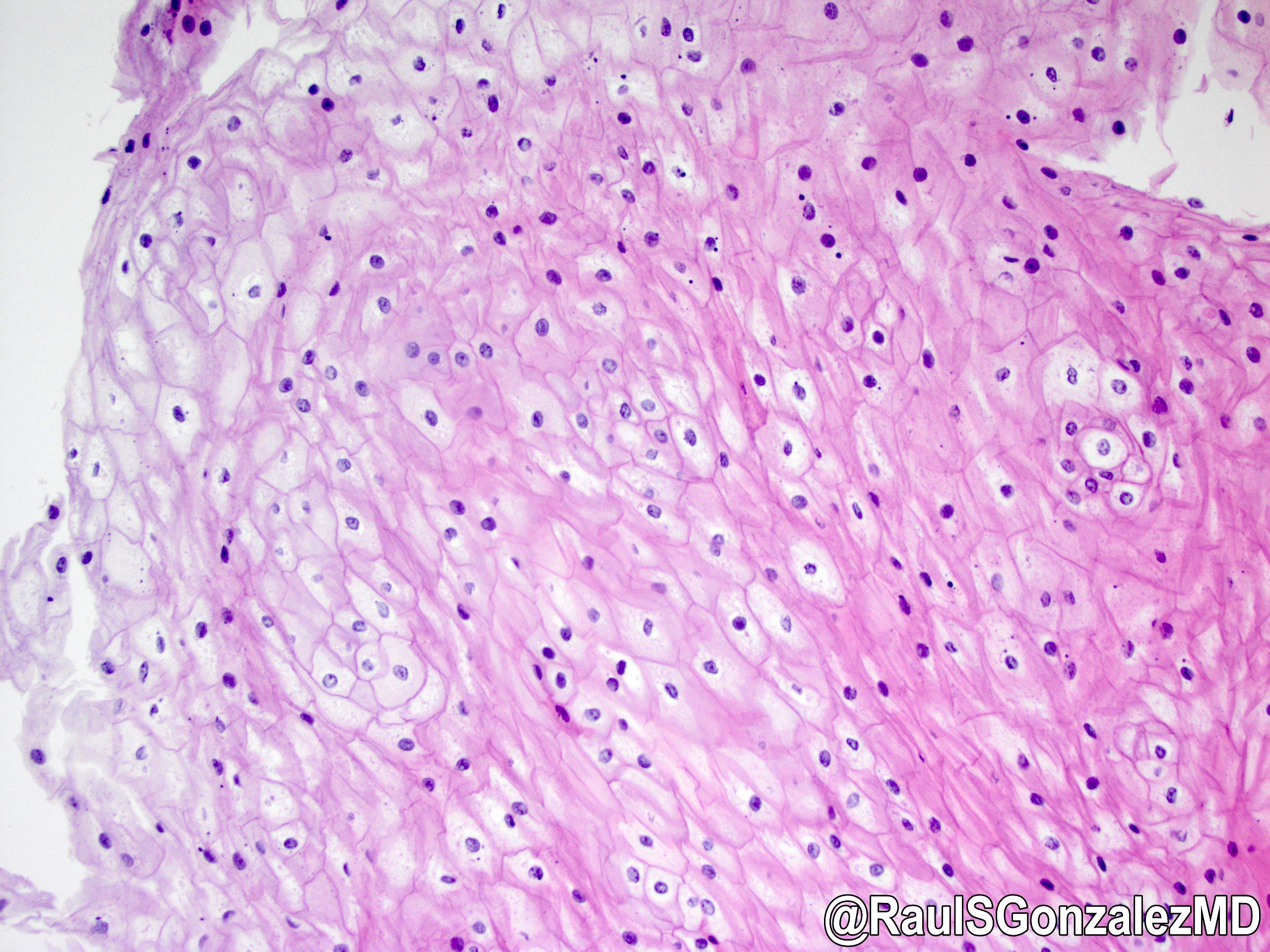
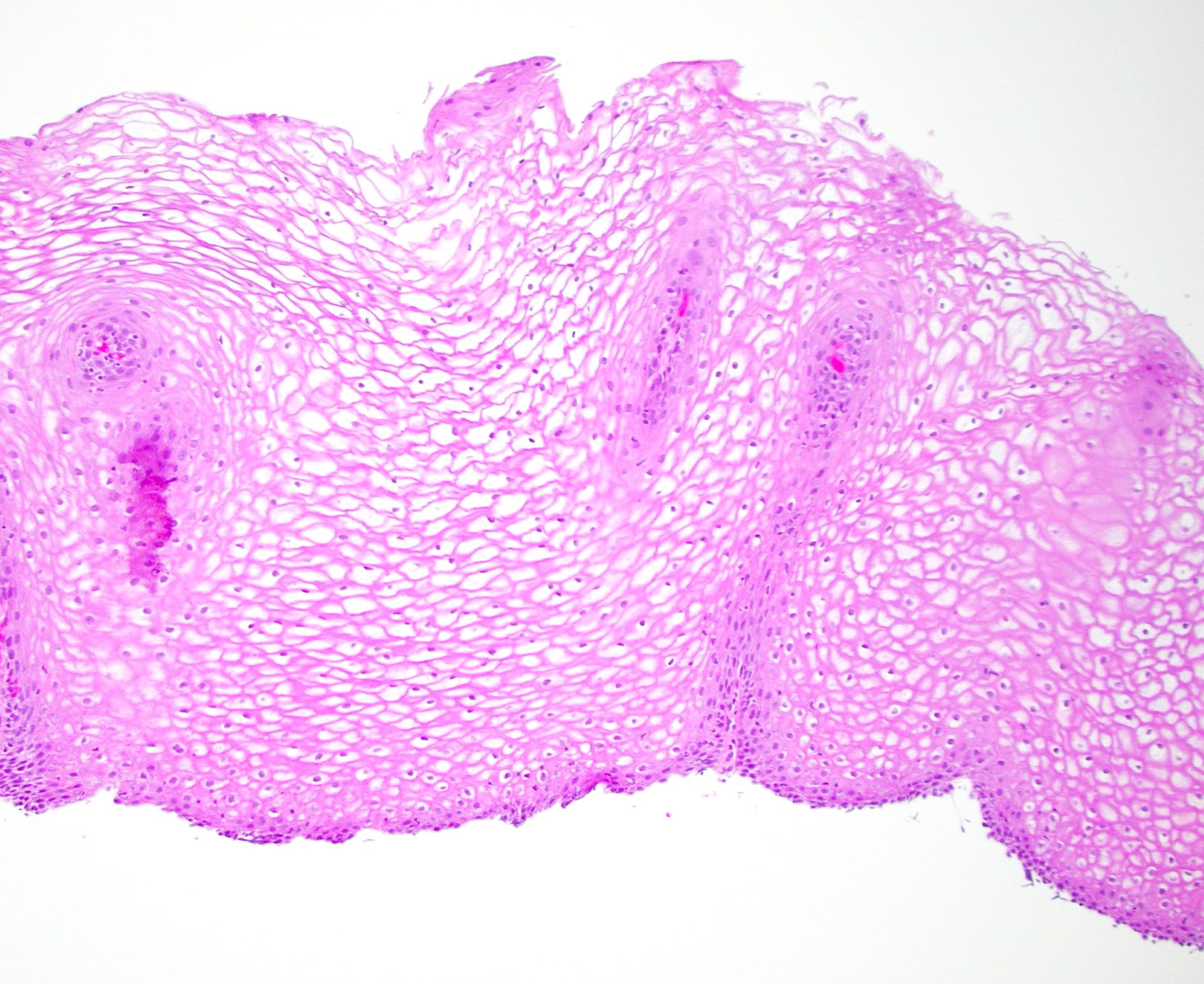
Microscopic (histologic) description
- Squamous hyperplasia of the esophageal epithelium with intracellular glycogen accumulation
- Glycogen is positive for PAS and sensitive to diastase; a combination of PAS and PASD stains may be helpful to confirm the diagnosis (PAS positive intracellular glycogen is removed with PASD stain, which will be negative)
- References: World J Gastroenterol 2015;21:1091, Prz Gastroenterol 2020;15:39
Microscopic (histologic) images
Positive stains
Negative stains
- See Positive stains
Sample pathology report
- Esophagus, nodule, biopsy:
- Glycogenic acanthosis (see comment)
- Comment: Glycogenic acanthosis is a benign esophageal lesion that may be associated with PTEN hamartoma tumor (Cowden) syndrome but is also a common finding in upper endoscopies in nonsyndromic patients. Correlation with clinical and endoscopic findings is recommended.
Differential diagnosis
- Normal esophageal mucosa:
- Probably the most challenging histologic differential diagnosis, easily missed if lesional and nonlesional epithelium are not present
- Look for glycogenated squamous epithelial cells comprising over 50% of the mucosal thickness
- Candidal esophagitis:
Additional references
Board review style question #1
A 56 year old man underwent an esophagogastroduodenoscopy for reflux symptoms. A biopsy was taken of a small, raised white nodule in the esophagus. The histology is depicted in the H&E image shown above. What is the best diagnosis?
- Candidal esophagitis
- Epidermoid metaplasia
- Glycogenic acanthosis
- Mucosal calcinosis
- Normal esophageal squamous mucosa
Board review style answer #1
C. Glycogenic acanthosis. The H&E image demonstrates accumulation of intracytoplasmic glycogen in the squamous epithelium and the best diagnosis is glycogenic acanthosis (GA). PAS and PASD stains would be helpful to confirm the diagnosis since glycogen is PAS positive and diastase sensitive. Glycogenic acanthosis can be difficult to distinguish from normal esophageal mucosa, particularly if nonlesional tissue is not present. The endoscopic impression of a nodule is helpful and the diagnosis of glycogenic acanthosis would explain the endoscopic findings. Mucosal calcinosis is rare in the esophagus and would have calcium deposition within the epithelium or mucosa. Epidermoid metaplasia can also appear white on endoscopy but is characterized by a granular cell layer within the squamous epithelium resembling skin, hence the term epidermoid.
Comment Here
Reference: Glycogenic acanthosis
Comment Here
Reference: Glycogenic acanthosis
Board review style question #2
A 45 year old woman with a history of hamartomatous gastrointestinal polyps undergoes an esophagogastroduodenoscopy. There are diffuse white plaques and nodules in the esophagus. Biopsies are taken of some of the esophageal lesions and demonstrate hyperplastic squamous epithelium with intracytoplasmic accumulation of glycogen consistent with glycogenic acanthosis. What syndrome does this patient likely have?
- Lynch syndrome
- Maffucci syndrome
- Peutz-Jeghers syndrome
- PTEN hamartoma tumor syndrome (Cowden syndrome)
Board review style answer #2
D. PTEN hamartoma tumor syndrome (Cowden syndrome). PTEN hamartoma tumor syndrome (PTHS) is an all encompassing term for Cowden, Bannayan-Riley-Ruvalcaba, PTEN related Proteus and PTEN related Proteus-like syndromes. Cowden syndrome (CS) is an autosomal dominant syndrome caused by a germline mutation in the PTEN tumor suppressor gene on chromosome 10. Esophageal glycogenic acanthosis, particularly if diffuse, is a manifestation of Cowden syndrome and is seen in around 80 - 90% of patients. Maffucci syndrome is characterized by multiple enchondromas and hemangiomas. Peutz-Jeghers syndrome (PJS) is a hamartomatous polyposis syndrome of the gastrointestinal tract with increased risk of certain malignancies. PJS is autosomal dominantly inherited and caused by mutations in the STK11 gene. Lynch syndrome is the most common cause of hereditary colorectal cancer and is due to mutations in mismatch repair genes. Patients with Lynch syndrome are also at risk of other types of cancers. None of these, except Cowden syndrome, have glycogenic acanthosis.
Comment Here
Reference: Glycogenic acanthosis
Comment Here
Reference: Glycogenic acanthosis