Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tateishi Y, Nakanishi Y. Crohn's disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophaguscrohn.html. Accessed April 2nd, 2025.
Definition / general
- Esophagitis associated with Crohn's disease
Essential features
- Incidence of esophageal Crohn's disease ranges from 0.3% to 10% in adults with Crohn's disease and from 4.2% to 42% in pediatric patients with Crohn's disease
- Aphthous ulcer, longitudinal ulcer, stricture and fistula
- Histologic features of esophageal Crohn's disease are generally nonspecific
- Nonnecrotizing granuloma(s) may be found
Terminology
- Esophagitis associated with Crohn's disease
ICD coding
- ICD-10: K509 - Crohn's disease, unspecified
Epidemiology
- Incidence of esophageal Crohn's disease ranges from 0.3% to 10% in adults with Crohn's disease and from 4.2% to 42% in pediatric patients with Crohn's disease (J Crohns Colitis 2020;14:624, Adv Anat Pathol 2022;29:2, J Crohns Colitis 2018;12:1073)
- Higher frequency of endoscopic and histological alterations was found when upper digestive endoscopy is performed routinely as part of the evaluation of the disease, regardless of the presence of gastrointestinal symptoms (World J Gastrointest Pharmacol Ther 2019;10:35, J Crohns Colitis 2018;12:1399, Inflamm Bowel Dis 2016;22:1896)
- Patients with proximal Crohn's disease including the esophagus were more likely to be younger at diagnosis (Am J Gastroenterol 2013;108:106, J Crohns Colitis 2018;12:1399)
- Male sex was an independent predictor for upper gastrointestinal tract involvement including the esophagus (J Crohns Colitis 2018;12:1399)
- 18 of 61 patients (30%) with lymphocyte rich inflammation in the mid or proximal esophagus had Crohn's disease (Am J Surg Pathol 2020;44:198)
- Patients in the lymphocytic esophagitis cohort had a higher than normal proportion of patients with Crohn's disease, raising the possibility that lymphocytic esophagitis could be associated with or a manifestation of inflammatory bowel disease (Am J Clin Pathol 2006;125:432, Am J Surg Pathol 2022;46:e55)
- Association between esophageal lymphocytosis and Crohn's disease has been reported in pediatric populations (Inflamm Bowel Dis 2011;17:45, Inflamm Bowel Dis 2014;20:1324, Am J Surg Pathol 2022;46:e55)
Sites
- Distal esophagus is the most common involved site, either alone or with the involvement of the entire esophagus (J Crohns Colitis 2020;14:624)
Pathophysiology
- Crohn's disease is a chronic inflammatory disease mainly affecting the intestine, especially the terminal ileum; Crohn's disease is characterized by the alternating periods of flares and remissions caused by a complex pathogenesis involving a reshaped microenvironment of the intestine (Biol Direct 2020;15:23)
Etiology
- Caused by a complex pathogenesis involving the interactions of environmental factors, the immune system, susceptibility genes and the host’s microbiome changes, leading to disruption of the intestinal mucosa; among these, inflammation plays a key role
- Etiology of esophageal Crohn’s disease remains unclear, as overall pathogenesis of Crohn’s disease remains poorly understood (Biol Direct 2020;15:23)
Clinical features
- Patients are asymptomatic or have nonspecific symptoms, such as dysphagia, odynophagia, heartburn, vomiting, chest pain and weight loss (J Crohns Colitis 2020;14:624, J Gastroenterol Hepatol 2018;33:355)
- Crohn's disease limited to the esophagus is extremely rare and almost all cases have concomitant intestinal Crohn's disease (Inflamm Bowel Dis 2015;21:2106, World J Gastrointest Pharmacol Ther 2019;10:35, J Crohns Colitis 2020;14:624, J Gastroenterol Hepatol 2018;33:355)
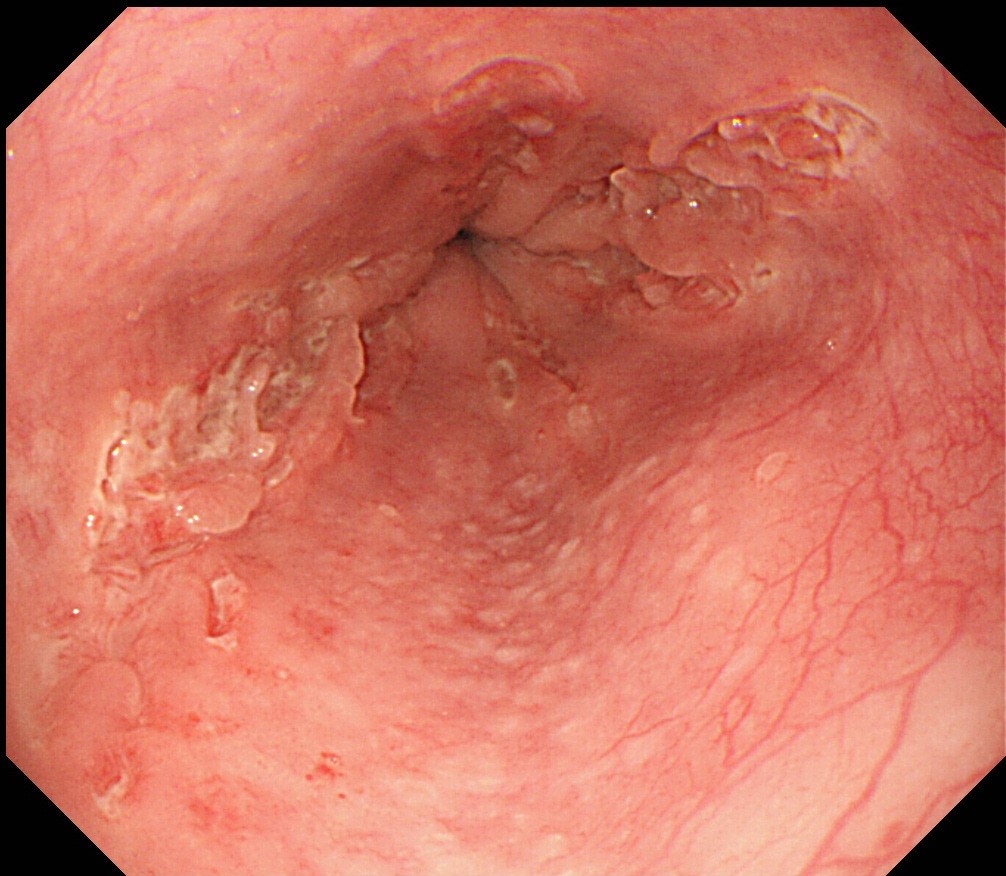
- Endoscopic findings are nonspecific including erosion, aphthous ulcer, granular and hyperemic mucosa and longitudinal ulcer (J Gastroenterol Hepatol 2018;33:355)
- Advanced disease may display cobblestone appearance, stricture and fistula (J Gastroenterol Hepatol 2018;33:355)
Diagnosis
- Clinicopathologic diagnosis including the patient's clinical history of Crohn's disease and endoscopic and histologic features, such as aphthous ulcer, longitudinal ulcer and granuloma(s)
Radiology description
- Aphthous ulcer, longitudinal ulcer, rose thorn fissure, a cobblestone appearance of the mucosa, stricture and fistula (Inflamm Bowel Dis 2015;21:2106, J Gastroenterol Hepatol 2018;33:355)
Prognostic factors
- Controversial
- Involvement of upper GI tract did not result in a worse outcome (J Crohns Colitis 2018;12:1399)
- Expected poor prognosis (J Crohns Colitis 2017;11:3)
Case reports
- 23 year old woman with Crohn's disease and esophageal involvement (BMJ Case Rep 2017;2017:bcr2016217960)
- 24 year old woman with Crohn's disease and esophageal involvement (ACG Case Rep J 2019;6:e00052)
- 30 year old woman with history of severe ileocolonic Crohn's disease presented with odynophagia and progressive dysphagia to liquids and solids (Dig Dis Sci 2017;62:2690)
- 33 year old woman with Crohn's disease and esophageal involvement (Clin Gastroenterol Hepatol 2022;20:A15)
- 51 year old woman with an esophageal stricture (Rev Esp Enferm Dig 2022;114:501)
Treatment
- Mild esophageal Crohn’s disease may be treated with a proton pump inhibitor only (J Crohns Colitis 2017;11:3)
- Severe or refractory disease requires additional systemic corticosteroids or anti-TNF therapy (J Crohns Colitis 2017;11:3)
- Surgery or dilatation by endoscopy are appropriate for symptomatic stricture
- Treatment is decided based on both esophageal Crohn's disease activity and extraesophageal involvement
Gross description
- Erythema, erosion, aphthous ulcer, longitudinal ulcer, stricture and fistula
Microscopic (histologic) description
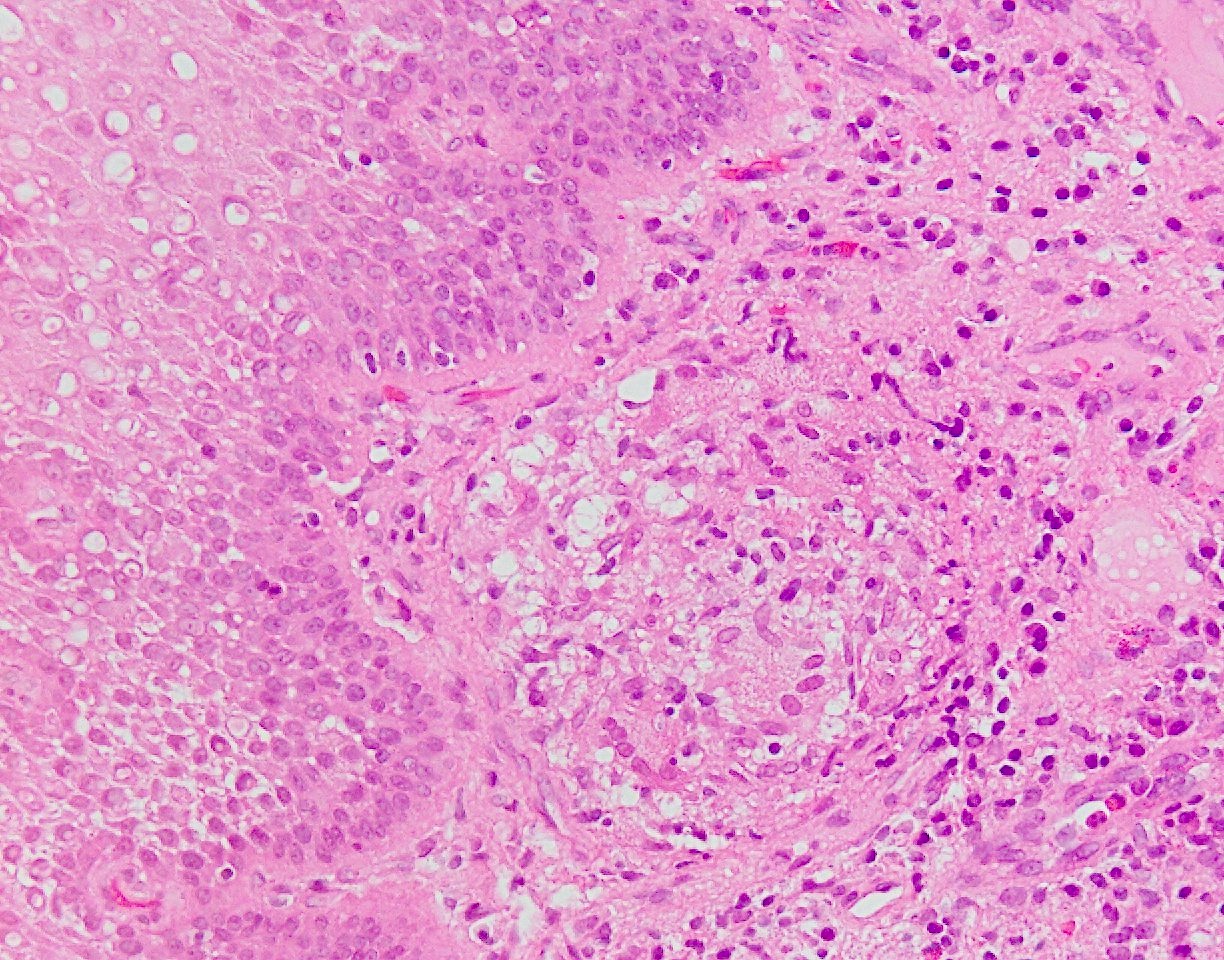
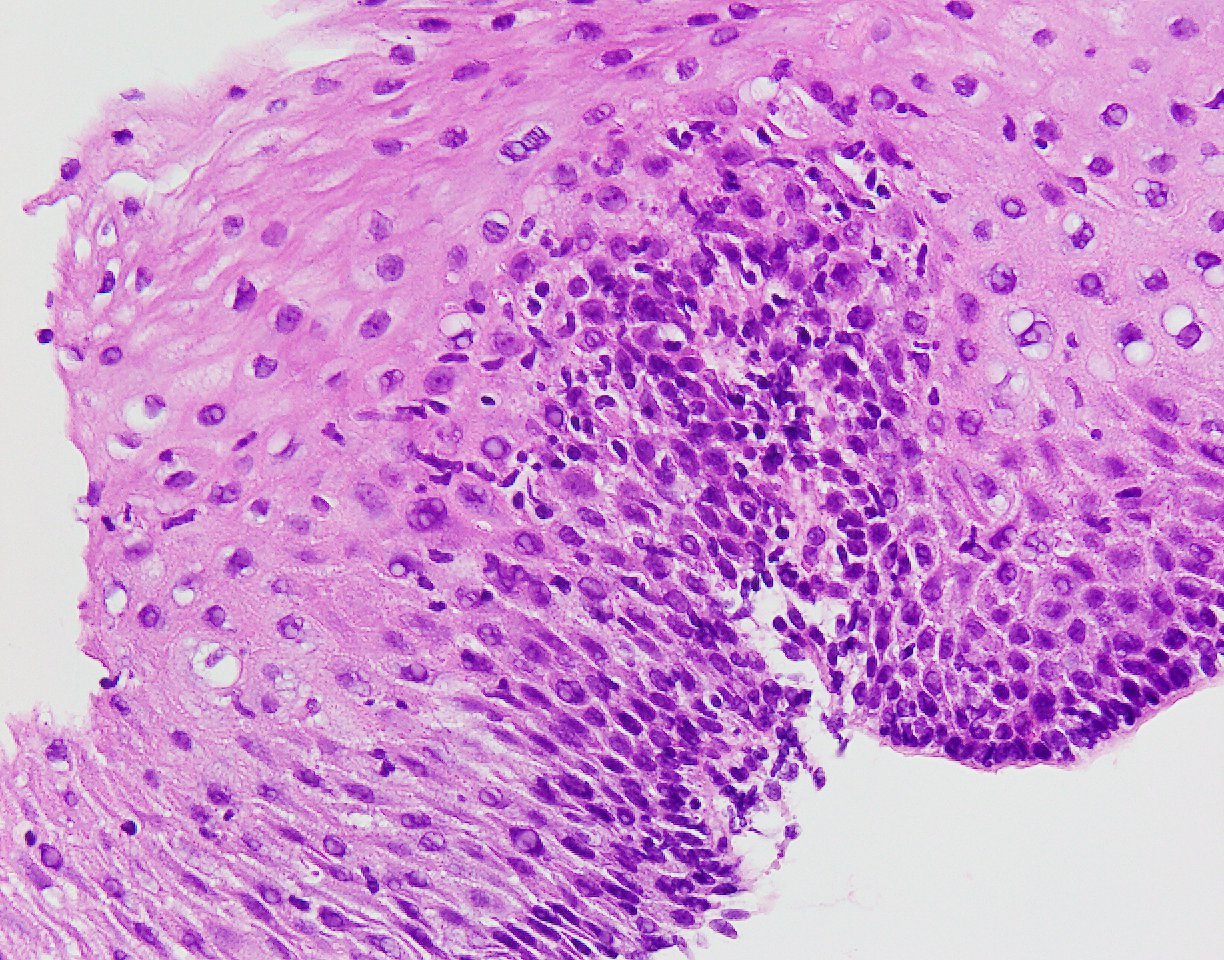
- Nonnecrotizing granuloma(s) may be found in up to 50% of cases (Gastrointest Endosc 1994;40:296, Inflamm Bowel Dis 2015;21:2106)
- Frequency of nonnecrotizing granuloma(s) varies greatly depending on the type of specimen (biopsy versus resection) (Adv Anat Pathol 2022;29:2, J Gastroenterol Hepatol 2018;33:355)
- Biopsy often shows chronic inflammation only
- Transmural chronic inflammation in the esophagectomy specimen, one of the histologic hallmarks of Crohn's disease, has been reported in a patient with uncontrollable stricture due to Crohn's disease (Rev Esp Enferm Dig 2022;114:501)
- Concurrent eosinophilic and lymphocytic esophagitis has been described in patients with Crohn's disease (Adv Anat Pathol 2022;29:2, Am J Surg Pathol 2020;44:198, Am J Surg Pathol 2022;46:e55)
Microscopic (histologic) images
Negative stains
Sample pathology report
- Esophagus, ulcer, biopsy:
- Squamous mucosa with nonnecrotizing granuloma(s) (see comment)
- GMS and PASF stains, negative for fungal infection.
- AFB stain, negative for acid fast bacilli.
- Comment: Given the patient's clinical history of Crohn's disease and the endoscopic findings of longitudinal and aphthous ulcers, the biopsy findings are compatible with granulomatous inflammation associated with Crohn's disease. Clinical correlation is suggested.
Differential diagnosis
- Histologic features of esophageal Crohn's disease are typically nonspecific
- In many cases, a definitive diagnosis of esophageal Crohn's disease cannot be established based on histologic features alone and only a diagnosis of compatible with esophageal CD can be achieved
- Lymphocytic esophagitis:
- Lymphocytic esophagitis is a term suggested for the finding of intraepithelial lymphocytosis (≥ 20 lymphocytes / high power field) in an esophageal biopsy
- History of Crohn's disease
- Esophagitis secondary to gastroesophageal reflux disease:
- Endoscopic findings and pH monitoring would be helpful
- Lichenoid pattern esophagitis:
- Important cause of lymphocyte rich esophagitis, affecting the esophagus in up to 50% of patients with oral or cutaneous disease (Endoscopy 2009;41:187, Am J Surg Pathol 2020;44:198)
- Biopsy samples show dense mononuclear cell rich lamina propria inflammation accompanied by band-like chronic inflammation underneath the epithelium
- Esophageal tuberculosis:
- Caseating granuloma(s) may be found
- AFB stain, culture and polymerase chain reaction testing for mycobacterium tuberculosis
- Clinical presentation and pathologic features useful for esophageal tuberculosis diagnosis includes fever, night sweaters, transverse ulcer, ileocecal lesion and caseating granuloma(s)
- Sarcoidosis:
- Esophageal involvement is an extremely rare occurrence in sarcoidosis
- Presence of T lymphocytes, mononuclear phagocytes and noncaseating granuloma(s)
- Involvement of other organs, especially lung
- Parasite and fungal infection:
- Granuloma(s) may be found (Rev Bras Parasitol Vet 2019;28:769)
- GMS stain, PAS stain and culture
- Foreign body granuloma(s) :
- Clinical history (wound, operation, endoscopic treatment, etc.)
- Cytomegalovirus (CMV) infection:
- Cytomegaly and nucleomegaly with CMV inclusions of infected cells including endothelial cells and mesenchymal cells
- Positive CMV immunostaining
- Candida esophagitis:
- Neutrophilic infiltration with fungal pseudohyphae in sloughed epithelial debris or squamous epithelium
- Drug induced esophagitis:
- Deposition of drug fragments, such as iron pill
- Behçet disease:
- Prominent vasculitis
- Round deep ulcers with sharp borders in the ileocecal location
Board review style question #1
Which of the following statements regarding the histologic features of esophageal Crohn’s disease is true?
- Chronic inflammation with predominantly lymphocytes and plasma cells is the most common finding in biopsy samples
- Elderly patients with Crohn's disease tend to show more frequent esophageal involvement
- Proximal esophagus is the most common site of involvement
- The finding of nonnecrotizing granuloma(s) is diagnostic of Crohn’s disease
Board review style answer #1
A. Chronic inflammation with predominantly lymphocytes and plasma cells is the most common finding in biopsy samples. The biopsy findings of esophageal Crohn's disease are generally nonspecific. Biopsy often shows chronic inflammation only. Epithelioid granuloma(s) may be found up to 50% of cases. Answer C is incorrect because the distal esophagus is the most common site of involvement. Answer D is incorrect because nonnecrotizing granuloma(s) can be seen in various conditions, such as sarcoidosis, tuberculosis and foreign body reaction, among others. Answer B is incorrect because there have been no established evidence / previous reports that elderly patients with Crohn's disease tend to show more frequent esophageal involvement.
Comment Here
Reference: Crohn's disease
Comment Here
Reference: Crohn's disease
Board review style question #2
Which of the following statements about esophageal Crohn’s disease is true?
- Almost all cases have concomitant intestinal Crohn's disease
- Granuloma(s) are frequently seen in biopsy samples
- Most patients will eventually require esophagectomy
- Often shows esophageal stricture
Board review style answer #2
A. Almost all cases have been reported to have concomitant intestinal Crohn's disease. Crohn's disease limited to the esophagus is extremely rare. Answer C is incorrect because esophagectomy is rarely performed for the treatment of esophageal Crohn's disease. Answer B is incorrect because granuloma(s) can be seen in up to (at most) 50% of cases. Answer D is incorrect because esophageal stricture due to Crohn's disease is not frequently seen.
Comment Here
Reference: Crohn's disease
Comment Here
Reference: Crohn's disease