Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kwon G, Pendse A. Adenocarcinoma of the esophagus and GE junction. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophagusadenocarcinoma.html. Accessed April 1st, 2025.
Definition / general
- Malignant epithelial neoplasm of the esophagus with glandular or mucinous differentiation
- Majority of cases occur in the lower esophagus and at the esophagogastric (GE) junction, which is defined endoscopically by the most proximal gastric fold or the distal end of the palisade vessels
Essential features
- According to WHO (5th edition), GE junction adenocarcinoma is defined as an adenocarcinoma with an epicenter within 2 cm of the GE junction and extending into the esophagus
- Rarely, adenocarcinoma can occur in the middle or upper third of the esophagus; such cases most likely develop from submucosal glands or ectopic columnar epithelium in the esophagus (also known as inlet patches or ectopic gastric mucosa)
- Evidence of glandular or mucinous differentiation within an invasive tumor originating in the esophagus and GE junction
- Barrett esophagus is an important risk factor
Terminology
- Adenocarcinoma of esophagus
- Adenocarcinoma of esophagogastric junction
ICD coding
Epidemiology
- Steady increase in incidence each year in developed countries since the 1970s through 2000, with the incidence rate eventually stabilizing in the United States through 2017 (J Natl Cancer Inst 2008;100:1184, Gastrointest Endosc Clin N Am 2021;31:1)
- Represents 15% of all esophageal cancers worldwide (the majority being esophageal squamous cell carcinoma), with men diagnosed more often than women (Gut 2020;69:1564)
- Predominance in men is greatest in the U.S., with an incidence ratio approaching 9:1 (Gut 2015;64:381, Gastroenterology 2022;163:649, Oncotarget 2016;7:38876, Clin Gastroenterol Hepatol 2016;14:338)
- Distinct geographical patterns compared with esophageal squamous cell carcinoma
- The majority of adenocarcinoma cases occur in Eastern Asia followed by North America, with China and the U.S. contributing most to the burden on a country level (Gut 2020;69:1564)
- Patients with Barrett esophagus have a 10 - 55 fold higher risk of adenocarcinoma (Dig Dis Sci 2018;63:1988)
- Rate of progression from Barrett esophagus to adenocarcinoma varies widely in the literature, within 0.07 - 3.6% and 1.5 - 2.5 fold higher when including high grade dysplasia (Gastroenterology 2015;149:577)
- Shorter segments (3 cm) of Barrett esophagus have a lower rate of progression to adenocarcinoma than longer segments (≥ 3 cm) (Endoscopy 2019;51:665)
- Unclear if proton pump inhibitors (PPI) have a protective effect on decreasing progression to adenocarcinoma (Transl Cancer Res 2021;10:1620)
- Can also occur in the setting of gastric heterotopia (Dig Liver Dis 2012;44:292)
Sites
- Esophagus
- Almost all cases occur in the lower third of the esophagus and esophagogastric junction
- Cases may occur in the upper and middle thirds of the esophagus, most likely developing from submucosal glands or ectopic columnar epithelium in the esophagus (also known as inlet patches or ectopic gastric mucosa)
Pathophysiology
- Primarily associated with Barrett esophagus, history of gastroesophageal reflux disease (GERD), obesity, tobacco smoking
- GERD is the single most important risk factor
- Intestinal metaplasia → genomic instability (often TP53 inactivation) → genome doubling and copy number alterations → malignancy (Cancer Prev Res (Phila) 2014;7:114, AORN J 1989;50:1182, Nat Genet 2015;47:1038)
- Mutations in TP53 and SMAD4 (only identified in high grade dysplasia and adenocarcinoma) occur in a stage specific manner (Nat Genet 2014;46:837)
- Next generation sequencing has identified additional genetic pathways and mutations involved, including Toll-like receptor signaling, receptor tyrosine kinase receptors and homologous recombination (PLoS Genet 2017;13:e1006808, Nat Genet 2016;48:1131)
Etiology
- ~7% of cases are familial (Cancer Epidemiol Biomarkers Prev 2006;15:1668, Dig Dis Sci 2016;61:1826, Clin Gastroenterol Hepatol 2014;12:1656)
Clinical features
- Progressive dysphagia, gastroesophageal reflux and weight loss are most common
- Iron deficiency anemia may result due to chronic gastrointestinal blood loss
- Odynophagia, nausea and vomiting are less common
- Most early (superficial) esophageal cancers are only detected serendipitously or by screening and surveillance of Barrett esophagus
- Intramucosal adenocarcinoma is not symptomatic
- ~6 - 10% are asymptomatic at the time of diagnosis (Ann Surg 2018;267:99)
Diagnosis
- Confirmed by endoscopic biopsy
- Radiographic imaging is necessary for staging to identify distant metastases
Radiology description
- CT may show esophageal wall thickening or a mass lesion, soft tissue with fat stranding
- Dilated proximal esophagus; oral debris may be present
- Tracheobronchial and aortic invasion may be present
- PET CT is useful to assess lymph node and distant metastases (Mol Imaging Biol 2011;13:166)
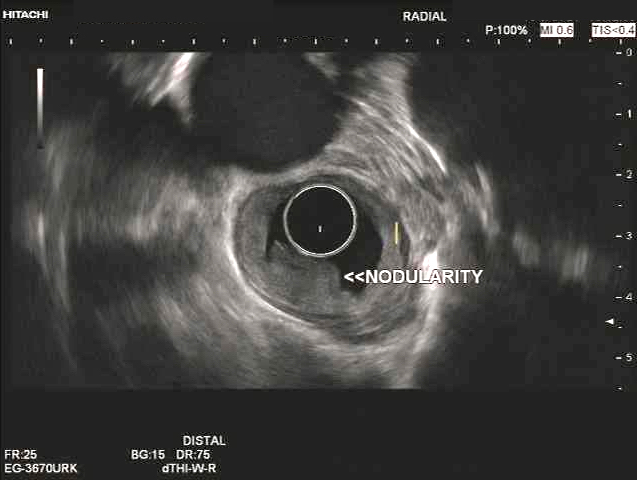
- Endoscopic ultrasound (EUS) is a modality of choice for tumor staging and locoregional lymph node involvement (Mol Imaging Biol 2011;13:166)
Prognostic factors
- Pathological stage is the most important prognostic factor
- Mortality is higher in men than women, with age standardized mortality rates of 8.2 versus 3.2 per 100,000 (Gastroenterology 2022;163:649)
- Signet ring cell morphology is associated with a poor prognosis (Ann Thorac Surg 2013;96:1927)
Case reports
- 51 year old man presented with 2 weeks of reflux, 35 pound weight loss and elevated alpha fetoprotein (AFP) (Clin J Gastroenterol 2017;10:7)
- 60 year old man presented with epigastric discomfort for one month and a mid esophageal adenocarcinoma arising from a heterotopic pancreas (Thorac Cancer 2022;13:1083)
- 71 year old man with a history of smoking and Barrett esophagus presenting with dysphagia and weight loss (Anticancer Res 2018;38:5999)
- 82 year old man presented with a 15 cm incarcerated hiatal hernia and an incidental 3 cm polypoid lesion on endoscopy at the level of the carina (BMJ Case Rep 2020;13:e235802)
- Dutch family with clustering of Barrett esophagus and esophageal adenocarcinoma (Fam Cancer 2018;17:435)
Treatment
- Dependent on tumor stage and patient's health status
- Generally less radiosensitive than esophageal squamous cell carcinoma
- Early (T1) lesions may be cured via endoscopic techniques (radiofrequency ablation, endoscopic mucosal resection, endoscopic submucosal dissection)
- Preoperative chemoradiation with or without immunotherapy targeting HER2 receptor followed by surgery is the most common treatment protocol for resectable tumors (J Natl Compr Canc Netw 2015;13:194)
- Esophagectomy and esophagogastrectomy performed in medically fit patients with localized thoracic esophageal cancer > 5 cm from the cricopharyngeus and in intra-abdominal esophageal and GE junction cancers respectively (J Natl Compr Canc Netw 2015;13:194)
- Definitive chemoradiation for cervical and cervicothoracic esophageal cancers within 5 cm of the cricopharyngeus
- Patients with esophageal adenocarcinoma who had a HER2 score of 3+ or 2+ on immunohistochemistry with positive FISH and treated with trastuzumab plus chemotherapy had a longer median survival compared with patients treated with chemotherapy alone (Lancet 2010;376:687)
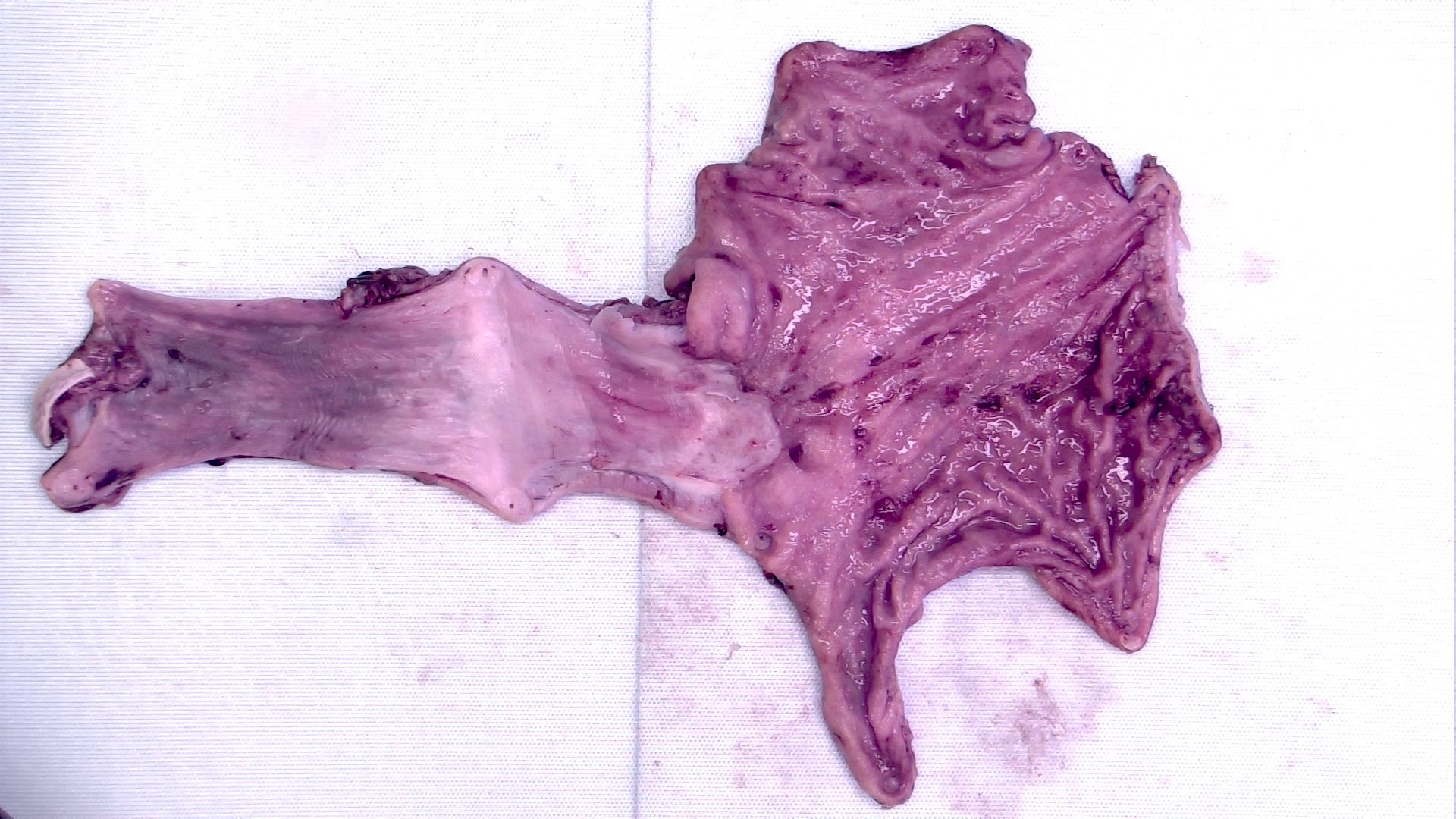
Gross description
- Often appear in advanced stages
- May be stricturing, polypoid, fungating, ulcerative or diffusely infiltrative
Gross images
Frozen section description
- Intraoperative frozen section analysis is usually performed for assessment of surgical margin status and to rule out involvement by distant metastases, as surgical management may not be effective if distant metastases are present
Frozen section images
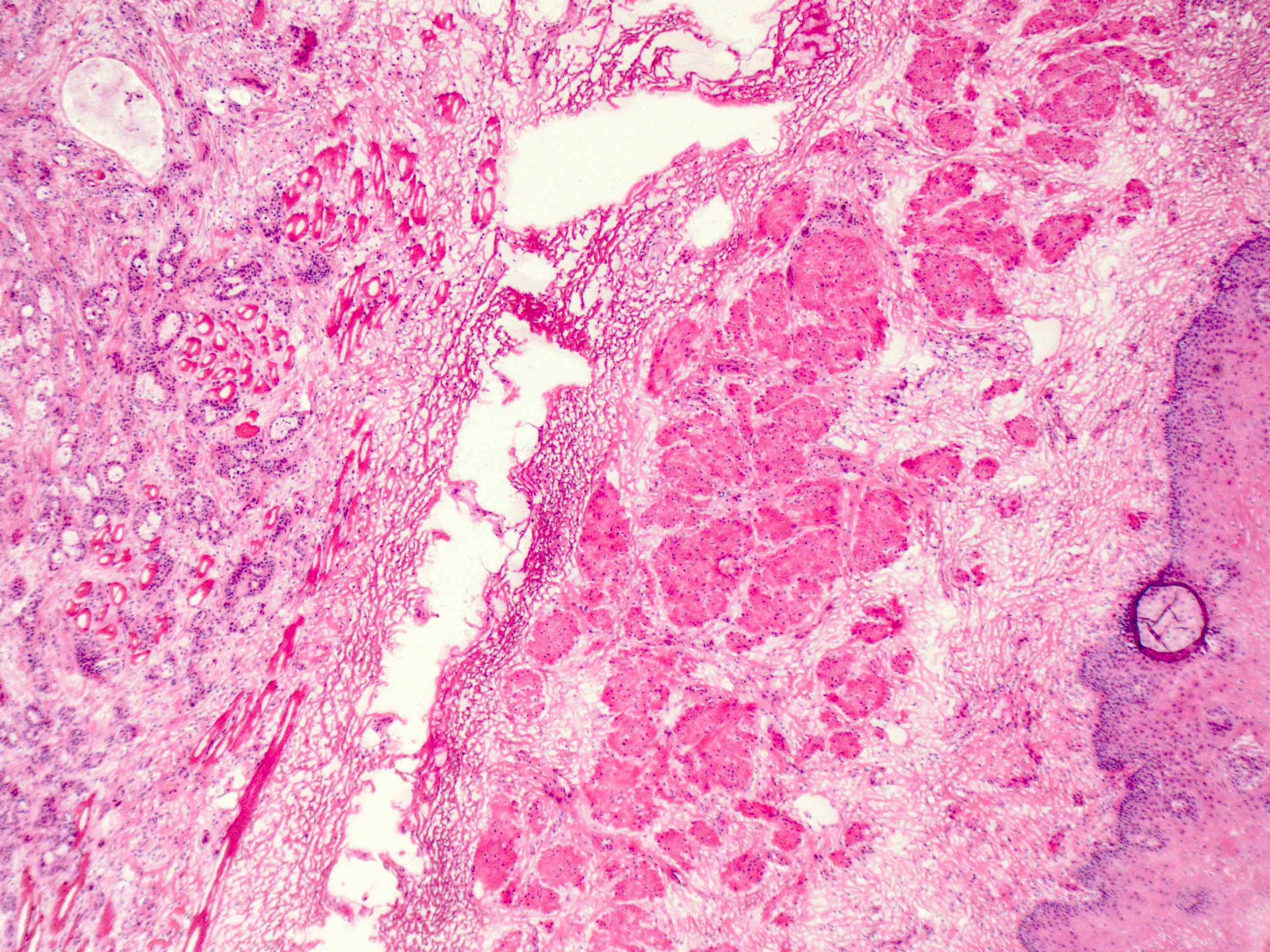
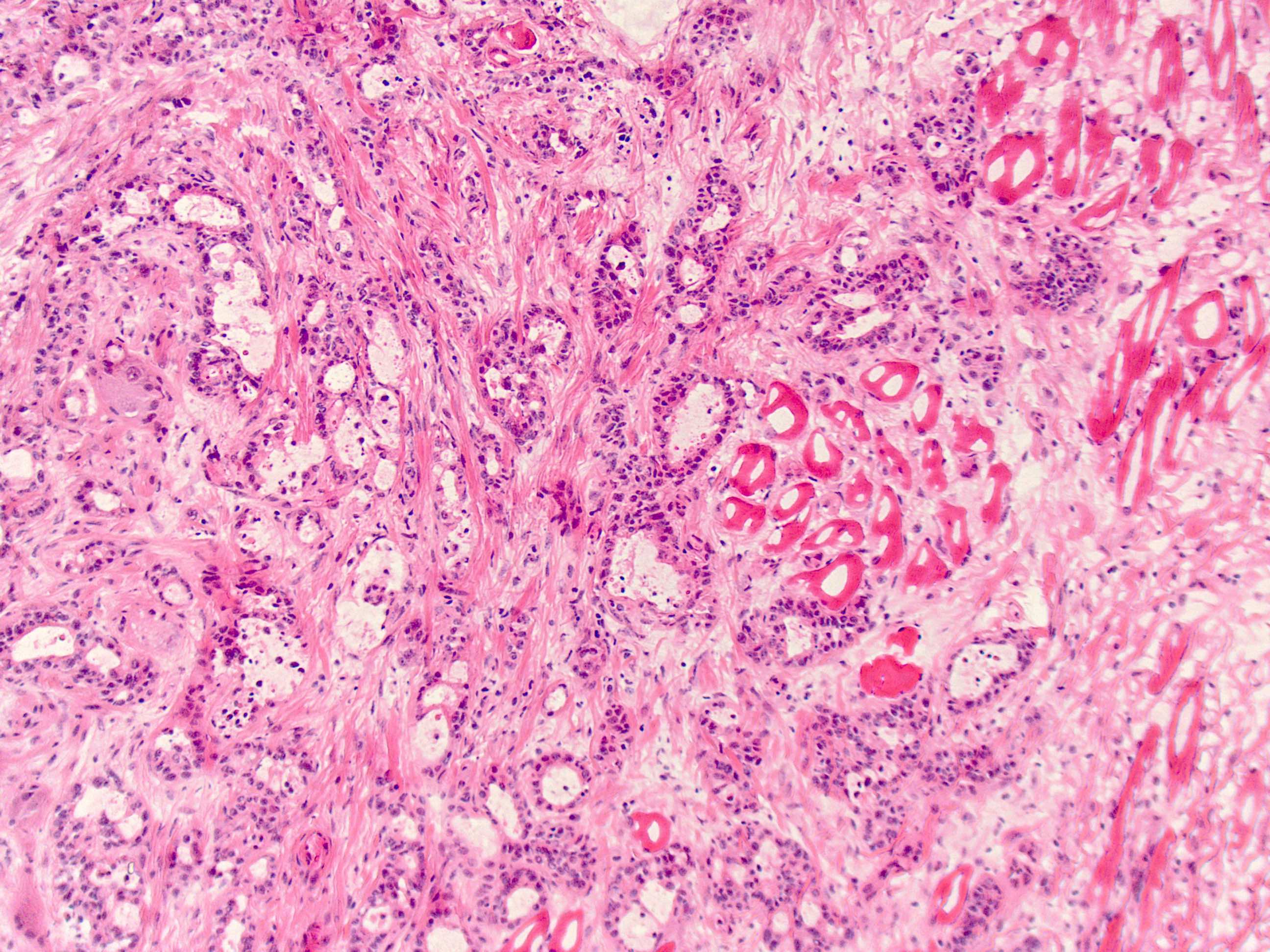
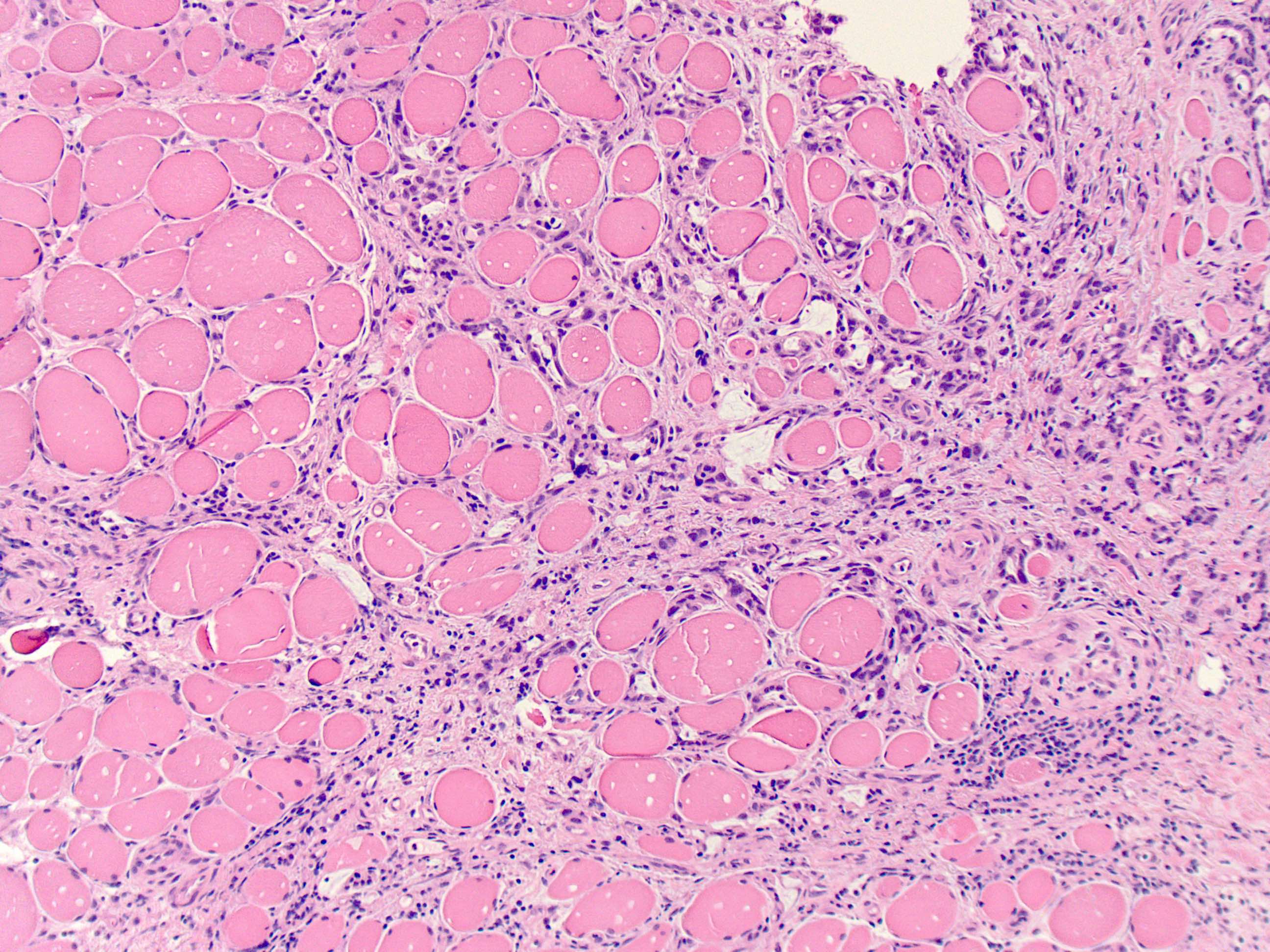
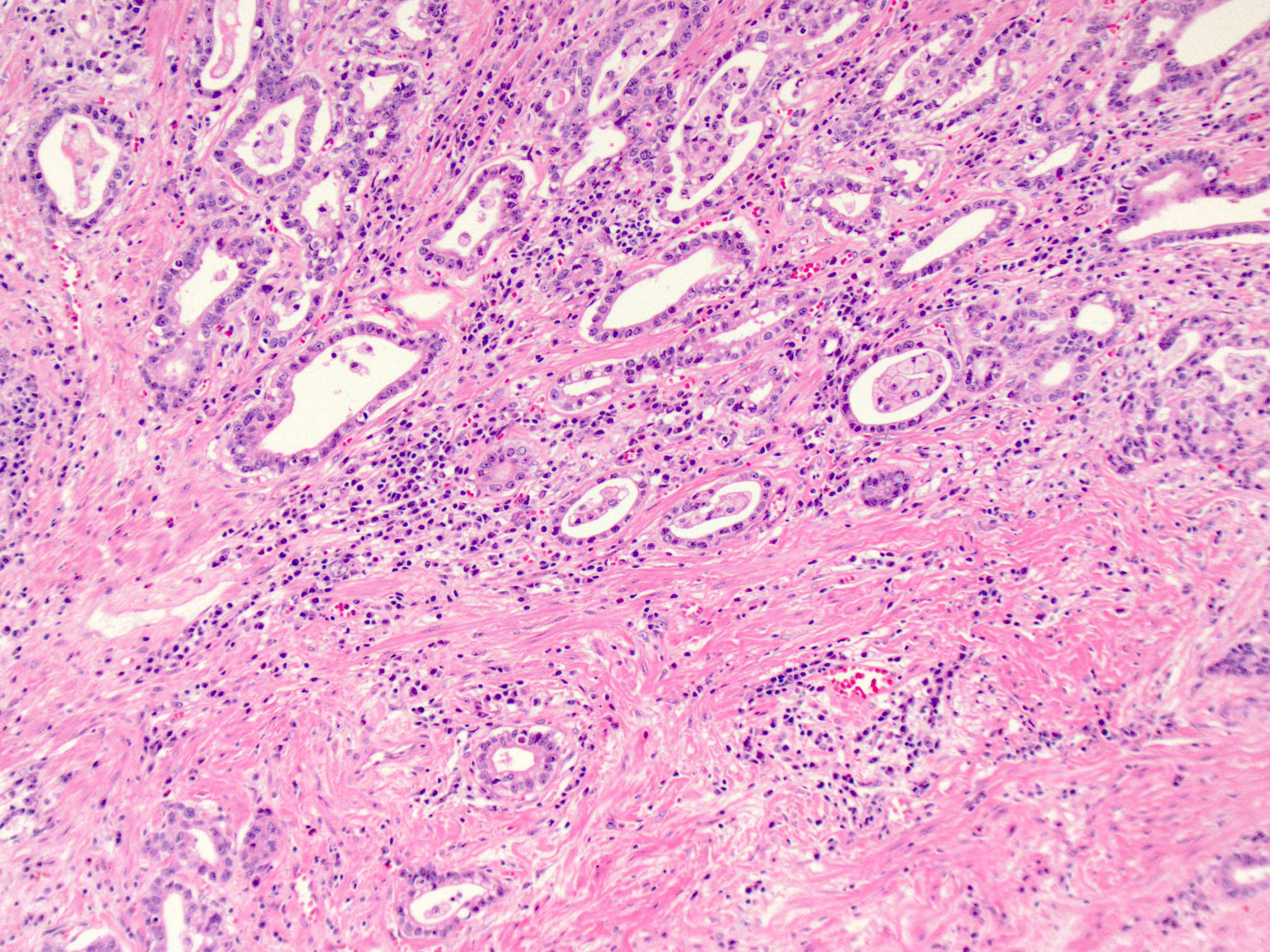
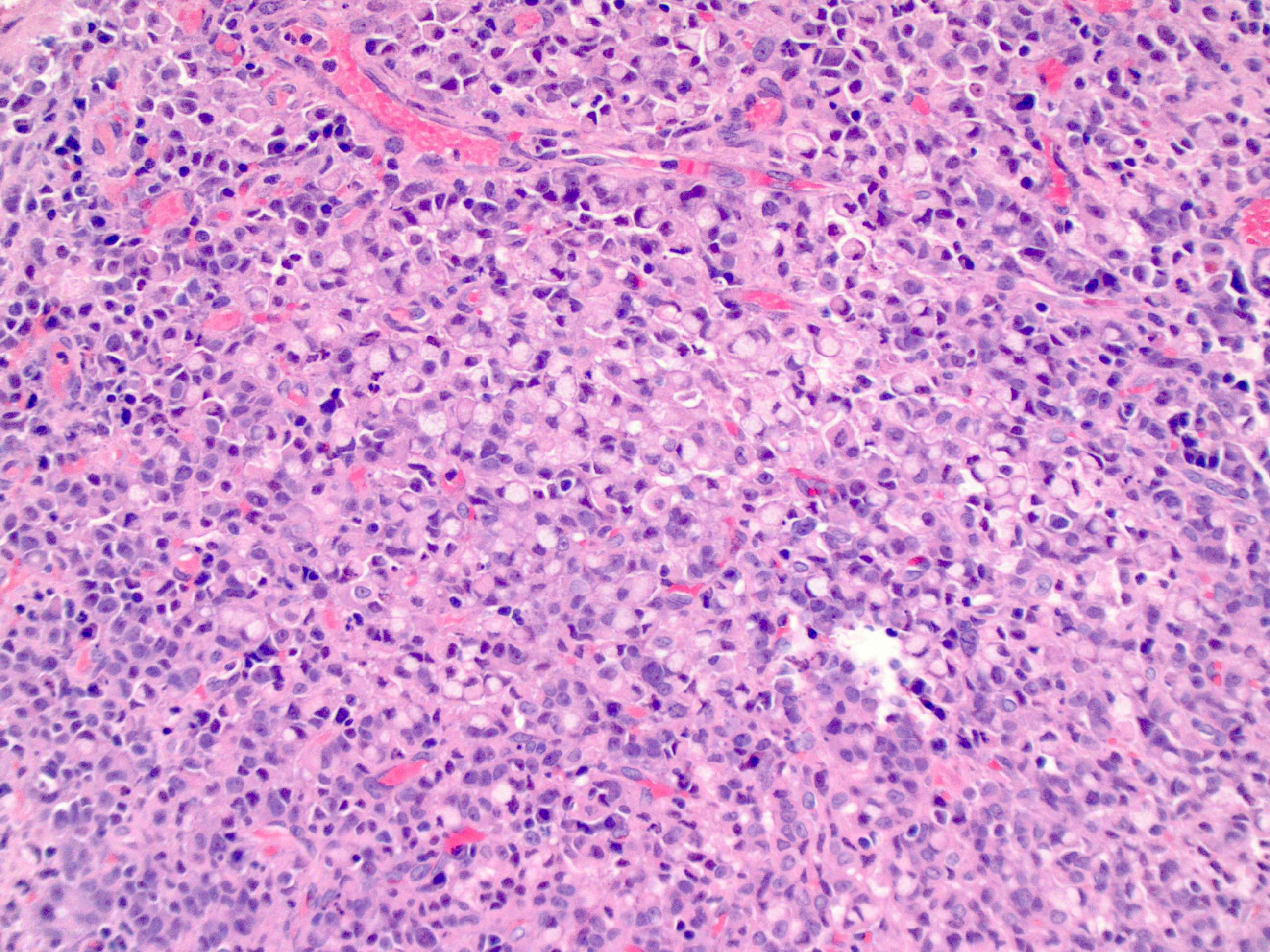
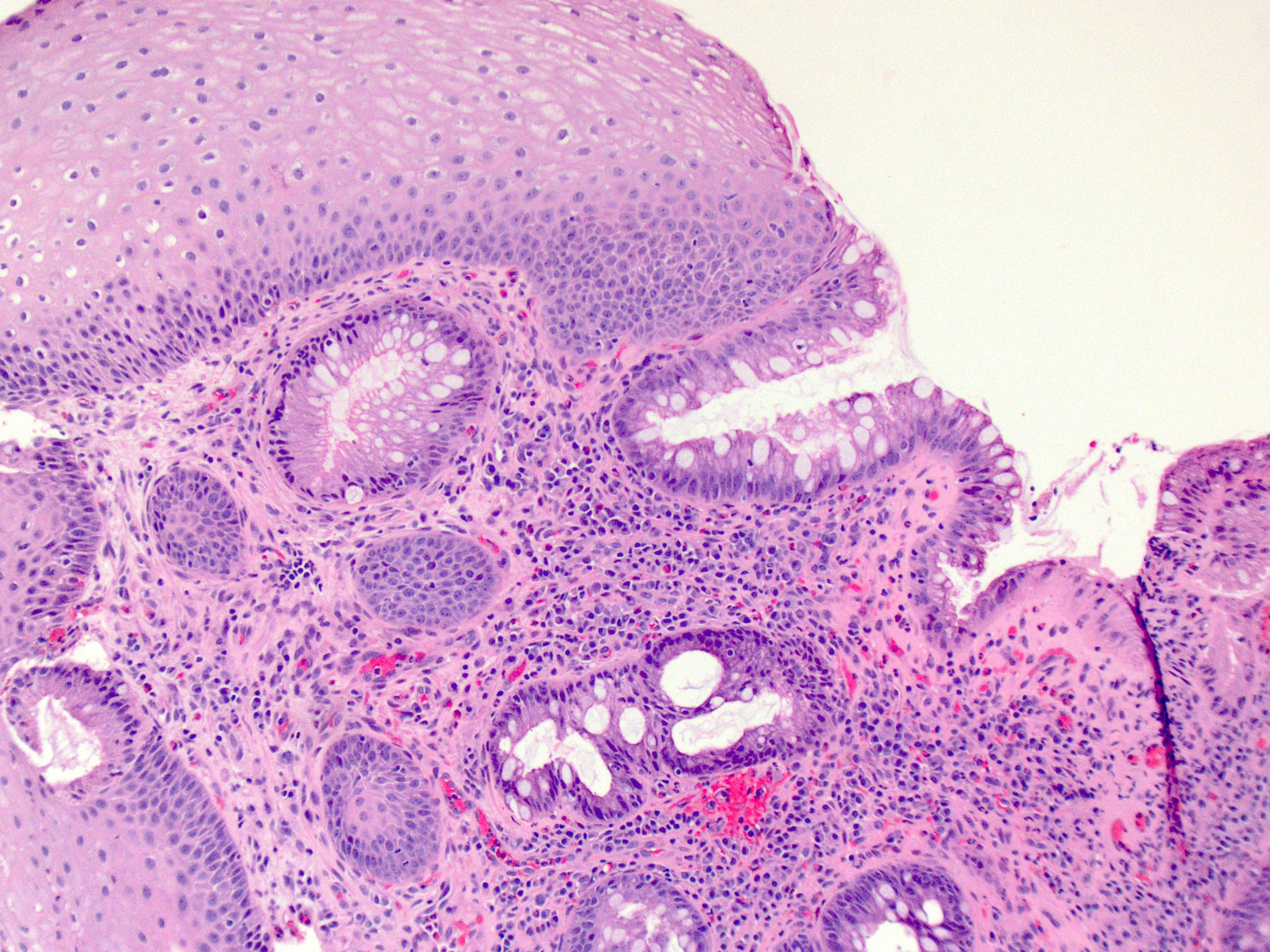
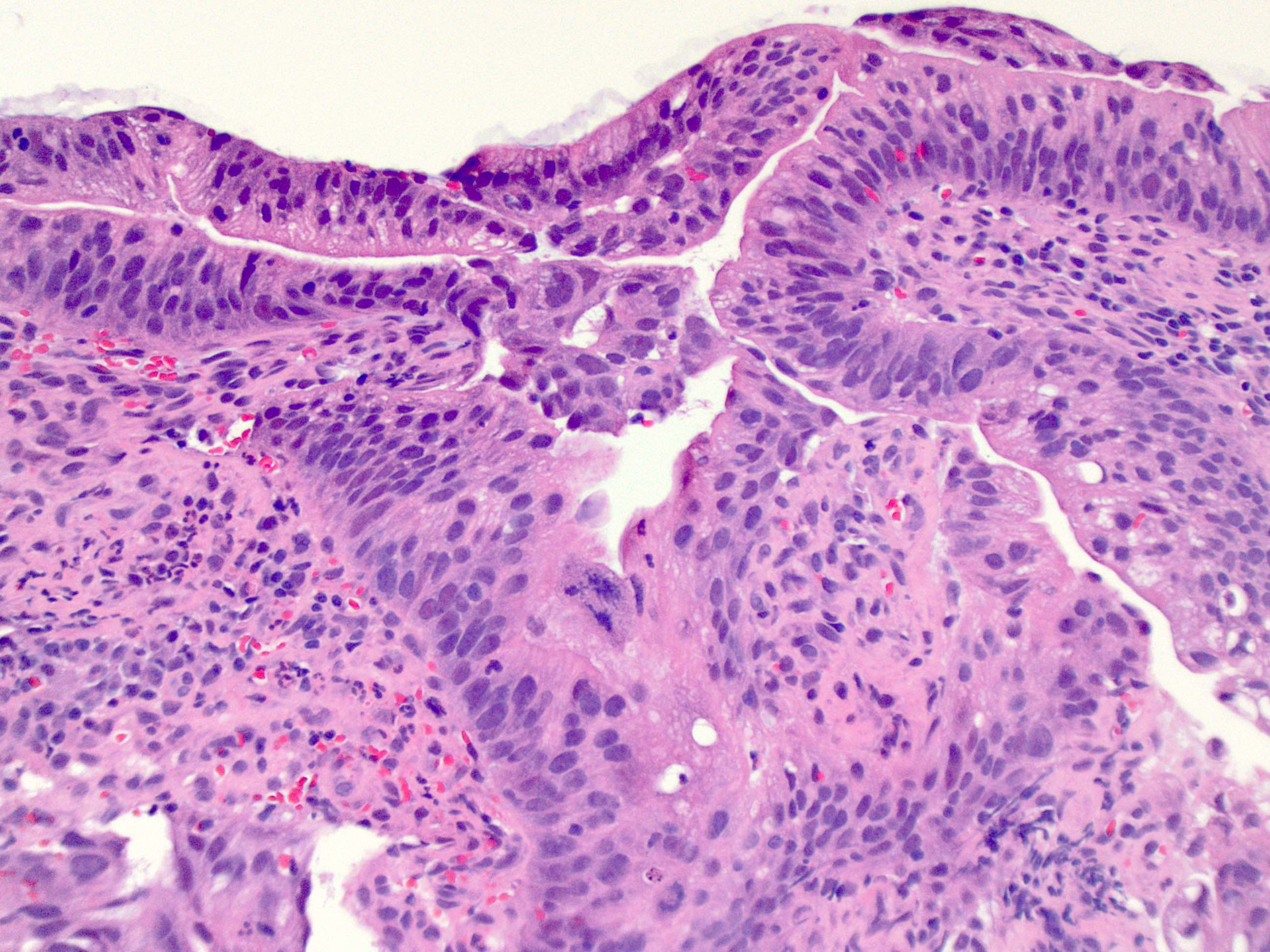
Microscopic (histologic) description
- Will show either gastric, intestinal or mixed lineage
- If in the lower esophagus, may show adjacent Barrett esophagus with intestinal metaplasia or dysplasia
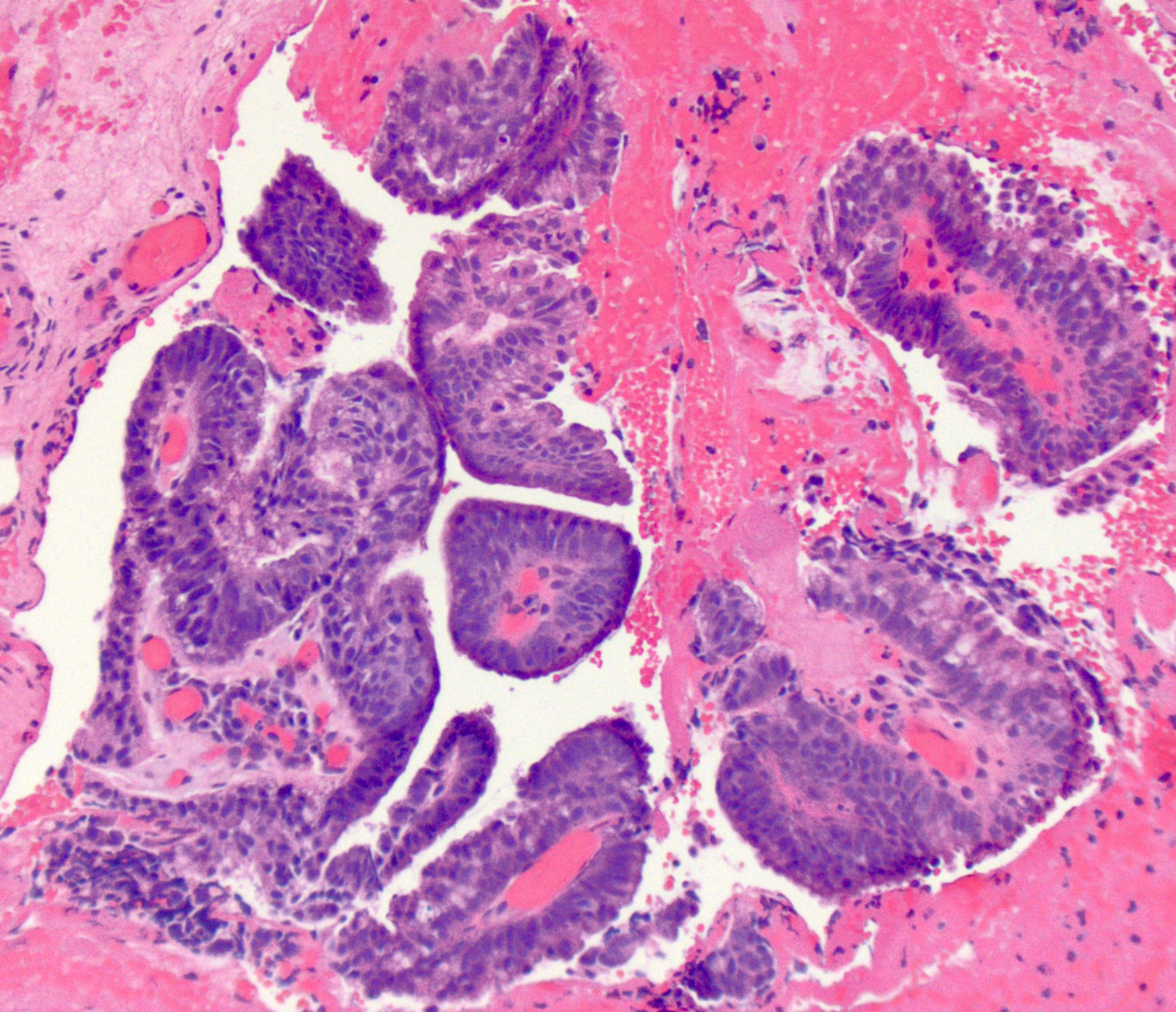
- Dysplasia may be low or high grade
- Low grade will have cytological atypia but little to no architectural atypia
- High grade will have increased cytologic atypia and architectural abnormalities but the dysplastic epithelial cells are still limited by basement membrane
- Classified as having tubular, papillary, mucinous and signet ring cell patterns
- Papillary pattern may show micropapillary architecture (Pathol Int 2016;66:583)
- Tubular pattern is most common, with irregular, single or anastomosing tubular glandular structures and a single or stratified layer of malignant epithelium
- Mucin production is variable
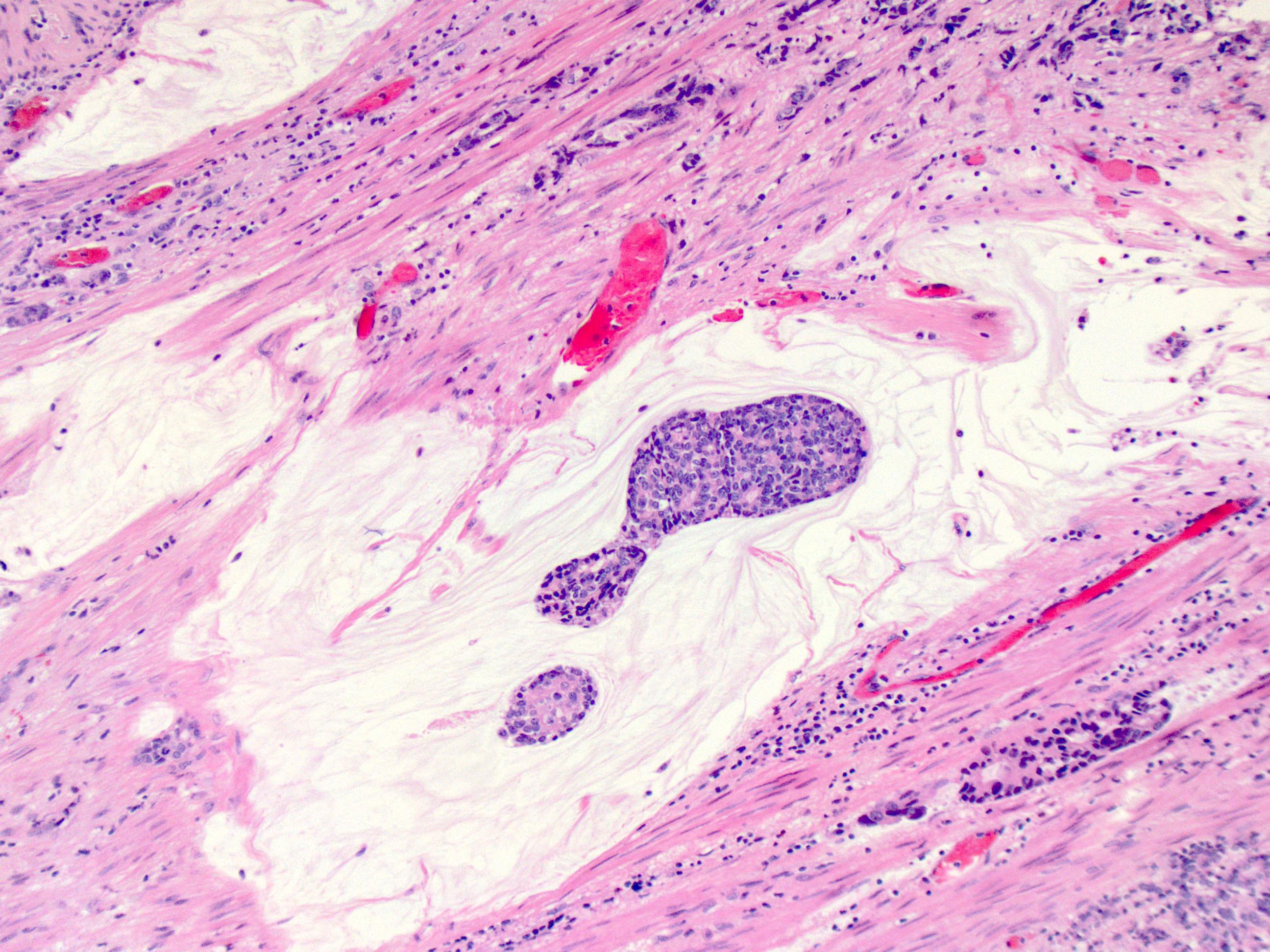
- ~50% of all esophageal adenocarcinomas are treated preoperatively with chemoradiation and therefore will show histologic changes consistent with treatment effect
- These include mucin pools that are acellular or containing small foci of residual adenocarcinoma
- Cytologic changes in the treated tumor cells include cytoplasmic eosinophilia, nuclear pyknosis and nuclear karyorrhexis
- Only residual viable tumor is considered in the determination of tumor stage and not the acellular mucin
- Similarly, lymph nodes with acellular mucin pools and therapy associated fibrosis but without viable tumor cells should be classified as no tumor within the lymph nodes (Mod Pathol 2018;31:4)
- Modified Ryan scheme for tumor regression score adapted by the College of American Pathologists (Histopathology 2005;47:141)
- 0: no viable cells (complete response)
- 1: single cells or rare groups of cancer cells (near complete response)
- 2: residual cancer with evident tumor regression but more than single cells or rare groups of cancer cells (partial response)
- 3: extensive residual cancer with no evidence of regression (poor or no response)
Microscopic (histologic) images
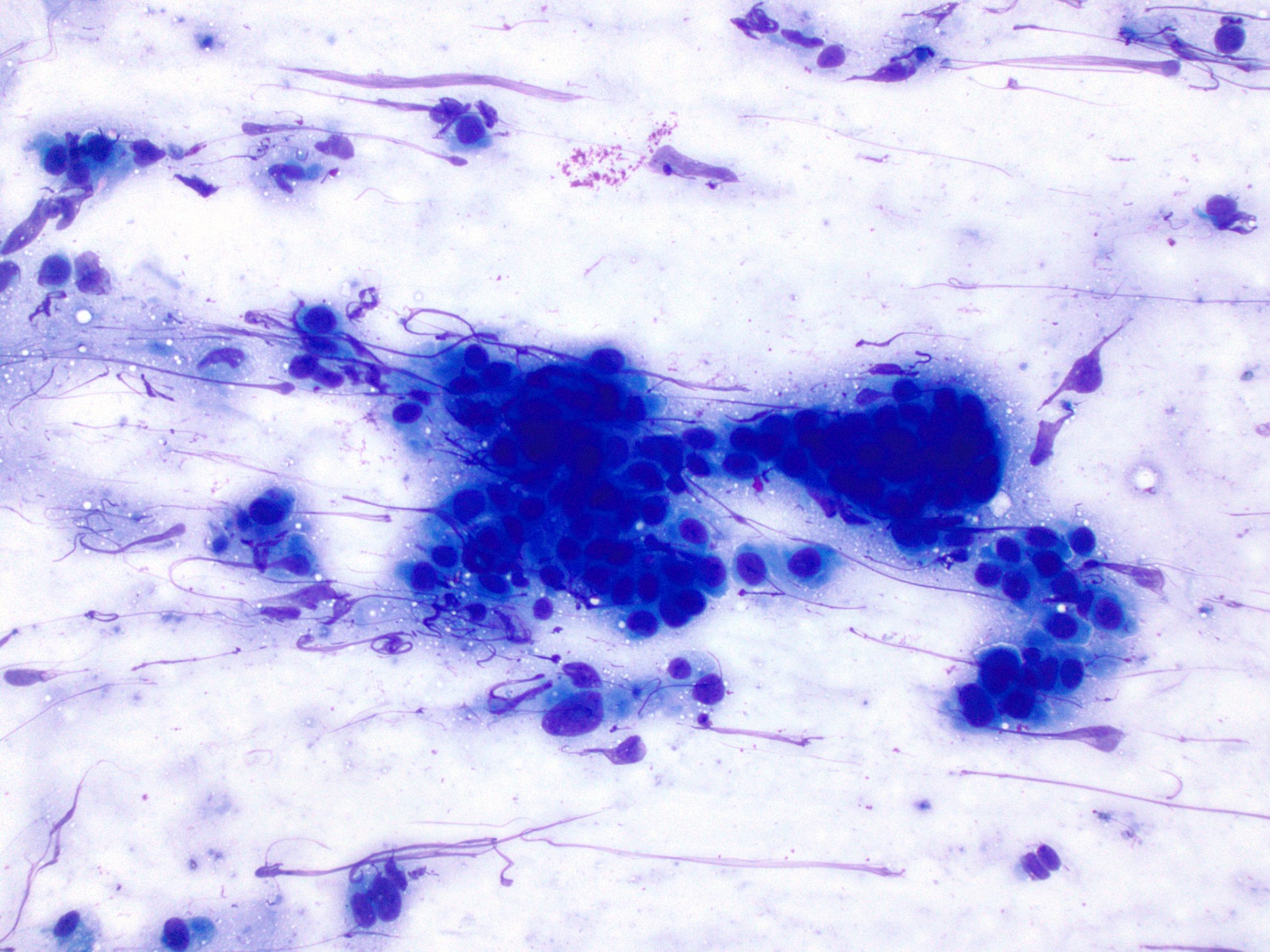
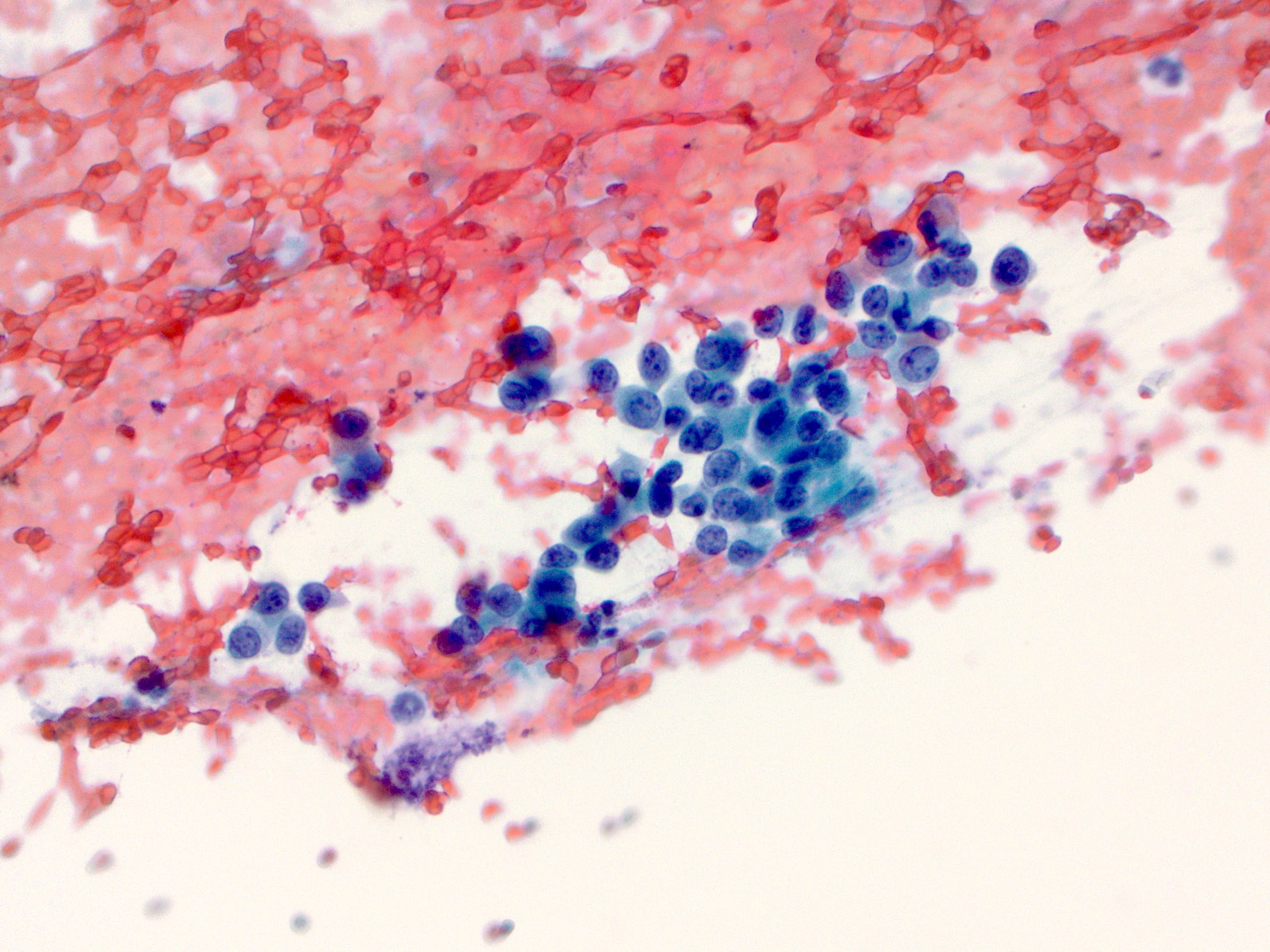
Cytology description
- Malignant glandular epithelial cells
- Smears are hypercellular with malignant cell groups showing nuclear enlargement, nuclear pleomorphism, hyperchromasia and irregular nuclear membranes
- Background may show tumor diathesis or necrosis
- Primary tumor is rarely sampled via cytology but endoscopic ultrasound guided fine needle aspiration (EUS-FNA) and transbronchial FNA sampling may be used to evaluate for paraesophageal and mediastinal / thoracic lymph node metastases (Clinics (Sao Paulo) 2011;66:1579)
Cytology images
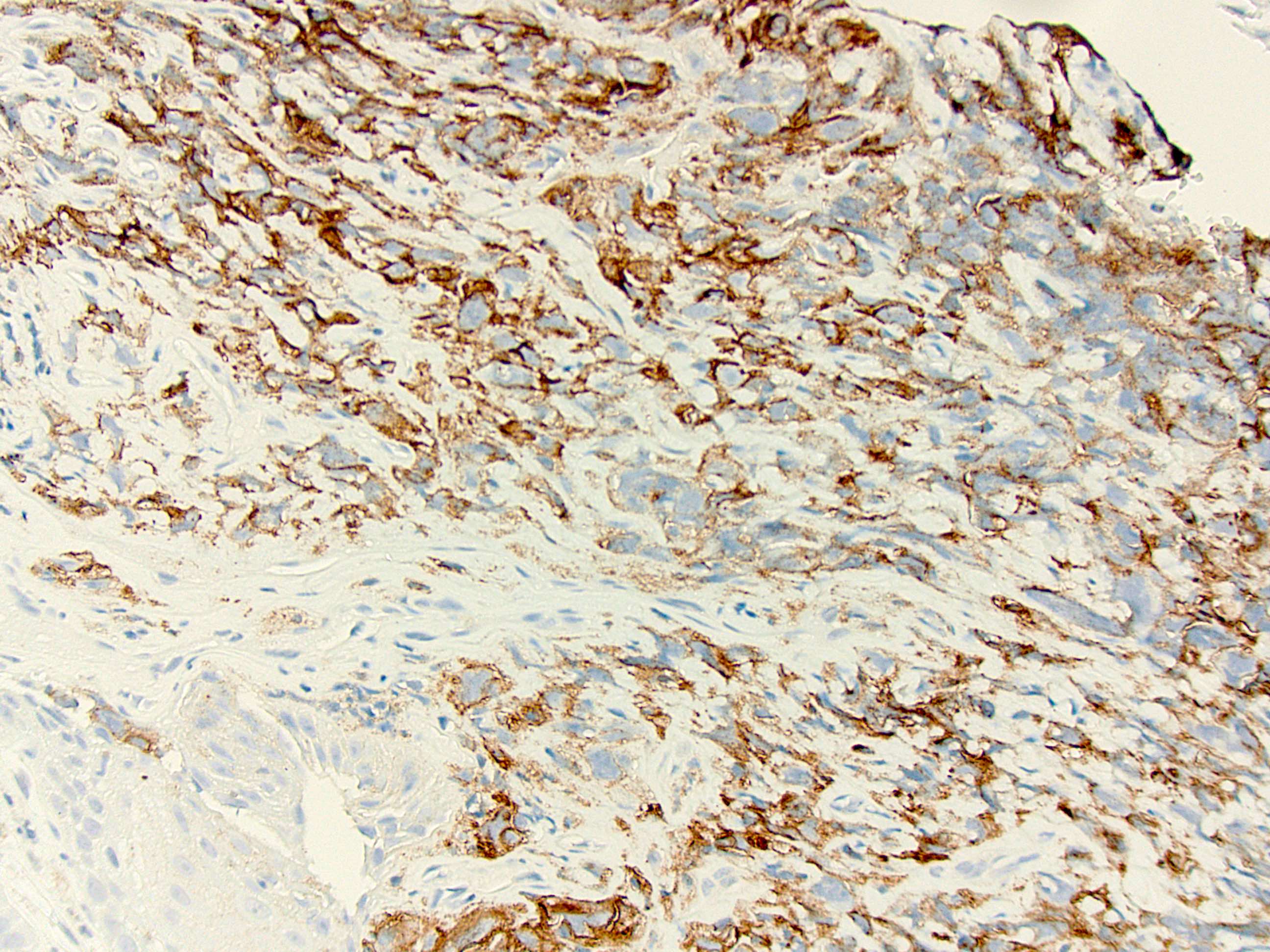
Positive stains
- Immunohistochemistry is rarely needed for a diagnosis
- CK7+, CK19+ (this will not distinguish it from gastric or pancreaticobiliary adenocarcinoma) (Mod Pathol 2004;17:49, Am J Surg Pathol 2002;26:1213)
- TTF1 has been shown to be positive in a small subset of esophageal adenocarcinoma (Arch Pathol Lab Med 2013;137:1094)
- HER2 testing by IHC or FISH is recommended in all patients with metastatic esophagogastric junction carcinoma at diagnosis (J Natl Compr Canc Netw 2015;13:194)
- Programmed death ligand 1 (PDL1) expression is currently used as a predictive biomarker (BioDrugs 2022;36:473)
- Expression can determine candidacy for immunotherapy (i.e., pembrolizumab, humanized monoclonal PD1 blocking antibody)
- Testing is recommended if metastatic disease is documented or suspected
- PDL1 expression is considered positive if the combined positive score (CPS) ≥ 1
- Pitfalls to PDL1 IHC evaluation include spatial and temporal intratumor heterogeneity (Pathologica 2023;115:57)
- PDL1 (22C3) indicated for gastric or esophagogastric junction adenocarcinoma
Negative stains
- CK20 (may show patchy staining in a minority of cases)
Molecular / cytogenetics description
- See Positive stains
Sample pathology report
- Esophagus, distal, endoscopic biopsy:
- Invasive moderately differentiated adenocarcinoma arising in the background of high grade dysplasia and intestinal metaplasia
- Esophagus, distal, endoscopic mucosal resection:
- Invasive poorly differentiated adenocarcinoma with signet ring cell differentiation
- Tumor is invasive into the submucosa, stage pT1b
- Lateral mucosal margin is negative for carcinoma, closest approach is 3 mm
- Deep resection margin is focally positive for carcinoma
- Negative for lymphovascular and perineural invasion
- No lymph nodes are present for evaluation
- Esophagogastric junction, distal esophagus and proximal stomach, esophagogastrectomy:
- Relationship of tumor to esophagogastric junction: tumor midpoint is located at the esophagogastric junction
- Distance of tumor center from eophagogastric junction:
- Other (specify): tumor midpoint is the esophagogastric junction
- Histologic type: adenocarcinoma
- Histologic grade: G2, moderately differentiated
- Tumor size: greatest dimension in centimeters is 1.9 cm
- Tumor extent: invades muscularis propria
- Treatment effect: present, with residual cancer showing evident tumor regression but more than single cells or rare small groups of cancer cells (partial response, score 2)
- Lymphovascular invasion: present
- Perineural invasion: not identified
- Margins: all margins negative for invasive carcinoma
- Closest margin to invasive carcinoma: proximal
- Distance from invasive carcinoma to closest margin: 1.8 cm
- Margin status for dysplasia and intestinal metaplasia: all margins negative for dysplasia and intestinal metaplasia
- Regional lymph node status
- Tumor present in regional lymph node(s)
- Number of lymph node(s) with tumor: 1
- Number of lymph node(s) examined: 8
- Distant metastasis: not applicable
- Pathologic stage classification: ypT2pN1
- Additional findings:
- Intestinal metaplasia (Barrett esophagus)
- Low grade glandular dysplasia
- High grade glandular dysplasia
- Special studies: HER2 IHC: positive, 3+
Differential diagnosis
- Differentiation between high grade glandular dysplasia and invasive adenocarcinoma into the lamina propria may be difficult, especially on small biopsies
- Intramucosal adenocarcinoma:
- Shows invasion into the lamina propria or into muscularis mucosa but not through the muscularis mucosa
- Desmoplasia favors invasive carcinoma when present
- Intramucosal adenocarcinoma:
- Squamous cell carcinoma of the esophagus:
- May be difficult to distinguish from poorly differentiated adenocarcinoma with solid areas
- Squamous cell carcinoma will be positive for CK5/6, p63, p40
- Positive mucicarmine staining will favor a diagnosis of adenocarcinoma
- Adenosquamous carcinoma:
- Composed of both malignant squamous and adenocarcinoma components
- The 2 components may be intermixed or separate
- Mucoepidermoid carcinoma (J Thorac Oncol 2011;6:1426):
- Rarely arises in the esophagus
- Composed of glands and nests of malignant squamoid cells, mucin containing glandular cells and intermediate cells
- Neuroendocrine tumors, especially those with prominent pseudoglandular architecture:
- Neuroendocrine tumors will show positivity for synaptophysin, chromogranin, CD56, INSM1
Additional references
Board review style question #1
Board review style answer #1
A. Barrett esophagus / intestinal metaplasia. Patients with Barrett esophagus have a 10 - 55 times higher risk of adenocarcinoma. Candida esophagitis (B), parakeratosis (C) and proton pump inhibitor therapy (D) do not increase the risk of glandular dysplasia and adenocarcinoma. Atypical parakeratosis may overlie a focus of squamous dysplasia. Proton pump inhibitor therapy may have some protective effect but this association needs more evidence.
Comment Here
Reference: Adenocarcinoma
Comment Here
Reference: Adenocarcinoma
Board review style question #2
A biopsy of a thoracic lymph node showed a CK7+, CK20- and TTF1+ metastatic adenocarcinoma. Is this immunohistochemistry profile sufficient to distinguish between an esophageal versus a pulmonary primary?
- Likely pulmonary primary but esophageal primary needs to be excluded via clinical / endoscopic / radiographic correlation
- No, does not support either esophageal or pulmonary primary
- Yes, favors esophageal primary
- Yes, favors pulmonary primary
Board review style answer #2
A. Likely pulmonary primary but esophageal primary needs to be excluded via clinical / endoscopic / radiographic correlation. A CK7+, CK20- and TTF1+ metastatic adenocarcinoma is likely to be of pulmonary origin; however, since a minority of esophageal adenocarcinomas are TTF1+, it is prudent to rule out that possibility by correlating with clinical findings. Answers B, C and D are incorrect because a CK7+, TTF+ immunohistochemistry profile is seen in both primary lung and esophageal adenocarcinoma.
Comment Here
Reference: Adenocarcinoma
Comment Here
Reference: Adenocarcinoma