Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Memon A, Ud Din N. Synovial & tenosynovial chondromatosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/jointssynovialosteochondromatosis.html. Accessed December 26th, 2024.
Definition / general
- Synovial chondromatosis is a locally aggressive neoplasm characterized by multiple hyaline cartilaginous nodules involving joint spaces, subsynovial tissue or tenosynovium
Essential features
- Benign locally aggressive neoplasm characterized by formation of hyaline cartilaginous nodules within the synovium or free within joint spaces
- Involves large joints, 60 - 70% of cases affecting the knee
- Occurs in the third to fifth decade and is 2 - 4 times more common in men than women
- Can recur in 15 - 20% of patients, more commonly in tenosynovial cases
- Malignant transformation is uncommon; reported in 5 - 10% of cases
Terminology
- Not recommended: synovial osteochondromatosis; synovial chondrosis; Reichel syndrome or Reichel-Jones-Henderson syndrome; synovial chondrometaplasia (Pediatr Surg Int 1999;15:437, J Am Acad Orthop Surg 2008;16:268)
ICD coding
Epidemiology
- Rare neoplasm, with an estimated incidence of ~1.8 cases per million person years (JBJS Rev 2016;4:e2)
- Typically occurs in third to fifth decades of life, with men being affected 2 - 4 times more frequently than women (Hum Pathol 1998;29:683, JBJS Rev 2016;4:e2)
Sites
- Involves the large joints; 60 - 70% of cases affecting the knee, followed by hip, shoulder, elbow, ankle and wrist
- Can affect any joint, including temporomandibular and intervertebral joints (Am Fam Physician 1987;35:157)
- May be extra-articular (tenosynovial chondromatosis or bursal chondromatosis), typically arising in hands and feet (Am J Surg Pathol 2003;27:1260)
Pathophysiology
- Benign neoplastic, rather than metaplastic, lesion
- Classified as primary and secondary synovial chondromatosis
- Monoarticular in primary form and may be multiarticular in secondary form
- Primary synovial chondromatosis is a self limited process that occurs in an otherwise normal joint
- Secondary chondromatosis occurs in a joint previously afflicted with disease, often post traumatic or degenerative osteoarthritis
- There are 3 phases of articular disease (J Bone Joint Surg Am 1977;59:792):
- Initial phase: active intrasynovial disease only, with no loose bodies
- Transitional phase: both active intrasynovial proliferation and free loose bodies
- Inactive phase: resolution of synovial proliferation but loose bodies remain in the joint
- Fusion between fibronectin 1 (FN1) and activin receptor 2A (ACVR2A) is found in at least 50% of cases of benign synovial chondromatosis, as well as in cases of malignant synovial chondromatosis (Mod Pathol 2019;32:1762)
- Chromosome 6 abnormalities have also been observed (Cancer Genet Cytogenet 2003;140:18, Br J Cancer 1996;74:251, Virchows Arch 1998;433:189)
- Possible role of fibroblast growth factor receptor 3 (FGFR3) and fibroblast growth factor 9 (FGF9) in primary synovial chondromatosis (Int J Exp Pathol 2000;81:183)
- Small risk of malignant transformation to chondrosarcoma (Skeletal Radiol 1993;22:623)
Etiology
- Although the etiology of primary synovial chondromatosis is unknown, a neoplastic etiology is supported by the identification of chromosomal abnormalities
- Elevated levels of bone morphogenic protein, interleukin 6 and vascular endothelial growth factor A have been found in affected synovial joints but importance is uncertain (StatPearls: Synovial Chondromatosis [Accessed 15 August 2022])
- Secondary synovial chondromatosis can occur due to mechanical changes in a joint due to degenerative arthropathy with formation of loose osteochondral bodies
Clinical features
- May be asymptomatic
- Pain and swelling, locking, crepitus and limited range of movement (JBJS Rev 2016;4:e2)
- Palpable nodules on examination
- Malignant change may be associated with persistent and increased pain
Diagnosis
- Use of diagnostic radiographic imaging of involved joints
- Histological evaluation of cartilaginous nodules
Laboratory
- Serological tests for arthritis in cases of secondary synovial chondromatosis
Radiology description
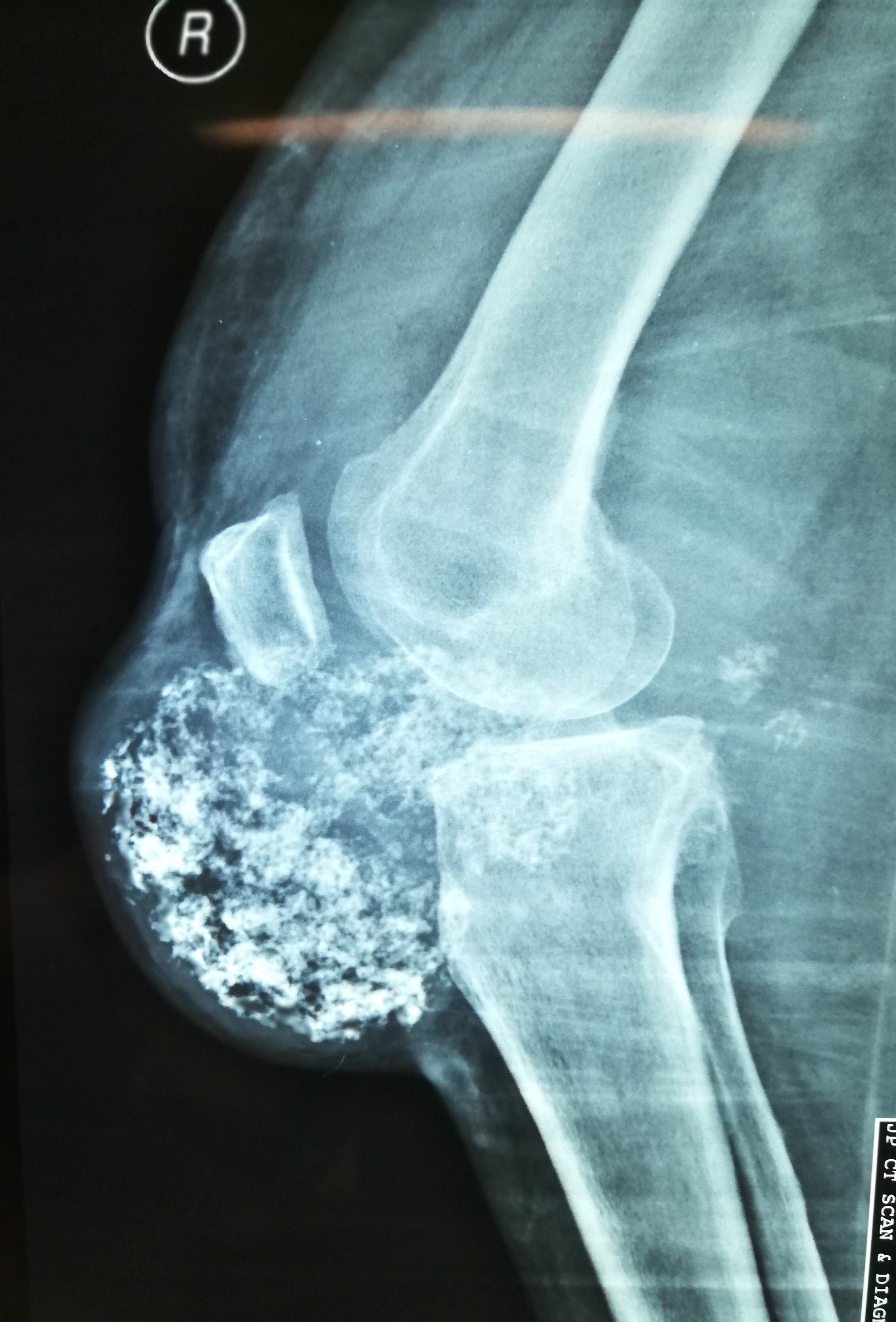
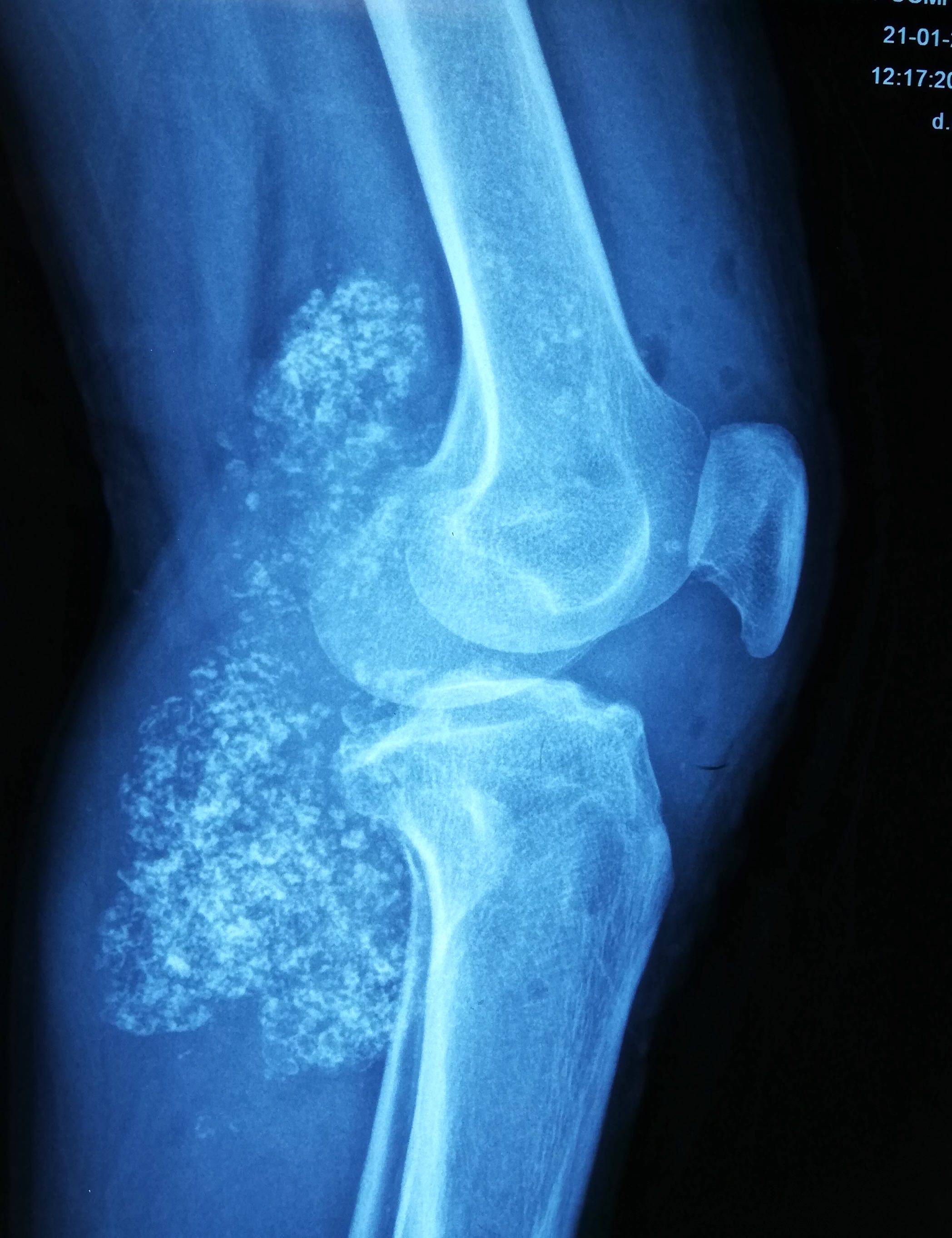
- Plain radiographs reveal multiple intra-articular calcifications of similar size and shape in 70 - 95% of cases (Radiographics 2007;27:1465)
- Or chondroid mineralization (punctate, ring and arc, so called feathery calcification) (Eur Radiol 2002;12:2112)
- Extrinsic erosion of bone is seen in 20 - 50% of cases
- Computed tomography (CT) optimally depicts the calcified intra-articular fragments and extrinsic bone erosion
- Magnetic resonance imaging (MRI) findings are more variable, depending on the degree of mineralization, although the most common pattern (77% of cases) reveals low to intermediate signal intensity with T1 weighting and very high signal intensity with T2 weighting with hypointense calcifications (Radiographics 2007;27:1465)
Radiology images
Prognostic factors
- Disease recurs in 15 - 20% of cases with higher rates reported in tenosynovial cases (JBJS Rev 2016;4:e2)
- Malignant transformation is uncommon and occurs in 5 - 10% of cases (Sarcoma 2014;2014:647939)
- Early or rapid growth after recurrence should raise suspicion of malignancy (Open Orthop J 2017;11:517)
Case reports
- 7 year old boy admitted due to pain in the right hip joint and limping for > 1 month (Medicine (Baltimore) 2018;97:e13199)
- 14 year old girl, a gymnast, with sustained pain in both elbows and limited elbow joint activity (BMC Musculoskelet Disord 2020;21:377)
- 30 year old man presented with a longstanding dull pain in front of the left ear (J Maxillofac Oral Surg 2017;16:387)
- 43 year old woman and 50 year old man presented with pain and stiffness in ankle (World J Orthop 2019;10:404)
- 53 year old woman presented with a left preauricular swelling (J Int Med Res 2021;49:3000605211000526)
Treatment
- Arthroscopic or open removal of loose bodies with or without a synovectomy
Clinical images
Gross description
- Multiple, grayish white, smooth or irregular, uniform or variably sized nodules as intra-articular loose bodies or embedded within / attached to synovium
Gross images
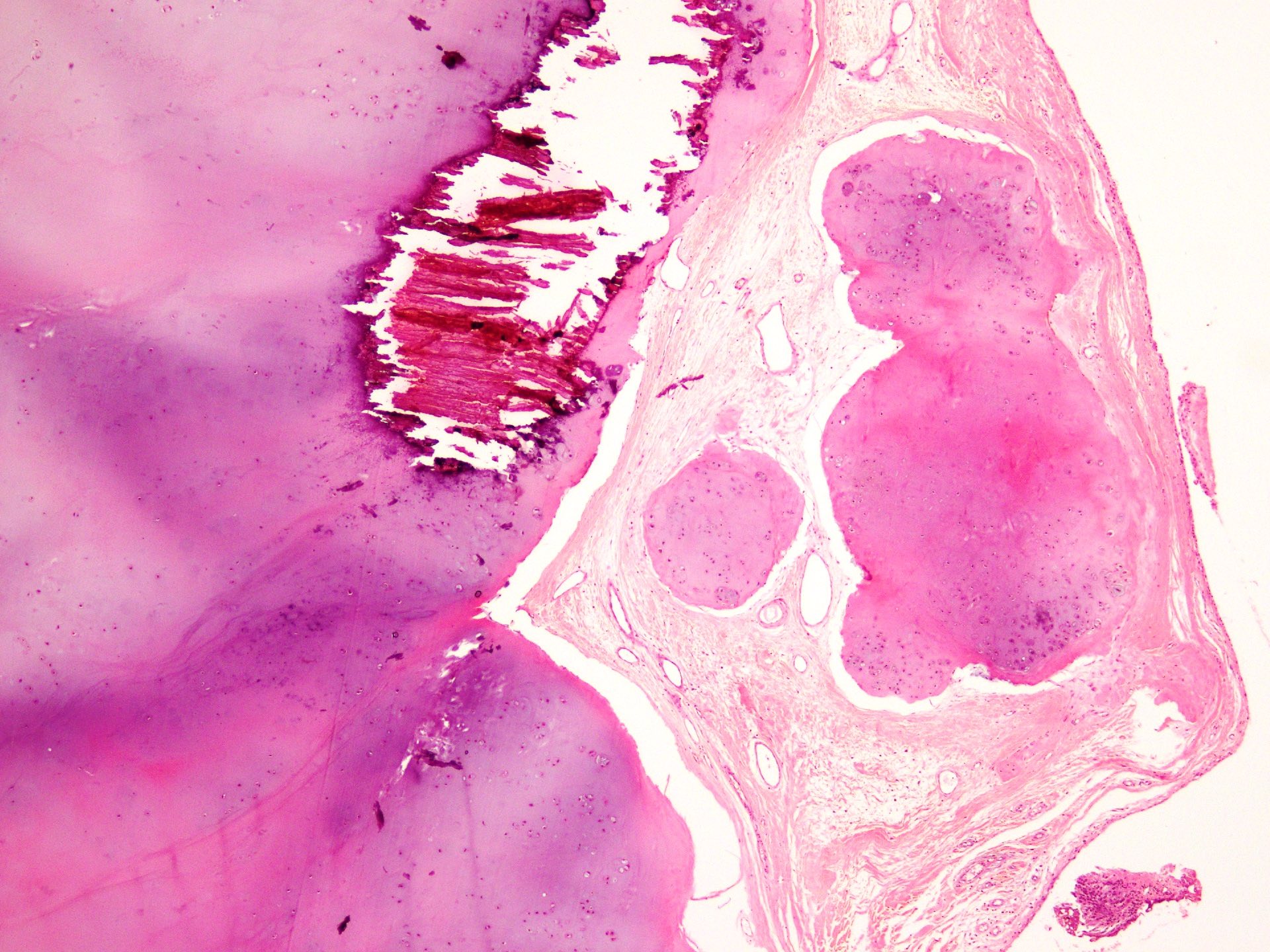
Microscopic (histologic) description
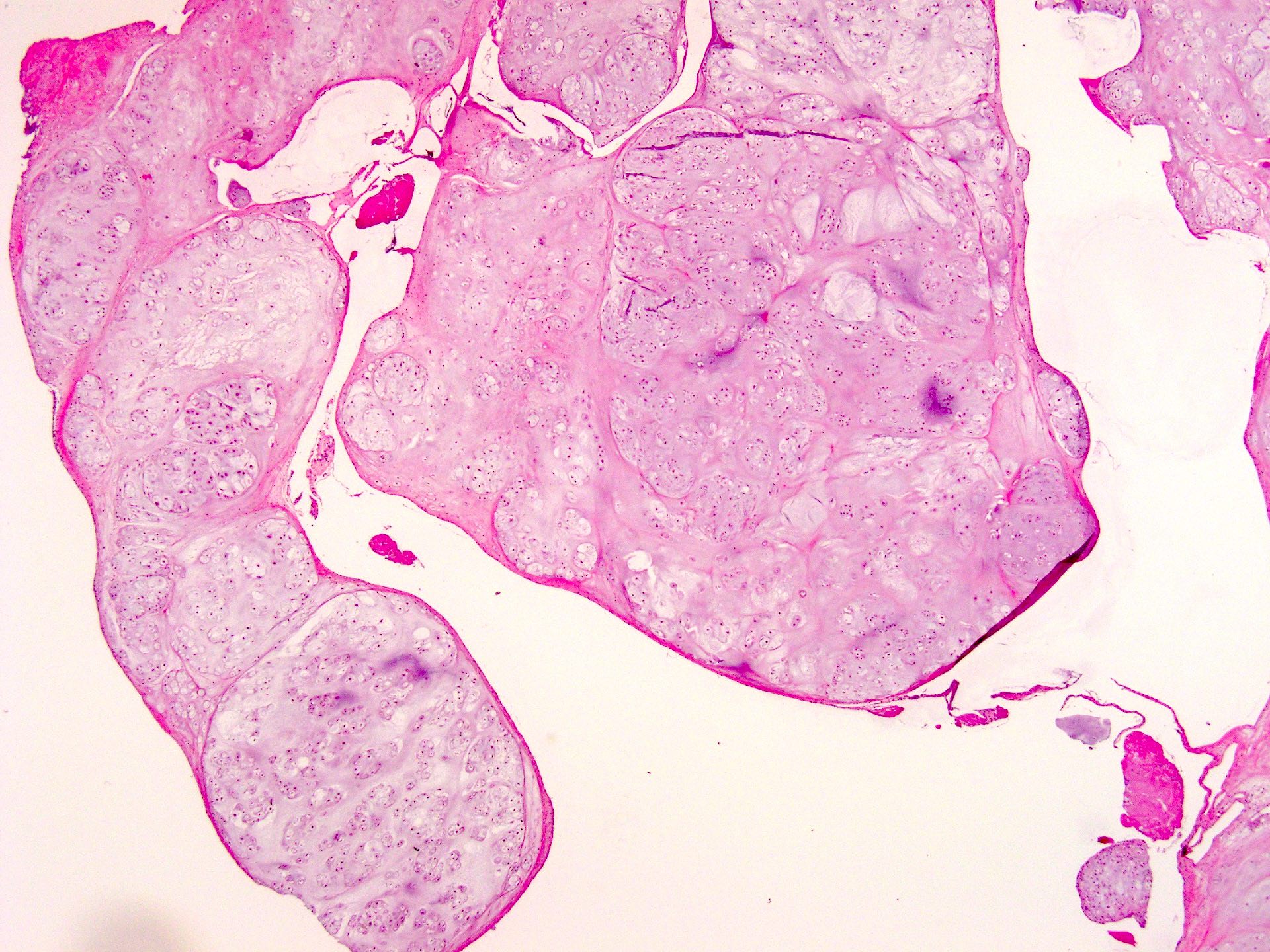
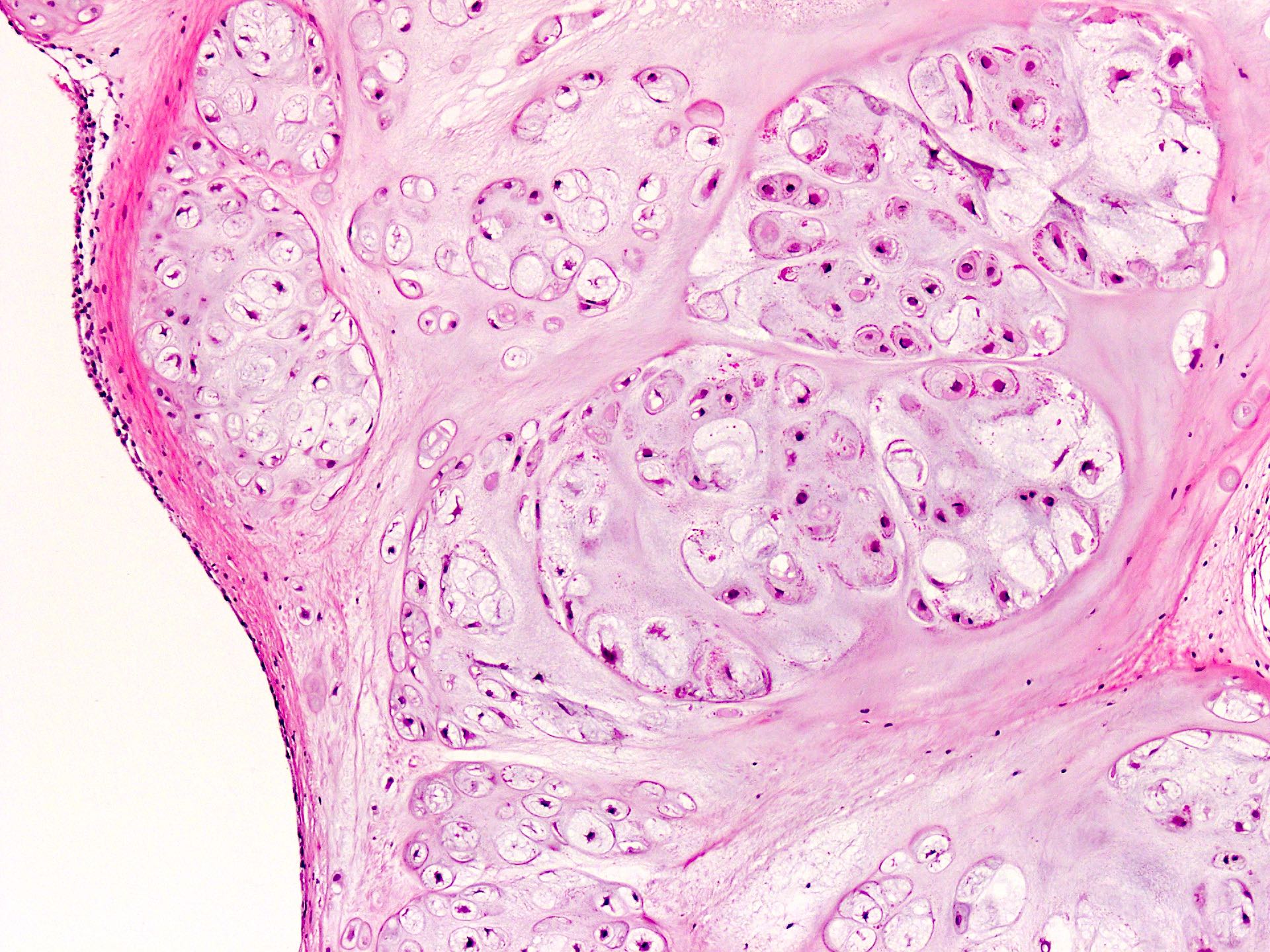
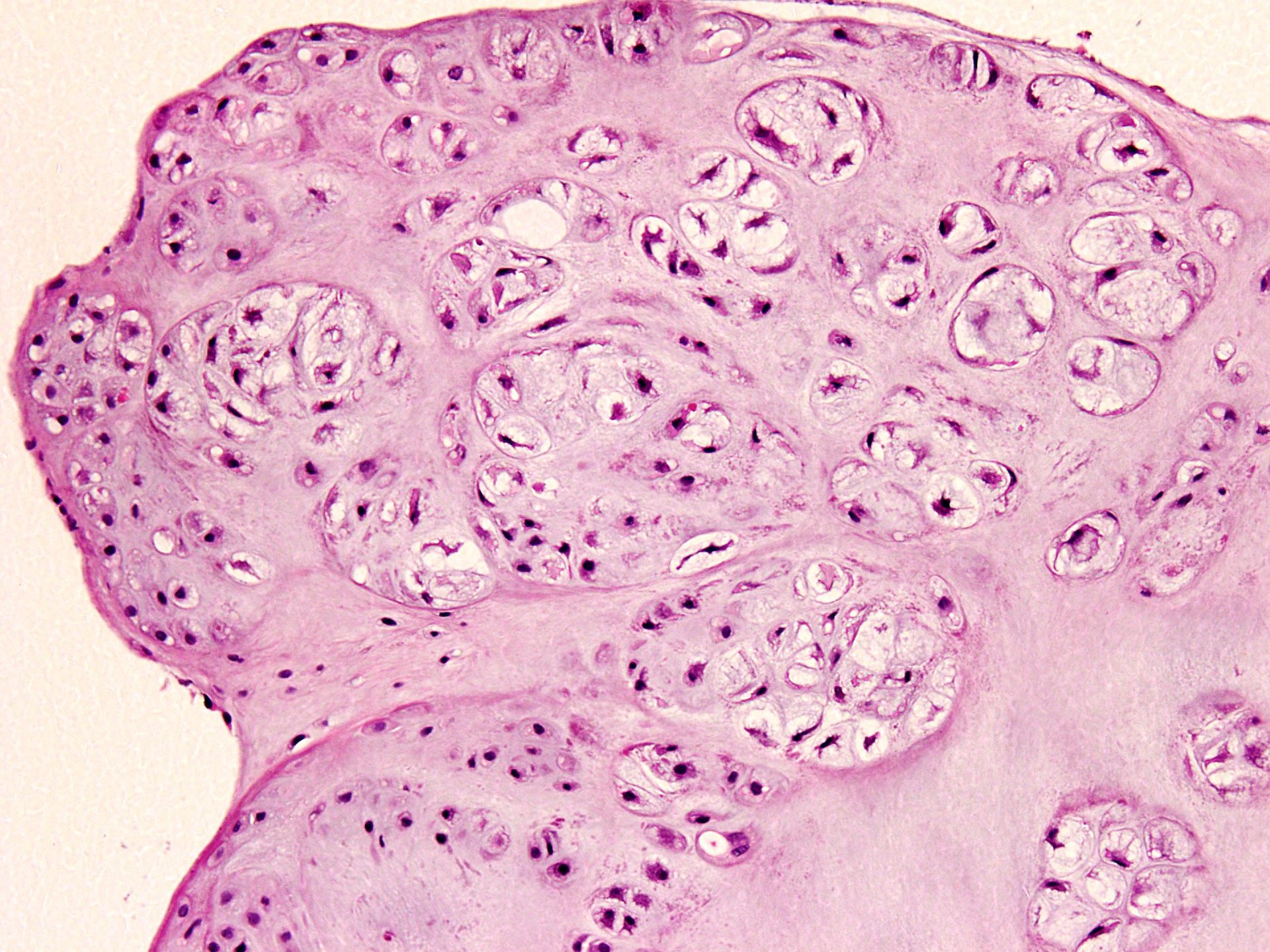
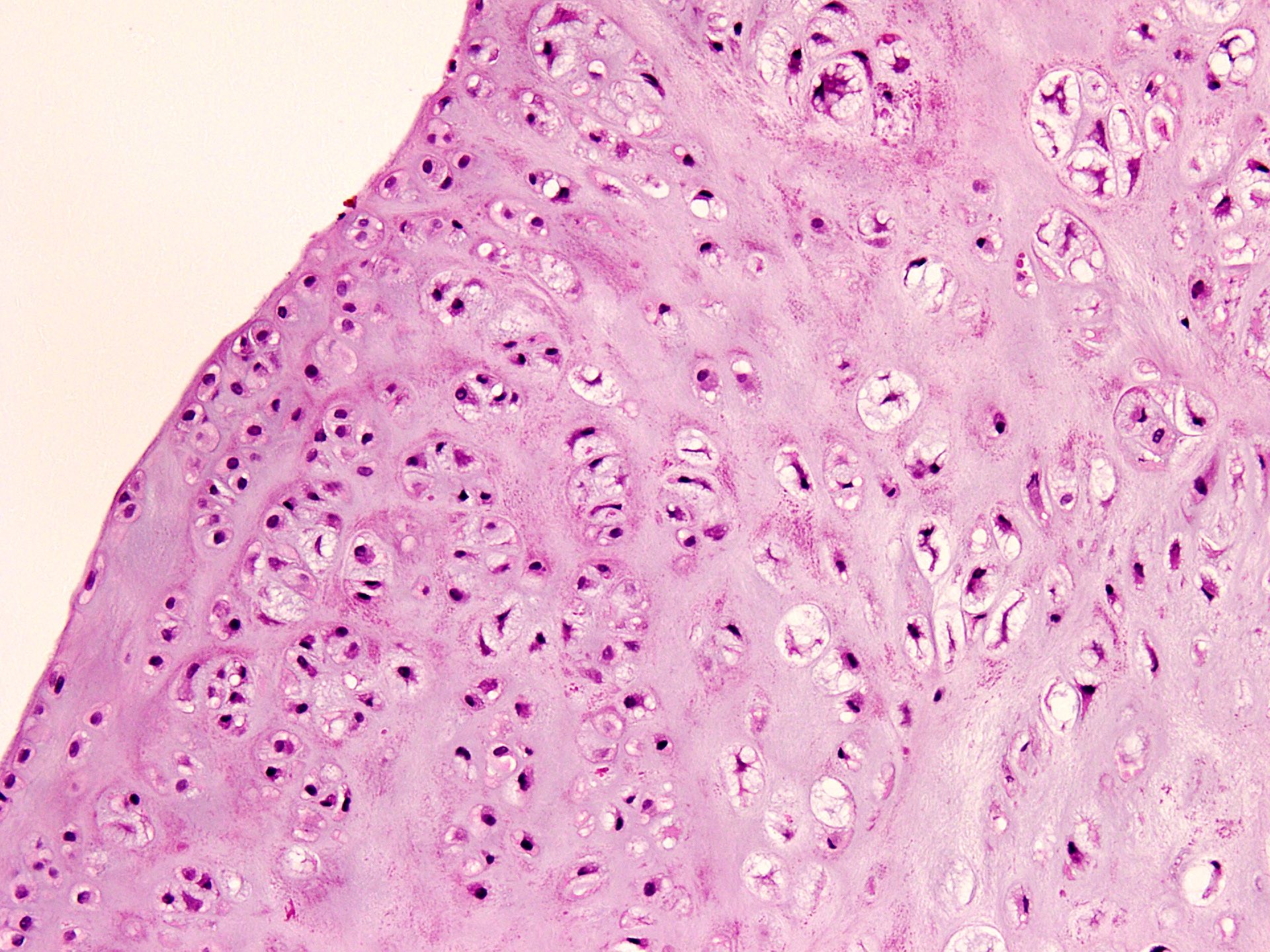
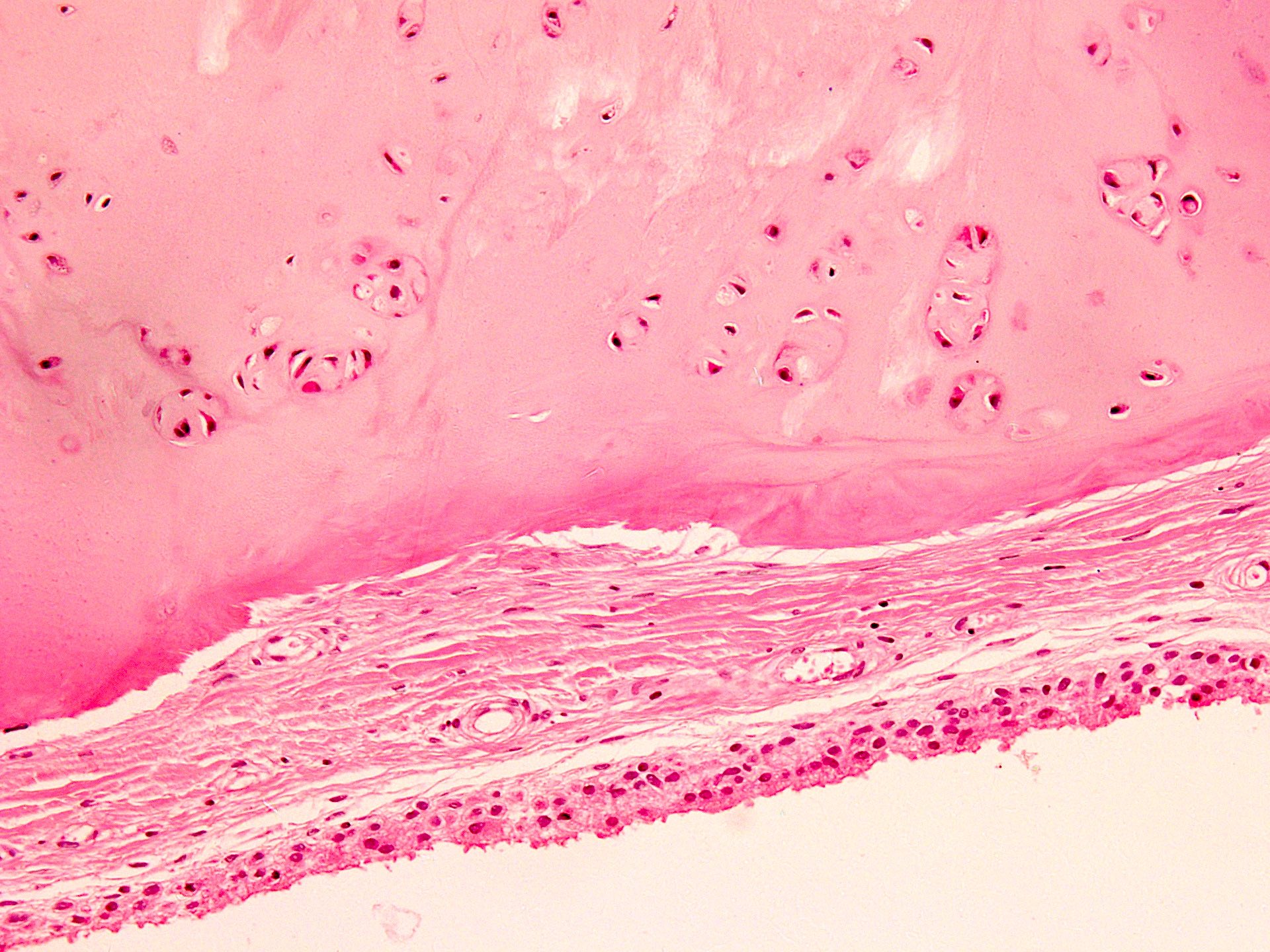
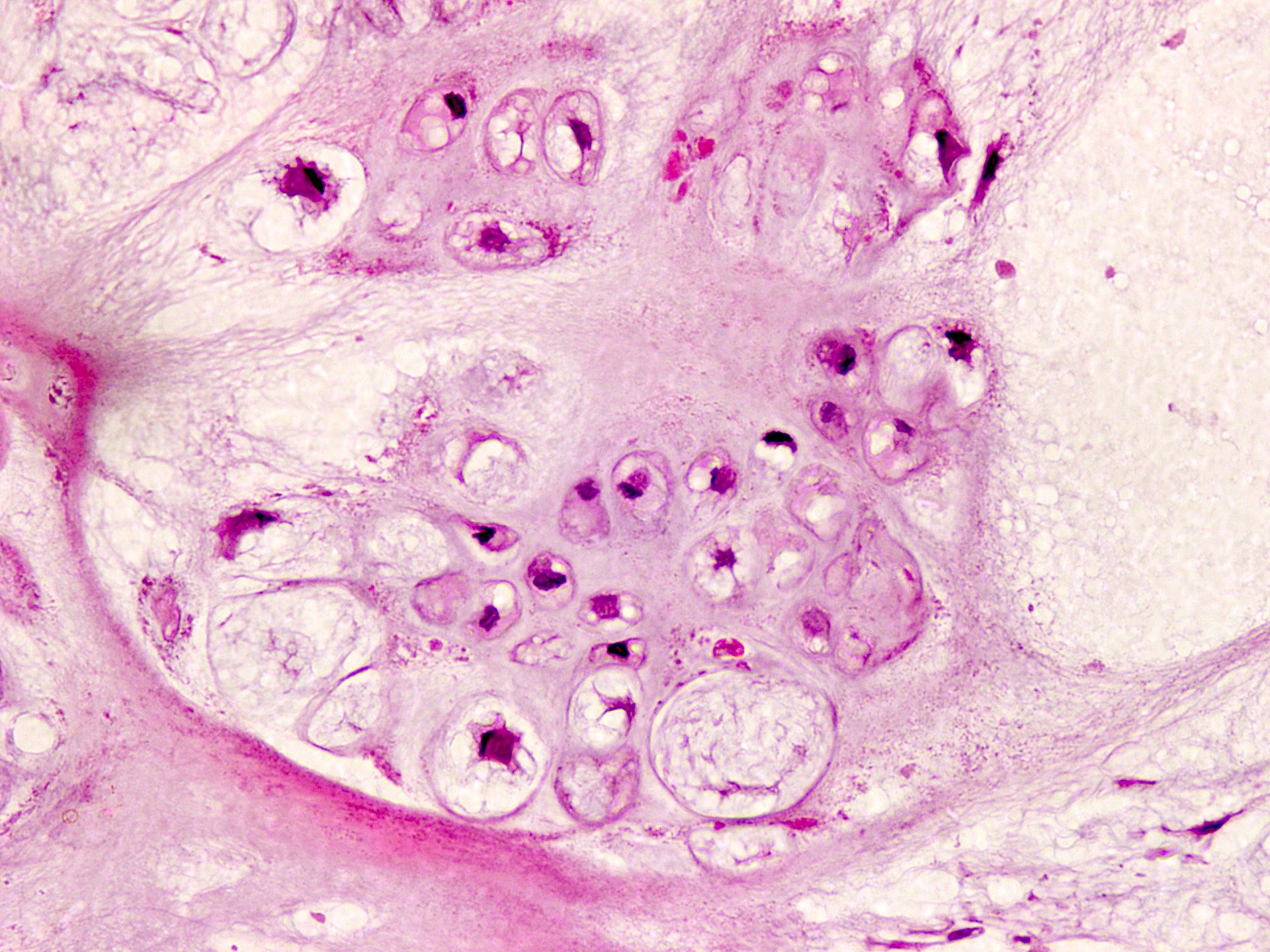
- Multiple hyaline cartilaginous nodules embedded in synovium or loose in joint spaces
- Clustering of chondrocytes
- Minimal atypia and increased cellularity
- Calcification or endochondral ossification may be seen in longstanding cases (JBJS Rev 2016;4:e2)
Microscopic (histologic) images
Cytology description
- Micronodular clusters of chondrocytes with no significant cytologic atypia
- Scant metachromatic chondroid matrix in background (Ann Diagn Pathol 2000;4:77)
Electron microscopy description
- Cells in hyaline cartilaginous nodules show ultrastructural features of typical mature chondrocytes with abundant rough endoplasmic reticulum, prominent golgi complexes and peripheral aggregates of glycogen (Arch Pathol Lab Med 1982;106:688)
Molecular / cytogenetics description
- FISH can be used to detect FN1::ACVR2A rearrangements
- IDH1 and IDH2 mutations are absent
Videos
Synovial chondromatosis:
5 minute pathology pearls
by Dr. Jerad Gardner
Sample pathology report
- Knee joint, incisional biopsy:
- Histological features are consistent with synovial chondromatosis (see comment)
- Comment: Light microscopy reveals multiple subsynovial mature hyaline cartilaginous nodules with no significant nuclear atypia, mitotic activity or infiltration of adjacent bone. Radiograph of knee joint shows multiple calcified densities with narrowing of joint spaces. Morphological and radiological features are characteristic of synovial chondromatosis. Synovial chondromatosis is a benign neoplasm but can be locally aggressive and can recur in 15 - 20% of patients with malignant transformation in 5 - 10% of cases. It can be primary (idiopathic) or secondary to degenerative joint diseases like osteoarthritis, rheumatoid arthritis or traumatic arthritis.
Differential diagnosis
- Degenerative joint disease (osteoarthritis):
- Radiology shows degenerative changes with narrowing of joint space
- Occurs in older age group
- Multiple osteochondral loose bodies with concentric layers of cartilage and orderly distribution of chondrocytes
- Soft tissue chondroma:
- No relation to synovium
- Most common location is fingers, followed by toes and feet
- Increased cellularity and cytologic atypia
- FN1 rearrangements can be seen but not with ACVR2A (Mod Pathol 2019;32:1762)
- Chondrosarcoma:
- Increased cellularity
- Loss of clustering pattern
- Increased or atypical mitoses
- Marked myxoid change
- Spindling of nuclei
- Permeative infiltration of adjacent bone
- Chondrocalcinosis (pseudogout):
- Distinct aggregates of basophilic to gray-brown material within tissues
- Surrounding chronic inflammation and histiocytic reaction
- Rhomboid to rod shaped crystals with positive birefringence under polarized light
- Osteochondroma:
- Arises from condylar head
- Cartilaginous cap present
- Osseous component contains fatty tissue or marrow elements
- Diffuse type tenosynovial giant cell tumor (pigmented villonodular synovitis):
- Not localized to a portion of joint
- More confluent masses
- Diffuse characteristic low intensity on MRI
- Neuropathic arthropathy or osteochondritis dissecans:
- Younger patients
- Associated with osteochondral fracture
- No lobulation, clustering or atypia
- Lipoma arborescens with osseous metaplasia:
- Fatty infiltration of subsynovial connective tissue
- Characteristic fat signal / density on radiology
- Tumoral calcinosis / hydroxyapatite deposition disease:
- Lobules of calcified material surrounded by histiocytic giant cells
- Elevated serum calcium, phosphate and vitamin D
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true regarding synovial chondromatosis?
- It is a metaplastic process rather than neoplastic
- It is twice as common in females than in males
- Knee is the most common site of involvement
- Most commonly occurs in adolescence
- There is a high risk of malignant potential
Board review style answer #2
C. Knee is the most common site of involvement
Comment Here
Reference: Synovial & tenosynovial chondromatosis
Comment Here
Reference: Synovial & tenosynovial chondromatosis
Board review style question #3
A 30 year old woman presented with pain and swelling of right ankle with palpable nodules. Radiographs revealed multiple radiopaque masses located on the anterior aspect of the ankle joint. Biopsy showed multiple nodules of mature hyaline cartilage within the synovium. Which of the following is an additional characteristic histological feature seen in synovial chondromatosis?
- Clustering of chondrocytes
- Concentric layering of chondrocytes
- Multinucleation of chondrocytes
- Myxoid degeneration
- Permeation of bone
Board review style answer #3