Table of Contents
Idiopathic cystic chondromalacia of auricular cartilage | Meniere disease | Necrotizing malignant external otitis | Otitis media | Otomycosis | Relapsing polychondritisCite this page: Pernick N. Infectious / inflammatory. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/earinfectiousinflam.html. Accessed April 2nd, 2025.
Idiopathic cystic chondromalacia of auricular cartilage
Definition / general
Case reports
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
Additional references
- Also called auricular or endochondral pseudocyst
- Benign cystic degeneration of auricular cartilage of unknown cause
- Usually men age 20 - 40 years
- Unilateral swelling of cartilage over weeks to years, most commonly on scaphoid fossa of auricle
- May be due to minor trauma
Case reports
- 32 year old man with auricular swelling (J Clin Pathol 1994;47:961)
Treatment
- Excision
Microscopic (histologic) description
- Fluid filled distended mass composed of cyst like wall with fibrous and granulation tissue lining but no epithelium
- Cyst contains 1 - 2 mm rim of cartilage
- Cyst fluid resembles olive oil
- No / mild atypia
Microscopic (histologic) images
Images hosted on other servers:
Differential diagnosis
- Chondrodermatitis nodularis helicis chronicus
- Relapsing polychondritis
- Subperichondrial hematoma
Additional references
Meniere disease
Definition / general
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Images hosted on other servers:
Additional references
- Also called endolymphatic hydrops
- Idiopathic disorder of inner ear associated with episodic attacks of vertigo, fluctuating sensorineural hearing loss, tinnitus and sensation of aural fullness
- Incidence varies from 7.5 per 100,000 in France to 157 per 100,000 in England
- 60% women, peaks in 40s to 60s but wide age range
- Rarely occurs in children (J Laryngol Otol 2006;120:343)
- Associated with HLA B8 / DR3
- May be due to accumulation of endolymph in membranous labyrinth, perhaps due to inadequate absorption by endolymphatic sac
Treatment
- Dietary modification, intermittent dehydration, diuretics, vasodilators in increase microcirculation of ear
- 60 - 80% improve
- Surgery includes shunting and decompression of endolymphatic sac, labyrinthectomy, sectioning of vestibular nerve (Laryngoscope 2005;115:1454)
Microscopic (histologic) description
- Initially involves cochlear duct and saccule
- Later entire endolymphatic system with dilation, rupture and collapse of membranous labyrinth with possible fistula
- May have severe atrophic changes with loss of cochlear neurons
Microscopic (histologic) images
Images hosted on other servers:
Additional references
Necrotizing malignant external otitis
Definition / general
Treatment
Case reports
Gross description
Microscopic (histologic) description
Positive stains
Differential diagnosis
Additional references
- Potentially fatal external otitis due to Pseudomonas aeruginosa (Ann Otolaryngol Chir Cervicofac 2000;117:291), Aspergillus or other fungal infection
- Usually older patients, often with diabetes, chronic debilitation or immunodeficiency; also undernourished African infants (Rev Laryngol Otol Rhinol 2002;123:225)
- Initially affects external auditory canal with symptoms of acute otitis externa; later pain, purulent otorrhea and swelling; may progress to cellulitis, chondritis, osteomyelitis, involve middle ear space or base of skull and cause cranial nerve palsies, meningitis, venous thrombosis or brain abscess (Rev Stomatol Chir Maxillofac 2006;107:167)
- Up to 75% mortality if treatment is delayed
- Due to tissue ischemia (from above primary pathologic state) plus neutrophilic migratory defect plus virulence of Pseudomonas
Treatment
- Antibiotics, surgical debridement, hyperbaric oxygen (HNO 2003;51:315)
Case reports
- Female patient with calcium oxalate crystal deposition in necrotizing otomycosis caused by Aspergillus niger (Mod Pathol 1993;6:493)
- Patient with necrotizing otitis externa caused by Stenotrophomonas maltophilia (Hautarzt 2003;54:1080)
- 47 year old man with necrotizing external otitis in a patient caused by Klebsiella pneumoniae (Eur Arch Otorhinolaryngol 2006;263:344)
- 58 year old man with necrotizing otitis externa caused byStaphylococcus epidermidis (Eur Arch Otorhinolaryngol 1999;256:439)
Gross description
- Ulcerated skin near osseous portion of external auditory canal, often with abundant necrotic and granulation tissue
Microscopic (histologic) description
- Epithelium is necrotic or ulcerated with pseudoepitheliomatous hyperplasia, marked mixed inflammatory infiltrate in subcutaneous tissue, necrotizing vasculitis
- Necrotic bone and cartilage with heavy inflammatory infiltrate in viable bone
- Variable sequestra of nonviable bone or cartilage
Positive stains
- Gram stain (Gram negative rods)
Differential diagnosis
Additional references
Otitis media
Definition / general
Treatment
Gross description
Microscopic (histologic) description
Differential diagnosis
Additional references
- Acute or chronic infectious disease of middle ear
- Usually childhood disease caused by Streptococcus pneumoniae or Haemophilus influenzae; also coinfection by viruses (Pediatr Infect Dis J 2004;23:1142, Clin Infect Dis 2006;43:1417)
- Rarely caused by fungi or pneumocystis in HIV+ patients
- Hyperemic, opaque and bulging tympanic membrane with limited mobility; may have purulent otorrhea
- Infection probably occurs post pharyngitis via eustachian tube
- Severe cases are associated with destruction of ossicles
- Tympanosclerosis: dystrophic calcification of tympanic membrane or middle ear associated with recurrent cases of otitis media, occurs in 3 - 33% of cases; may be reversible in children, usually irreversible in adults and associated with conductive hearing loss
Treatment
- Antibiotics or observation (Pediatr Infect Dis J 2006;25:1102, Lancet 2006;368:1429)
- Complications of mastoiditis, labyrinthitis, meningitis or abscess are now rare
Gross description
- Not a common specimen but may have small fragments of soft / rubbery granulation tissue
Microscopic (histologic) description
- Acute and chronic inflammatory cells, haphazard glandular metaplasia with cilia, fibrosis, hemorrhage, foci of calcification (tympanosclerosis), cholesterol granulomas and reactive bone formation (Laryngoscope 1982;92:273)
- Cholesterol granulomas: foreign body granulomas in response to cholesterol crystals from rupture of red blood cells and breakdown of lipid bilayer in cell membrane, prominent cholesterol clefts; associated with interference to drainage or ventilation of middle ear space; not related to cholesteatomas
Differential diagnosis
- Middle ear adenoma:
- Regular, not haphazard glands, no cilia
Additional references
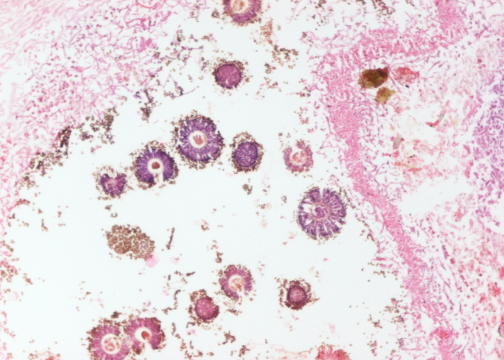
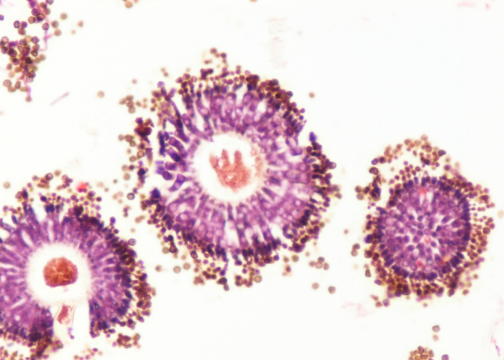
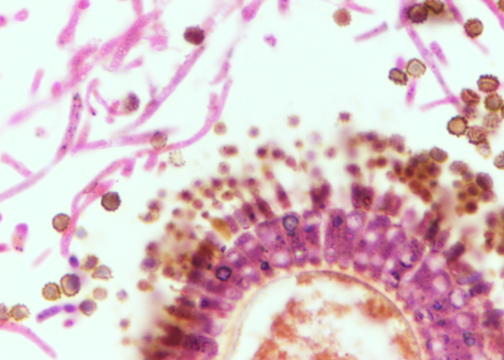
Otomycosis
Relapsing polychondritis
Definition / general
Laboratory
Treatment
Microscopic (histologic) description
Positive stains
Additional references
- Also called polychondropathia
- Uncommon systemic episodic or relapsing disease with progressive degeneration of cartilage throughout the body
- Probable autoimmune process (antibodies to type II collagen) associated with other autoimmune disorders
- Whites, no gender preference, usually symptomatic in 40s to 60s although affects all ages
- 90% have involvement of auricular cartilage, usually bilateral, with swelling, erythema and tenderness
- Earlobes are typically spared
- Variable relapsing of disease
- May cause cauliflower ear and saddle node deformities
- Clinical diagnosis requires 3 of the following
- Recurrent chondritis of both auricles
- Nonerosive inflammatory arthritis
- Chondritis of nasal cartilage
- Ocular inflammation including conjunctivitis, keratitis, scleritis, episcleritis or uveitis
- Chondritis of upper respiratory tract including larynx or tracheal cartilage
- Cochlear or vestibular damage with sensorineural hearing loss, tinnitus or vertigo
Laboratory
- Nonspecific elevated sedimentation rate, mild leukocytosis, normochromic normocytic anemia; variable elevated ANCA
- Prognosis varies from prolonged course to aggressive and fulminant disease leading to death from respiratory tract or cardiovascular involvement (aortic insufficiency)
Treatment
- Responds to steroids or dapsone (this also confirms diagnosis)
- Advanced cases require immunosuppressive agents
Microscopic (histologic) description
- Mixed inflammatory infiltrate (lymphocytes, plasma cells, neutrophils, occasional eosinophils) extending into cartilage with blurring of interface between cartilage and adjacent soft tissue
- Cartilage shows loss of normal basophilia, loss of chondrocytes and destruction of lacunar architecture at advancing edge of inflammation with cartilage replaced by fibrous tissue
Positive stains
- Granular deposition of IgG and C3 in perichondrial fibrous tissue (Hum Pathol 1980;11:19)
Additional references