Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology / etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Videos | Differential diagnosis | Additional referencesCite this page: Bychkov A. Branchial pouch / cleft anomalies. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidbranchial.html. Accessed April 1st, 2025.
Definition / general
- Congenital lesions due to incomplete obliteration of the branchial apparatus
- May be cyst, sinus, fistula or cartilage in anterolateral neck
- Cysts derived from branchial cleft have squamous epithelium; cysts derived from branchial pouch have respiratory epithelium, although repeated infections may cause squamous metaplasia (Ann R Coll Surg Engl 2007;89:W12)
Terminology
- A sinus is a blind ending tract
- "Branchial cleft sinus" connects to the skin, but a "branchial pouch sinus" connects to the pharynx; neither arises from the mesenchyme of the branchial arch (J Laryngol Otol 2004;118:19)
- A "true fistula" is a communication between two epithelialized surfaces; a "congenital branchial fistula" should be present at birth and should communicate between a persistent pouch and a cleft
- Most of the branchial fistulas are pseudofistulas, formed between a pouch remnant and a skin opening produced following an infection or a surgical incision or are just sinuses (AJNR Am J Neuroradiol 2010;31:755)
Epidemiology
- 20 - 40 years old, M = F
- 20% of cervical masses in children (Int J Pediatr Otorhinolaryngol 2011;75:1020)
- Cysts: fistulas = 10:1 (Eur J Inflamm 2012;10:39)
- 2% - 3% are bilateral (Ear Nose Throat J 2008;87:291)
Sites
- Sites of cysts:
- First branchial cleft: preauricular area (type I cyst) or below the angle of mandible (type II), may be connected to external auditory canal; cysts are rarely malignant (Diagn Cytopathol 2008;36:876); 5% - 8%
- Second branchial cleft: anterior to sternocleidomastoid muscle in midneck, may communicate with pharynx; 95% (Singapore Med J 2015;56:203)
- Third / fourth branchial cleft (Pyriform sinus fistula): 2% - 5%
- May be misdiagnosed as bronchogenic cyst
- Usually left sided and associated with neck infection, treatment is ipsilateral thyroidectomy as lesions pass through thyroid
Pathophysiology / etiology
- Branchial theory suggests that incomplete obliteration of branchial cleft mucosa, which remains dormant until stimulated to grow later in life, results in cyst formation (Ascherson, 1832) (Am J Pathol 1967;50:533)
- More theories: persistence of vestiges of the precervical sinus, thymopharyngeal duct origin and cystic lymph node origin (J Am Dent Assoc 2003;134:81)
Diagrams / tables
Clinical features
- Slow growing movable mass in the lateral neck, often asymptomatic
- Manifested as inflammatory neck mass or fistula
- Rarely associated with squamous cell carcinoma (J Laryngol Otol 1994;108:1068), but cystic neck masses should be considered to be nodal metastases until proven otherwise (common sites of small primary occult tumors are tonsil, posterior tonsillar pillar, retromolar tongue, nasopharynx)
- Clinical branchial cysts may rarely:
- Arise within thyroid gland (Korean J Radiol 2006;7:149)
- Actually be cystic remnants of ultimobranchial body
- Actually be papillary thyroid carcinoma (Kaohsiung J Med Sci 2007;23:634)
- Arise within ectopic thyroid tissue that transforms to papillary carcinoma (Ear Nose Throat J 2006;85:675, World J Surg Oncol 2006;4:24)
- 33% of patients with congenital third branchial arch anomalies and 45% with fourth branchial arch abnormalities present with acute infectious thyroiditis (Otolaryngol Head Neck Surg 2010;142:21, J Pediatr Surg 2009;44:1432)
Diagnosis
- Imaging and fluoroscopic fustulography to visualize cyst / fistula and anatomic tract
- Pyriform sinus examination via direct laryngoscopy to detect third / fourth branchial cleft anomaly
Radiology description
- Ultrasound: low echogenic lesion with lack of internal septation
- CT scan and MRI require sedation in children
Radiology images
Prognostic factors
- Recurrence rate depends on completeness of resection, mean 5% (Dentomaxillofac Radiol 2012;41:696)
Case reports
- 18 month old child with third branchial pouch cyst presenting as stridor (Ann R Coll Surg Engl 2007;89:W12)
- 9 year old boy and 42 year old man with fourth branchial complex anomaly (Case Rep Otolaryngol 2011;2011:958652)
- 10 year old girl with branchial cleft cyst at an unusual location (Dentomaxillofac Radiol 2012;41:696)
- 12 year old girl with type II first branchial cleft anomaly presenting as a post auricular salivary fistula (Ann Med Health Sci Res 2014;4:136)
- 22 year old woman with type I first branchial cleft cyst masquerading as a parotid tumor (Natl J Maxillofac Surg 2014;5:84)
- 32 year old woman with intrathyroidal branchial cleft cyst (Korean J Radiol 2006;7:149)
- 50 year old woman with branchial cleft cyst (J Oral Maxillofac Pathol 2014;18:150)
- Multiple branchial cleft-like cysts in Hashimoto thyroiditis (Am J Surg Pathol 1989;13:45)
Treatment
- Complete surgical excision of cyst and associated tract after clearing infection
- Endoscopic cauterization via pyriform sinus for fourth branchial cleft cysts
Clinical images
Images hosted on other servers:
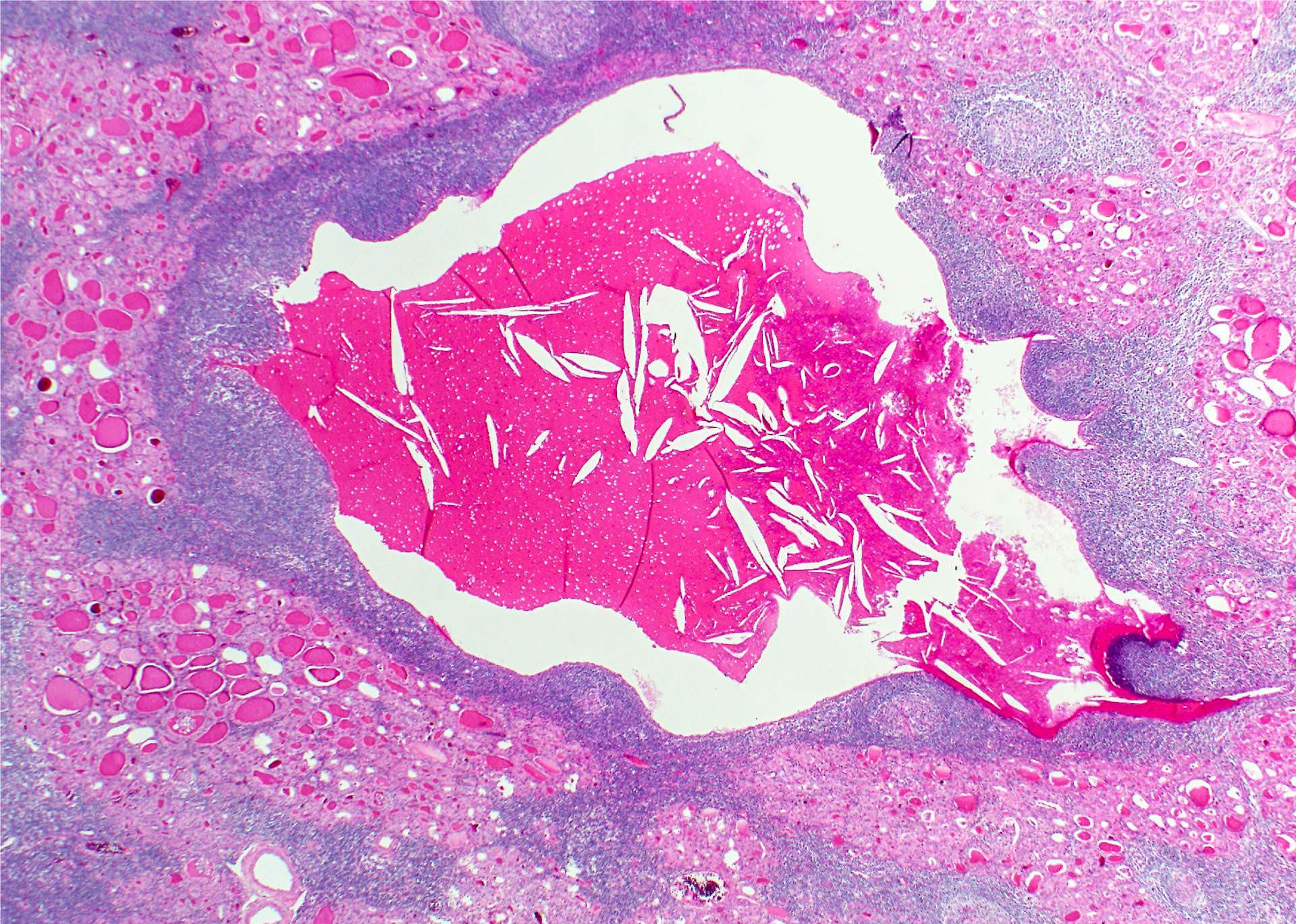
Gross description
- A smooth walled cyst with mucoid or watery contents, 2 - 6 cm in diameter (up to 10 cm in greatest dimension)
- Infected / ruptured cyst may be obscured or obliterated by the fibroinflammatory reaction; the surrounding soft tissues may be densely fibrotic
Gross images
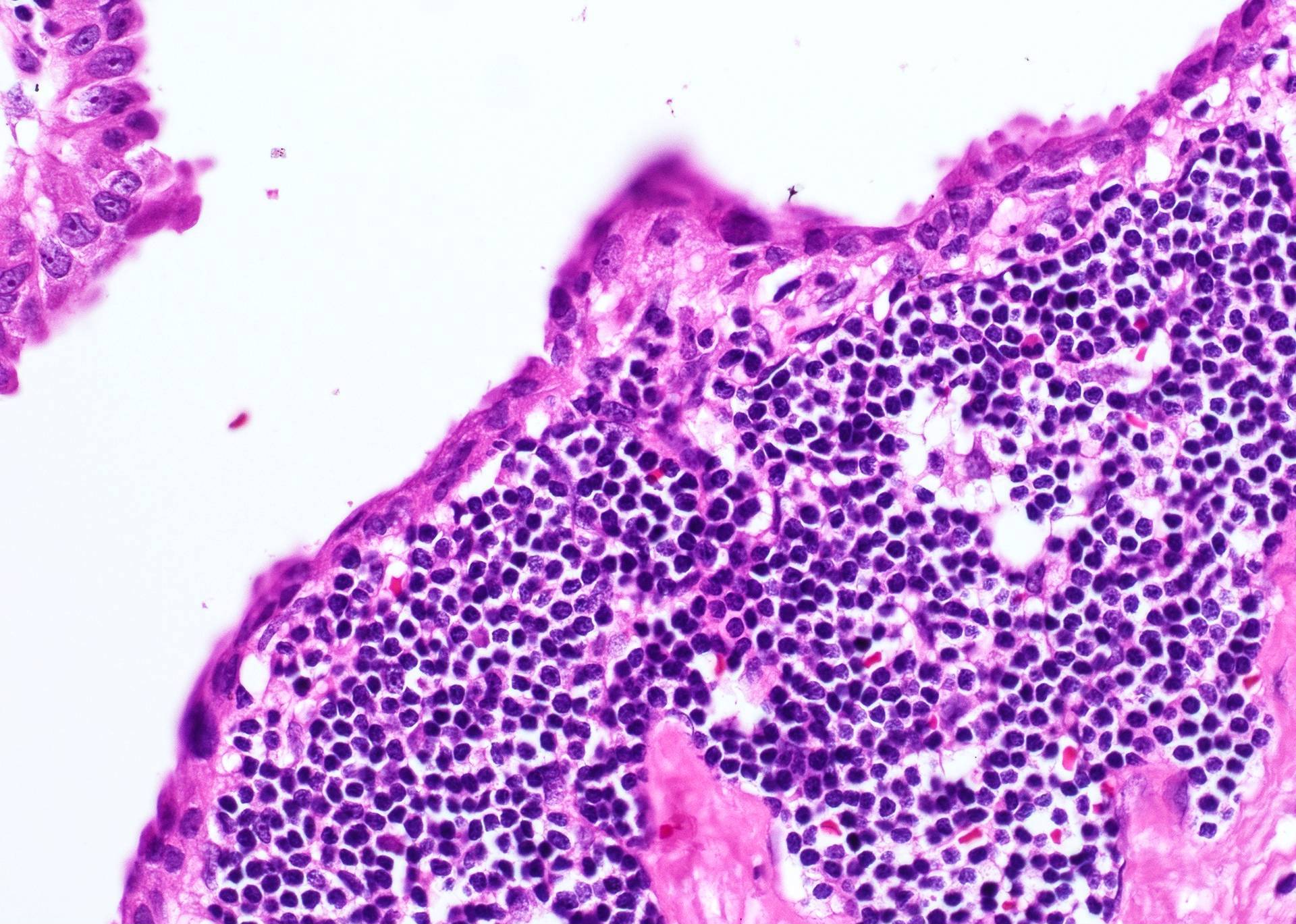
Microscopic (histologic) description
- Stratified squamous or ciliated columnar epithelium lining (Am J Pathol 1967;50:765, APMIS 1997;105:623)
- Fibrotic wall with lymphoid follicles resembling lymph node or tonsil
- May be secondarily infected
- Cysts may have sebaceous or mucinous glands
- Occasionally found in thyroid tissue as heterotopic cartilage, thymus or solid cell nests representing ultimobranchial body remnants
- Parathyroid glands, thymic tissue, tiny masses of cartilage and tiny glands lined by ciliated cells may be seen in normal thyroid glands, presumably related to anomalies of the development of the branchial pouches (J Anat 1976;122:77)
Microscopic (histologic) images
Contributed by Andrey Bychkov, M.D., Ph.D.
Images hosted on other servers:
Cytology description
- Squamous epithelial cells of variable maturity, abundant lymphocytes, macrophages, background of amorphous debris - these features are nonspecific (Acta Dermatovenerol Alp Pannonica Adriat 2006;15:85, Eurocytology)
- May be interpreted as suspicious for carcinoma (Cytopathology 2007;18:184)
Cytology images
Videos
Pharyngeal pouches
Differential diagnosis
- First branchial cleft cyst: epidermoid cyst, dermoid cyst, cystic sebaceous lymphadenoma
- Second branchial cleft cyst: lateral thyroglossal duct cyst
- Third branchial cleft cyst: papillary carcinoma with cystic change (positive for TTF1, thyroglobulin)
- Fourth branchial cleft cyst: thymic cyst
Additional references
- Gnepp: Diagnostic Surgical Pathology of the Head and Neck, 2nd ed, 2009, Barnes: Surgical Pathology of the Head and Neck, 3rd ed, 2008
- eMedicine - Branchial Cleft Cysts Imaging, Branchial anomalies - Powerpoint, Dr. Gleisner, University of Texas Medical Branch, Branchial Cleft Cysts, Powerpoint - Dr. Chaky, UNC Chapel Hill