Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Atiq A, Raza M, Ud Din N. Angiolymphoid hyperplasia with eosinophilia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesangiolymphoidhyperplasiawitheosinophili.html. Accessed April 2nd, 2025.
Definition / general
- Angiolymphoid hyperplasia with eosinophilia (ALHE) is a rare, benign vascular neoplasm characterized by proliferation of blood vessels along with inflammatory infiltrate rich in eosinophils
Essential features
- Nonmalignant vasoproliferative lesion
- Predominant epithelioid or histiocytoid endothelial cells
- Papules or nodules
- Mixed inflammatory infiltrate composed of lymphocytes, plasma cells and eosinophils
Terminology
- Angiolymphoid hyperplasia with eosinophilia
- Epithelioid hemangioma
- Obsolete terms
- Histiocytoid hemangioma
- Angiomatous nodule
- Pseudopyogenic granuloma
- Inflammatory angiomatous nodule
ICD coding
- ICD-10: L98.8 - other specified disorders of the skin and subcutaneous tissue
Epidemiology
- Most common in middle aged adults
- Slight female preponderance
- More frequent in Asian populations, particularly in individuals of Japanese and Chinese descent (J Am Acad Dermatol 2016;74:506)
Sites
- Most common sites are skin and subcutaneous tissue of head and neck, particularly the face, scalp and ear lobes (Int J Surg Pathol 2016;24:59)
- Less common sites are limbs, oral mucosa and genitalia
Pathophysiology
- Pathophysiology of ALHE is likely multifactorial, involving a complex interplay of angiogenesis, immune dysregulation and possibly genetic and environmental factors (Dermatol Pract Concept 2018;8:28)
- Initial inflammatory event or injury to the blood vessels triggers a cascade of events leading to the proliferation of blood vessels known as angiogenesis
- Eosinophils are known to have a role in allergic and inflammatory response
- Presence of eosinophils is very much suggestive of a dysregulated immune response
- Inflammatory mediators released by eosinophils may be a contributing factor to the vascular changes seen in ALHE
- Other possible contributing factors are
- Arteriovenous shunting
- Local trauma
- Elevated serum estrogen levels
Etiology
- Idiopathic condition
- Theories include vascular abnormalities, immunologic factors, inflammatory response, infectious agents, genetic factors, hormonal factors (Open Access Maced J Med Sci 2017;5:423)
Clinical features
- Slow growing cutaneous lesions
- Can be single or multiple
- Firm, red to violaceous (purple) nodules or papules (J Am Acad Dermatol 2016;75:e19)
- Size ranges from a few millimeters to centimeters
- Sometimes can be pruritic and occasionally ulcerate (Dermatol Pract Concept 2021;11:e2021003)
- Rarely associated with tenderness / pain
- Some patients may experience regional lymphadenopathy near the affected area
- Systemic involvement is rare
- Can be clinically mistaken for hemangioma or other vascular lesions
- Peripheral eosinophilia has been reported in few cases (Indian J Dermatol 2020;65:556)
Diagnosis
- Definite diagnosis requires a biopsy and histopathological examination
- Imaging modalities can help distinguish ALHE from other vascular or soft tissue lesions (J Am Acad Dermatol 2016;74:506)
- Additional diagnostic tests can be performed to rule out the other causes of eosinophilia, if clinically indicated (J Am Acad Dermatol 2016;74:506)
Laboratory
- Eosinophilia and elevated IgE levels may be present in patients with ALHE (Indian J Dermatol 2020;65:556)
Radiology description
- Radiology is typically not required
- Ultrasound shows isoechoic or hypoechoic masses with increased blood flow (Open Access Maced J Med Sci 2017;5:423)
Prognostic factors
- Benign localized disease with indolent course
- Does not regress without intervention
- Recurrence is a common feature; can appear at the same site or in different locations (Indian Dermatol Online J 2017;8:267)
Case reports
- 13 year old Caucasian girl with bilateral, huge, protruding and yellowish nostril masses (J Med Case Rep 2018;12:89)
- 21 year old woman presented with multiple erythematous to skin colored, dome shaped, firm papules and plaques (BMJ Case Rep 2018;2018:bcr2017223447)
- 28 year old woman presented with multiple, well delimited, infracentimetric erythematous papules with a smooth surface on the left frontal, temporal and preauricular regions (Acta Dermatovenerol Croat 2019;27:40)
- 37 year old Filipino man with lesions located on the central face (J Clin Aesthet Dermatol 2021;14:49)
- 48 year old woman presented with a painful subungual nodule of the left first fingernail (Dermatol Online J 2017;23:13030)
Treatment
- Total surgical excision is the current treatment of choice
- Other treatment options include laser therapy and corticosteroid injections (J Am Acad Dermatol 2013;68:e48)
Clinical images
Gross description
- Single or multiple, dome shaped, light pink to red brown papules or subcutaneous masses with no specific distinguishing surface features (J Am Acad Dermatol 2016;74:506)
- Size may range from few millimeters to a centimeter
- There might be erosion or crust formation of the surface (J Am Acad Dermatol 2016;74:506)
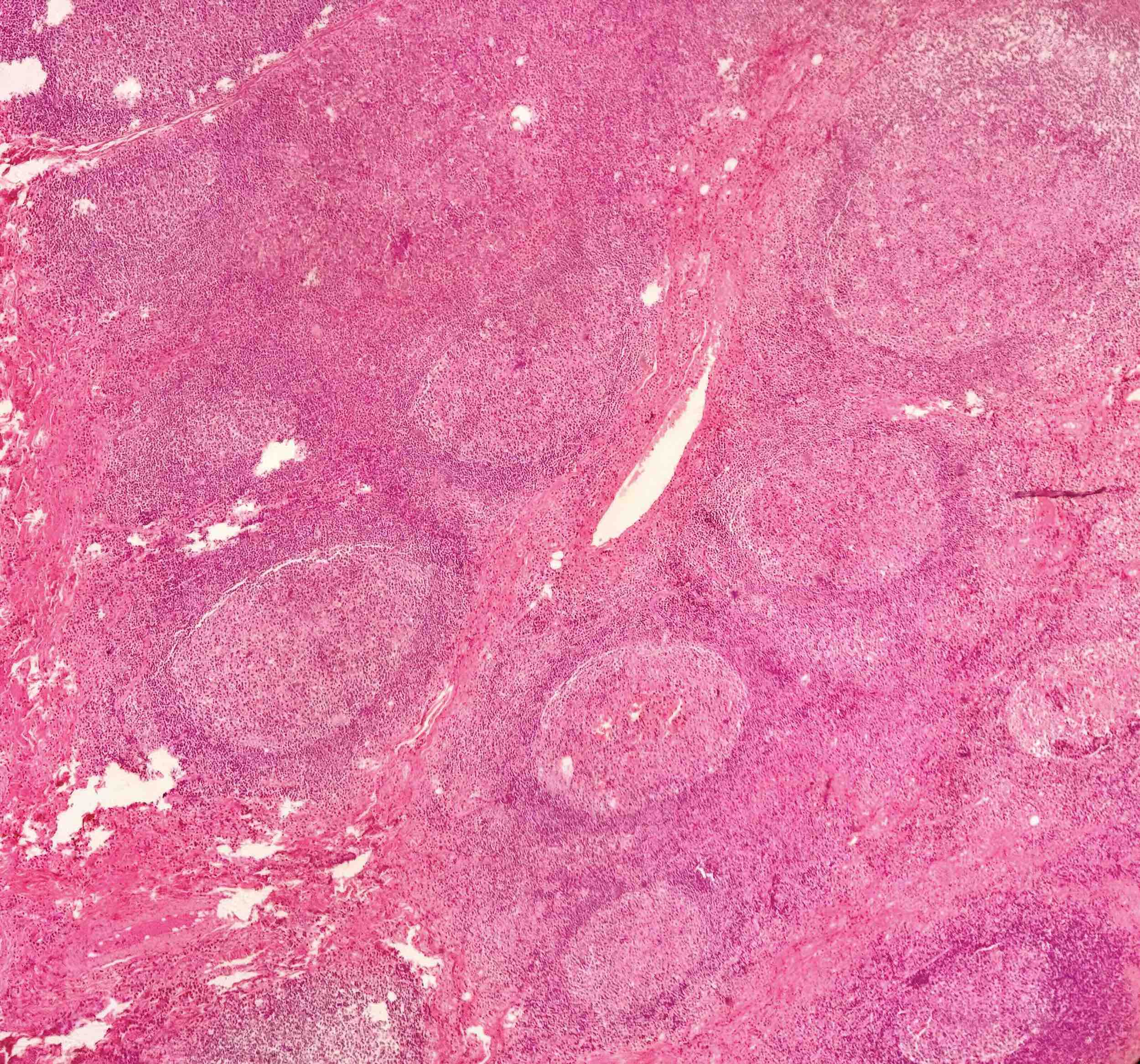
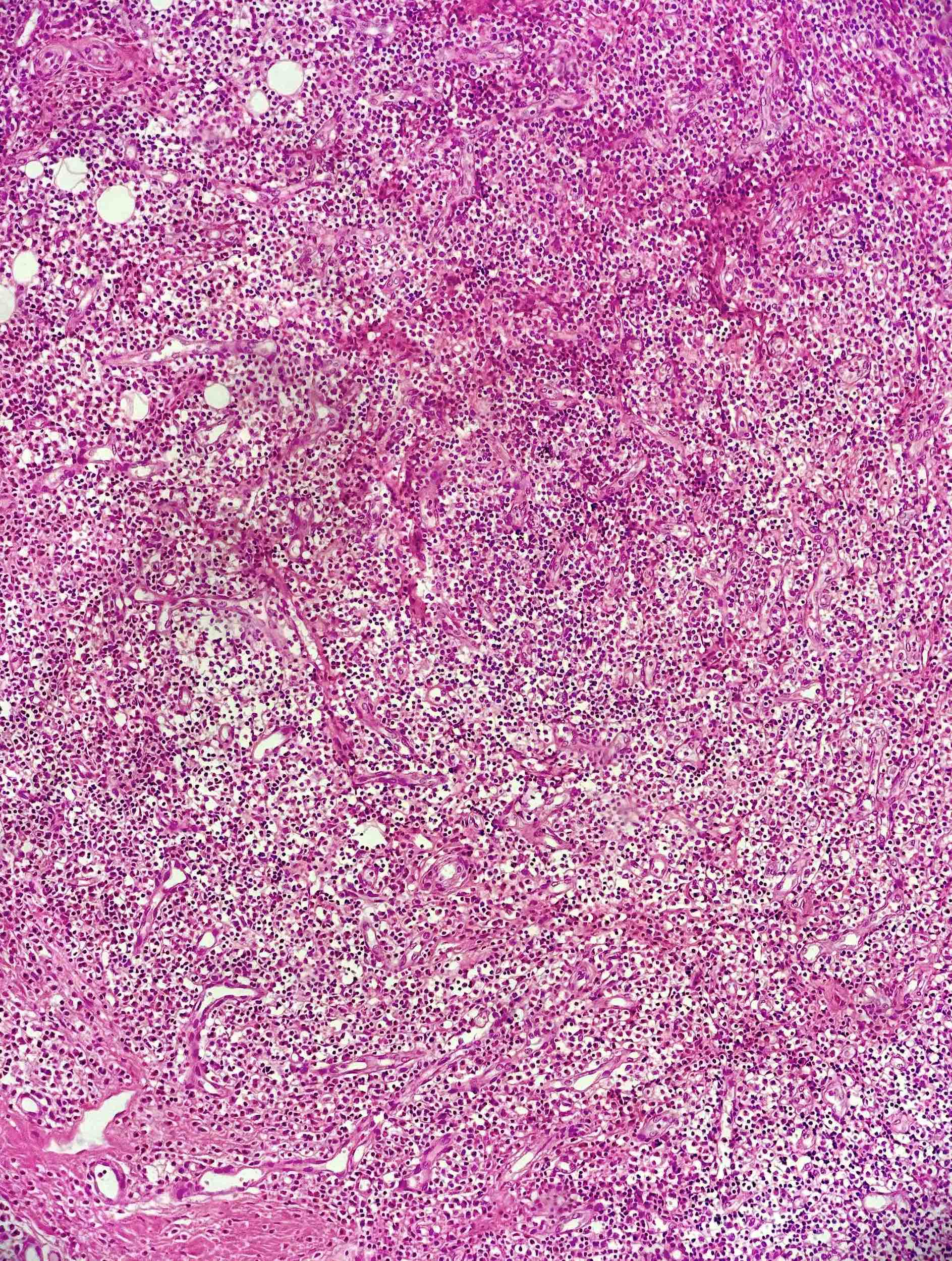
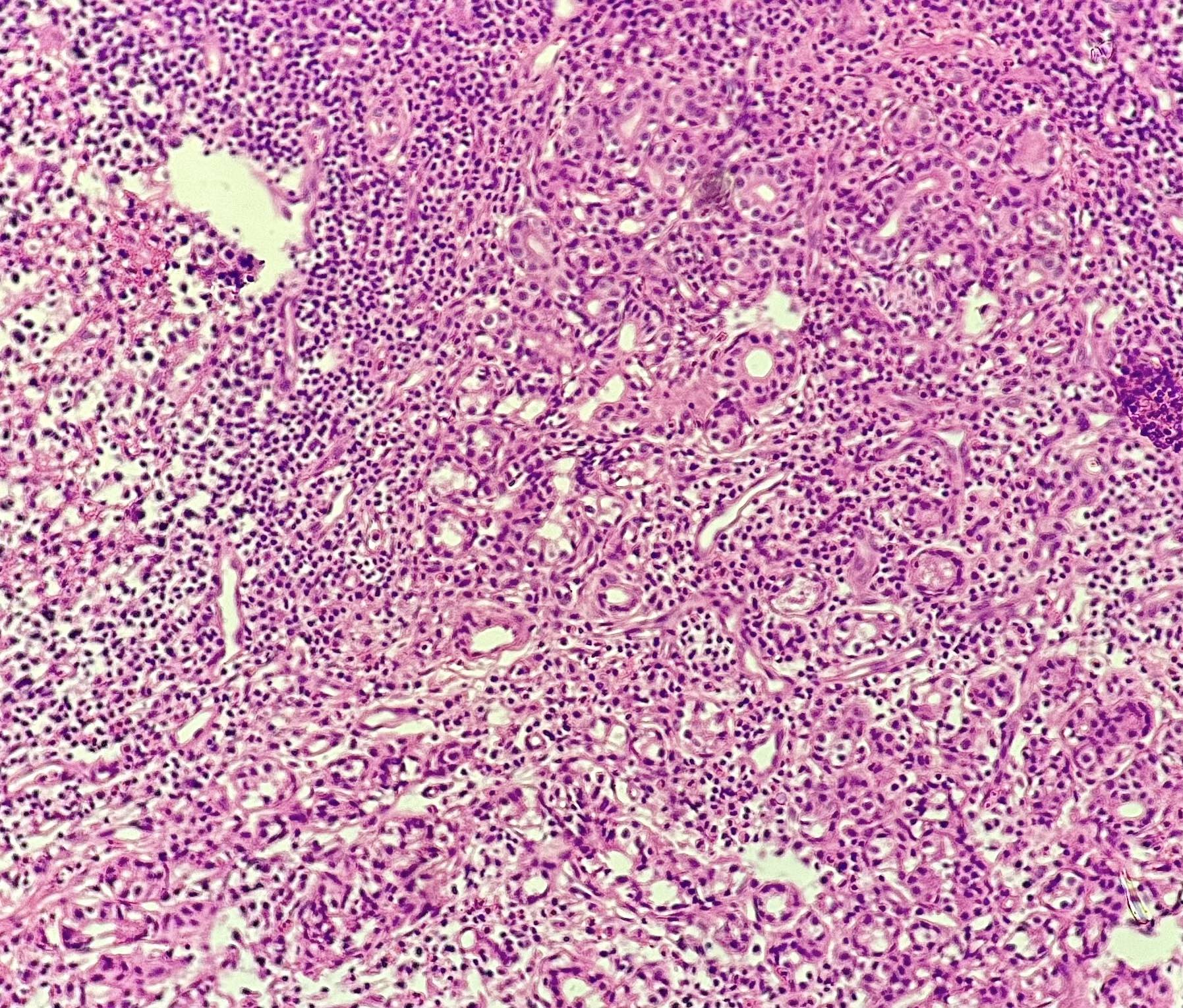
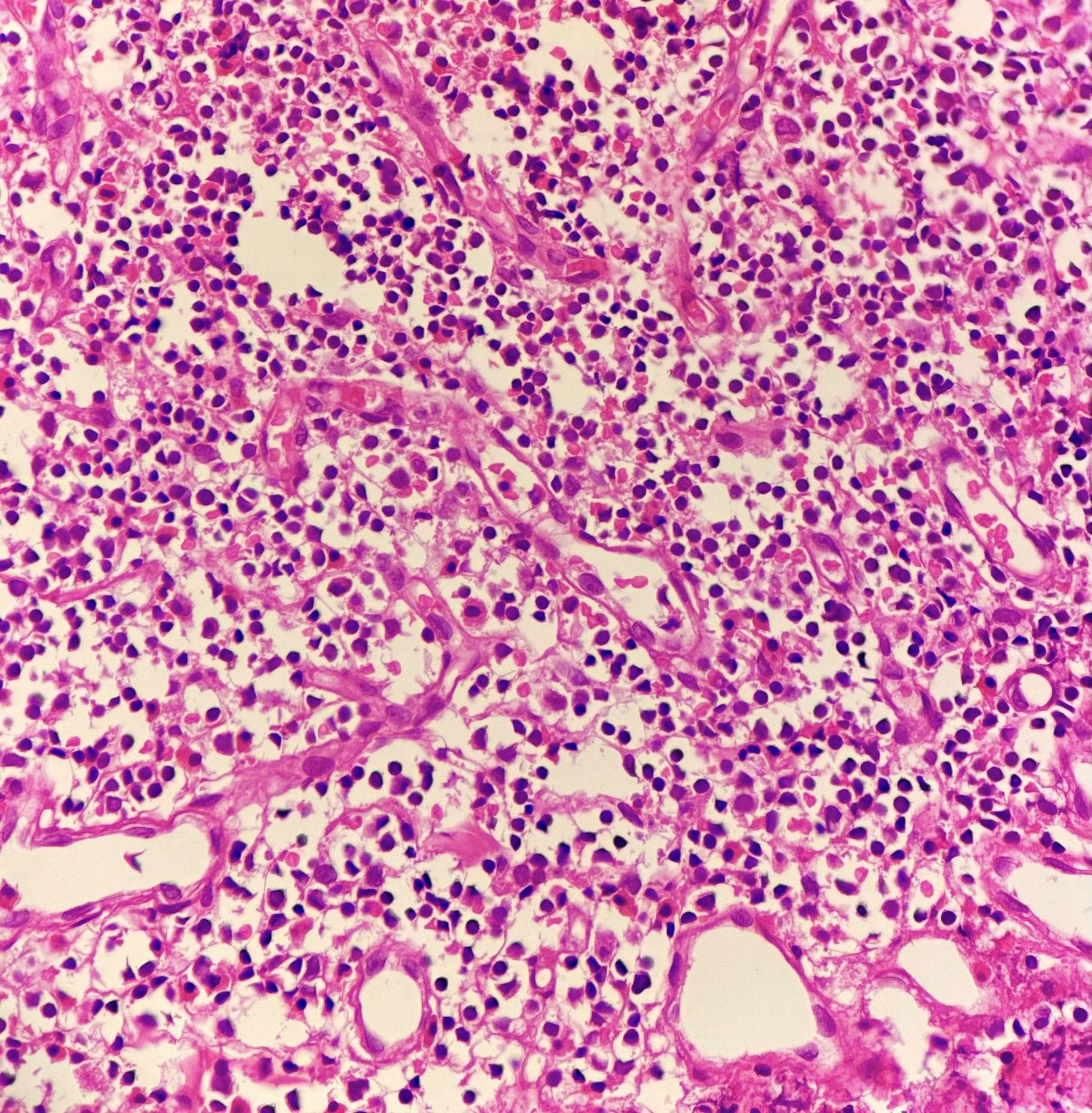
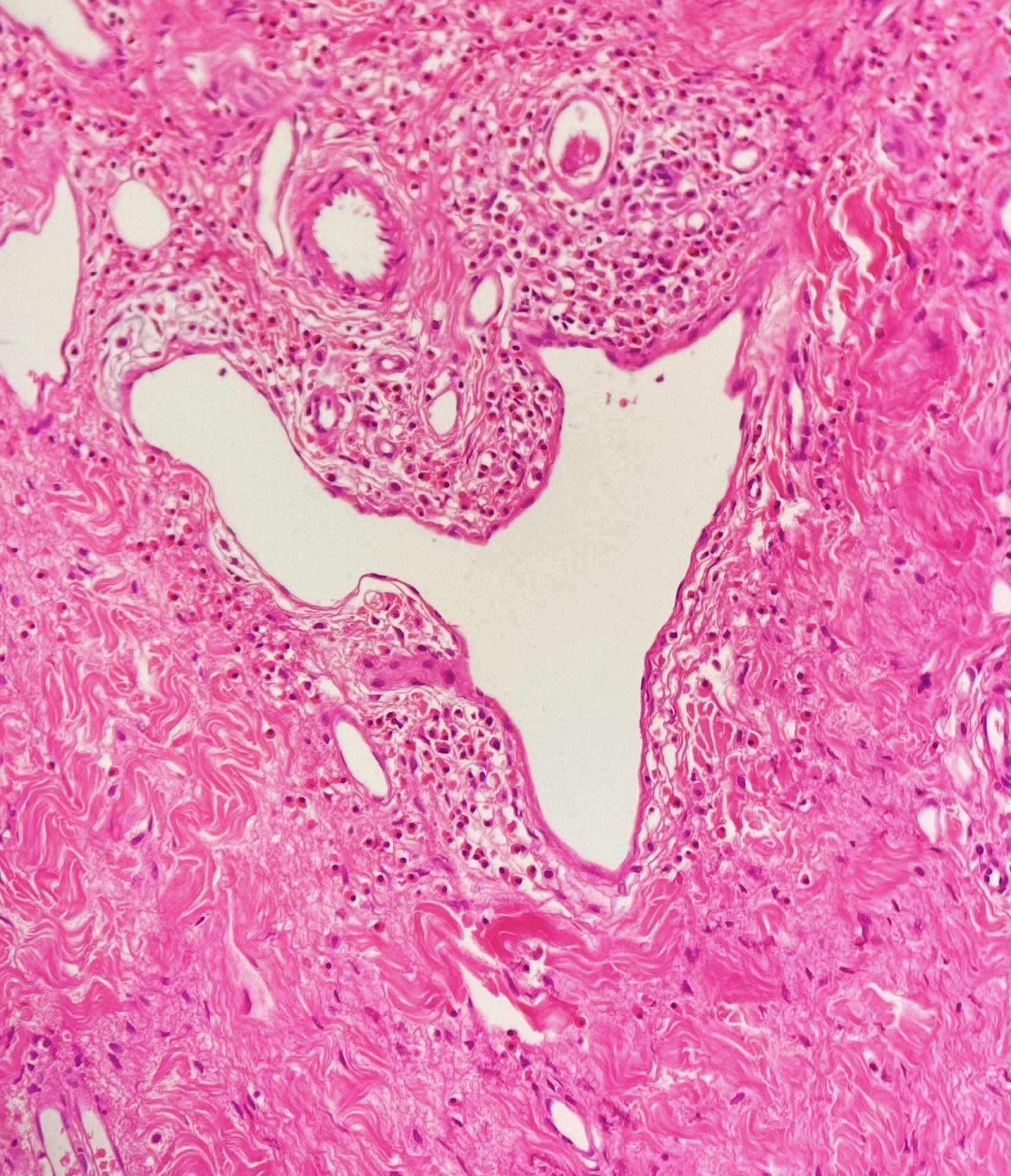
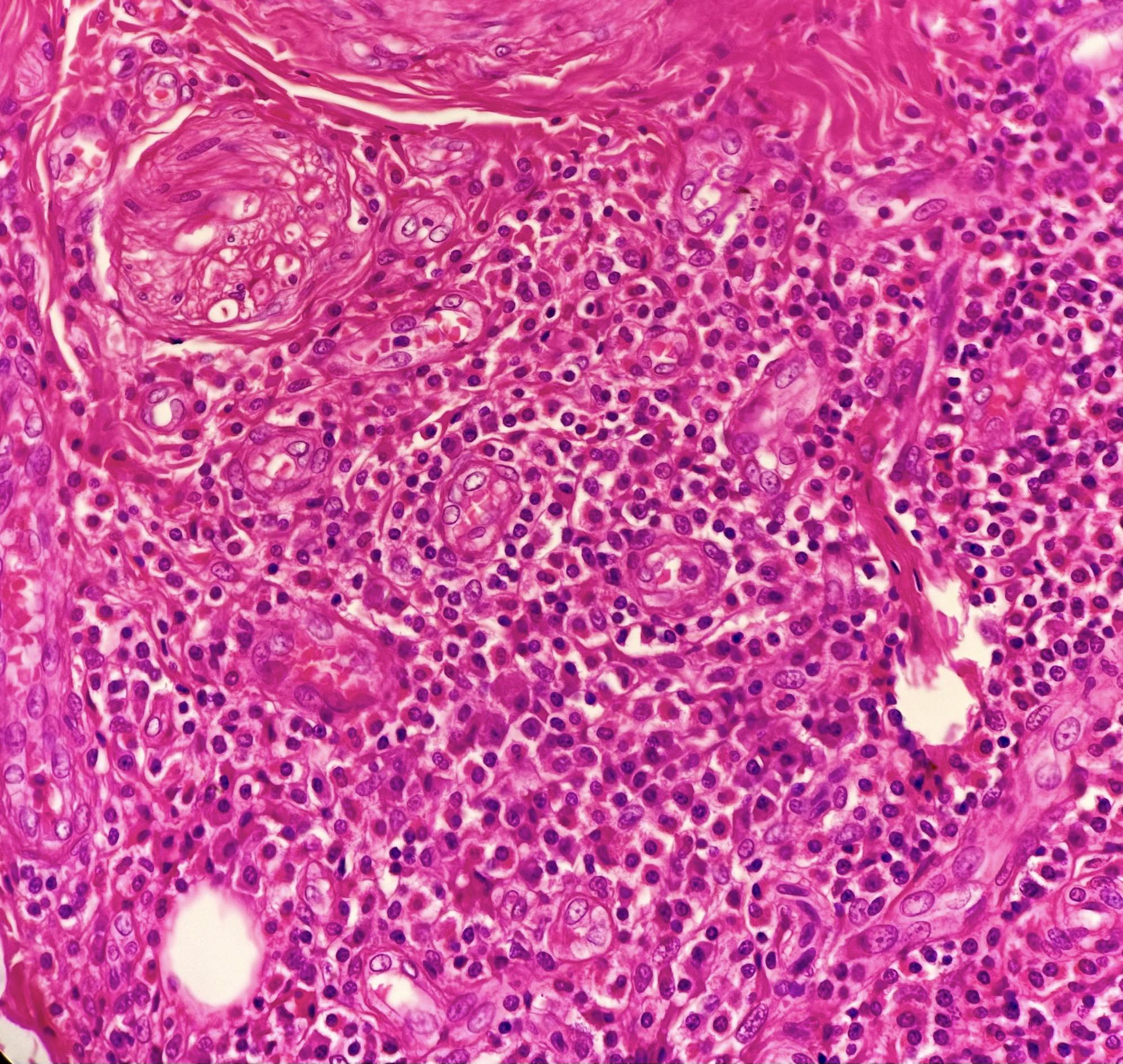
Microscopic (histologic) description
- Dermal based lesion with extension into the subcutaneous tissue
- Proliferation of vascular channels as nests and cords of endothelial cell proliferations with admixed lymphocytes, plasma cells and eosinophils, accompanied by hemorrhage and proliferation of thick and thin walled blood vessels (Dermatol Pract Concept 2018;8:28)
- Endothelial cells show large vesicular nuclei with acidophilic and sometimes vacuolated cytoplasm, imparting a hobnail appearance (Clin Colorectal Cancer 2010;9:179)
- Mitoses can be seen but lack atypical features and anaplasia
- Eosinophilia is usually a striking feature
- Stroma may show varying degrees of fibrosis, which can be a contributing factor to the firmness observed clinically (StatPearls: Angiolymphoid Hyperplasia With Eosinophilia [Accessed 19 January 2024])
Microscopic (histologic) images
Cytology description
- Plump polygonal endothelial cells with vesicular nuclei and deeply eosinophilic cytoplasm (Diagn Cytopathol 2021;49:E7)
- Background shows eosinophils and lymphocytes
Positive stains
- CD31: strong staining in endothelial cells
- CD34: lesser reactivity as compared to CD31 (Am J Surg Pathol 2004;28:523)
- Factor VIII related antigen: weak positive but not as specific as CD31 (Am J Surg Pathol 2004;28:523)
- FOSB: strong nuclear expression in endothelial cell (J Cutan Pathol 2018;45:395)
Negative stains
Electron microscopy description
- Electron microscopy of ALHE reveals features that support the endothelial origin (Ann Pathol 1985;5:271)
Molecular / cytogenetics description
- Molecular basis of ALHE is limited and further studies are needed to be done to understand the underlying genetic and molecular alterations driving this condition
Videos
Angiolymphoid hyperplasia with eosinophilia
Sample pathology report
- Right cheek, excision:
- Angiolymphoid hyperplasia with eosinophilia (see comment)
- Comment: Histologic sections consist of skin with a dermal based lesion composed of proliferation of vascular channels accompanied by inflammatory infiltrate. Endothelial cells are showing epithelioid morphology with hobnail nuclei. The inflammatory infiltrate is composed of lymphocytes, plasma cells and eosinophils. The lesion appears to be completely excised and excision is curative.
Differential diagnosis
- Kimura disease (An Bras Dermatol 2017;92:392):
- More common in young Asians
- Age range: second to sixth decades
- Most have lymph node involvement
- Peripheral eosinophilia is usually present
- Vascular proliferation is less notable than in ALHE, lacks plump endothelial cells
- Angiosarcoma (Arch Pathol Lab Med 2015;139:683):
- Occurs in older age group
- Cutaneous involvement is rare
- Irregular vascular channels and fascicular arrangement
- Mitotic activity, pleomorphism and nuclear hyperchromasia
- Epithelioid hemangioendothelioma (Diagn Pathol 2014;9:131):
- Wide age range
- Any location
- Strands, cords and nests of vacuolated endothelial cells separated by myxohyaline stroma
- WWTR1::CAMTA1
- Kaposi sarcoma (Cutis 2013;92:110):
- Skin is the most common location
- Spindle cell proliferation with slit-like vascular spaces
- Stain positively with HHV8
- Pyogenic granuloma (Cutis 2013;92:110):
- Very common
- Rapidly growing polypoid red mass
- Capillary sized vessels separated by fibromyxoid stroma, not seen in ALHE
Additional references
Board review style question #1
A 35 year old man presented with skin lesions and was diagnosed with angiolymphoid hyperplasia with eosinophilia (ALHE) on biopsy. Which of the following is true about ALHE?
- Common in head and neck area
- HHV8 is usually positive
- Inflammatory infiltrate in the lesion is composed of eosinophils only
- Presence of mitosis is suggestive of malignancy
- Shows strong positivity with all vascular markers
Board review style answer #1
A. Common in head and neck area. ALHE is most common in head and neck area. Answer B is incorrect because HHV8 is negative in almost all cases. Answer C is incorrect because the inflammatory infiltrate in the lesion is usually a mixture of lymphocytes, plasma cells and eosinophils. Answer D is incorrect because ALHE can show occasional mitosis but lacks anaplasia, so presence of mitosis does not warrant a diagnosis of malignancy. Answer E is incorrect because ALHE can show stronger staining with CD31 as compared to other vascular markers.
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia
Board review style question #2
Board review style answer #2
A. Angiolymphoid hyperplasia with eosinophilia. Proliferating blood vessels with histiocytoid-like endothelial cells is a feature of angiolymphoid hyperplasia with eosinophilia. Answer B is incorrect because cells in angiosarcoma show marked atypia. Answer C is incorrect because bacillary angiomatosis shows proliferation of small blood vessels and is characterized by the presence of small bacilli. Answer D is incorrect because glomeruloid hemangioma is a hemangioma with glomeruloid structures associated with POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein, skin changes). Answer E is incorrect because Masson tumor is an intraluminal papillary growth due to an organized thrombus.
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia
Comment Here
Reference: Angiolymphoid hyperplasia with eosinophilia