Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Kamal M, Hassell LA. Juvenile (retention) polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorjuvenilepolyp.html. Accessed April 2nd, 2025.
Definition / general
- Most common type of pediatric intestinal polyp, with prominent, cystically dilated glands and inflammatory stroma (> 90% of childhood colon polyps) (Clin Colon Rectal Surg 2008;21:280)
- Juvenile refers to the type of polyp (hamartomatous), not the age of presentation
- Majority are solitary (Gastroenterol Hepatol (N Y) 2010;6:185); solitary juvenile polyps have minimal malignant potential (Clin Pediatr (Phila) 2011;50:910); multiple juvenile polyps may indicate a premalignant condition (juvenile polyposis coli or juvenile polyposis syndrome [JPS]) (Clin Gastroenterol Hepatol 2010;8:795)
Essential features
- Most common type of pediatric intestinal polyp, with prominent, cystically dilated glands and inflammatory stroma
- Solitary juvenile polyps have minimal malignant potential; multiple juvenile polyps may indicate a premalignant condition (juvenile polyposis coli or juvenile polyposis syndrome [JPS])
- Juvenile polyposis syndrome is autosomal dominant and caused by a germline defect in SMAD4 or BMPR1A
Terminology
- Retention polyps and juvenile hamartomatous polyps (Can J Gastroenterol 2007;21:233)
- Juvenile polyposis syndrome (WHO 5th edition):
- > 3 - 5 juvenile polyps in the colorectum or
- Juvenile polyps throughout the gastrointestinal tract or
- Any number of juvenile polyps with a positive family history of juvenile polyposis (World J Gastroenterol 2011;17:4839)
- Other syndromes involving hamartomatous gastrointestinal polyps should be ruled out clinically or by pathological examination
Epidemiology
- Age: 3 to 10 years; sporadic polyps are uncommon before 2 years of age and rare in the first year of life (Clin Colon Rectal Surg 2008;21:280)
- M:F = 1.4:1 (Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1995;36:197)
Sites
- Majority in distal colon / rectosigmoid
- Less frequently seen in stomach and small bowel
Pathophysiology
- Earliest morphologic lesions are focal areas of mucosal hyperplasia, which seem to evolve into minute hyperplastic polyps
- These become inflamed, frequently with ulceration and scarring of their surface, sealing over some of the crypts, with subsequent cystic dilatation of the crypts, accumulation of mucus within the cysts, enlargement of the structure to form a typical juvenile polyp and further inflammation and scarring
- In some of the larger polyps, focal epithelial atypia develops
- Second hypothesis: landscape defect, in which an abnormal stromal environment leads to neoplastic transformation of adjacent epithelium (World J Gastroenterol 2011;17:4839)
- Juvenile polyposis syndrome is caused by a germline defect in SMAD4 or BMPR1A (Am J Surg Pathol 2011;35:530)
Etiology
- Juvenile polyposis syndrome is autosomal dominant
Clinical features
- Most frequent presentation: painless hematochezia
- Others: hematochezia with pain, abdominal pain, chronic iron deficiency anemia, intussusceptions and prolapsing rectal mass (J Pediatr Gastroenterol Nutr 2019;69:668, J Pediatr Gastroenterol Nutr 2020;71:491, Case Rep Surg 2014;2014:856765, Cureus 2020;12:e11222)
- Sessile or pedunculated polyp on endoscopy
Diagnosis
- Colonoscopy is the modality of choice (J Pediatr Gastroenterol Nutr 2019;69:668)
- Capsule endoscopy (Clin Gastroenterol Hepatol 2020;18:e73)
- Genetic testing and screening colonoscopies if suspicion of juvenile polyposis syndrome (J Pediatr Gastroenterol Nutr 2020;71:491)
Radiology description
- Filling defect on barium enema
- Rounded hypoechoic nodule within the lumen of gastrointestinal tract with a peripheral hyperechoic layer (Ital J Pediatr 2020;46:66)
Prognostic factors
- Extremely low risk of malignant transformation unless syndromic (J Pediatr Gastroenterol Nutr 2019;69:668)
- Recurrence is common in juvenile polyps; occurs with both multiple and solitary polyps (Clin Gastroenterol Hepatol 2010;8:795)
Case reports
- 3 year old girl with juvenile polyp in small intestine presenting with chronic iron deficiency anemia (J Pediatr Gastroenterol Nutr 2020;71:491)
- 10 year old boy with rectal prolapse and lower abdominal pain (Cureus 2020;12:e11222)
- 14 year old boy with osseous metaplasia in a juvenile polyp presenting with bleeding per rectum (J Clin Diagn Res 2013;7:2004)
- 37 year old man with a solitary colorectal juvenile polyp identified during followup of ulcerative colitis (World J Gastroenterol 2020;26:877)
- 46 year old man presented with a 6 week history of loose stools and hematochezia (BMJ Case Rep 2018;2018:bcr2018224770)
Treatment
- Many of these polyps outgrow their blood supply, become ischemic and autoamputate
- For solitary juvenile polyp:
- Colonoscopy / sigmoidoscopy and polypectomy
- No further evaluation or followup is needed after polypectomy
- Adenomatous changes in a juvenile polyp: followup and screening endoscopy is recommended (Clin Colon Rectal Surg 2008;21:280)
- For juvenile polyposis syndrome:
- High suspicion of JPS: endoscopic screening of the colon and upper gastrointestinal tract at age 15 or at the time of first symptoms
- Followup: recommended every 2 to 3 years in patients with juvenile polyposis syndrome
- Surgery: considered in patients with colorectal polyposis unmanageable by endoscopy (> 50 - 100 polyps), those with severe gastrointestinal bleeding or diarrhea, juvenile polyps with dysplasia and patients with a strong family history of colorectal cancer (World J Gastroenterol 2011;17:4839)
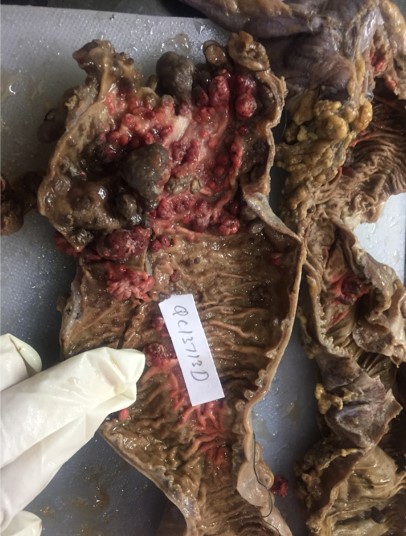
Gross description
- Sessile or pedunculated hamartomatous polyps
- 5 mm to 50 mm, typically spherical, lobulated and pedunculated with surface erosion
- Reference: World J Gastroenterol 2011;17:4839
Gross images
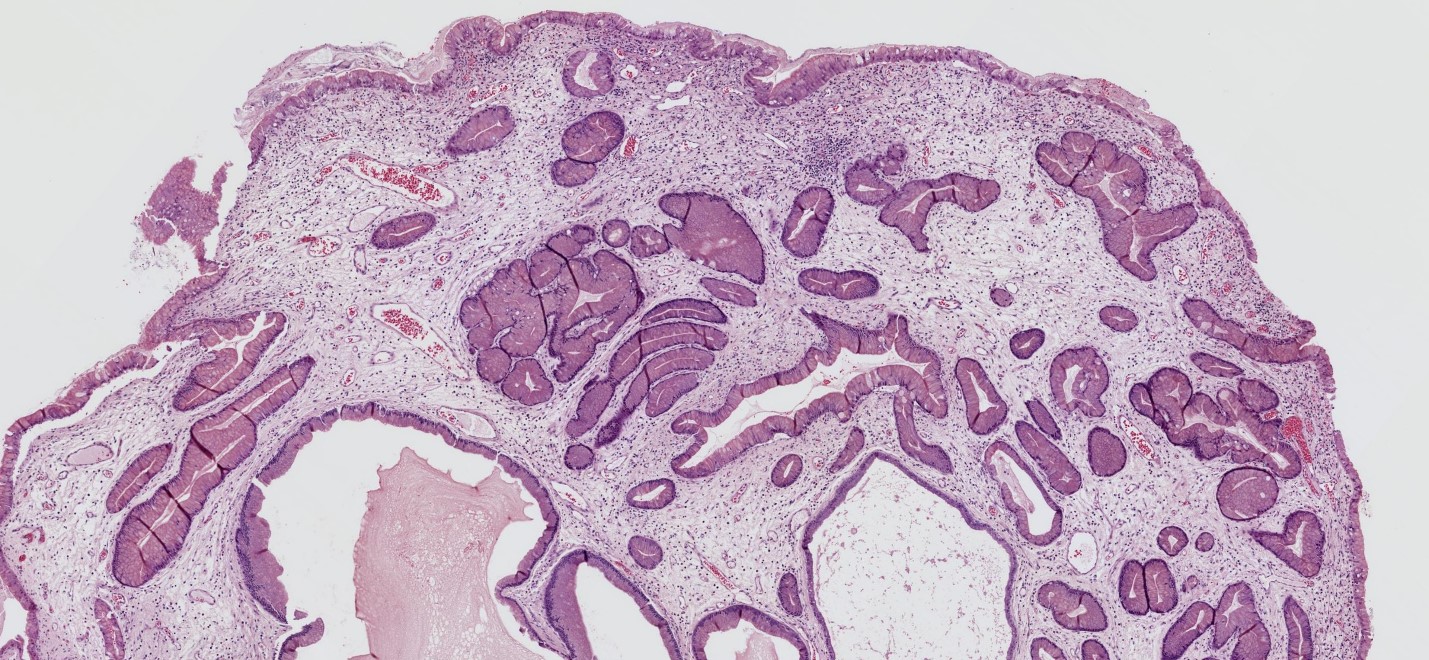
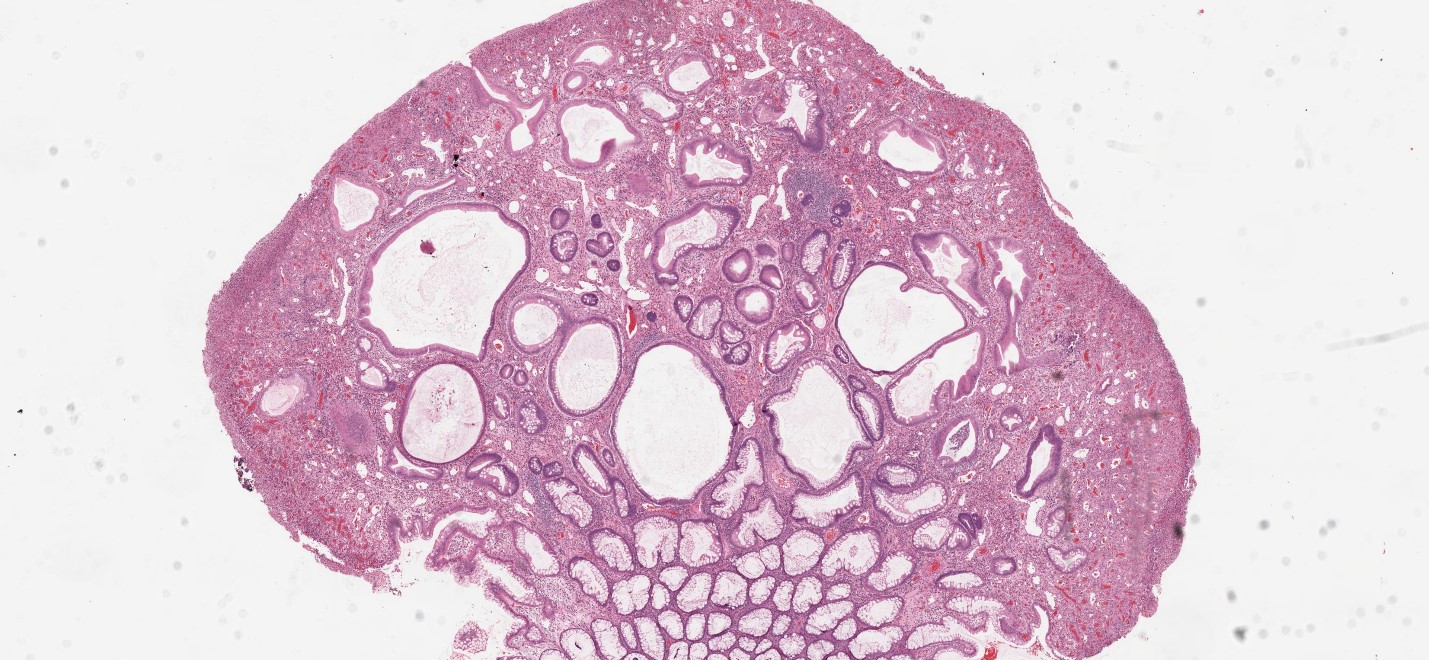
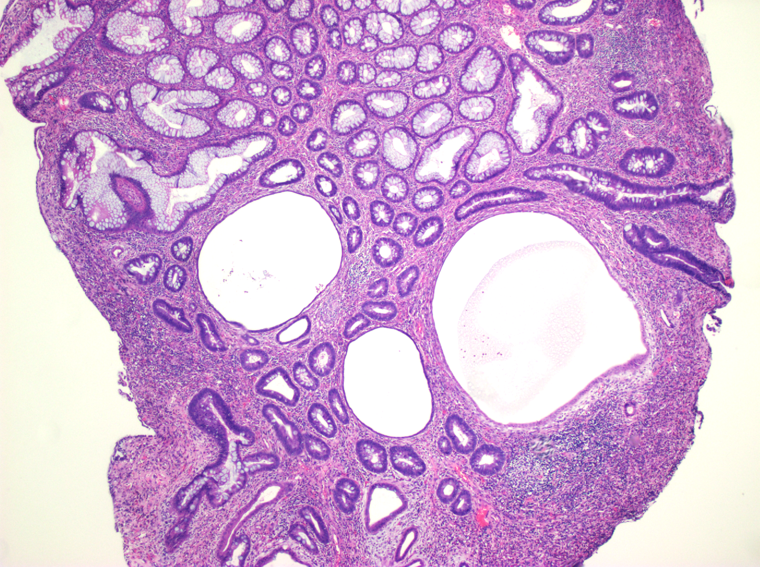
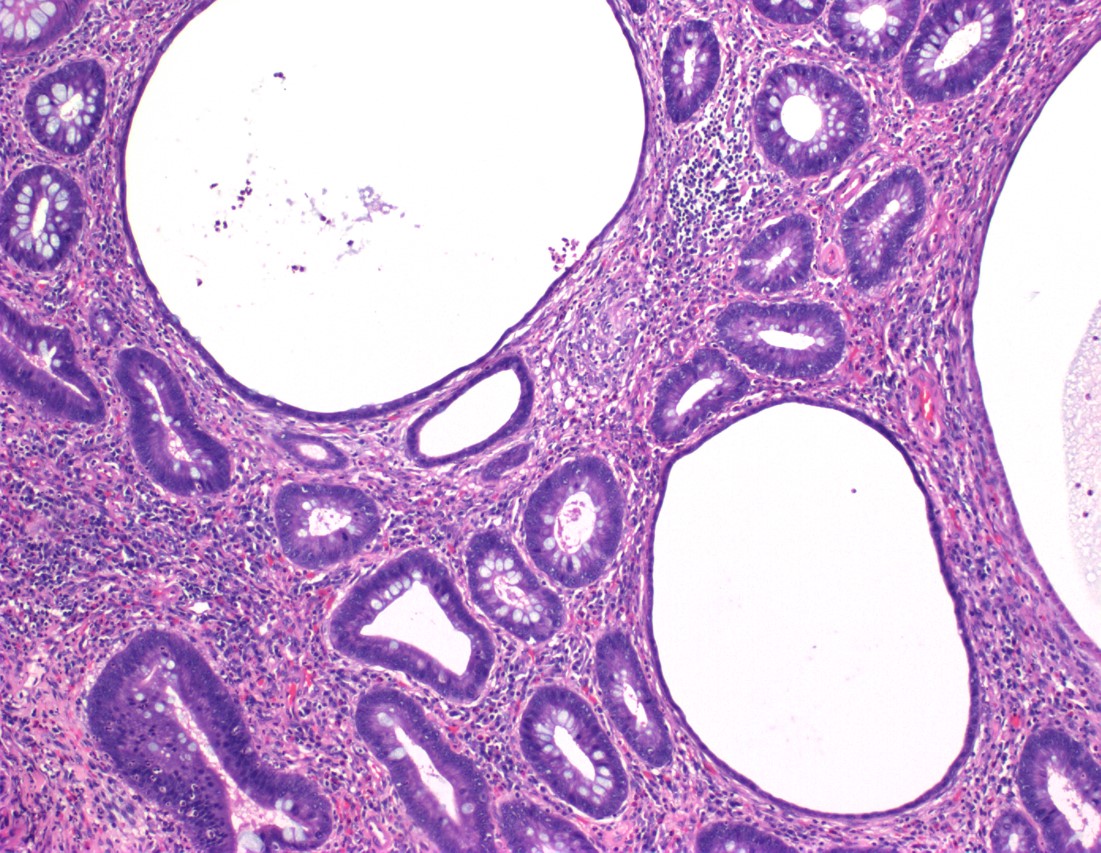
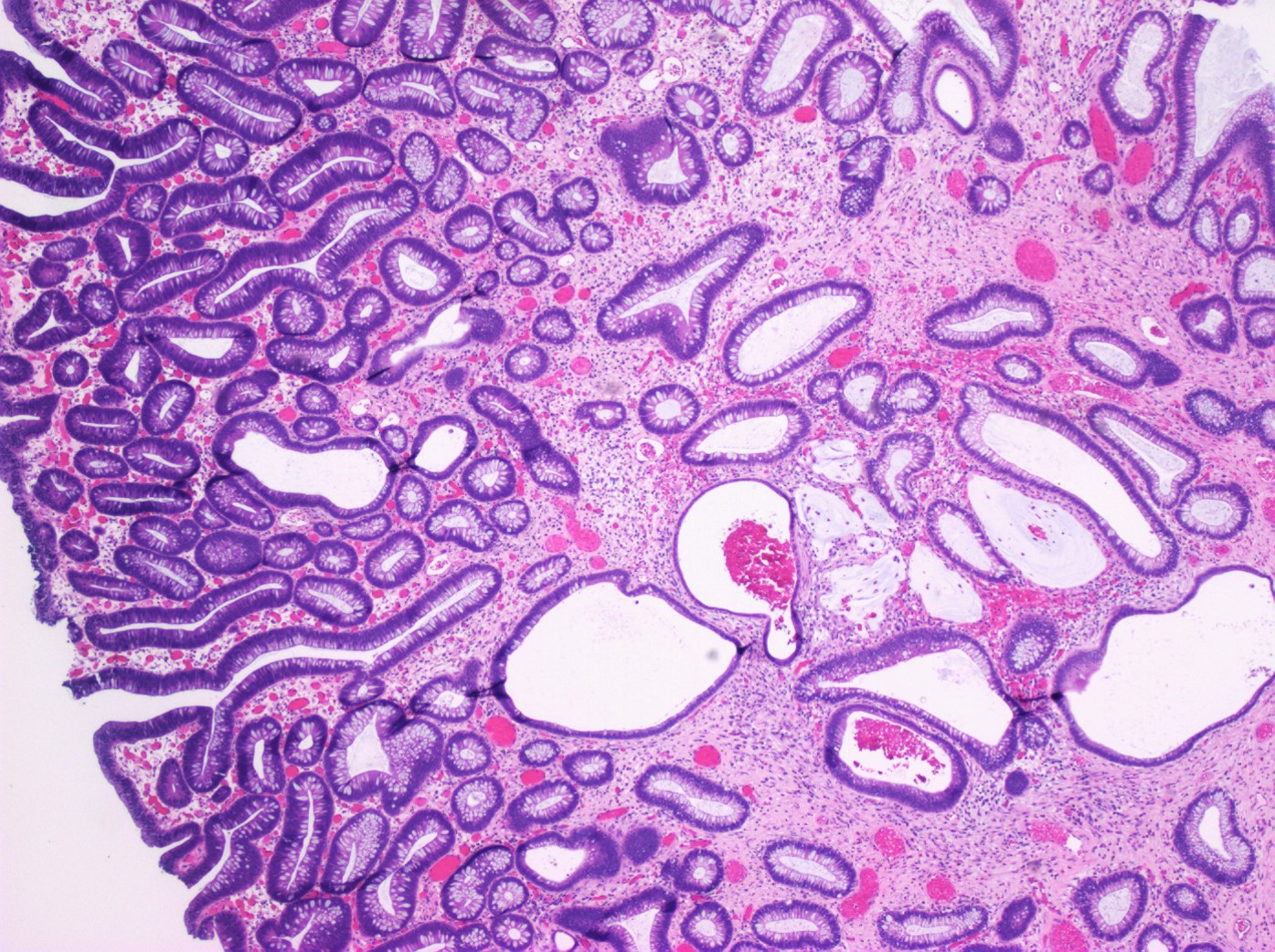
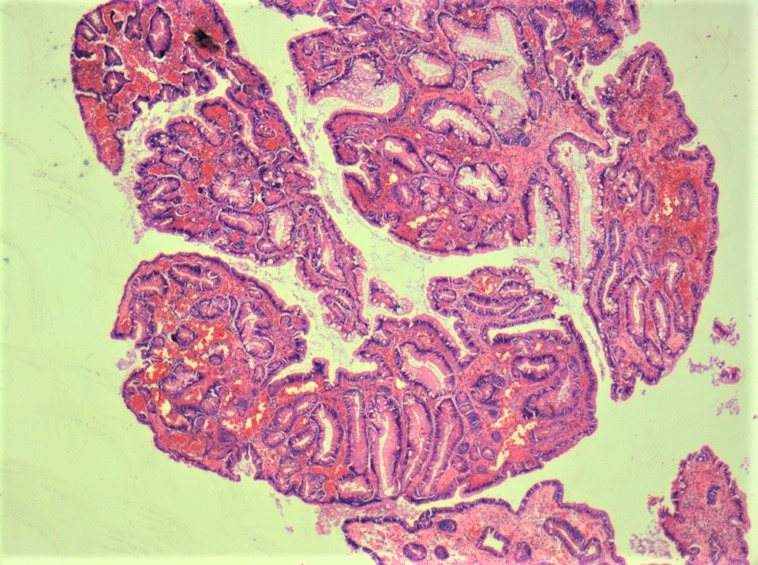
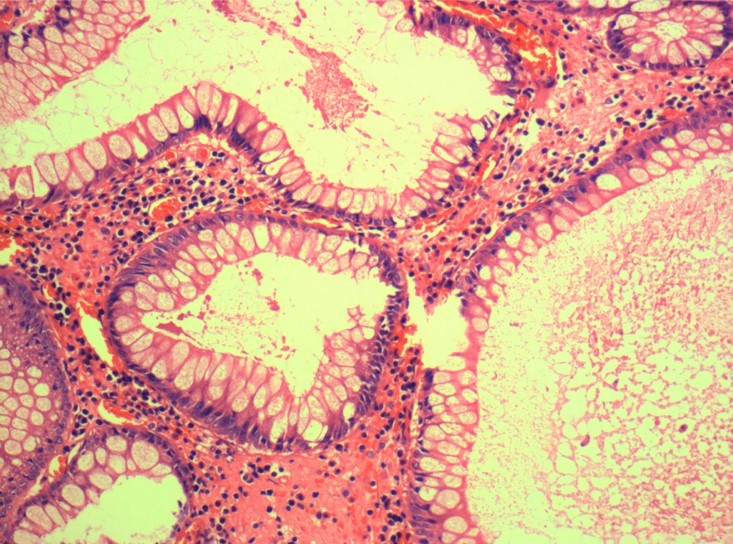
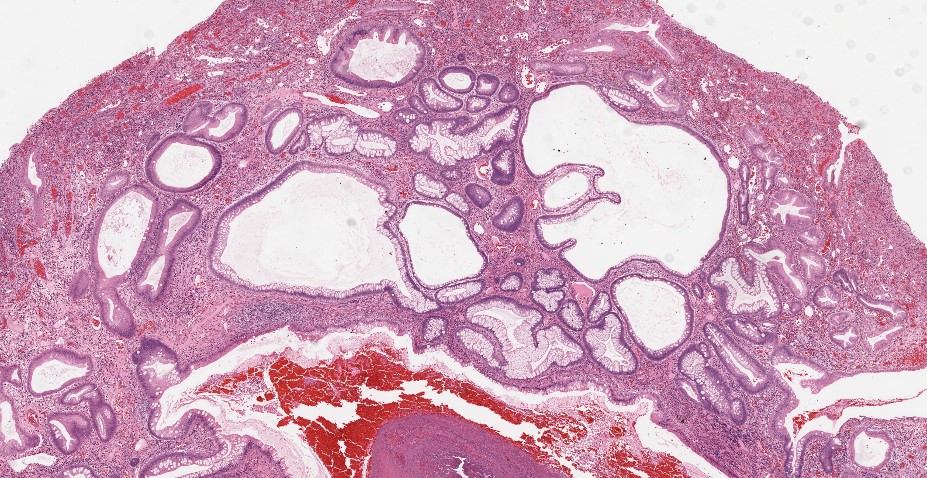
Microscopic (histologic) description
- Characterized by an abundance of edematous lamina propria with inflammatory cells and cystically dilated glands lined by cuboidal to columnar epithelium with reactive changes (nonneoplastic, hamartomatous, epithelial retentions)
- Dilated glands filled with mucus and inspissated inflammatory debris
- Juvenile polyposis syndrome:
- Polyps appear similar to sporadic solitary juvenile polyps, although syndromic polyps often have a frond-like growth pattern with less stroma, fewer dilated glands and more proliferative smaller glands
- JPS polyps frequently show neoplastic changes to the epithelium not common in sporadic solitary juvenile polyps
- Reference: World J Gastroenterol 2011;17:4839
Microscopic (histologic) images
Virtual slides
Positive stains
- TP53 mutations (p53 mutated pattern staining) can be seen with high grade dysplasia in polyps of juvenile polyposis syndrome
Negative stains
- p53 shows wild type pattern staining in benign solitary juvenile polyp, as there is no dysplastic change
Molecular / cytogenetics description
- Germline mutation in the SMAD4 (18q21.1) or BMPR1A (10q23.2) gene is found in 40 - 60% of patients with juvenile polyposis syndrome
- JPS patients with SMAD4 mutations are associated with more aggressive gastric polyps and appear to have a higher risk for gastric cancer (J Pediatr Gastroenterol Nutr 2019;68:453)
Videos
Histopathology of juvenile polyps
Endoscopy of juvenile polyps
Sample pathology report
- Colon, polypectomy:
- Solitary juvenile polyp (see comment)
- Comment: Negative for dysplasia or malignancy
Differential diagnosis
- Cronkhite-Canada syndrome:
- Changes in the surrounding mucosa, clinical findings (nail atrophy, skin pigment, alopecia)
- Hyperplastic polyp:
- Sawtoothed appearance of glands, cystic dilatation not prominent
- Inflammatory polyp:
- Common in inflammatory bowel disease and diverticulitis; irregularly dilated glands, no prominent cystic dilationn
- Peutz-Jeghers polyp:
- Prominent arborizing smooth muscle bundles
- Tubular adenoma:
- Cytologic dysplasia, cystic dilation usually not prominent, inflamed stroma usually not prominent
Additional references
Board review style question #1
Board review style answer #1
B. Hamartomatous polyp. The picture shows a juvenile polyp with cystically dilated glands in an edematous and inflammatory stroma with ulceration. Juvenile polyp is a hamartomatous polyp.
Comment Here
Reference: Juvenile (retention) polyp
Comment Here
Reference: Juvenile (retention) polyp
Board review style question #2
Which of the following is true regarding juvenile polyp?
- Most common clinical presentation is intussusception
- Mostly seen in proximal stomach
- Solitary juvenile polyp has minimal risk of malignant transformation
- Uncommon type of pediatric polyp
Board review style answer #2
C. Solitary juvenile polyp has minimal risk of malignant transformation. Juvenile polyp is the most common type of pediatric intestinal polyp, mostly seen in distal colon. Painless rectal bleed is the most common clinical presentation. Solitary juvenile polyps have minimal malignant potential; however, multiple juvenile polyps may indicate a premalignant condition (juvenile polyposis coli or juvenile polyposis syndrome [JPS]).
Comment Here
Reference: Juvenile (retention) polyp
Comment Here
Reference: Juvenile (retention) polyp