Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Fernández-Aceñero MJ. Inflammatory fibroid polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorinflammatoryfibroid.html. Accessed March 29th, 2025.
Definition / general
- Rare mesenchymal polypoid neoplasms that arise anywhere throughout the GI tract but most commonly in the stomach and small intestine
Essential features
- Benign mesenchymal polypoid neoplasm centered in the submucosa
- Rare in the large bowel
- Proliferation of bland spindle cells with a variable myxoid background and varying degree of inflammatory infiltration
- Association with activating PDGFRA gene mutation
Terminology
- Formerly known as Vanek tumor (no longer recommended)
- Terminological confusion in older literature (e.g., granuloblastoma, gastric fibroma with eosinophilic infiltration, eosinophilic granuloma)
- Inflammatory fibroid polyp (IFP) is the recommended term
ICD coding
- ICD-10: K51.419 - inflammatory polyps of colon with unspecified complications
Epidemiology
- Predominance in middle aged adults (median 53 years), with wide variation (4 - 84 years)
- Very rare in children (World J Clin Pediatr 2015;4:160)
- Slight predominance in women (1.3:1) (In Vivo 2021;35:81)
- Increased frequency in menopausal women has led to postulate a potential relationship with androgens (Anticancer Res 2014;34:7203)
Sites
- Most frequent location is the stomach (> 65% in a recent meta analysis of 417 cases), mainly the antrum (In Vivo 2021;35:81)
- < 10% of cases arise in the large bowel
Pathophysiology
- For a long time, it was considered reactive in nature (autoimmune, allergic)
- Discovery of overexpression and mutations in platelet derived growth factor receptor alpha (PDGFRA) has led to considering inflammatory fibroid polyp a neoplastic process
Etiology
- Unknown
- May be familial (Devon polyposis syndrome) (Gut 1992;33:1004)
Clinical features
- Symptoms largely depend on location
- For large bowel lesions, abdominal pain and acute intestinal obstruction are the most frequent presenting symptoms
- Nonmalignant potential
- Some familial cases and occasional association with GI malignancies (Trop Gastroenterol 2014;35:196, Ann Diagn Pathol 2012;16:148)
- Not usually associated with peripheral eosinophilia
- No endoscopic surveillance is required after the histological diagnosis is confirmed
Diagnosis
- Histologic
Prognostic factors
- Good prognosis with no risk of malignization
Case reports
- 23 year old woman with iron deficiency anemia and a 4.5 cm polypoid lesion in the descending colon removed with a needle knife (Yonsei Med J 2008;49:680)
- 50 year old woman with bloating and abdominal pain with a diagnosis of intussusception undergoes an emergency right hemicolectomy (Medicina (Kaunas) 2022;58:310)
- 53 year old man with diabetes and hypercholesterolemia undergoes a routine colonoscopy, which reveals a 4 cm lobular mass in the proximal rectum removed by transanal resection (J Surg Case Rep 2019;2019:rjz164)
- 65 year old woman with mild abdominal pain for 3 years and a large elongated mass in the cecum (Chin Med J (Engl) 2017;130:2130)
Treatment
- Resection is the preferred therapy
- Endoscopic resection is the preferred option, either polypectomy or endoscopic submucosal or radical resection
- Need of surgical resection in some complicated cases
- No further therapy is necessary
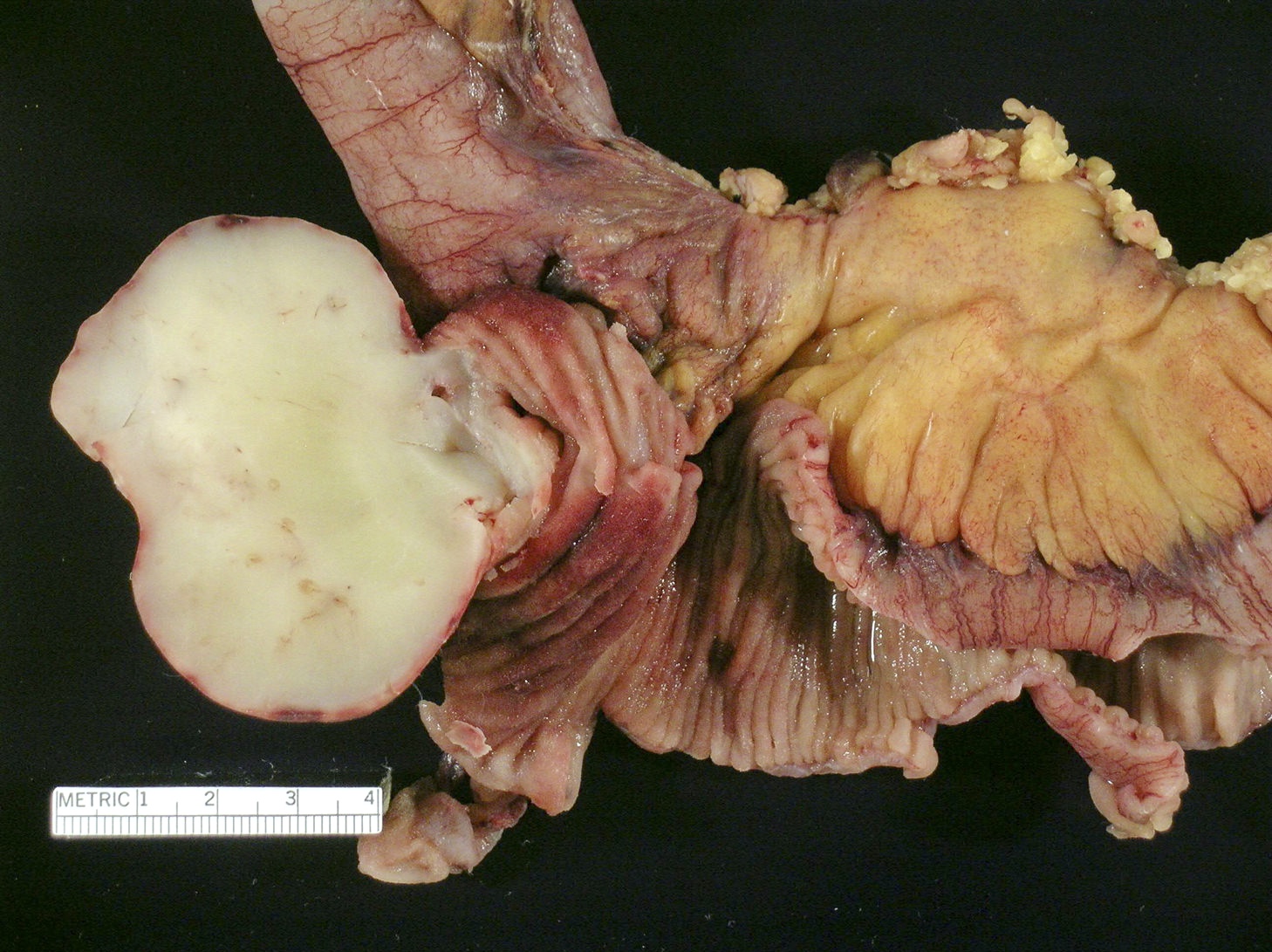
Gross description
- Solitary intraluminal, usually sessile polypoid lesion
- Frequently ulcerated
- Can reach large size (giant inflammatory fibroid polyp measuring > 4 cm)
- As opposed to usual gastric inflammatory fibroid polyp, large bowel lesions can infiltrate through the wall, reaching neighboring structures and mimicking malignancy (Kaohsiung J Med Sci 2013;29:460)
Gross images
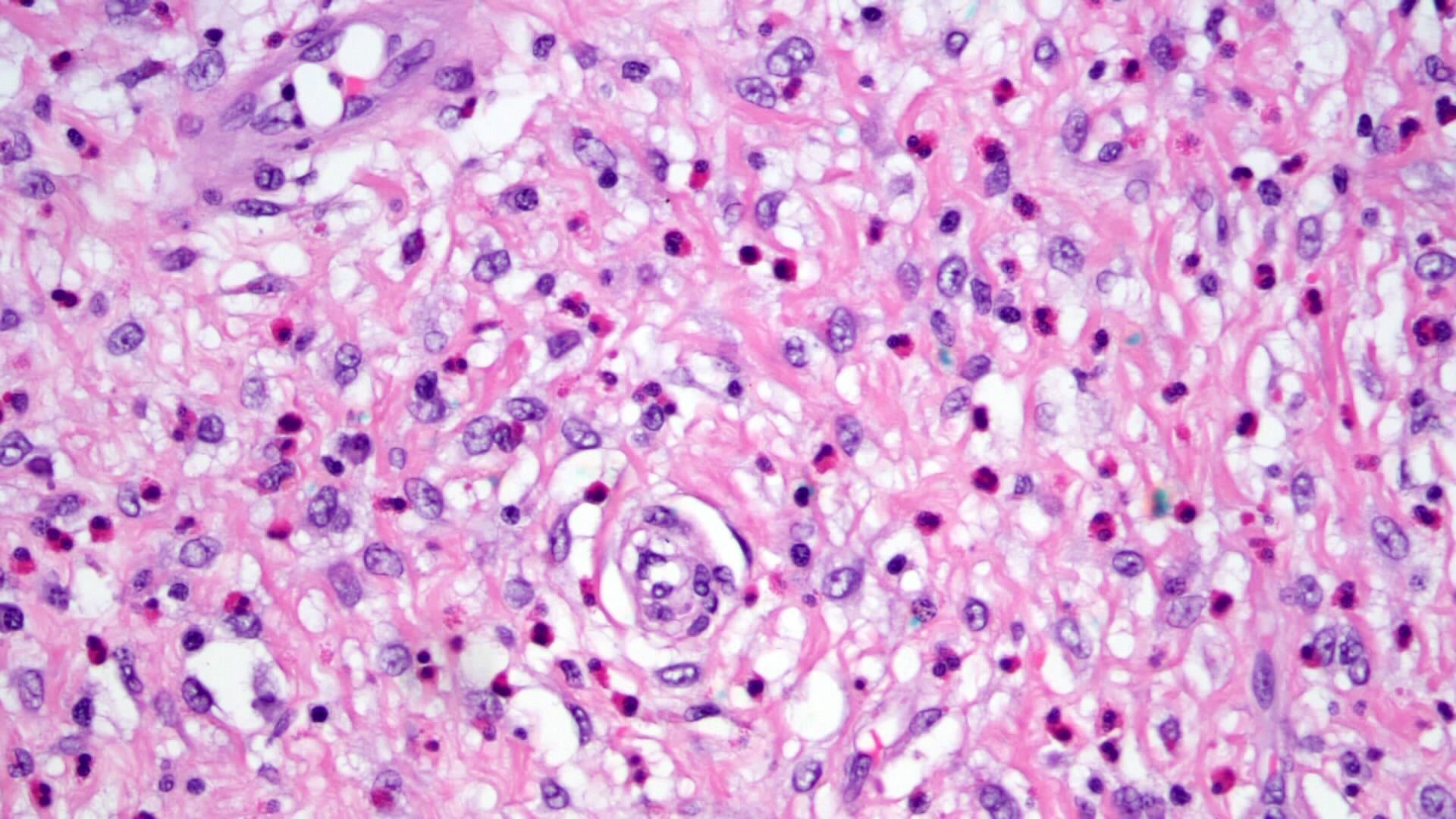
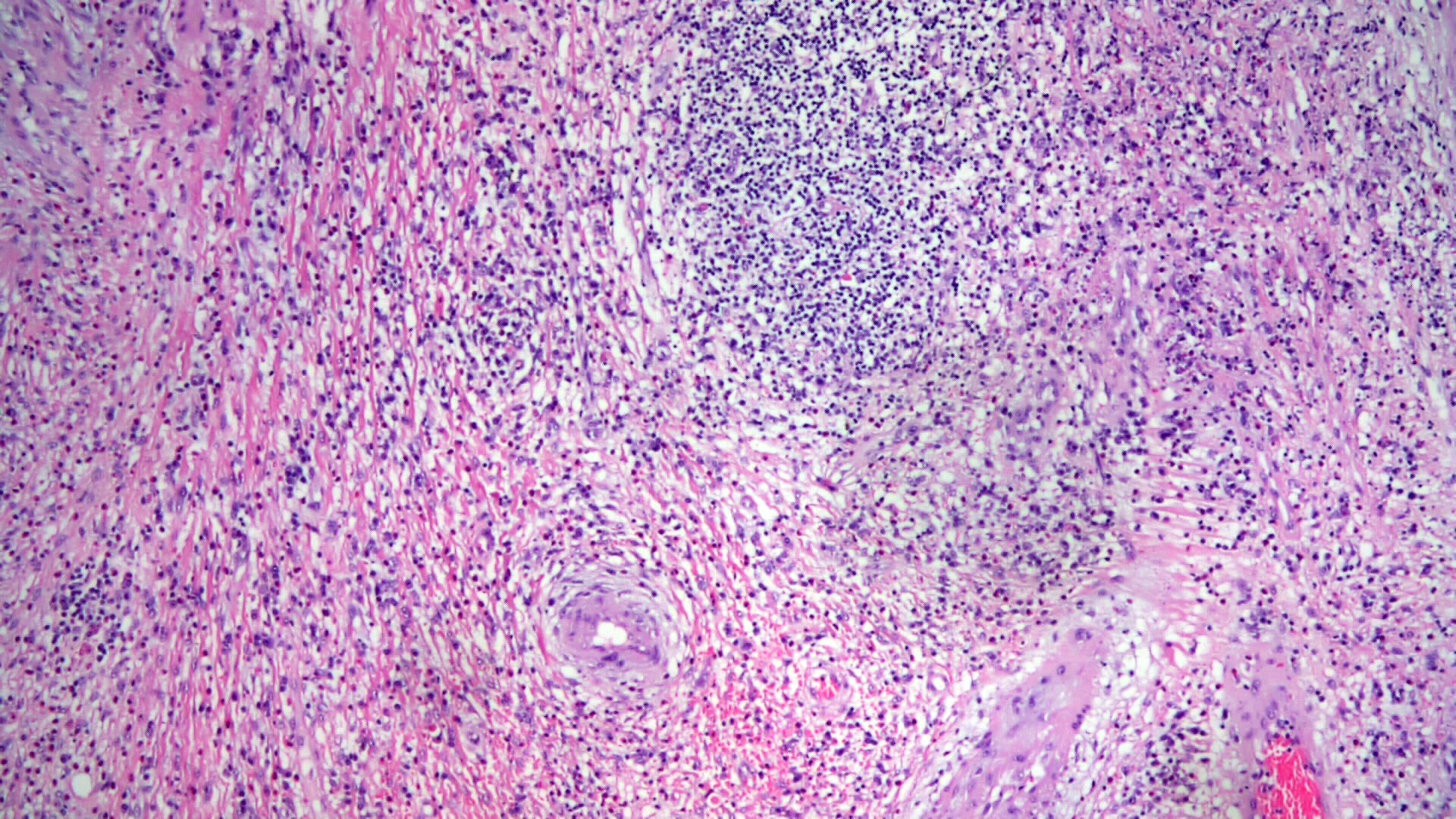
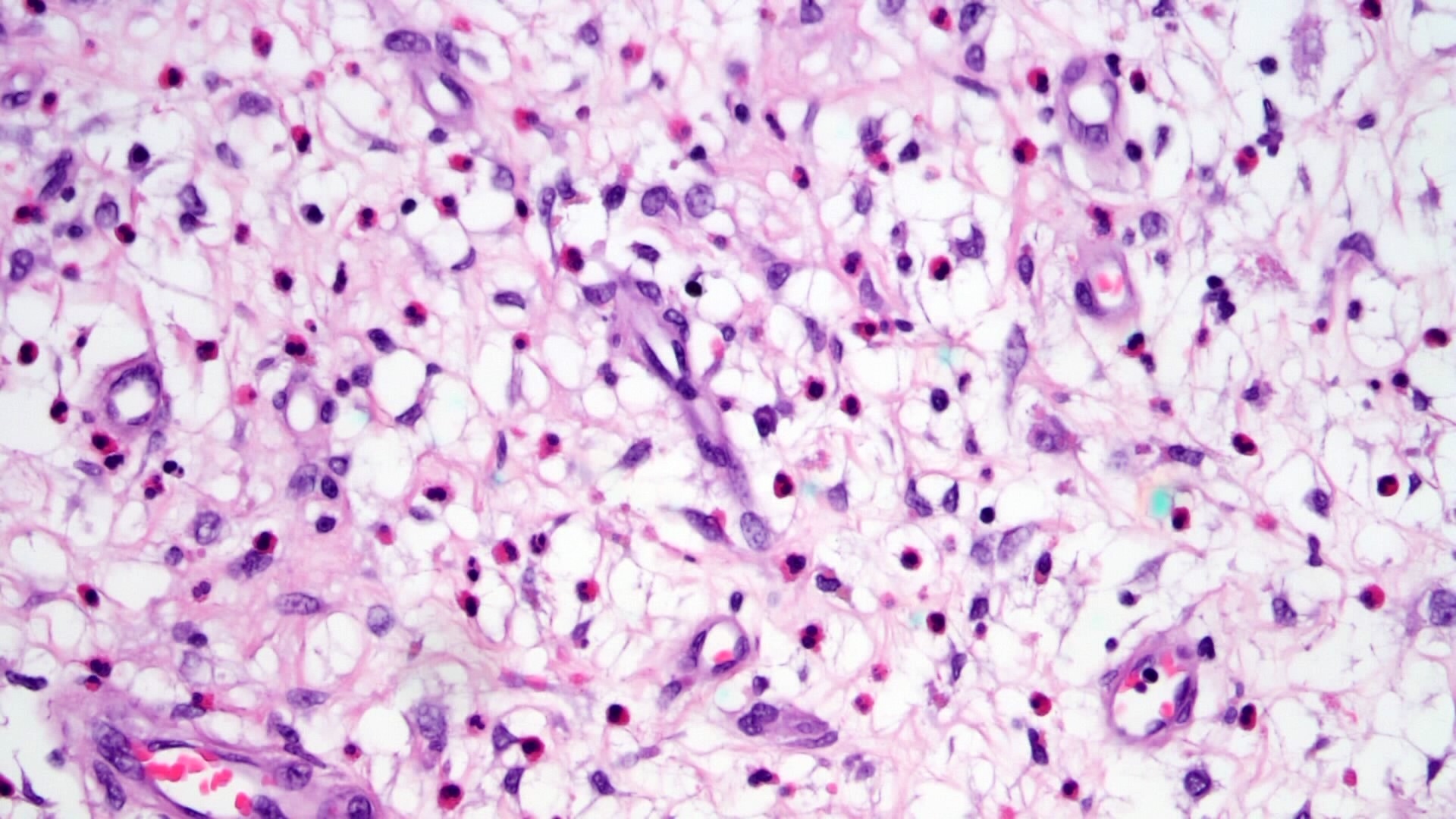
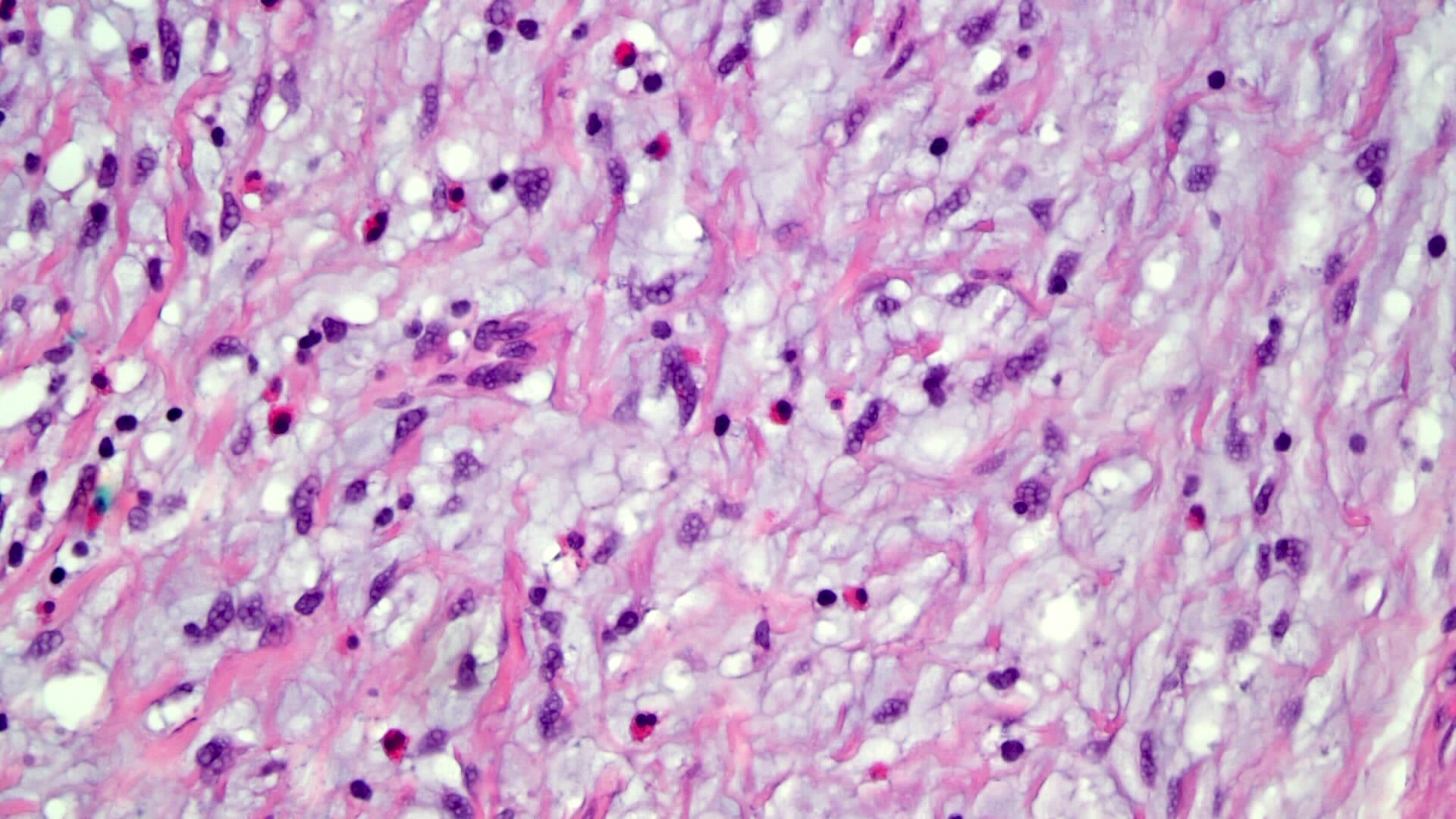
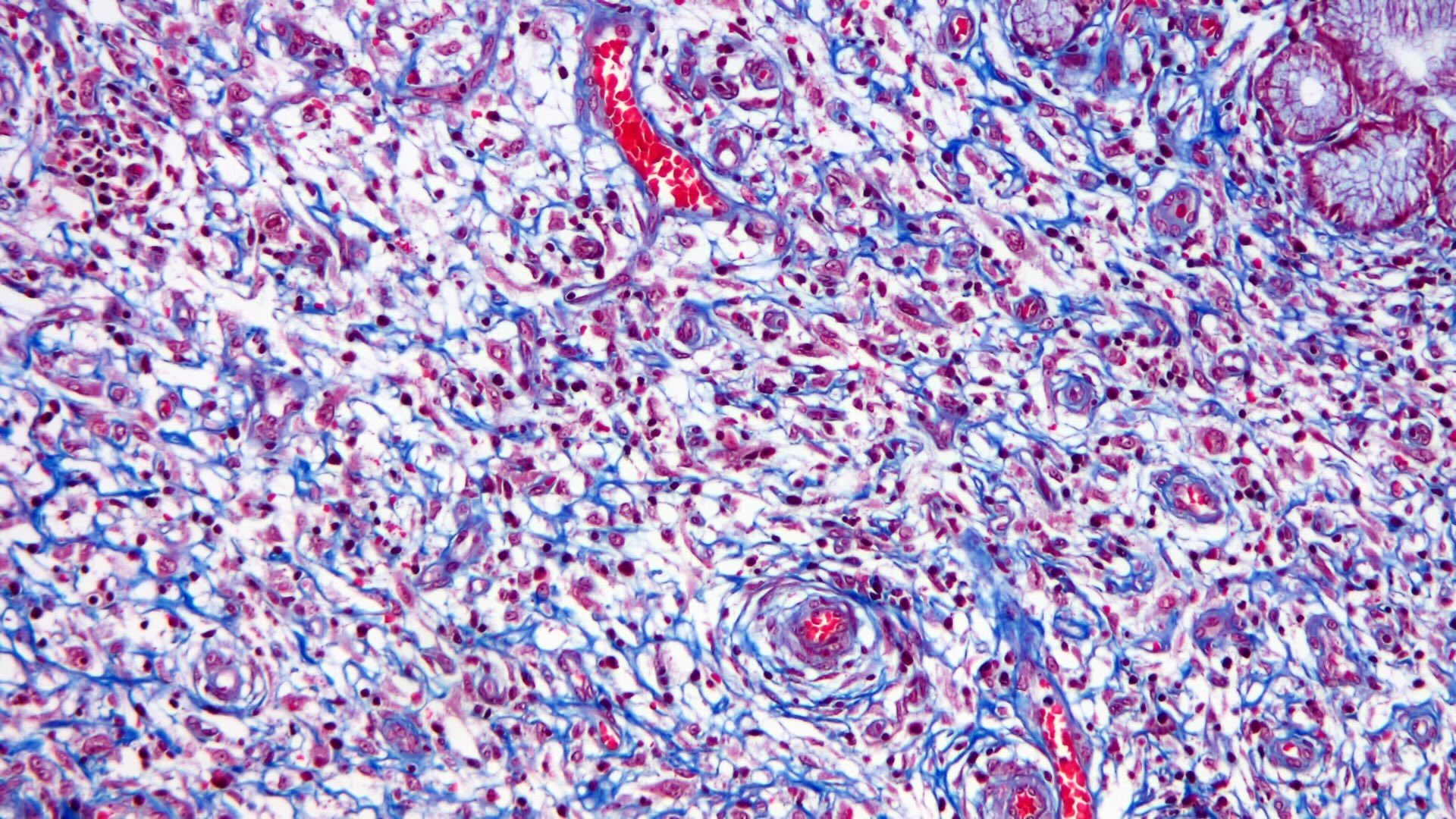
Microscopic (histologic) description
- Mostly centered in the submucosa but can infiltrate lamina propria
- Well demarcated but encapsulated
- Proliferation of bland mesenchymal cells
- Background with small vessel proliferation, little collagen, inflammatory infiltrates and variable degrees of edema
- Distinctive onion skin arrangements of spindled cells around vessels
- Vessels can be ectatic
- Inflammatory infiltrate rich in eosinophils
- 5 histopathological patterns proposed, probably representing a spectrum of disease over time:
- Classical fibrovascular
- Nodular
- Sclerotic
- Edematous
- Atypical (very rare)
- Scarce mitosis, never atypical
Microscopic (histologic) images
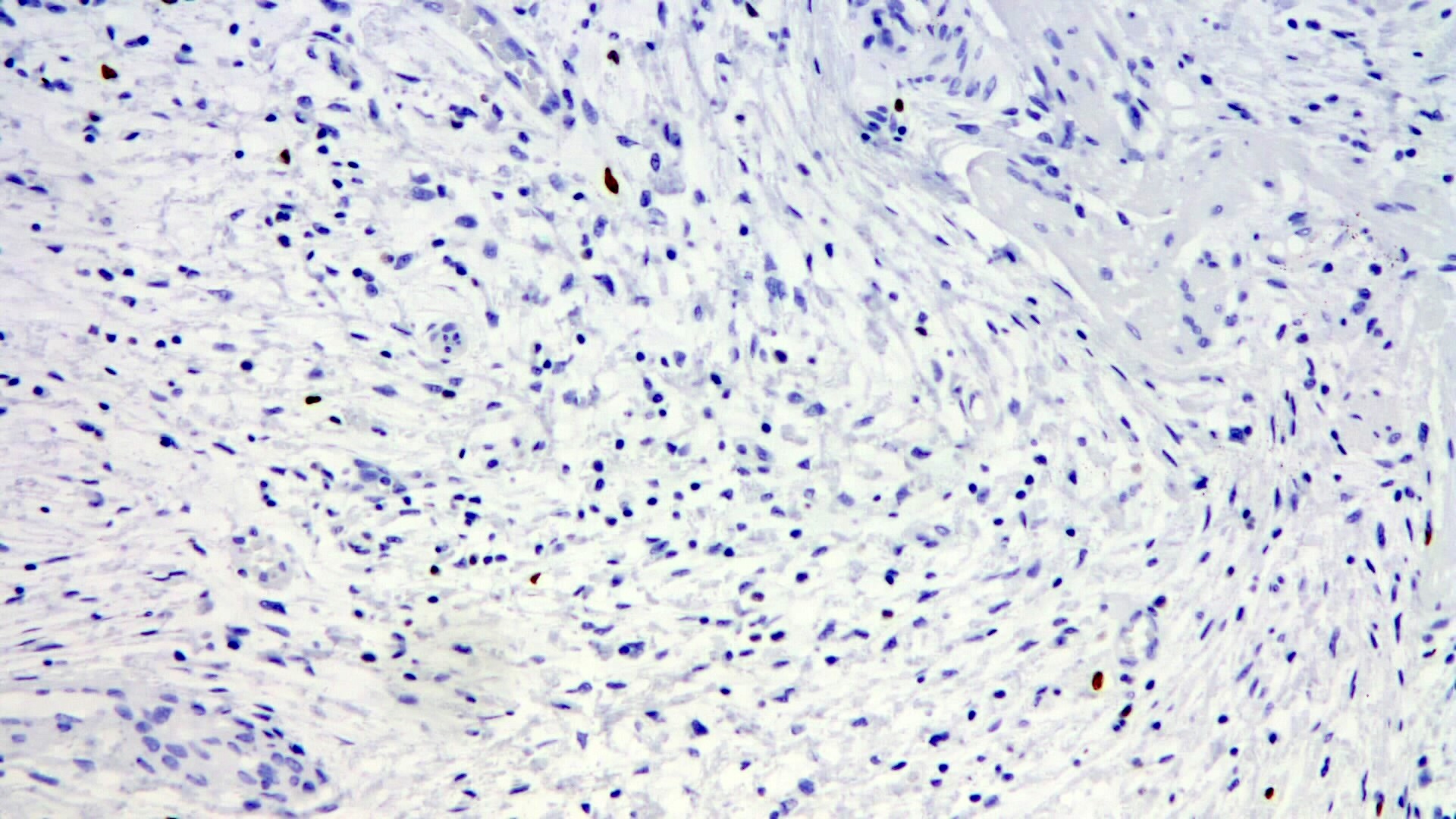
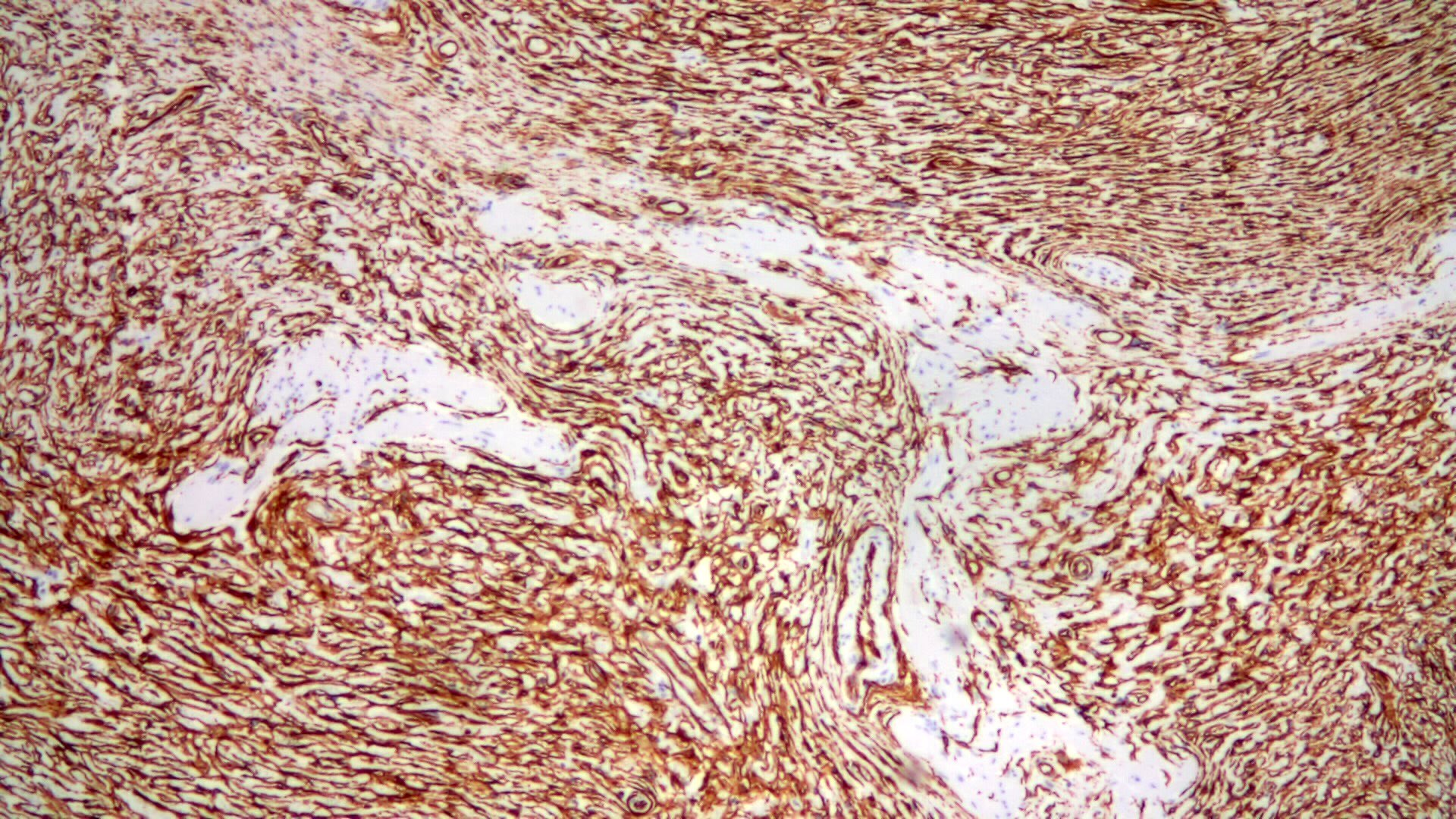
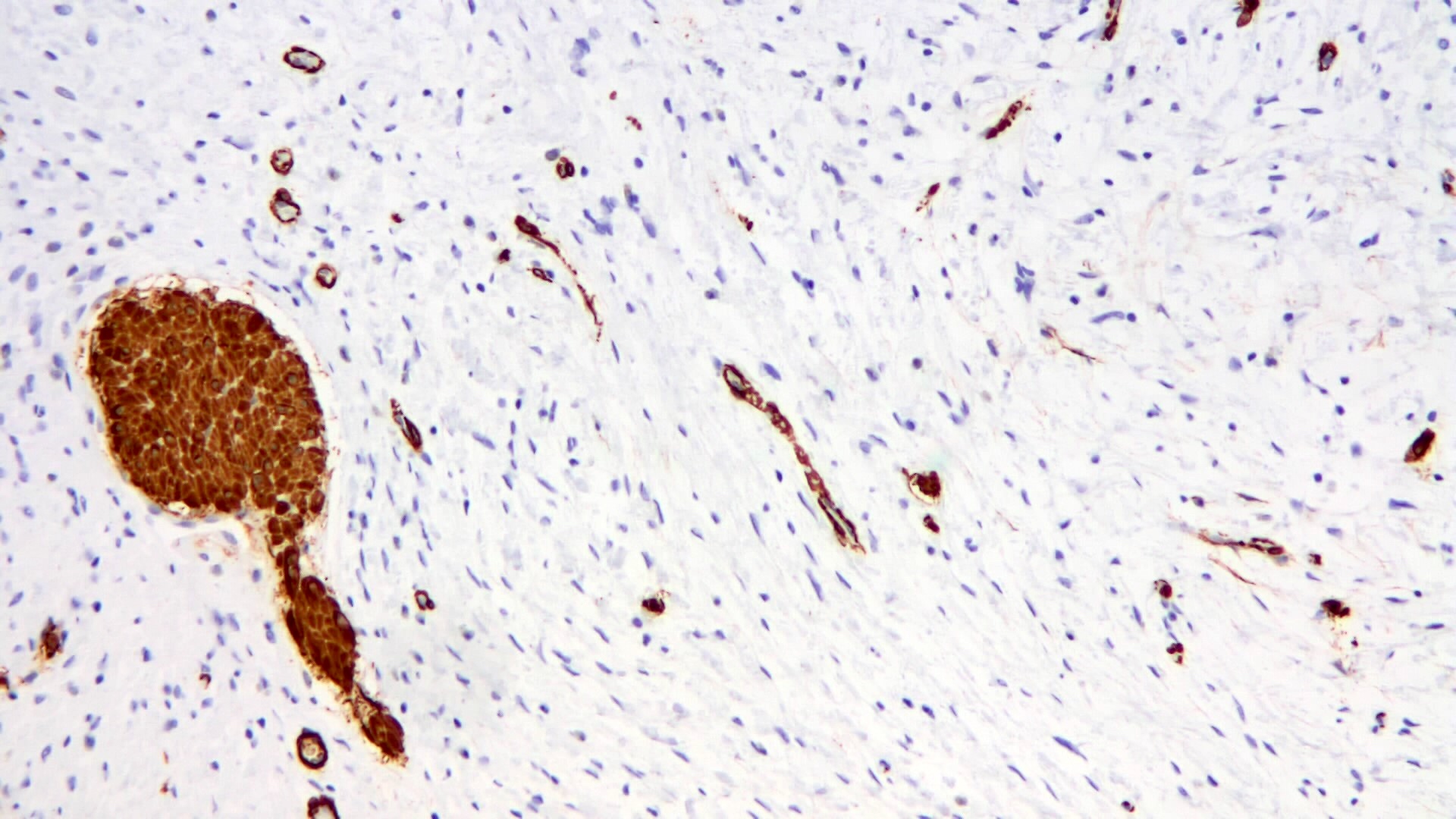
Positive stains
- Spindle cells are usually positive for CD34 (82 - 100%), with a variable intensity
- Variable smooth muscle actin
- PDGFRA frequently positive, even in cases with no PDFGRA mutations by molecular testing (Pathol Int 2018;68:205)
Negative stains
- CD117 (KIT) (although mast cells are CD117+), DOG1 and S100
- Anaplastic lymphoma kinase (ALK)
- Alpha smooth muscle actin can be focally positive
Electron microscopy description
- No recent reports regarding electron microscopy features of this lesion
- Older reports indicate a combination of fibroblastic and histiocytic features in the tumor cells
- Putative origin in primitive submucosal stromal cells
Molecular / cytogenetics description
- Activating mutations in exons 12, 14 and 18 of PDGFRA in > 50% of inflammatory fibroid polyps, with described differences according to location (Mod Pathol 2009;22:1049)
- PDGFRA mutations seem less frequent in large bowel lesions (Pathol Int 2018;68:205)
- Descriptions of germline mutations in PDGFRA leading to familial cases of inflammatory fibroid polyp or gastrointestinal stromal tumor (GIST) (Cancer Genet 2021;256:106)
Sample pathology report
- Large bowel, endoscopic polypectomy
- Inflammatory fibroid polyp (1.3 cm) (see comment)
- Comment: The lesion is centered in the submucosa and is composed of bland proliferation of spindled cells with prominent eosinophils. The lesional cells express CD34 and are negative for CD117 and DOG1.
Differential diagnosis
- Gastrointestinal stromal tumor:
- Inflammatory myofibroblastic tumor:
- Histology can be similar with spindle cell myofibroblasts and fibroblasts on an inflammatory background with lymphocytes and plasma cells
- Eosinophils are less prominent
- Tumor cells express alpha SMA and desmin and are CD34 negative
- ALK expression by IHC with rearrangements of the ALK gene locus 2p23 in up to 70% of cases
- Inflammatory polyp:
- Usually associated with inflammatory bowel disease
- CD34 negative
- Inflammatory myoglandular polyp (BMC Gastroenterol 2010;10:10):
- Rare nonneoplastic polyp of the large bowel
- Pedunculated and more frequent in the sigmoid colon, with a ripe wild strawberry endoscopic aspect
- Inflammatory granulation tissue with engorged capillaries in lamina propria
- Hyperplastic glands with cystic dilatations
- Proliferation of smooth muscle from the muscularis mucosae
- Angiolymphoid hyperplasia with eosinophilia:
- Extremely rare in the large bowel
- Proliferation of immature blood vessels with epithelioid endothelial cells and infiltration by lymphocytes and eosinophils
- Lack of PDGFRA IHC expression
- Perineuroma / fibroblastic polyps:
- Proliferation of spindle cells limited to mucosa and submucosa
- Frequent association with serrated crypts
- IHC: EMA, claudin1 and GLUT1 positive
- Frequent BRAF p.V600E mutations in the epithelial component (Clin Med Insights Pathol 2018;11:1179555718815918)
- Schwannomas:
- Typical pattern of growth with Verocay bodies
- IHC: S100 positive
- Reference: Histopathology 2020;76:342
Board review style question #1
Board review style answer #1
D. It is polypoid and originates in the submucosa. Inflammatory fibroid polyps are usually polypoid and originate in the submucosa, as opposed to other kind of stromal lesions, like gastrointestinal stromal tumors or schwannoma.
Comment Here
Reference: Inflammatory fibroid polyp
Comment Here
Reference: Inflammatory fibroid polyp
Board review style question #2
Which statement is true regarding IHC for PDGFRA in inflammatory fibroid polyps?
- Allows differential diagnosis with GIST
- Always positive
- Always negative
- Confirms reactive nature of the process
- Does not always reflect a mutation in PDGFRA gene
Board review style answer #2
E. Does not always reflect a mutation in PDGFRA gene. IHC for PDFGRA can be positive in cases with no shown mutation of PDGFRA gene.
Comment Here
Reference: Inflammatory fibroid polyp
Comment Here
Reference: Inflammatory fibroid polyp