Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology / etiology | Diagrams / tables | Clinical features | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Obeidin F, Alexiev B. Fibromatosis-desmoid. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuefibromatosisdeep.html. Accessed December 18th, 2024.
Definition / general
- Locally aggressive fibroblastic / myofibroblastic tumor arising in deep soft tissues with no metastatic potential
Essential features
- Benign tumor with infiltrative borders and a propensity for local recurrence
- May be associated with familial adenomatous polyposis (Gardner syndrome)
- Histology: long, sweeping fascicles with thin walled vessels and microhemorrhages; bland cells with mild to moderate cellularity and minimal atypia
- Immunohistochemistry: SMA+ and nuclear beta catenin+
- Molecular: CTNNB1 and APC mutations may be seen
Terminology
- Synonyms: aggressive fibromatosis, musculoaponeurotic fibromatosis, desmoid tumor, deep fibromatosis
ICD coding
- ICD-O: 8821/1 - desmoid type fibromatosis
- ICD-10: D48.1 - neoplasm of uncertain behavior of connective and other soft tissue
- ICD-11:
- 2F7C & XH13Z3 - neoplasm of uncertain behavior of connective or other soft tissue & desmoid type (aggressive) fibromatosis
- 2F7C & XH6116 - neoplasm of uncertain behavior of connective or other soft tissue & abdominal (mesenteric) fibromatosis
Epidemiology
- ~0.03% of all neoplasms; < 3% of all soft tissue tumors
- 10 - 30% of familial adenomatous polyposis (FAP) patients have desmoid type fibromatosis (also called Gardner syndrome); 7.5 - 16% of patients with fibromatosis have FAP
- Mean age: 36 - 42 years
- Female predominance from puberty to age 40; younger and older patients have M:F = ~1:1 (Am J Clin Pathol 1982;77:665)
- Male predominance in FAP of 3:1 (Int J Cancer 2011;129:256)
Sites
- 37 - 50% occur in the abdominal region; shoulder girdle, chest wall and inguinal regions are the most prevalent extraabdominal sites
- In FAP: majority (51 - 67%) are intraabdominal or in the abdominal wall
- Sporadic: extraabdominal are more common
- Tendency of premenopausal and pregnant women to develop fibromatosis in the abdominal wall musculoaponeurosis (Fam Cancer 2006;5:191)
Pathophysiology / etiology
- CTNNB1 and APC gene mutations can account for up to 89% of cases (Genes Chromosomes Cancer 2010;49:560)
- May be driven by a combination of genetic mutations, high estrogen states and antecedent trauma which leads to activation of the canonical Wnt / β catenin pathway
Clinical features
- Extraabdominal tumors are deep seated, poorly circumscribed and painless
- Abdominal wall tumors typically arise in gravid or postpartum women
- Intraabdominal tumors arise as slowly growing, painless masses that may mimic ovarian tumors
Radiology description
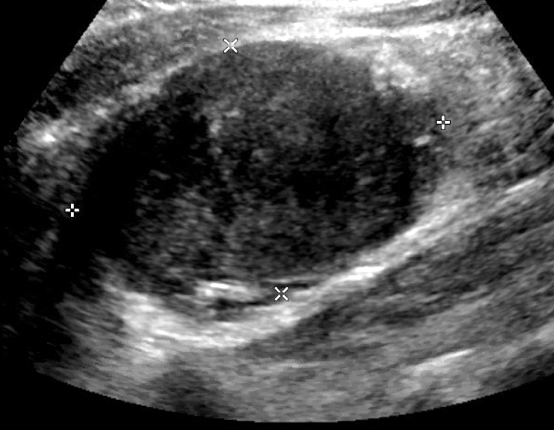
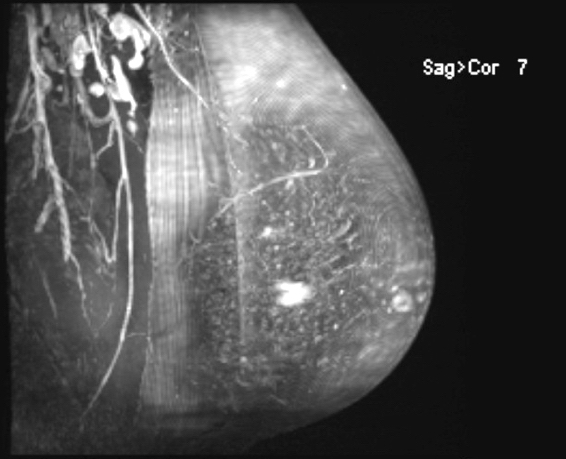
- Ultrasound:
- Can be used with palpable masses of the extremities, abdominal, chest wall, breast, etc.
- Oval, well to poorly marginated solid soft tissue mass with variable echogenicity
- May have thin, linear extension along fascial planes (fascial tail sign) or intramuscular finger-like extensions (staghorn sign)
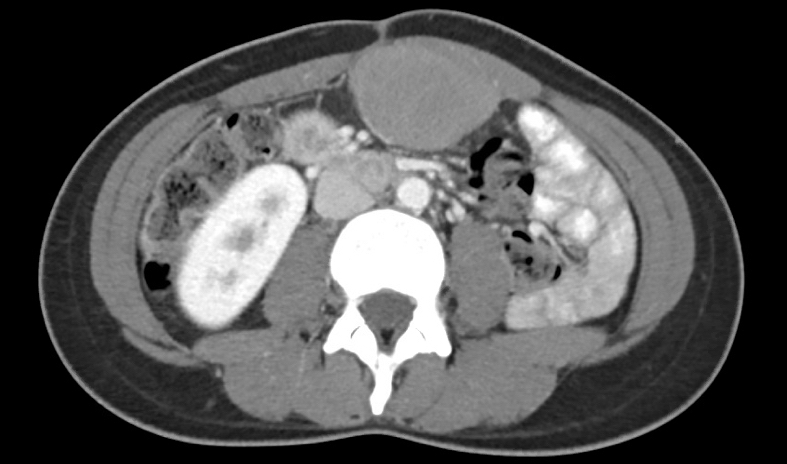
- CT:
- Most commonly used for intraabdominal tumors and associated complications (like small bowl obstruction)
- Soft tissue mass with well to poorly defined margins, variable attenuation and mild to moderate enhancement
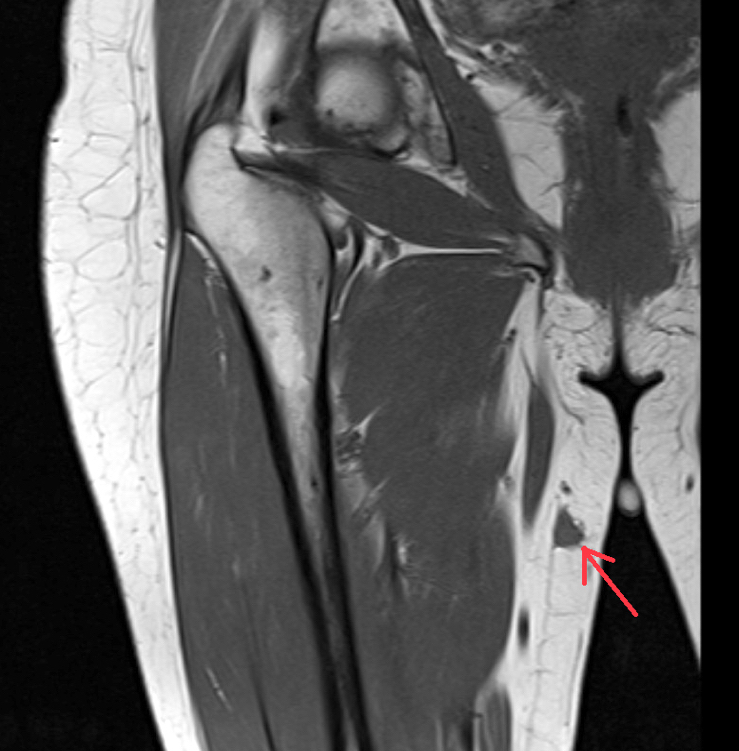
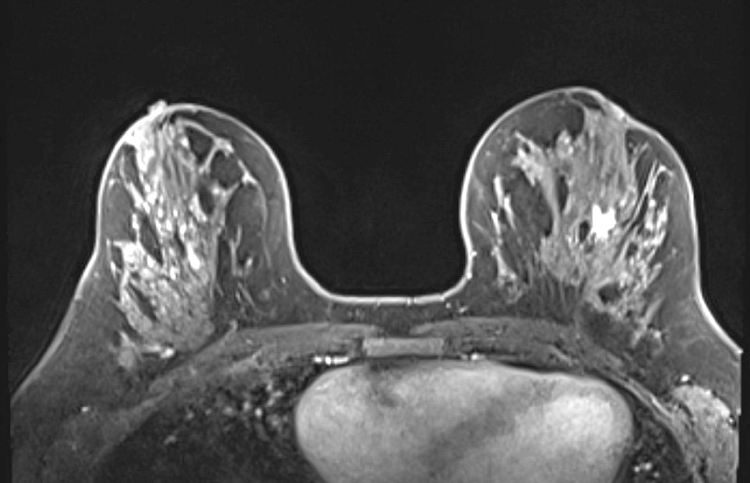
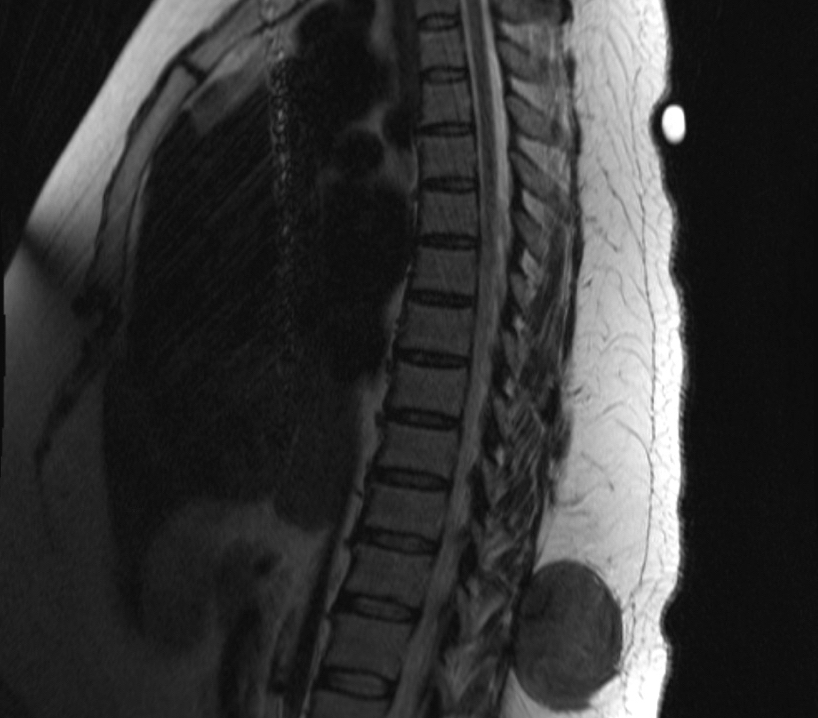
- MRI:
- Preferred modality for abdominal wall and extraabdominal tumors
- Heterogeneous iso to hyperintense to skeletal muscle on T2, isointense to muscle on T1
- Nonenhancing linear bands (Band sign) can be seen in 60 - 90% of cases
- Moderate to marked enhancement after gadolinium based contrast (Radiographics 2016;36:767)
Radiology images
Prognostic factors
- Local recurrence in 20 - 30%
- Margin status shown to predict local recurrence in primary tumors but was not significant in recurrent presentations
- Other factors such as age, gender, presentation status, tumor size, tumor focality and histologic type have shown inconsistent predictive value
- Complete excision may cause significant morbidity and mortality in certain locations (Cancer 1999;86:2045, J Surg Oncol 2009;100:563, Ann Surg Oncol 2012;19:4028)
- CTNNB1 S45F mutation associated with significantly increased risk of recurrence (Ann Surg Oncol 2015;22:1464)
Case reports
- 9 month old girl with a recurrent tongue mass (J Med Case Rep 2016;10:173)
- 14 month old boy with an 8 cm mass in the right parapharyngeal space (Am J Otolaryngol 2016;37:372)
- 9 year old boy with intraabdominal tumor invading colonic wall (Eur J Pediatr Surg 2005;15:196)
- 25 year old man with a tongue mass (Head Neck Pathol 2016;10:527)
- 40 year old man with an initial diagnosis of a lower leg deep vein thrombosis with progressive calf swelling (Am J Case Rep 2016;17:967)
- 42 year old woman with a left neck mass for 1 year (Saudi Med J 2015;36:101)
- 72 year old man with colonic mesenteric tumor causing acute abdomen (Indian J Gastroenterol 2002;21:199)
- 75 year old woman with an abdominal mass located in the anterior pancreas (Pathol Res Pract 2016;212:484)
Treatment
- Highly variable natural course, with up to 25% undergoing spontaneous regression
- Increasing tendency to follow with observation only (Ann Surg Oncol 2013;20:4096)
- Mainstay of treatment is surgical resection, which can result in significant morbidity
- Radiotherapy alone and surgery plus adjuvant radiotherapy have shown improved local control over surgery alone; however, long term effects of radiation therapy prevent standard use, especially in young patients
- Systemic therapy for advanced disease (Oncologist 2011;16:682):
- Antihormonal therapy (tamoxifen) can be used as first line in asymptomatic patients
- Nonsteroidal anti-inflammatory drugs (NSAIDs) have shown good response in some studies but no randomized trials yet
- Several conventional chemotherapy have been assessed, doxorubicin and dacarbazine combination or pegylated liposomal doxorubicin preferred
- Response evaluation criteria in solid tumors (RECIST) trial shows some response with receptor tyrosine kinase inhibitors; sorafenib and sunitinib may be more efficacious than imatinib but studies are ongoing
Clinical images
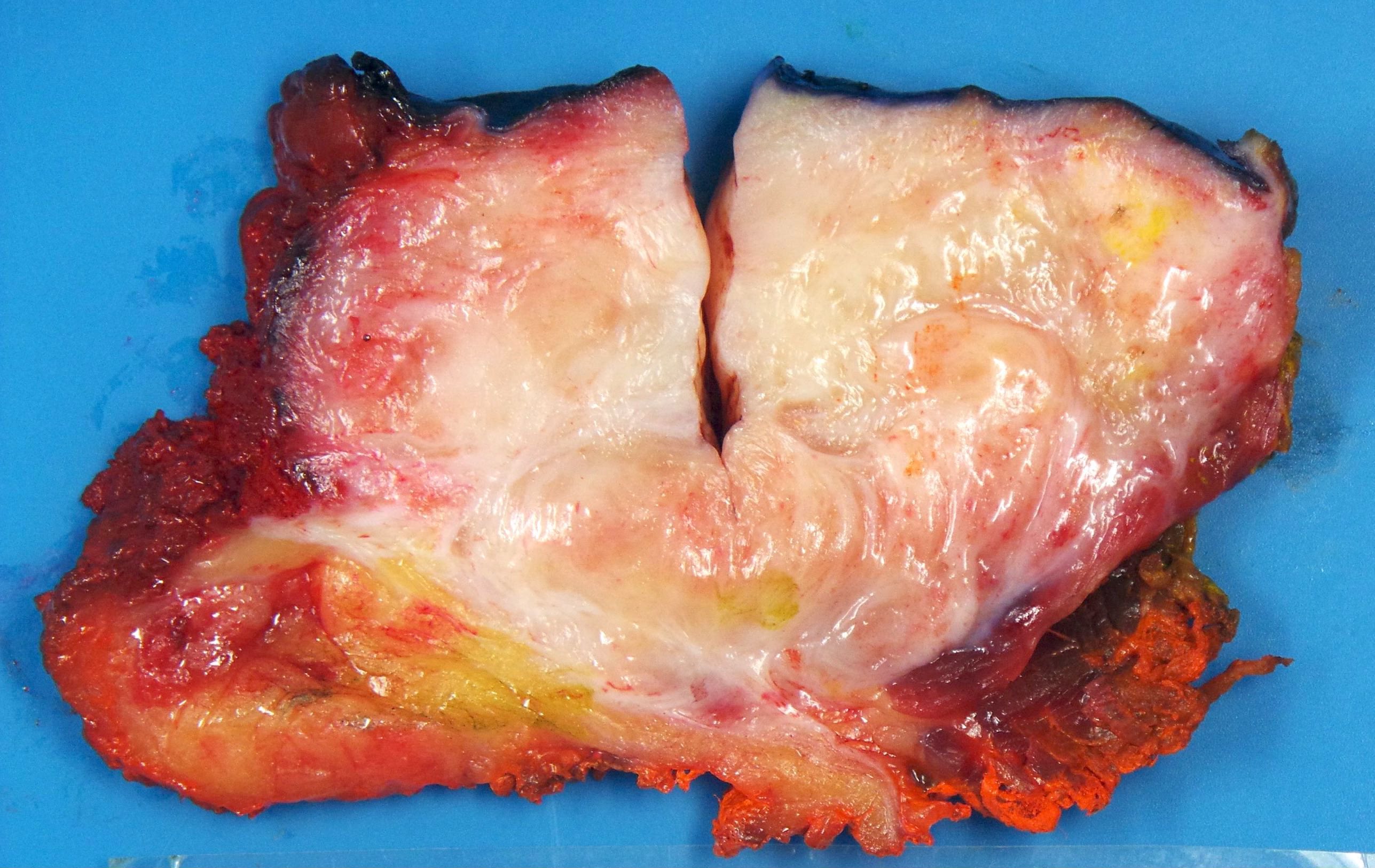
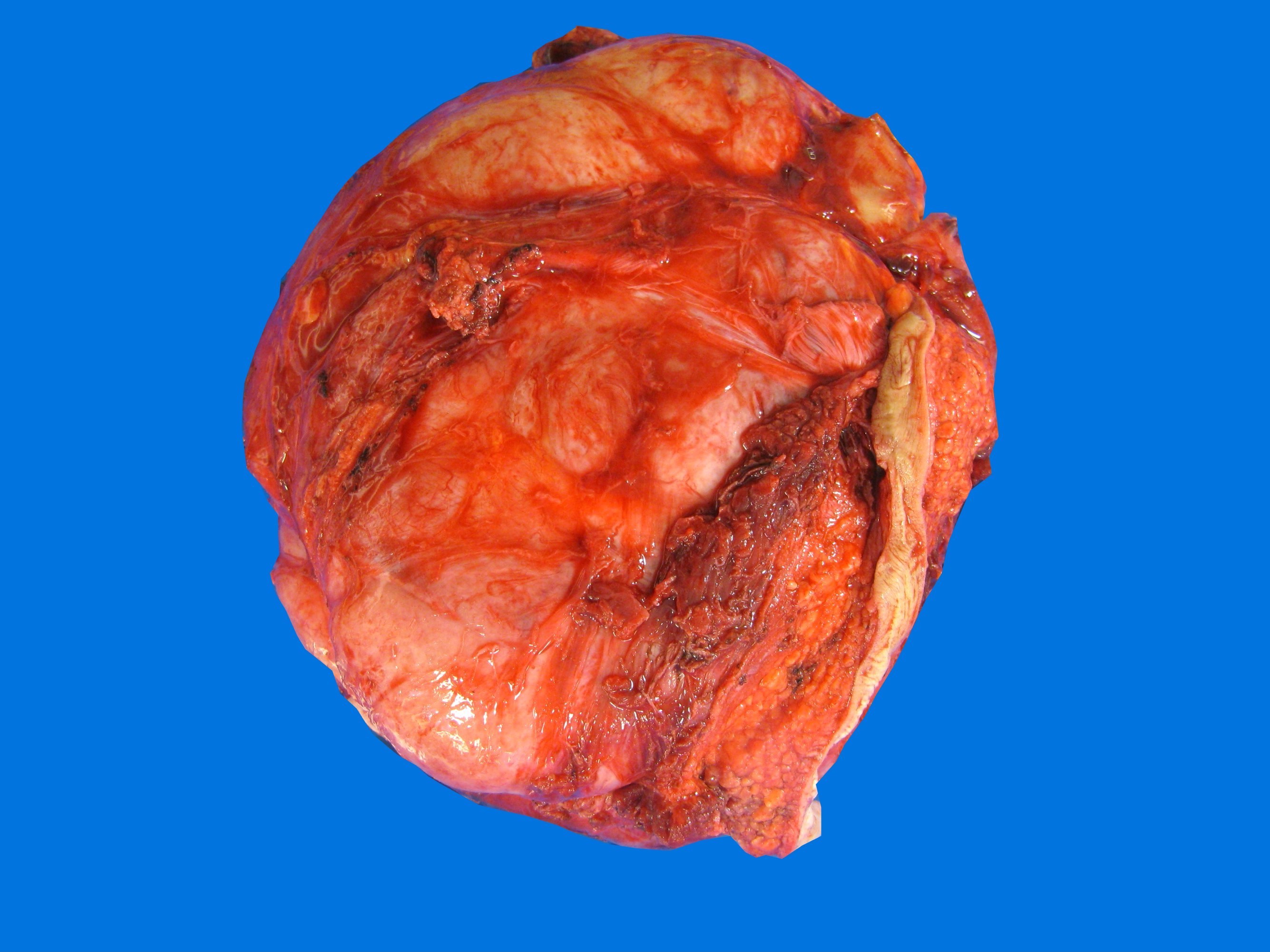
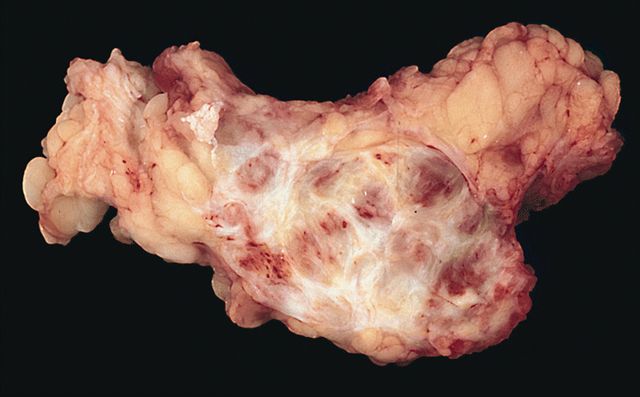
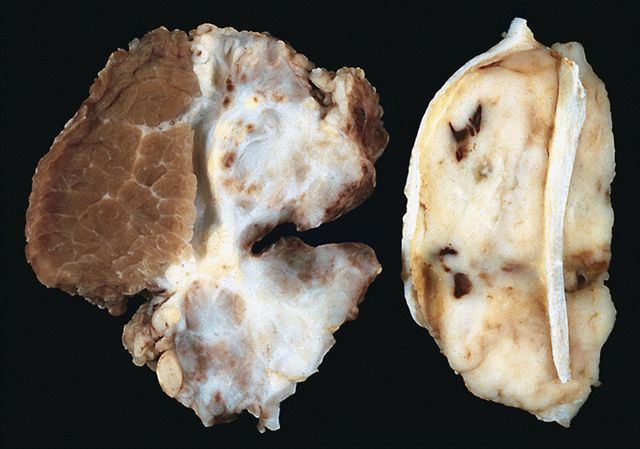
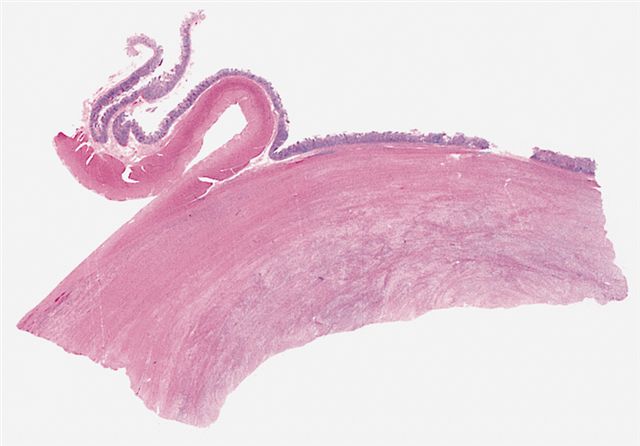
Gross description
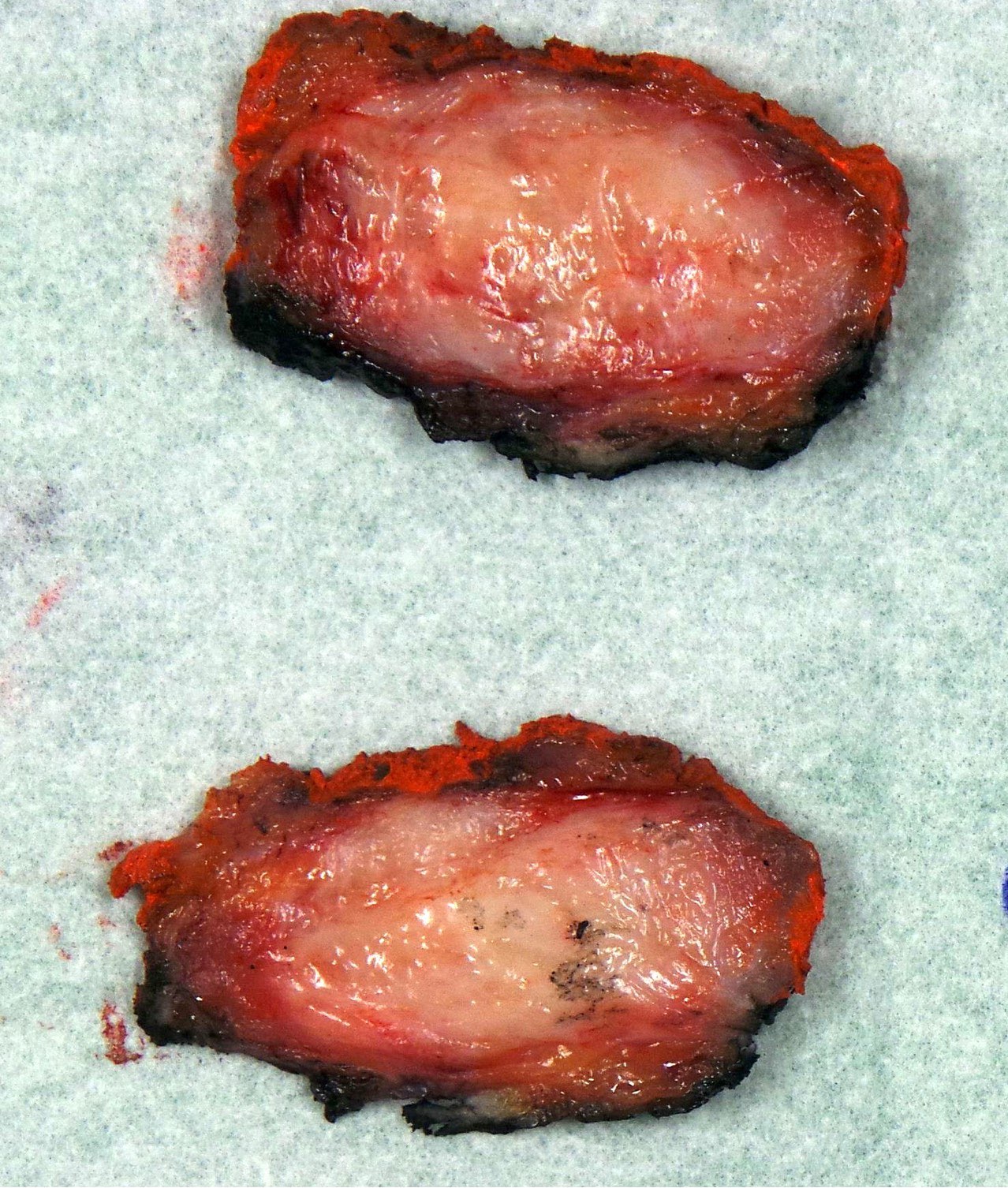
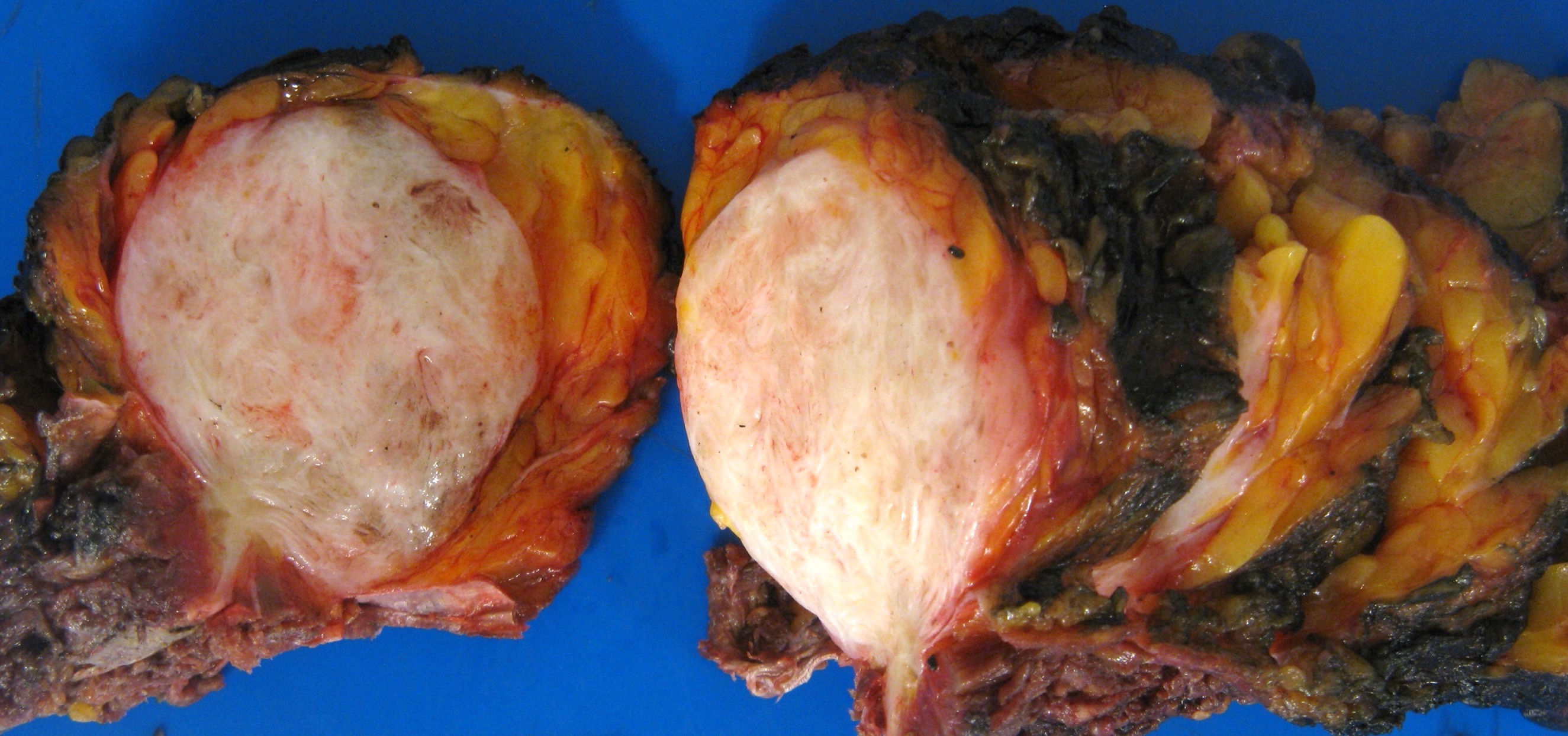
- Typically 5 - 10 cm; may be poorly defined or well circumscribed
- Firm, glistening white, gritty and coarsely trabeculated cut surface resembling scar tissue
Gross images
Contributed by Farres Obeidin, M.D. and AFIP images
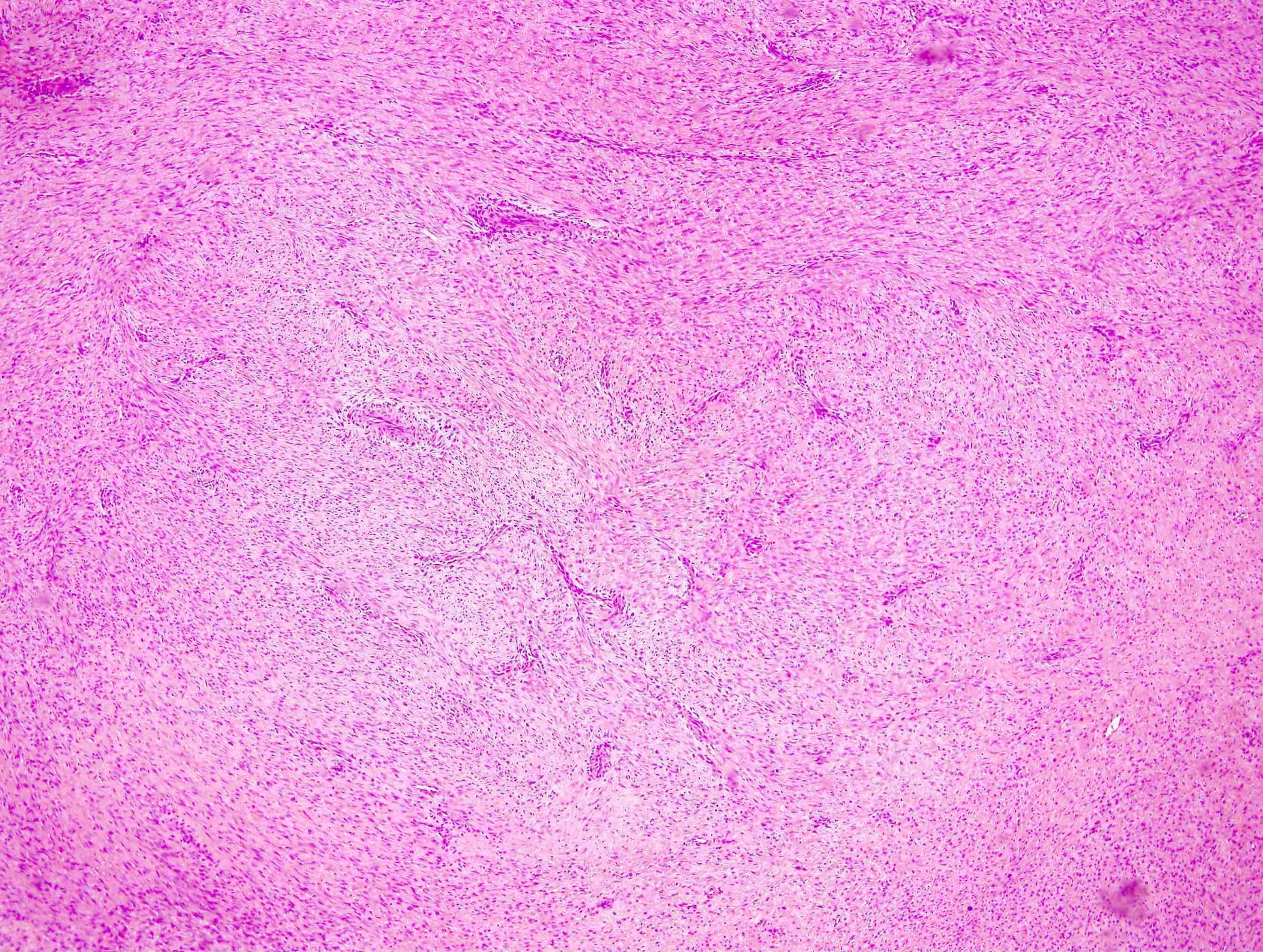
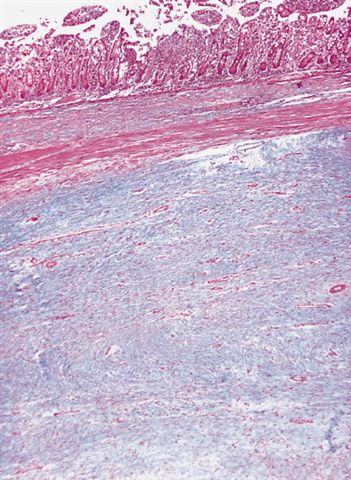
Microscopic (histologic) description
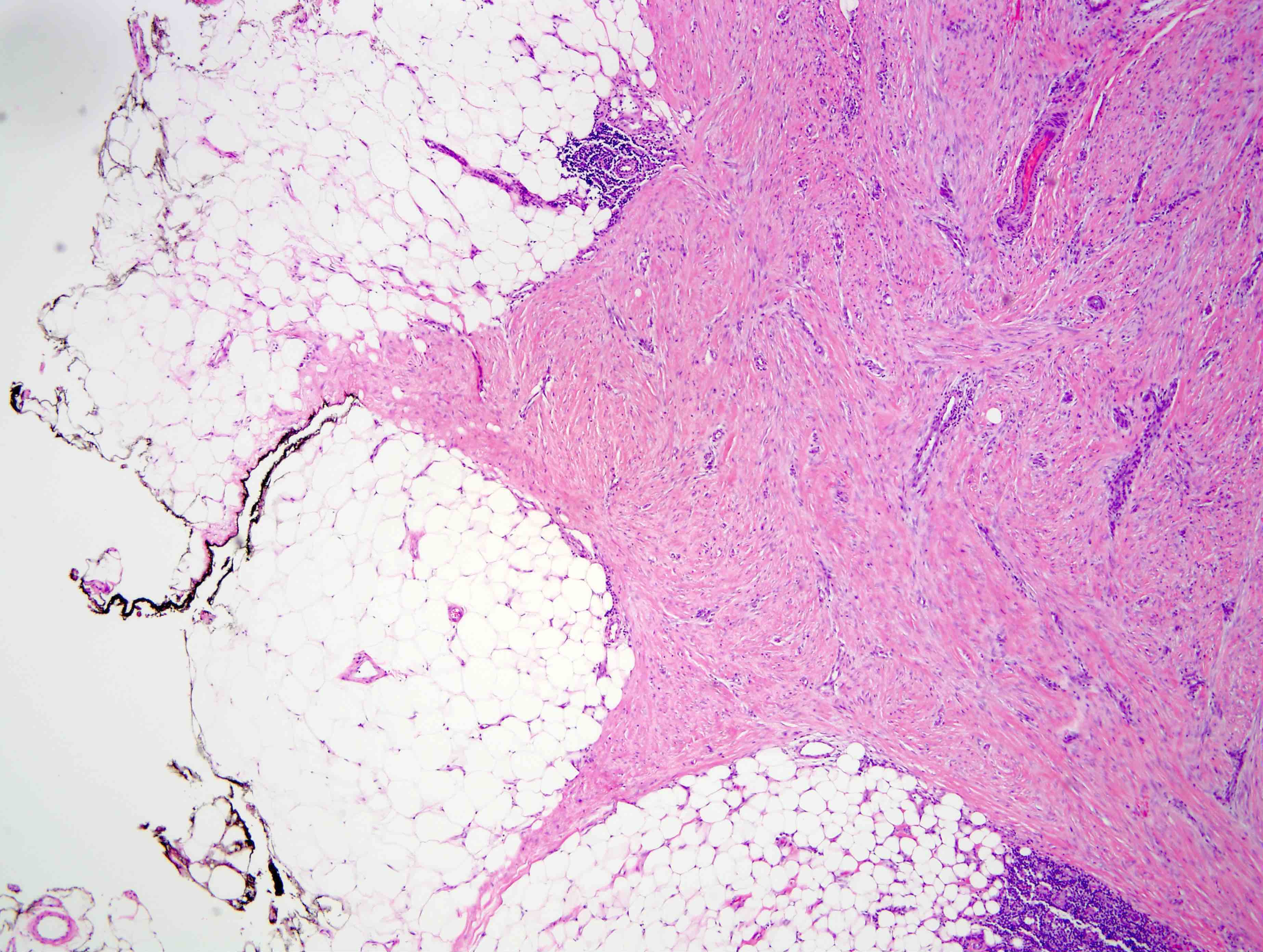
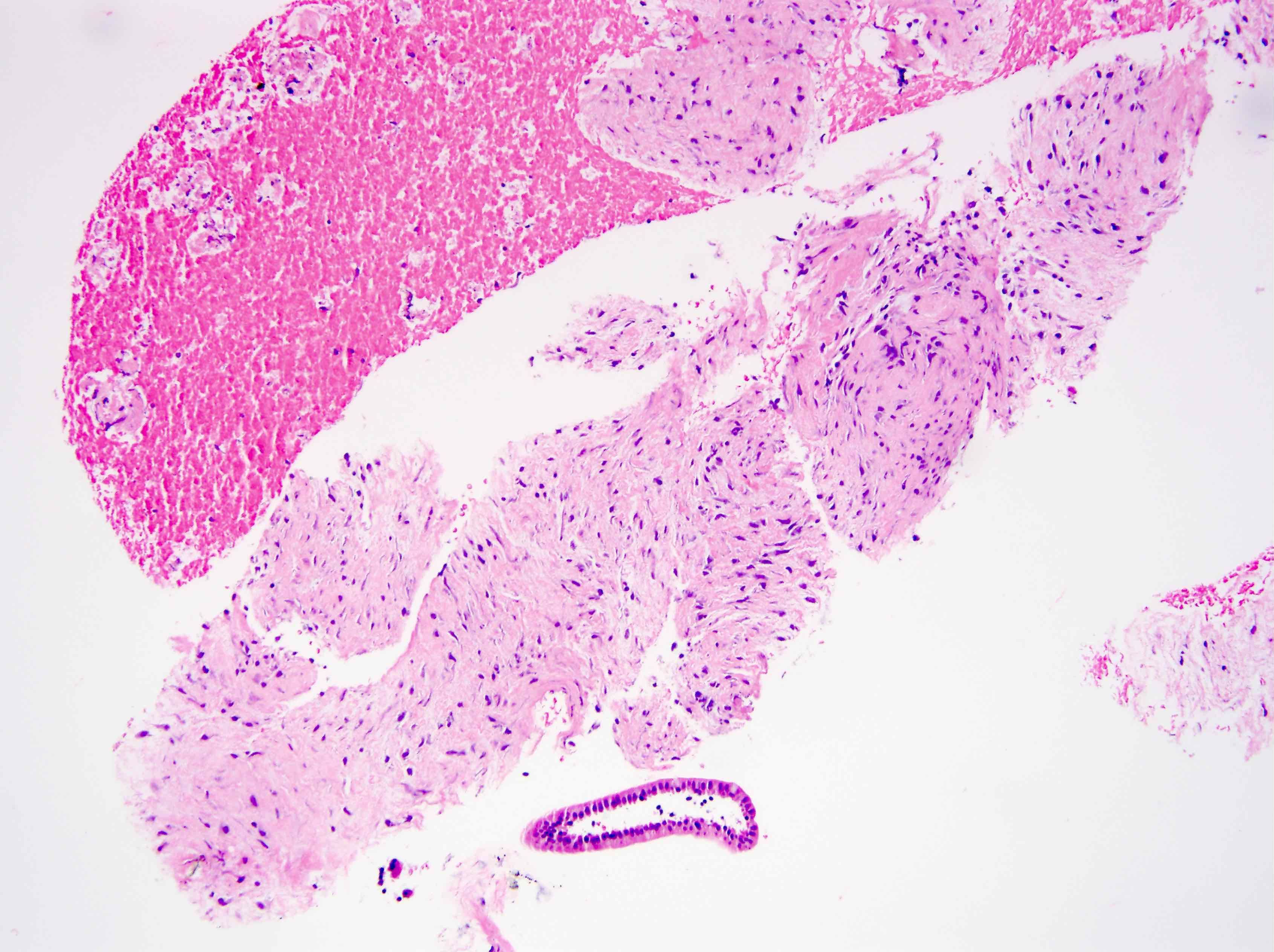
- Typically poorly defined borders
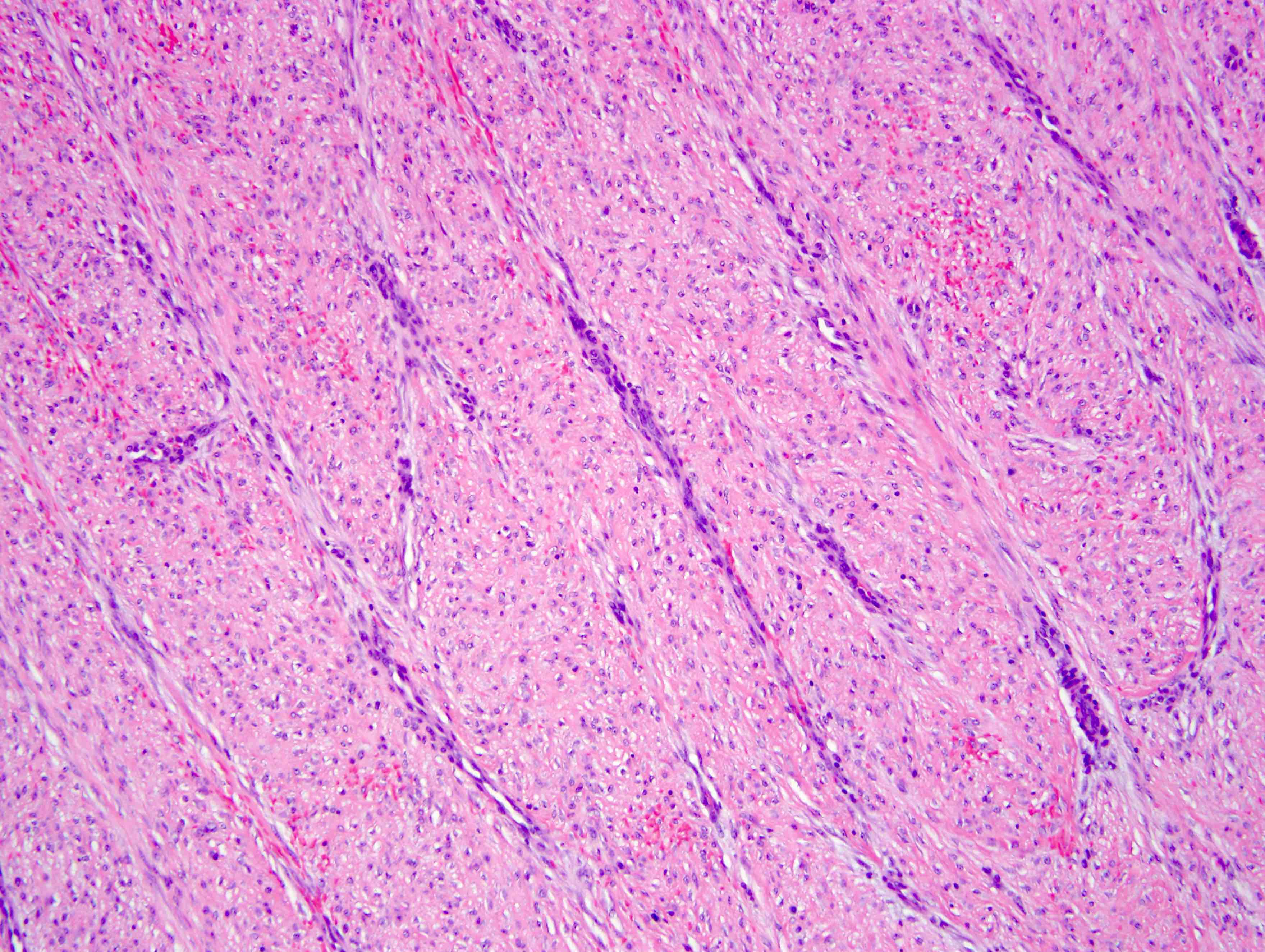
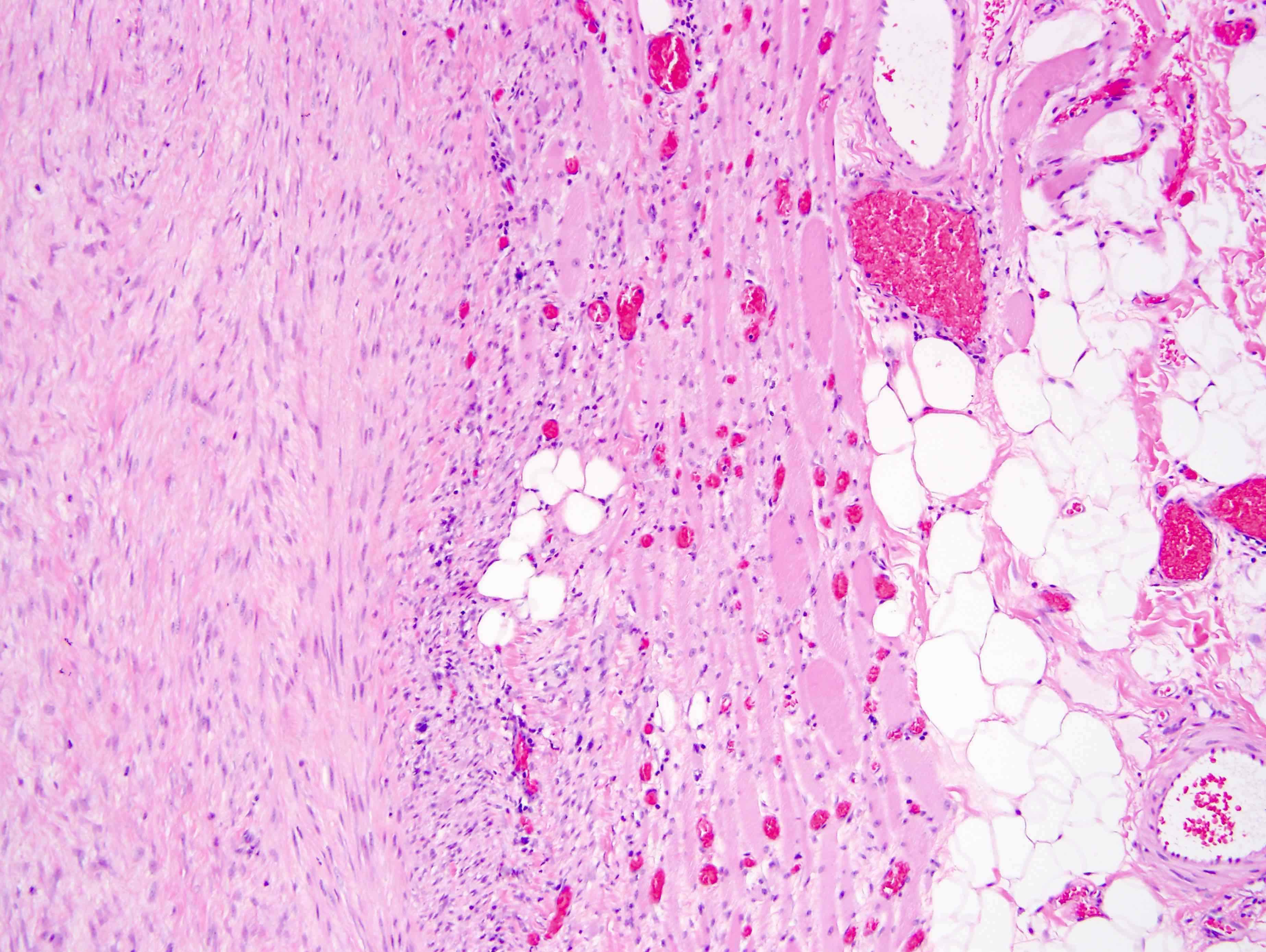
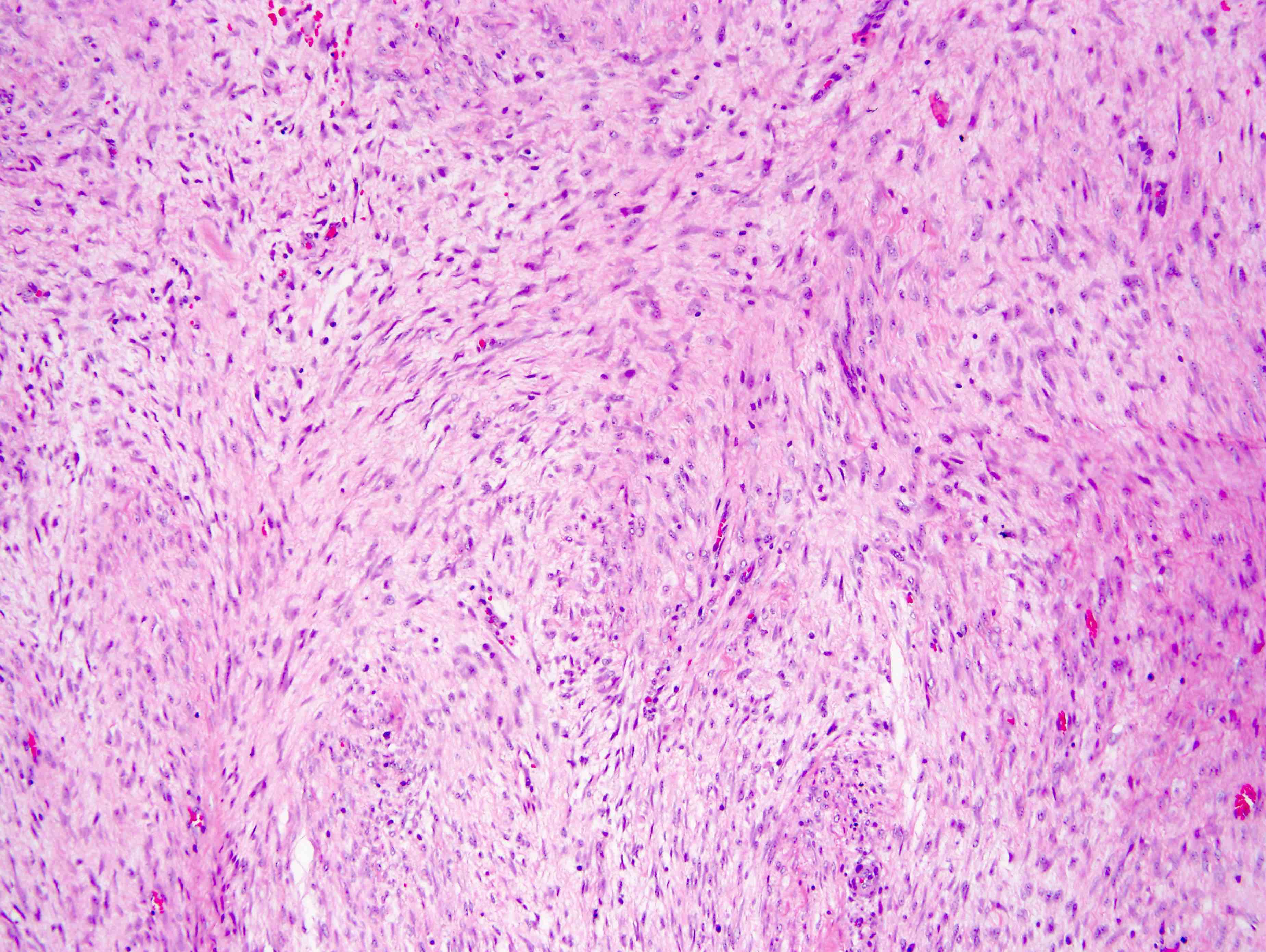
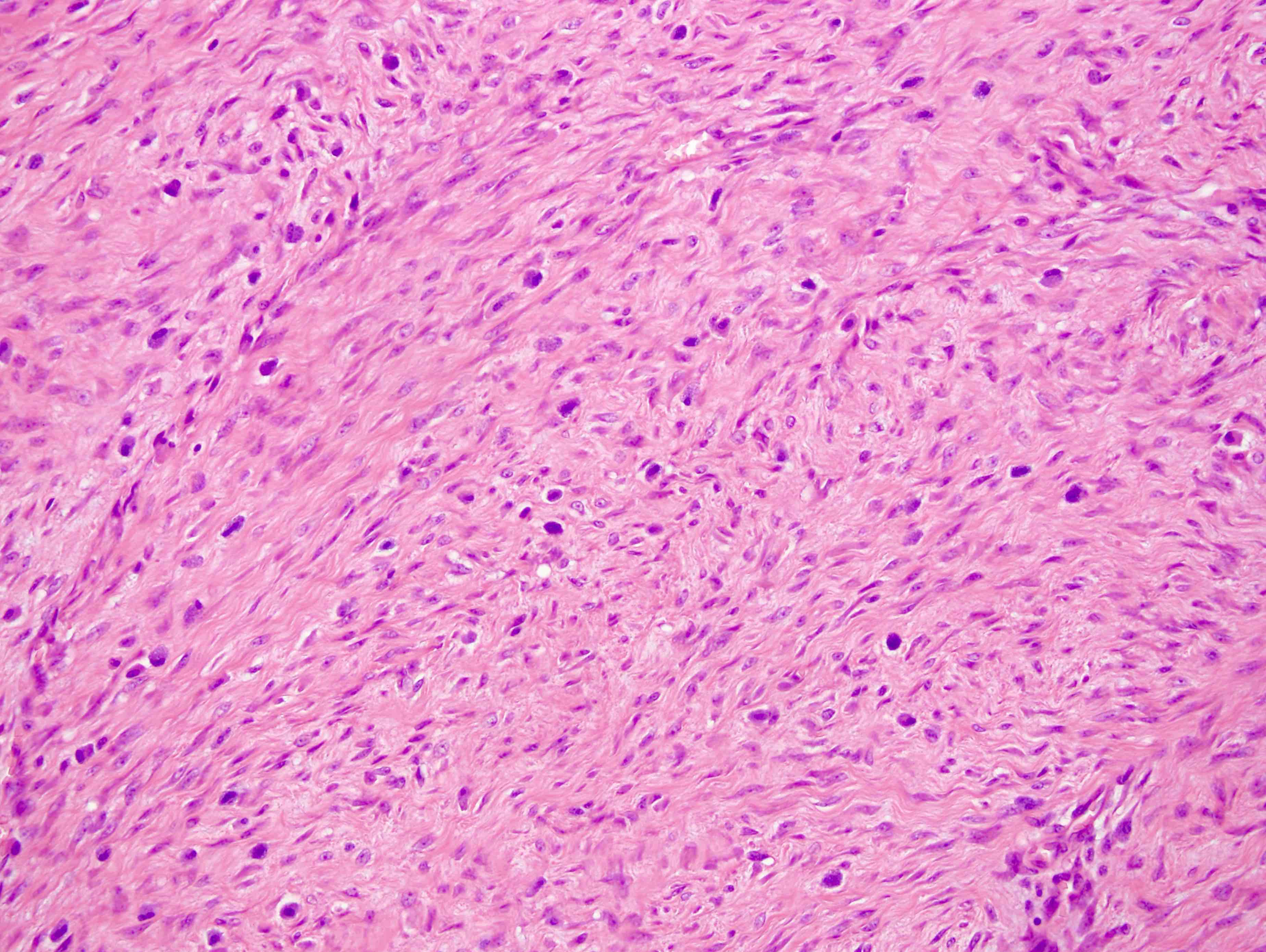
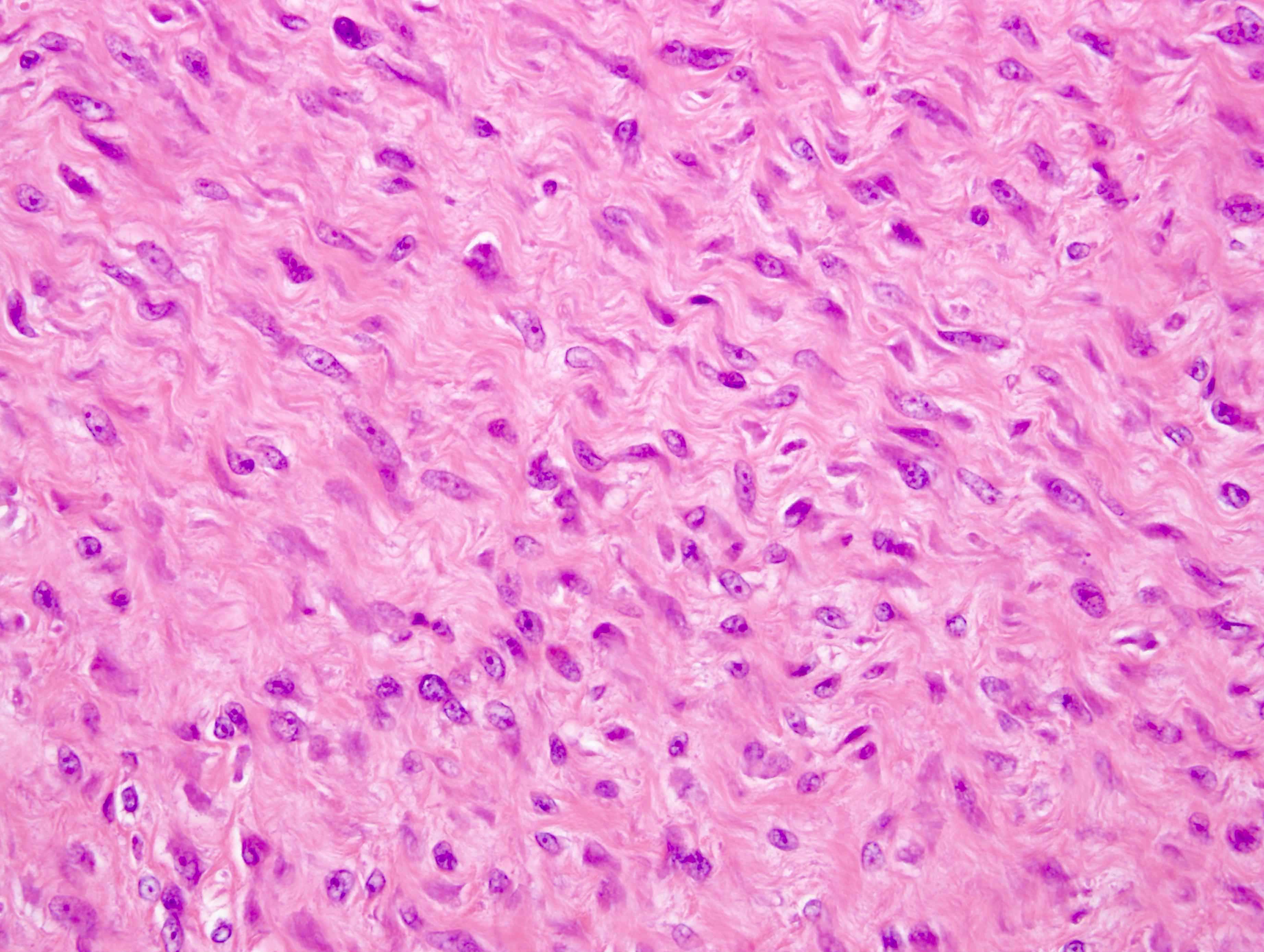
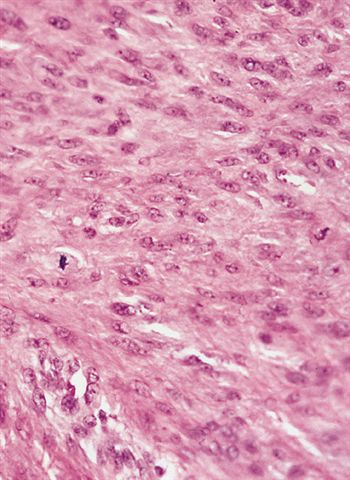
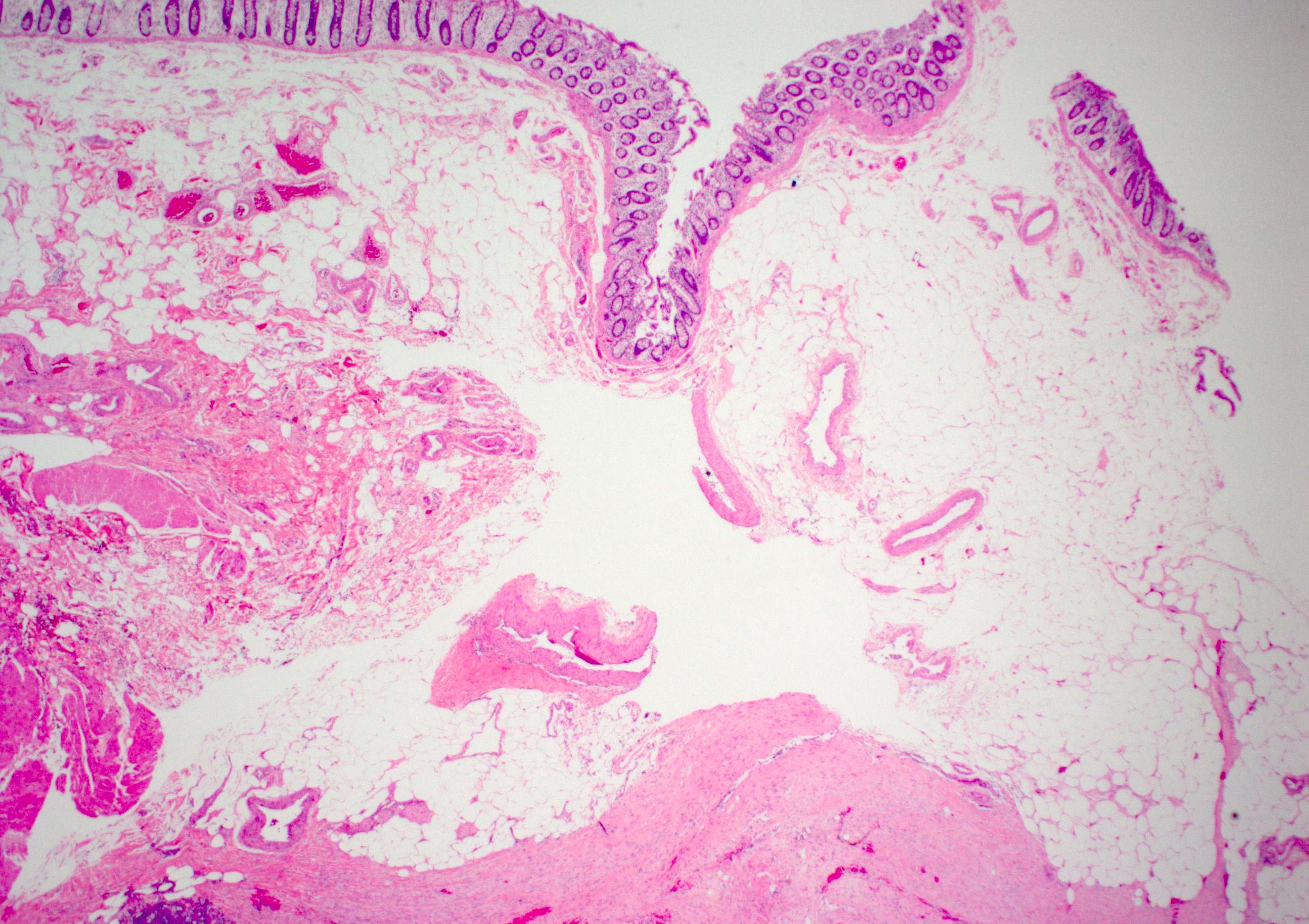
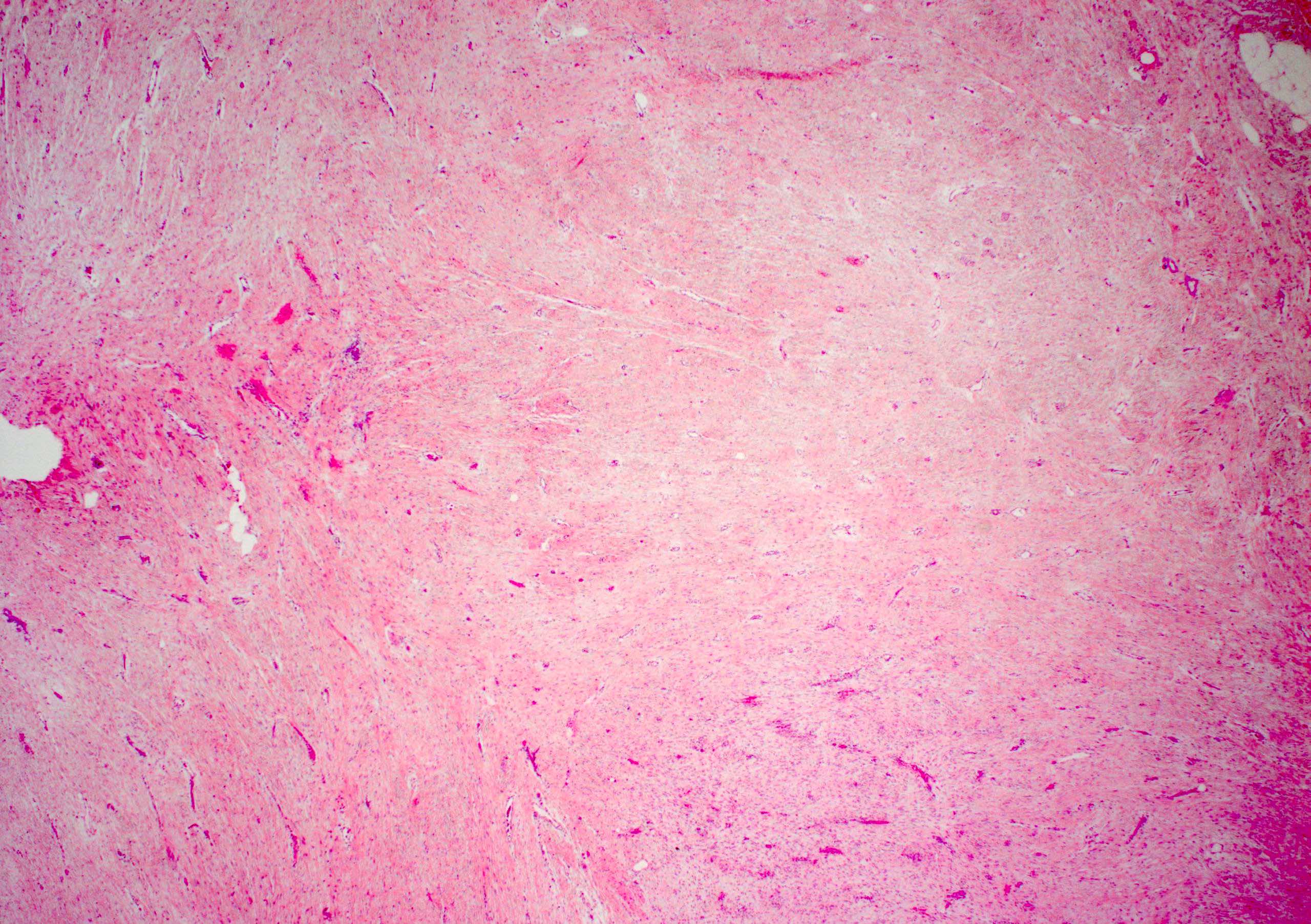
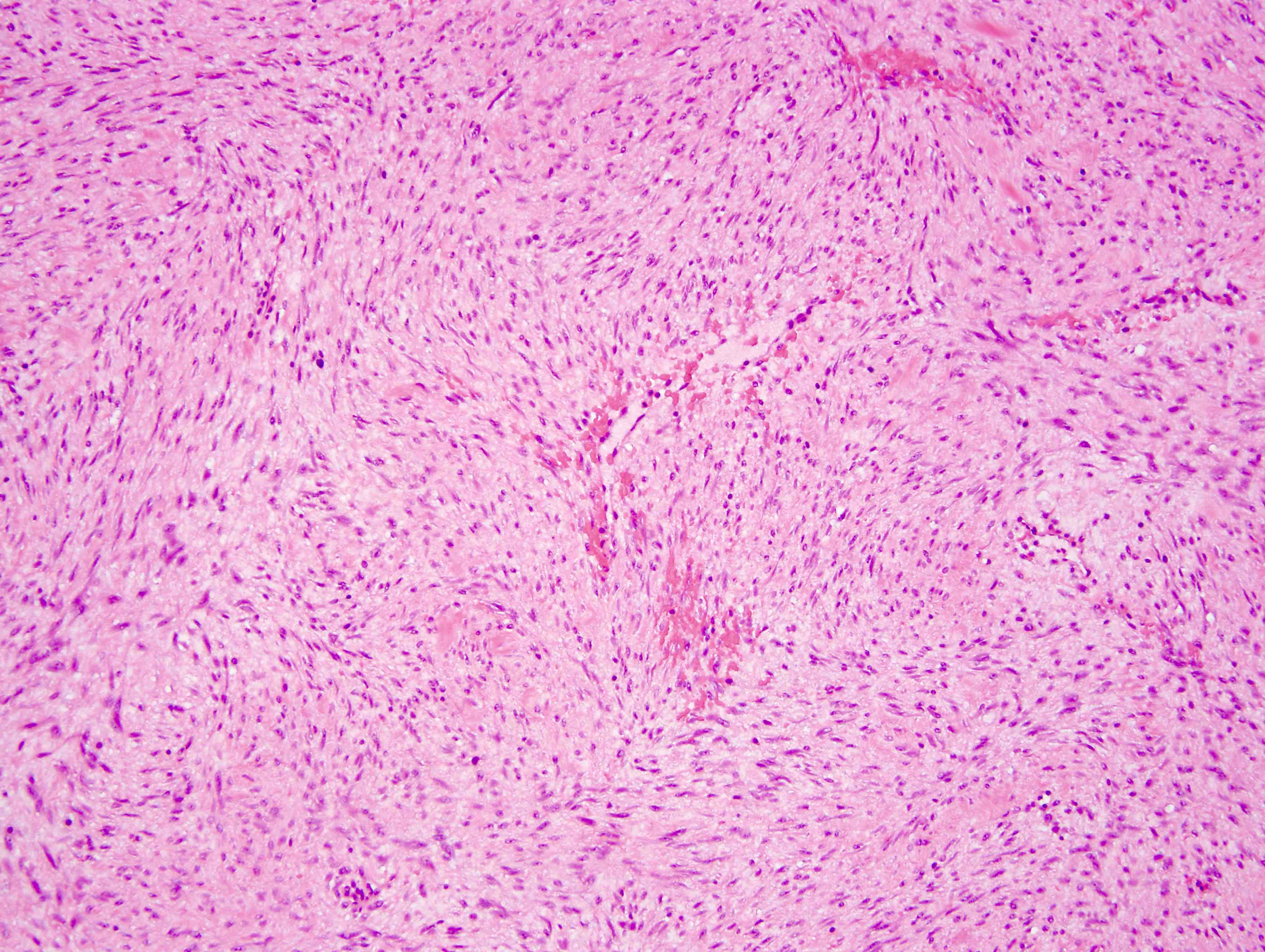
- Conventional pattern (Am J Clin Pathol 2016;145:332):
- Most common pattern; present at least focally in almost all tumors
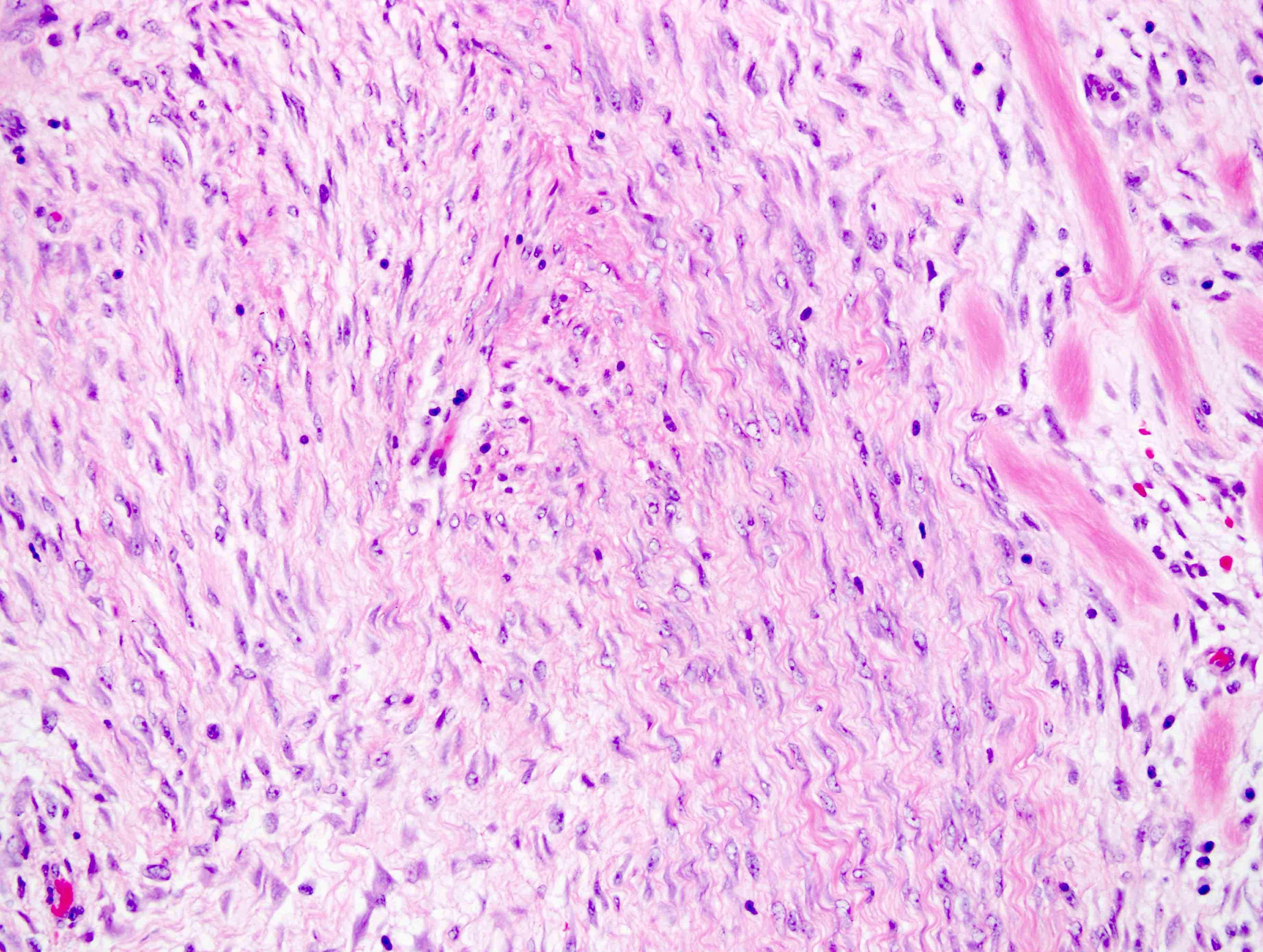
- Long sweeping fascicles with elongated, slender, spindled cells of uniform appearance and pale cytoplasm set in a collagenous stroma
- No nuclear hyperchromasia, minimal cytologic atypia and variable mitotic rate (typically low but may be focally increased)
- Thin walled and prominent blood vessels with perivascular edema
- Vascular microhemorrhages may be seen
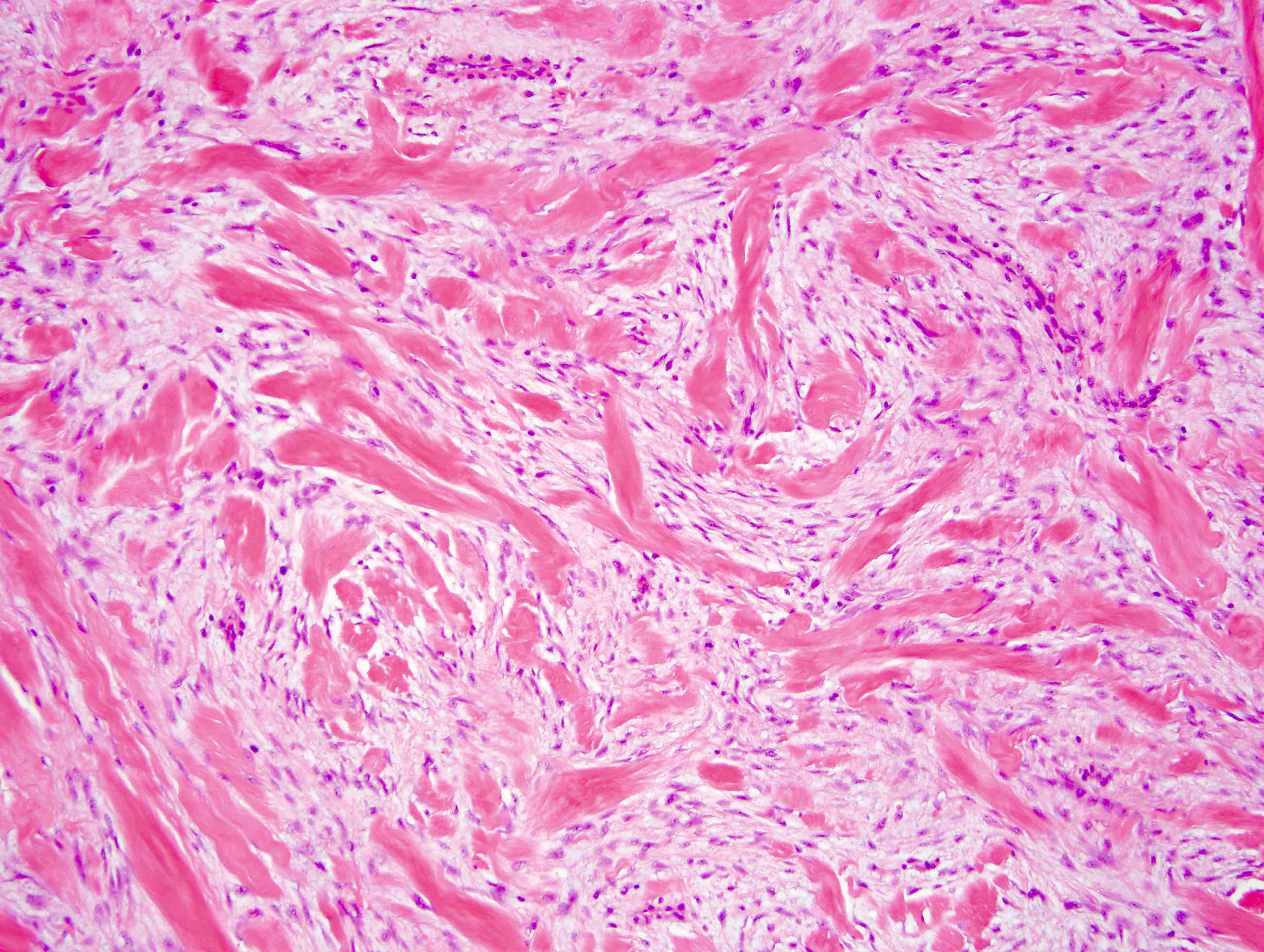
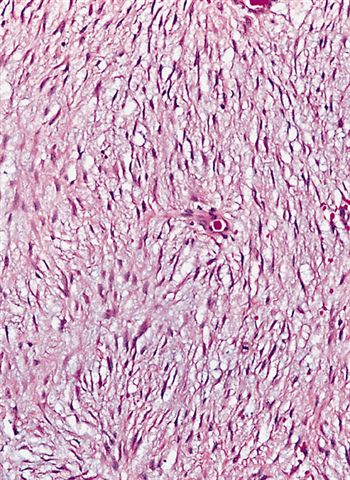
- Hypocellular / hyalinized pattern:
- Second most common pattern
- More hypocellular, prominent stromal hyalinization, compressed and thin walled vessels
- Staghorn vessel pattern:
- ~20% of cases
- Prominent, dilated, branching blood vessels
- Myxoid pattern:
- ~15% of cases
- Myxoid stroma with less discrete fascicles; lacks the typical thin walled blood vessels
- Keloidal pattern:
- ~15% of cases
- Variably sized bands of keloidal collagen fibers throughout the tumor; fascicles are disrupted and typical vascular pattern is lacking
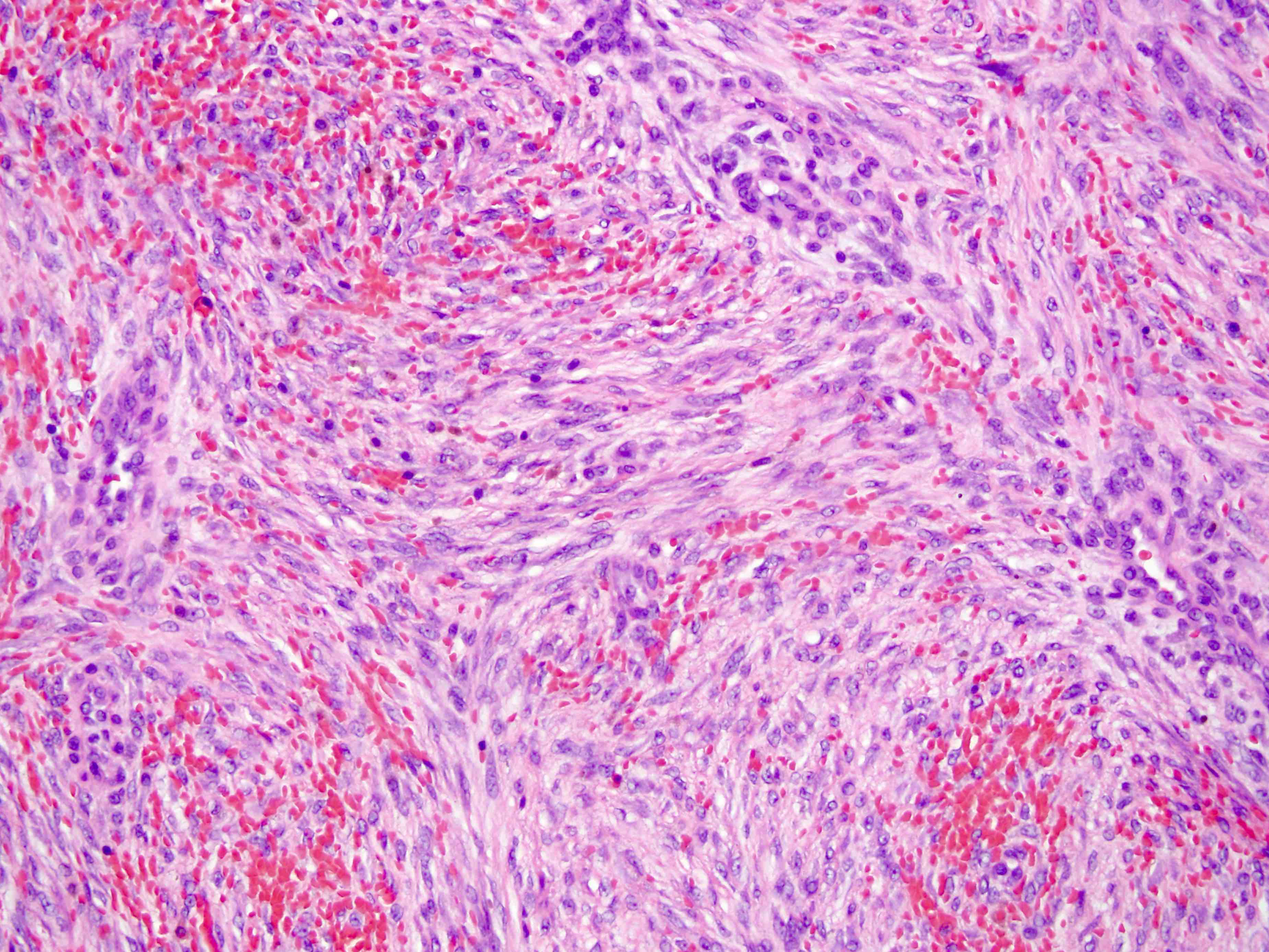
- Nodular fasciitis-like pattern:
- ~10% of cases
- Spindle to stellate cells in a loose tissue culture arrangement with variable amounts of stromal hemorrhage
- Hypercellular pattern:
- ~5% of cases
- Resembles conventional pattern but with increased cellular density and frequently overlapping nuclei
- Without cytologic atypia or nuclear hyperchromasia
Microscopic (histologic) images
Contributed by Farres Obeidin, M.D., Raul S. Gonzalez, M.D. and AFIP images
Cytology description
- Bland spindle cells with long, fusiform nuclei and metachromatic matrix material
- Tumor cells are individual or as fragments within matrix (Cancer 2007;111:166)
- Fine needle aspiration is fairly reliable for diagnosis but core needle biopsy is better (Acta Orthop 2006;77:926)
- May have long fascicular arrangement of spindle cells (Diagn Cytopathol 2012;40:45)
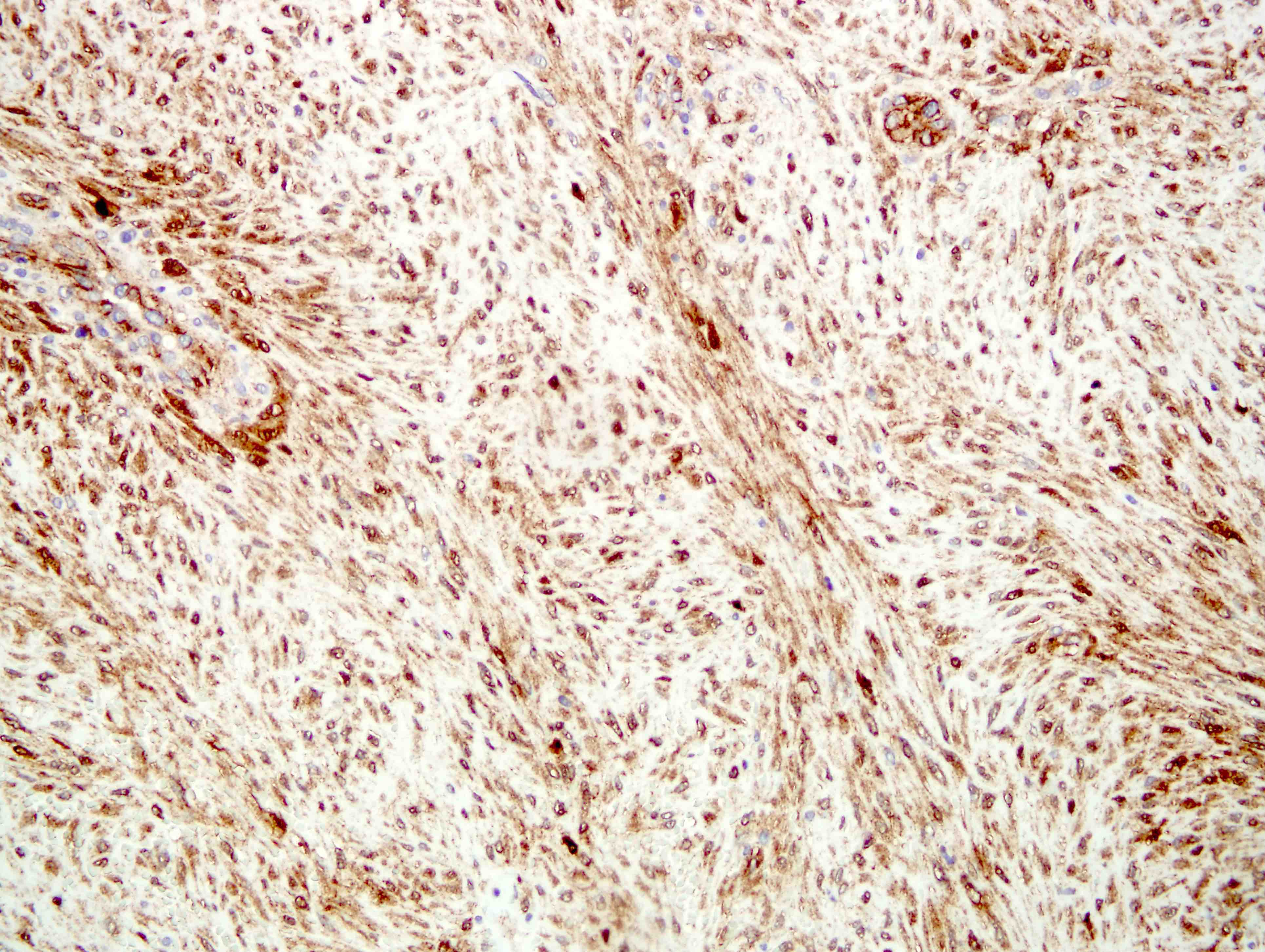
Positive stains
- Variable positivity for SMA and MSA; rarely focal desmin (Arch Pathol Lab Med 2008;132:476)
- Beta catenin (70 - 98%; higher in mesenteric / FAP associated tumors) (Histopathology 2013;62:294, Am J Pathol 2008;173:1518)
- Cyclin D1 (71 - 75%) (Arch Pathol Lab Med 2006;130:1503)
- Calretinin (75%) (Am J Surg Pathol 2012;36:1404)
- Sex hormones may show variable staining: ER (8%), PR (0 - 33%), AR (6 - 53%) (J Clin Pathol 2005;58:1152, Tohoku J Exp Med 2006;210:189)
- Vimentin (100%)
- Cathepsin D (100%; limited utility due to positive staining in normal stromal cells and other soft tissue tumors) (J Clin Pathol 2005;58:1152)
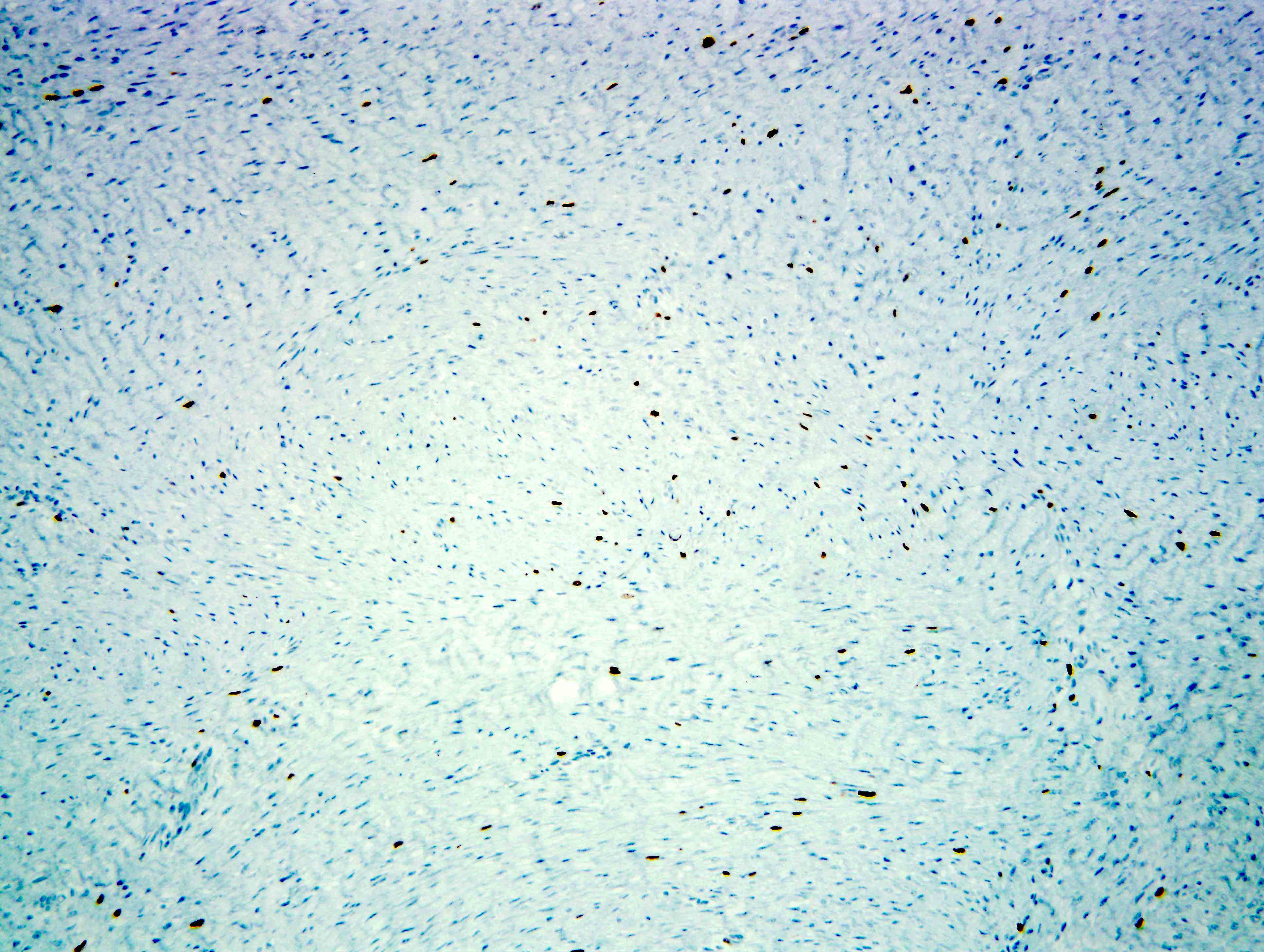
Negative stains
- CD34, S100, cytokeratins (Arch Pathol Lab Med 2008;132:476)
- DOG1, c-kit (Am J Pathol 2004;165:107, Am J Clin Pathol 2003;119:339)
- ALK1 (small sample size) (Arch Pathol Lab Med 2006;130:1503)
- STAT6 (found in ~8%) (Am J Clin Pathol 2015;143:672)
- MUC4 (Am J Surg Pathol 2011;35:733)
- Ki67 (low, ~1 - 3%) (Diagn Pathol 2013;8:50)
Electron microscopy description
- Fibroblastic and myofibroblastic features, including intrareticular collagen fibers, thin filament bundles, cytoplasmic dense bodies
Molecular / cytogenetics description
- CTNNB1 mutations reported in ~90% of cases, usually in exon 3; most common mutations are T41A, S45F and S45P (Virchows Arch 2015;467:203)
- FAP patients have germline mutations in APC leading to deregulation of the Wnt / beta catenin pathway (Eur J Surg Oncol 2009;35:3)
Sample pathology report
- Abdominal wall, mass, resection:
- Desmoid type fibromatosis (see comment)
- Margins of resection are negative, with tumor closest at 1 cm from the inked margin.
- Comment: Microscopic sections show a proliferation of bland spindle cells with thin blood vessels and focal areas of hemorrhage infiltrating into surrounding skeletal muscle and adipose tissue. A beta catenin immunostain shows nuclear positivity in the majority of cells, supporting the diagnosis of desmoid type fibromatosis.
Differential diagnosis
- Scar tissue:
- Very hypocellular with a noninfiltrative growth pattern
- Typically have a history of trauma or surgical procedure at the site
- Beta catenin-
- Gardner fibroma:
- Smaller, more hypocellular lesion with dense collagen bundles and clefting artifact
- Most commonly associated with Gardner syndrome and is beta catenin+
- Palmar / plantar fibromatosis:
- Occurs on hands or feet
- Beta catenin more focal and CTNNB1 / APC gene mutations not found
- Nodular fasciitis:
- Nodular architecture with areas of more loosely arranged, stellate and tissue culture-like cells
- Mitotic activity is more common
- Beta catenin- and shows a USP6 gene rearrangement
- Proliferative fasciitis / myositis:
- Similar features to nodular fasciitis but also has large ganglion-like cells not seen in fibromatosis
- Myofibroma / myofibromatosis:
- Has distinct myoid nodules and is typically diffuse for SMA
- May have prominent hemangiopericytic vasculature
- Beta catenin-
- Calcifying fibrous pseudotumor:
- Densely collagenized, hypocellular lesion with psammomatous calcifications and variable lymphoplasmacytic infiltrate
- Beta catenin-
- Sclerosing mesenteritis / idiopathic retroperitoneal fibrosis:
- Nonneoplastic with variable histology based on the age of the lesion, from fasciitis-like to densely sclerotic
- Beta catenin-
- Solitary fibrous tumor:
- Classic hemangiopericytic vasculature with a ropey collagenous background
- May be beta catenin+ but is typically diffuse for CD34 and STAT6
- Gastrointestinal stromal tumor (GIST):
- Leiomyoma:
- Composed of smooth muscle cells
- SMA+, desmin+, calponin+, h-caldesmon+
- Nerve sheath tumors:
- Fibrosarcoma:
- Diagnosis of exclusion
- Typically more cellular with monotonous, hyperchromatic cells, mitotic activity and herringbone pattern
- Beta catenin-
- Inflammatory myofibroblastic tumor:
- Usually has background inflammation composed of plasma cells and lymphocytes
- ~50% have ALK1 gene rearrangements and beta catenin-
- Low grade myofibroblastic sarcoma:
- Very infiltrative lesion with at least focal atypia
- Has a predilection for the head and neck
- SMA+ and beta catenin usually negative
- Low grade fibromyxoid sarcoma:
- Alternating zones of hypocellular collagenous and more cellular myxoid tissue; prominent arcades of vessels in the myxoid areas
- MUC4+ and has a characteristic FUS-CREB3L2 translocation
- Beta catenin-
Board review style question #1
A mass was excised from the abdominal wall of a 28 year old woman. The histology is shown above. Stains were performed and the lesion shows nuclear positivity for beta catenin. Which of the following is true about this lesion?
- It harbors an ALK1 gene rearrangement
- It has high potential for recurrence if incompletely excised
- It has metastatic potential
- The lesional cells arose from the interstitial cells of Cajal
Board review style answer #1
B. It has high potential for recurrence if incompletely excised. This is a desmoid type fibromatosis. They don't have metastatic potential but have a high change for recurrence, particularly in the abdomen. GIST cells arise from the interstitial cells of Cajal in the muscularis propria of the bowel and inflammatory myofibroblastic tumors may have ALK1 gene rearrangements.
Comment Here
Reference: Fibromatosis-desmoid
Comment Here
Reference: Fibromatosis-desmoid
Board review style question #2
Which of the following genetic syndromes is associated with an increased chance of developing desmoid type fibromatosis?
- Gardner syndrome
- Li-Fraumeni syndrome
- Maffucci syndrome
- Neurofibromatosis
Board review style answer #2
A. Gardner syndrome is an expansion of familial adenomatous polyposis (FAP) that includes additional features such as desmoid type fibromatosis, Gardner fibromas and rhabdomyosarcomas.
Comment Here
Reference: Fibromatosis-desmoid
Comment Here
Reference: Fibromatosis-desmoid