Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Joldoshova A, Jain S. Adenoma with invasive carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumorcarcinomaarising.html. Accessed March 31st, 2025.
Definition / general
- Malignant colorectal polyps are colorectal adenomas containing invasive adenocarcinoma that extend through the muscularis mucosae into the submucosa and do not extend into the muscularis propria (Am J Gastroenterol 2020;115:1751)
- They are classified as pT1 in the current TNM classification system in the 8th edition of AJCC Cancer Staging Manual (CA Cancer J Clin 2017;67:93)
Essential features
- Colorectal adenoma with invasive carcinoma represents the earliest form of carcinoma because submucosal invasion leads to further risk for lymphatic and vascular metastasis even if the polyp / tumor has been completely resected (Gastroenterology 2004;127:385)
- Colorectal adenomas with intramucosal carcinomas limited to the surface epithelium, lamina propria or muscularis mucosae are staged as carcinoma in situ (Tis) and should be excluded from this category (Am J Gastroenterol 2020;115:1751)
- On a limited biopsy specimen when a clinical mass lesion is identified, we can diagnose invasive carcinoma in a colorectal adenoma if we see marked desmoplasia, infiltrative pattern, poorly differentiated morphology or lymphovascular space invasion (LVI) (Gastroenterology 1995;108:1657)
Terminology
- Also called malignant epithelial / colorectal polyp, cancerous polyps
ICD coding
- ICD-10: C18.9 - malignant neoplasm of colon, unspecified
Epidemiology
- Prevalence of malignant polyps is between 0.2% and 12.0% (average: ~5.0%) in endoscopic polypectomies (Endoscopy 1995;27:153)
- Incidence is increasing due to more efficacious colonoscopy screening programs, which are fundamental in the prevention of colorectal cancer and the treatment of some advanced polyps (World J Gastroenterol 2010;16:3103)
- Malignant polyps are also classified based on the depth of invasion, which is the most important feature; in 1985, Haggitt et al. put forward a classification system for pedunculated and sessile polyps based on the depth of invasion of adenocarcinoma (Gastroenterology 1985;89:328)
- Risk factors for finding invasive carcinoma in colonic adenomas depends on
- Size of adenoma
- 1% risk if adenoma is < 1 cm; 10% risk if adenoma is 1 - 2 cm adenoma; 46% risk if adenoma is > 2 cm (Cancer Epidemiol Biomarkers Prev 2002;11:622)
- But infrequently, > 20 cm sessile adenomas can be benign
- Villous component in adenomatous polyp
- High grade dysplasia has a 35% risk of having carcinoma (versus low grade dysplasia, which has only a 6% risk)
- Age of the patient (older patients are at higher risk of having malignant transformation of their colorectal polyps)
- Size of adenoma
Sites
- Any part of the colon
Pathophysiology
- 95% of colorectal cancers arise from adenomatous polyps and follow adenoma - carcinoma sequence, which is an indolent process taking many years to progress after a stepwise collection of genetic alterations
- Sessile serrated adenoma is presumed to be the precursor of right sided adenocarcinomas with high levels of microsatellite instability (MSI-H) (Am J Gastroenterol 2012;107:1315)
Clinical features
- Asymptomatic to rectal bleeding
Diagnosis
- Colonoscopy with polypectomy and histopathological evaluation
Radiology description
- Polyps are divided endoscopically by their size into (Am J Gastroenterol 2018;113:303)
- Diminutive: < 5 mm
- Small: 6 - 9 mm (account for > 80% of polyps encountered during colonoscopy and have little overall risk for advanced histology [0.8 - 1.6%] and malignancy [0 - 0.1%])
- Large: ≥ 10 mm
- Colon polyps > 10 mm have a 22.9% likelihood of advanced pathology, while those lesions that are 30 mm carry a 60% risk of high risk pathology (Gastrointest Endosc 2012;75:1022)
Prognostic factors
- Risk factors leading to lymph node metastasis or local recurrence from residual malignancy following polypectomies are (Endoscopy 2013;45:827)
- Higher histologic grade (poorly differentiated or undifferentiated carcinoma, signet ring cell carcinoma)
- Tumor ≤ 1 mm from the resection margin
- Lymphatic / venous vessel involvement
- Histologic factors that have adverse prognostic factors for distant metastasis are as follows (Mod Pathol 2017;30:1299)
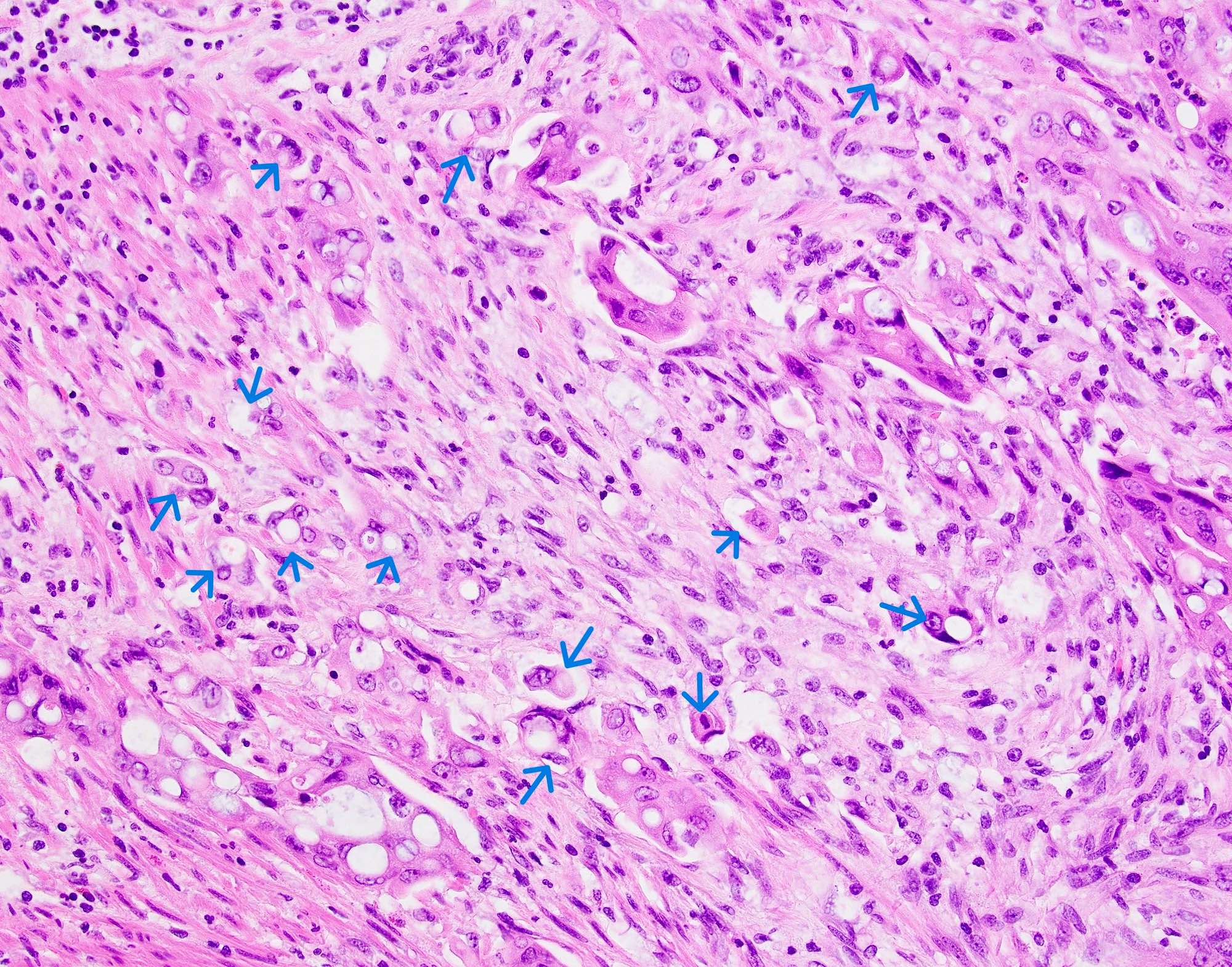
- Quantity of tumor budding (Hum Pathol 2016;47:4)
- Depth or area of submucosal invasion (submucosal invasion > 1 mm) (World J Surg 2018;42:2635)
- In en block resections of pedunculated or nonpedunculated colorectal lesions with submucosal invasion, the pathologists need to measure and report the depth of invasion, distance of the tumor from the deep and lateral surgical resection margins, in addition to prognostic histologic features, such as degree of differentiation, presence or absence of lymphovascular invasion and tumor budding
Case reports
- 43 year old woman with a 2 cm pedunculated polyp in the descending colon showing poorly differentiated adenocarcinoma, invading into the submucosa and demonstrating a lymphatic invasion (World J Surg Oncol 2021;19:269)
- 60 year old woman with rectal bleeding and a smooth 0.8 cm polyp in the cecum, with a pathology revealing an infiltrating adenocarcinoma arising within the hyperplastic polyp (Am J Gastroenterol 2005;100:S211)
- 88 year old man presented with ischemic colitis and incidental 8 mm ascending colon polyp with invasive adenocarcinoma was found in a single section from the ascending colon (Cureus 2021;13:e13928)
Treatment
- Polypectomy with complete removal of the malignant colorectal polyp; prevention of colorectal cancer progression is the primary goal
- Endoscopic resection can provide complete resection and obviate the higher morbidity, mortality and cost associated with alternative surgical treatment
- Complete excision with conventional endoscopic snare polypectomy for < 1 cm adenomas, which accounts for 80 - 90% of colorectal polyps (Am J Surg Pathol 2018;42:1083)
- Cold or hot snare polypectomy (with or without submucosal injection) to remove 10 - 19 mm nonpedunculated lesions
- Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) are used for > 20 mm nonpedunculated colorectal polyps but are usually only available in specialized centers
- Benefit of EMR and ESD is the ability to obtain 1 large piece of tissue, avoiding fragmented excision with clear margins and making it easier to orient, section and evaluate margins
- Colectomy with lymph node dissection is recommended for pedunculated polyps with any unfavorable histology, invasion into submucosa of bowel wall (Haggitt level 4) and any sessile / flat adenomas with invasion (Haggitt level 1 - 4)
- First follow up surveillance colonoscopy is 6 months for larger colorectal polyps ≥ 20 mm and the interval to the next colonoscopy is at 1 year and then 3 years (Am J Surg Pathol 2018;42:1083)
Gross description
- Grossly the polyps are described as polypoid (pedunculated or sessile) and nonpolypoid (flat or ulcerated) subtypes according to the Paris classification (Gastrointest Endosc 2003;58:S3)
Microscopic (histologic) description
- Adenocarcinoma can arise in adenomatous (tubular, tubulovillous or villous), serrated (sessile serrated adenoma / polyp or traditional serrated adenoma) or hamartomatous polyps
- For malignant pedunculated polyps, submucosal involvement by carcinoma has been divided into 4 Haggit levels (head, neck, stalk and beyond stalk in the submucosa) (Gastroenterology 1985;89:328)
- Level 1: invasion limited to head of pedunculated polyp
- Level 2: invasion extends to neck of pedunculated polyp
- Level 3: invasion extends to stalk of pedunculated polyp
- Note: levels 1 - 3 have the lowest risk of metastasis (< 1%)
- Level 4: invasion of submucosa in bowel wall proper (beyond the stalk of pedunculated polyp)
- Note: level 4 has the highest risk of lymph node metastasis, up to 27%
- For malignant sessile polyps, submucosal involvement by carcinoma has been divided into superficial, mid and deep levels (Kikuchi levels SM1, SM2 and SM3) (Am J Gastroenterol 2020;115:1751)
- SM1: invasion into upper third of submucosa
- SM2: invasion into middle third of submucosa
- Note: SM1 / SM2 are associated with low risk of metastasis; reported to be 0% for SM1 and ~10% for SM2
- SM3: invasion into lower third of submucosa; the greatest risk of lymphatic spread, up to 25%
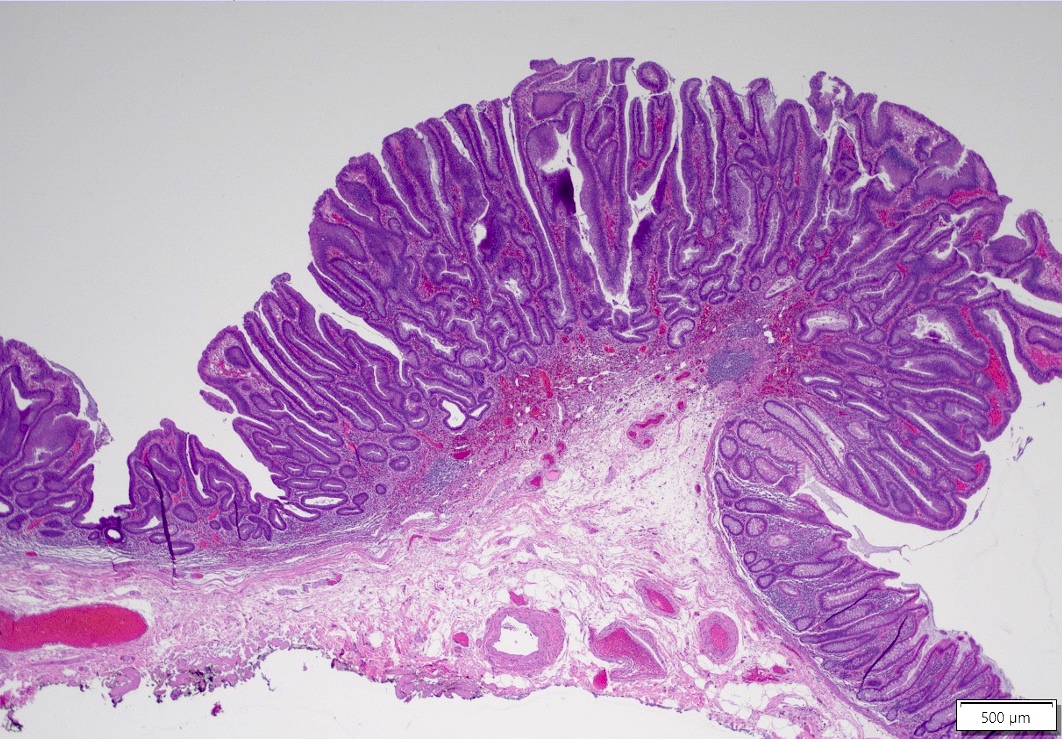
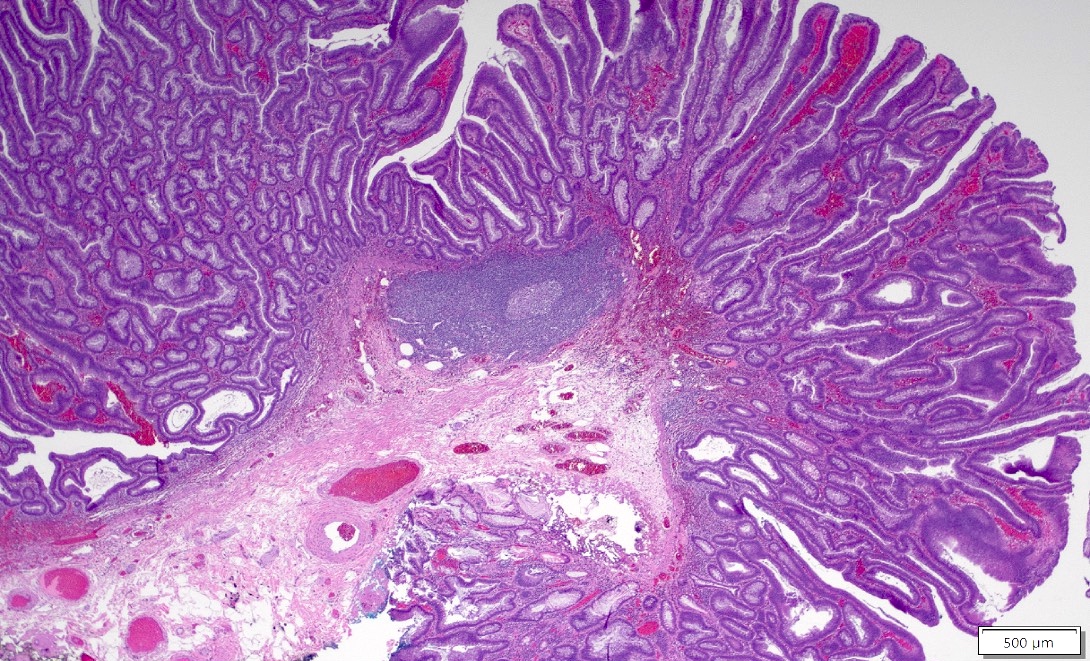
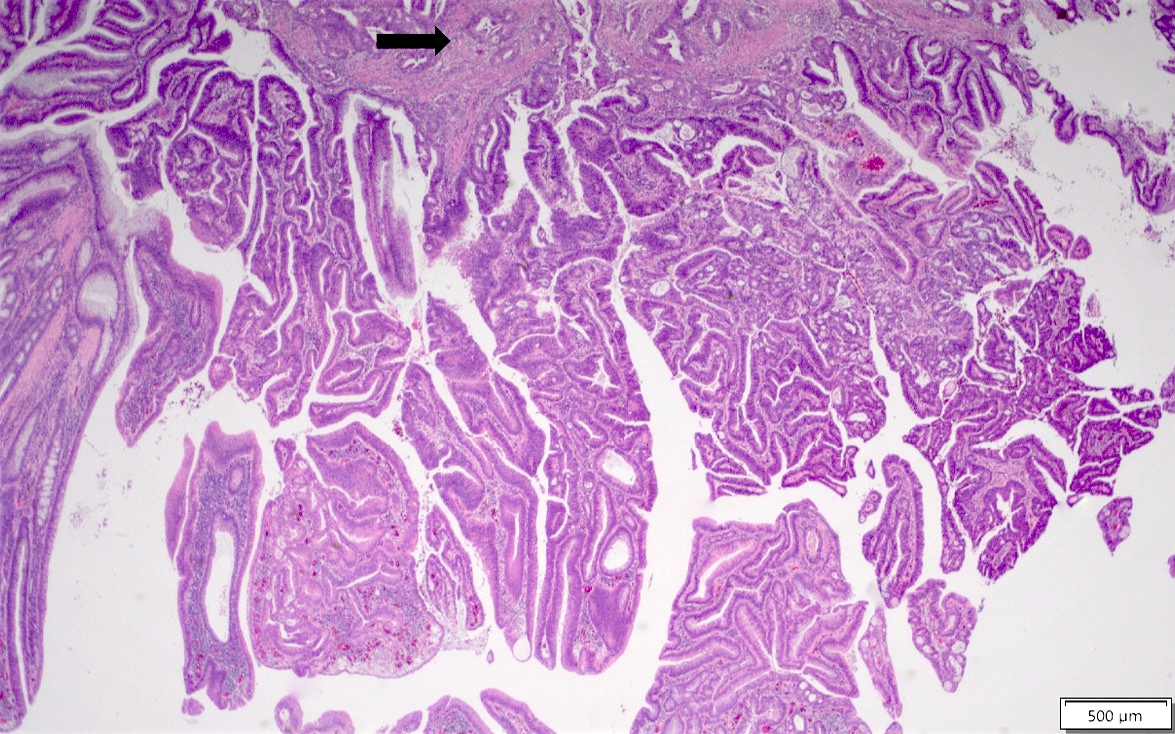
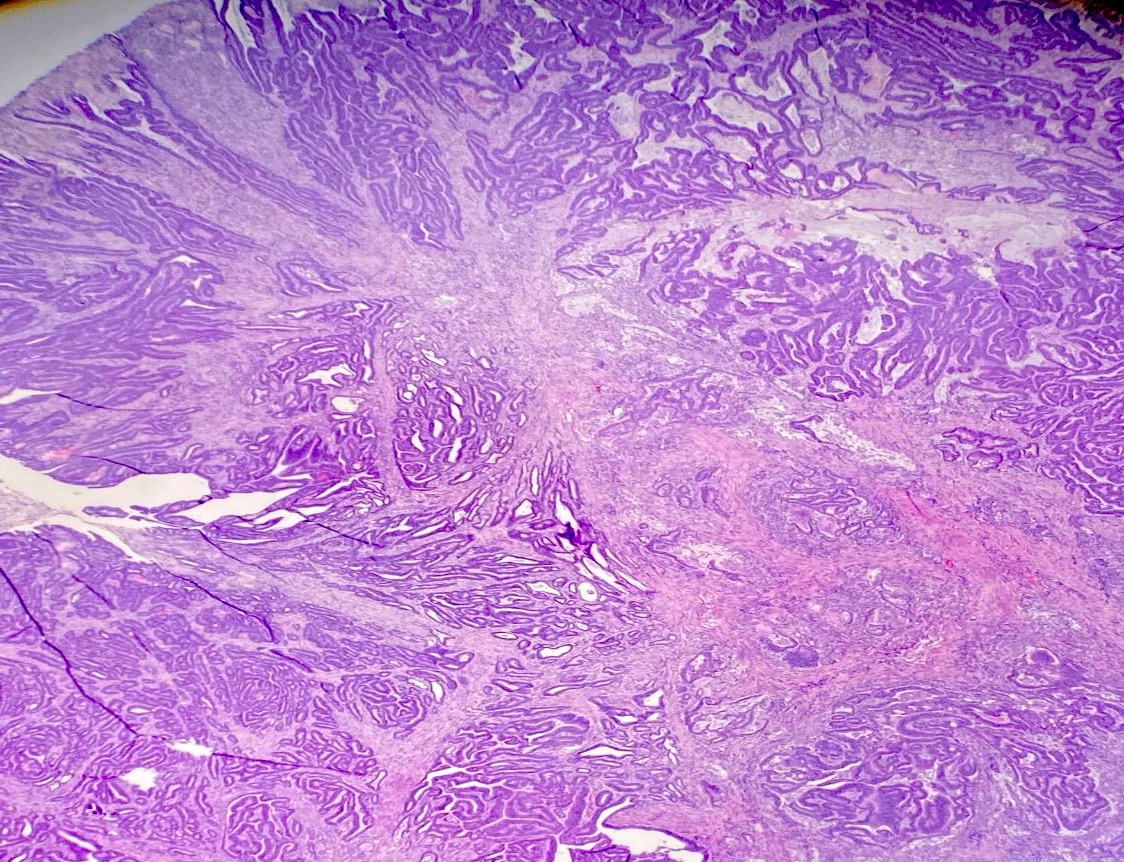
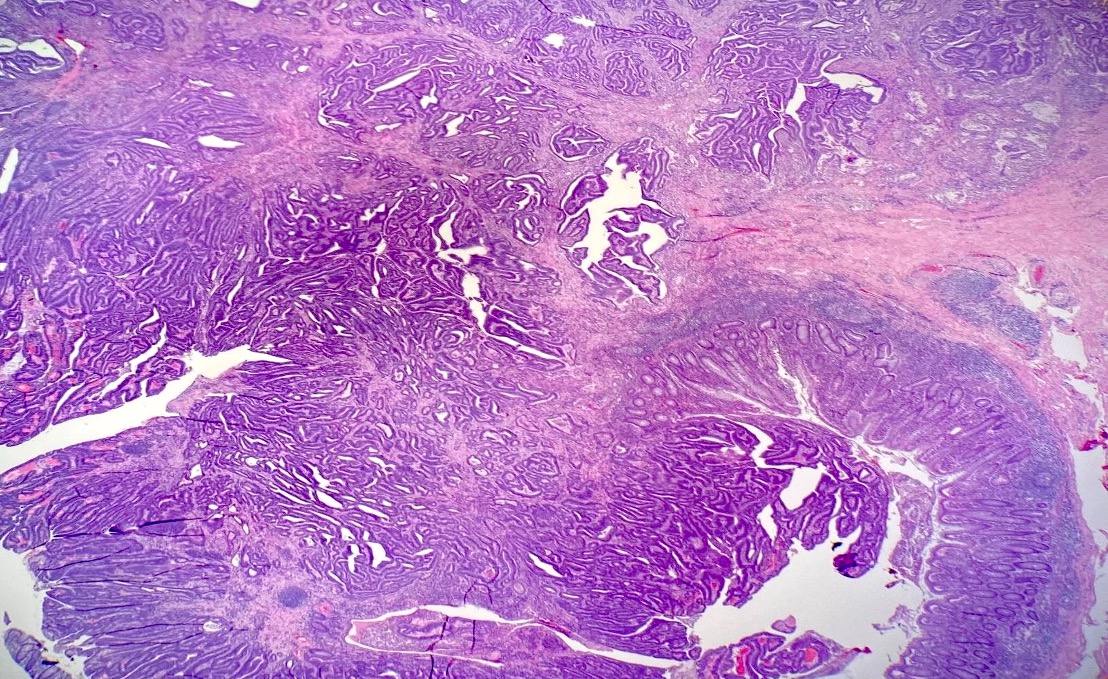
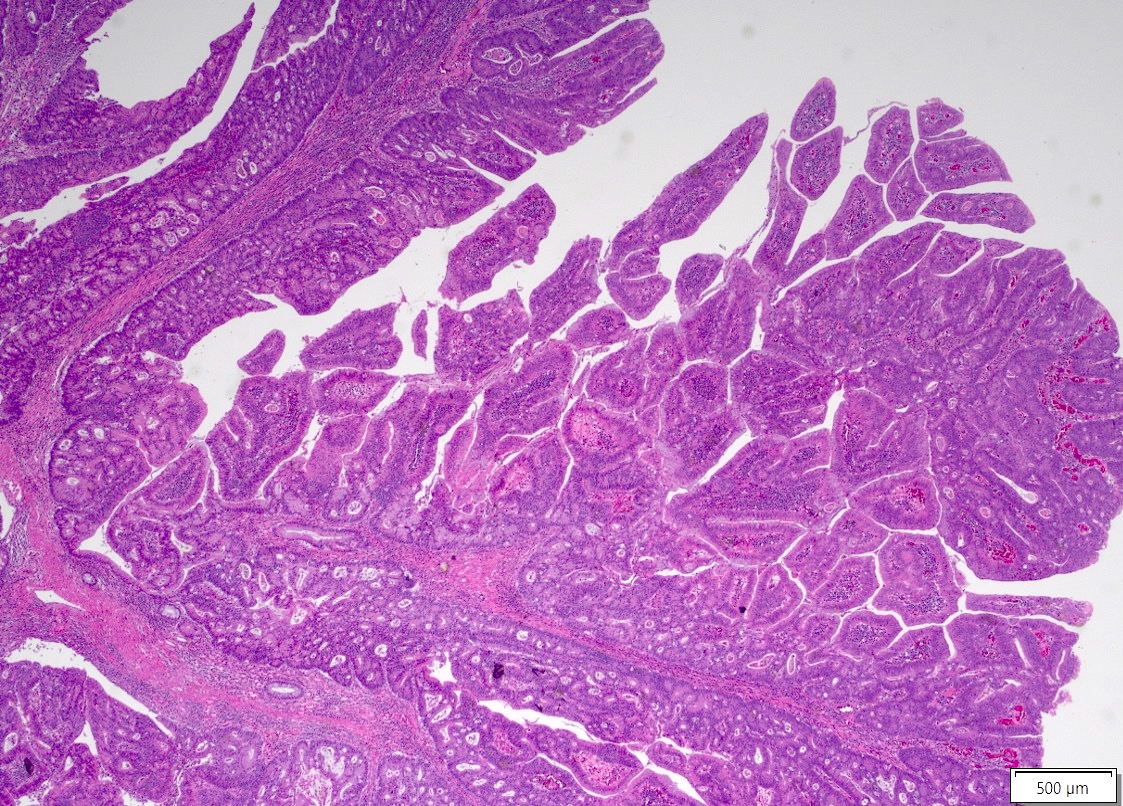
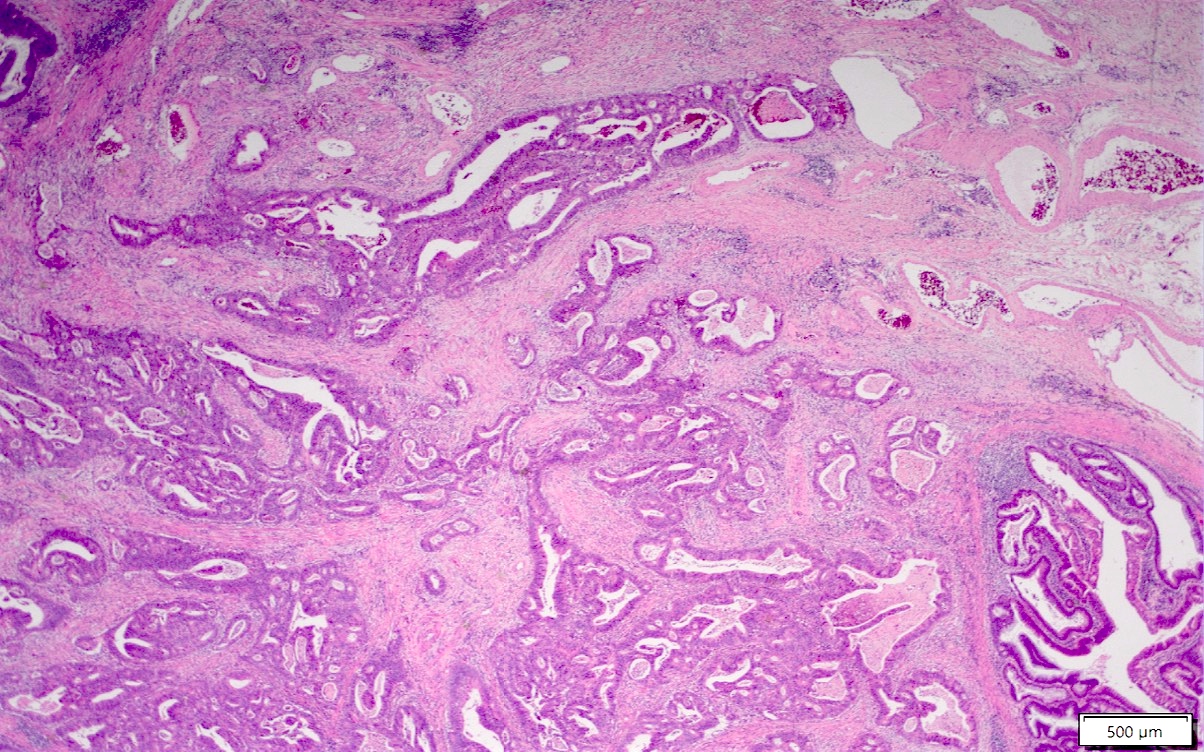
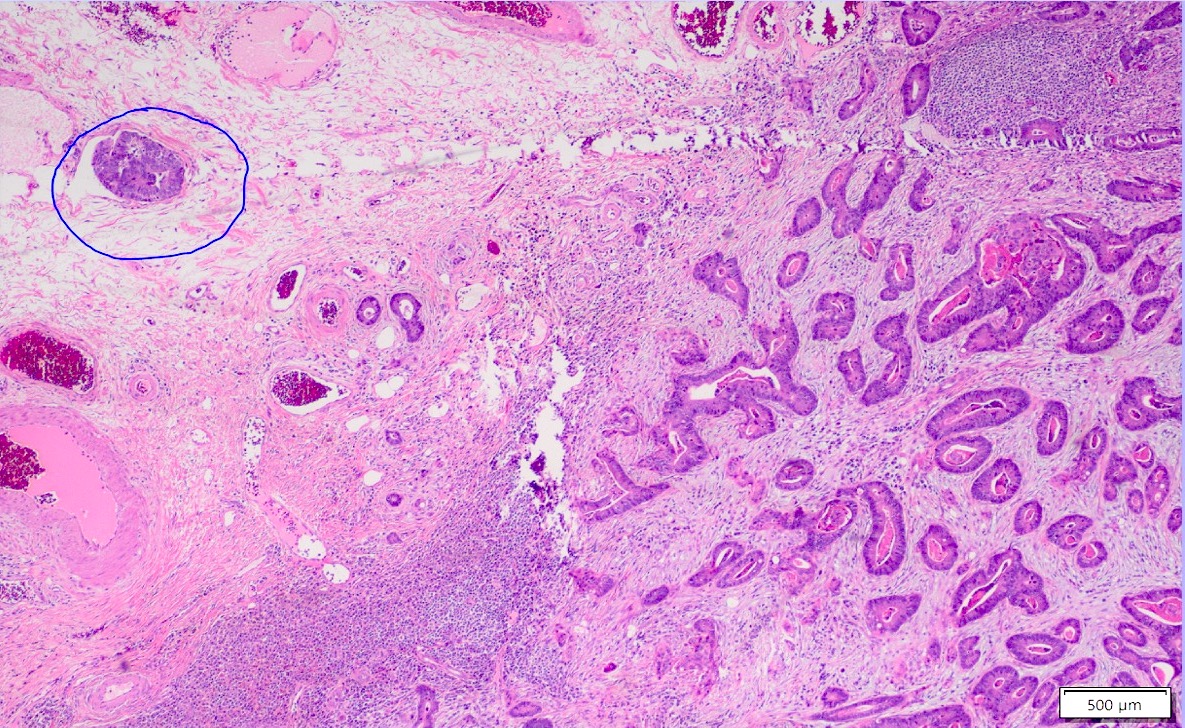
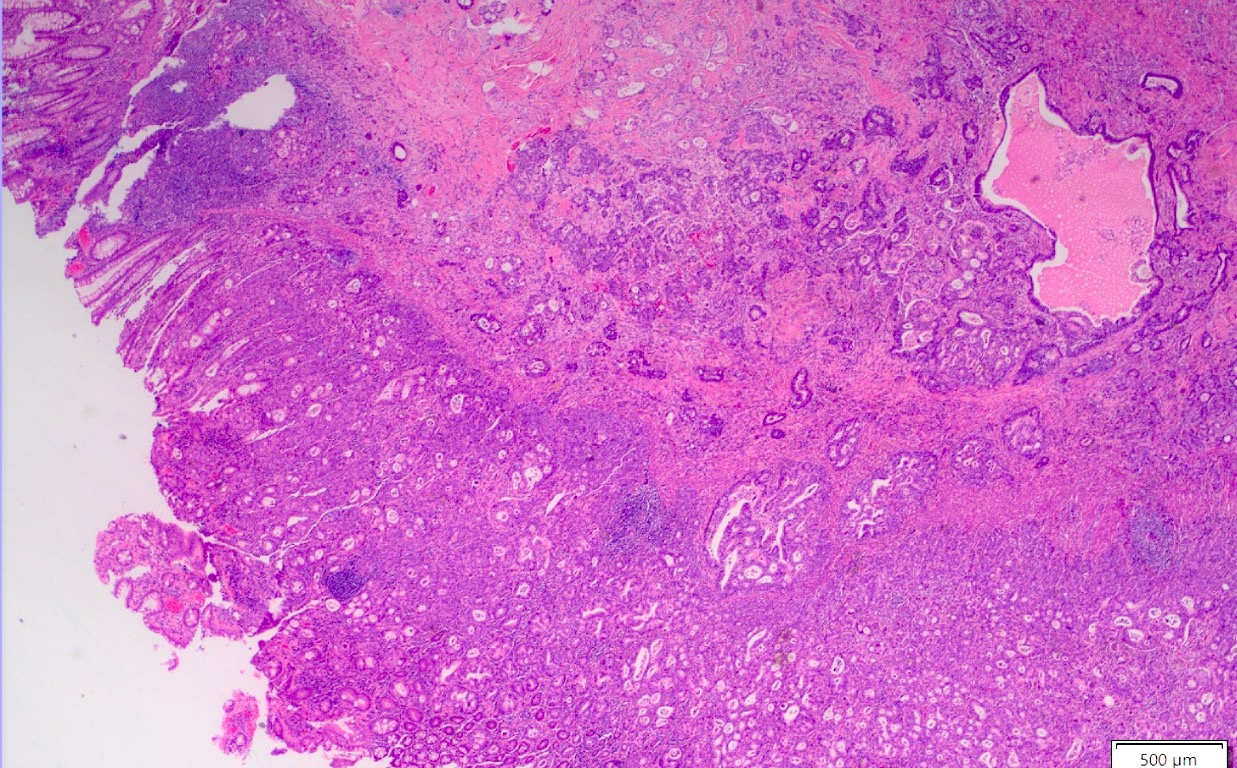
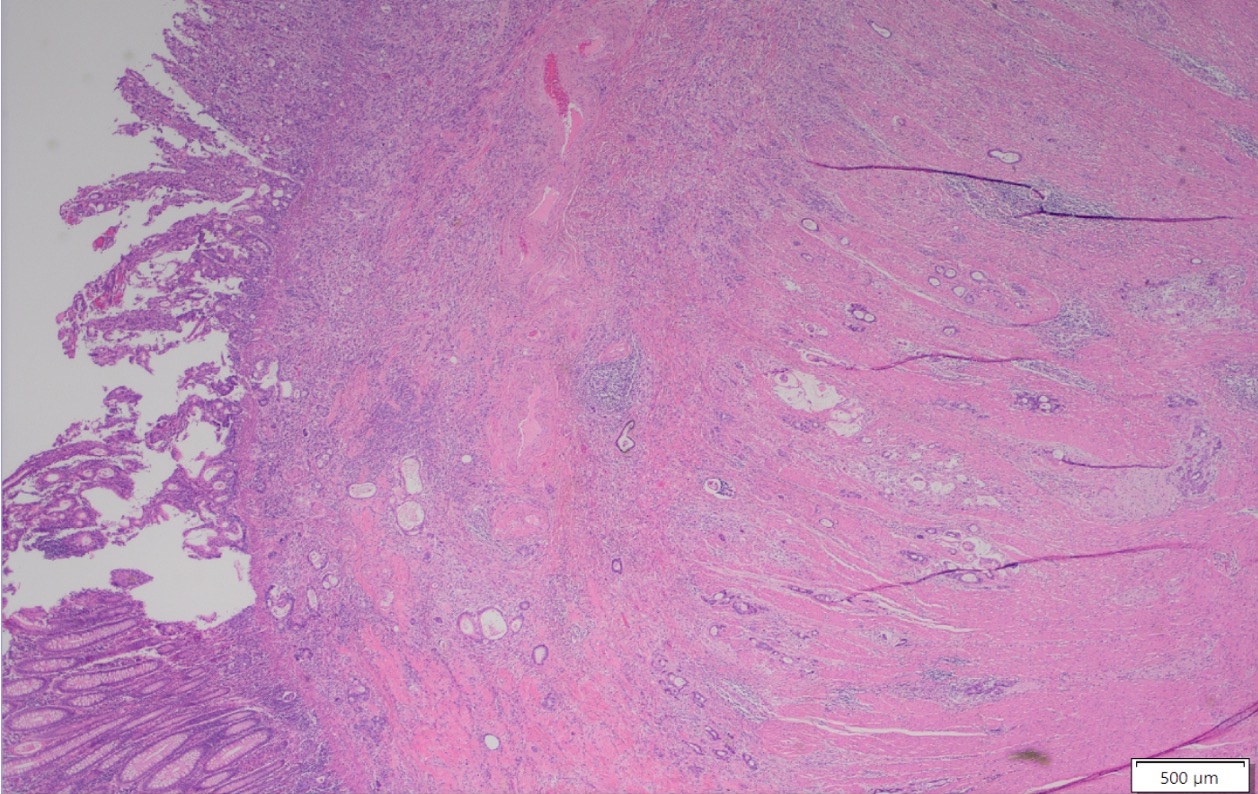
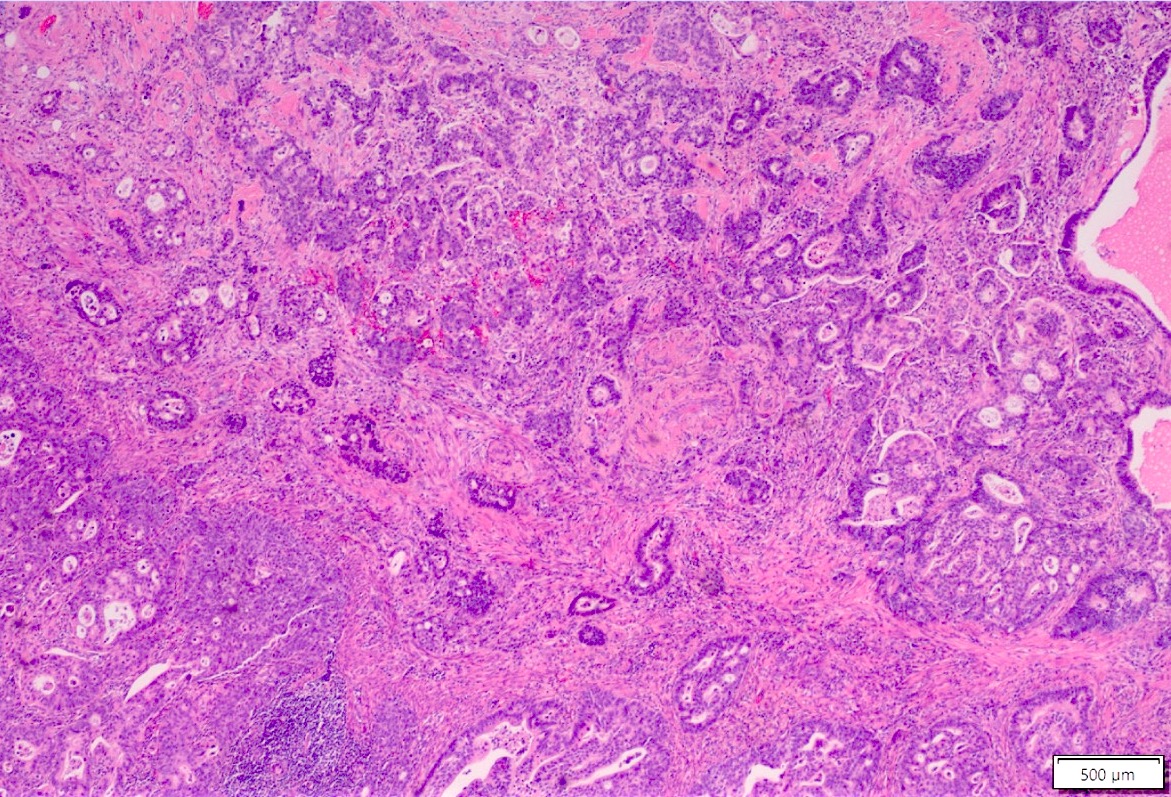
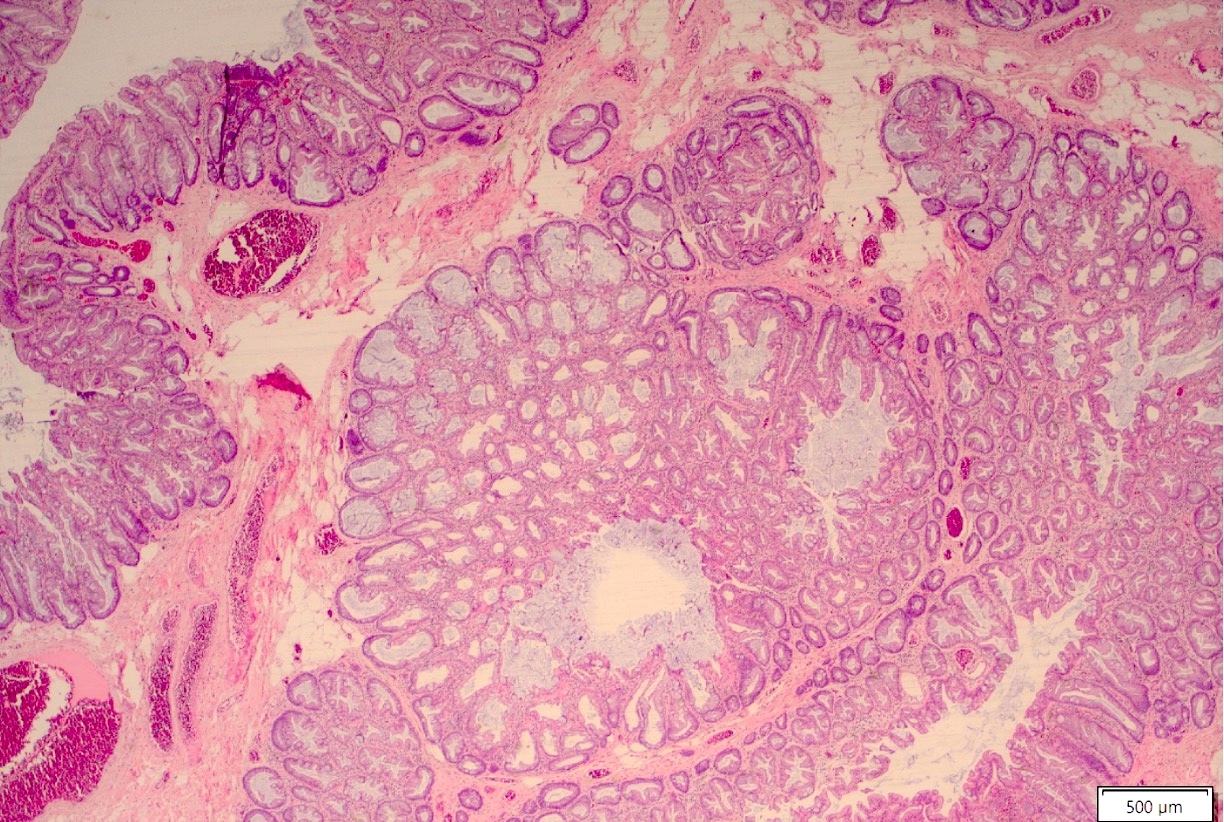
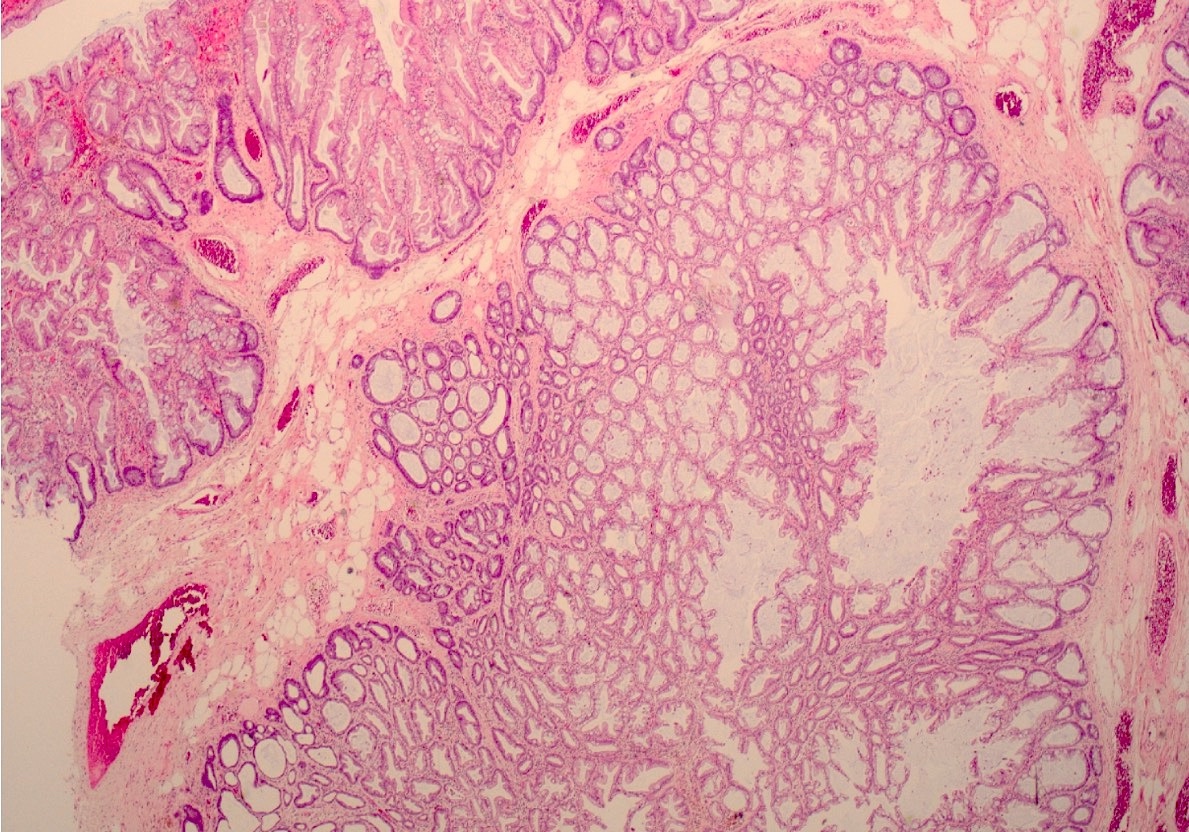
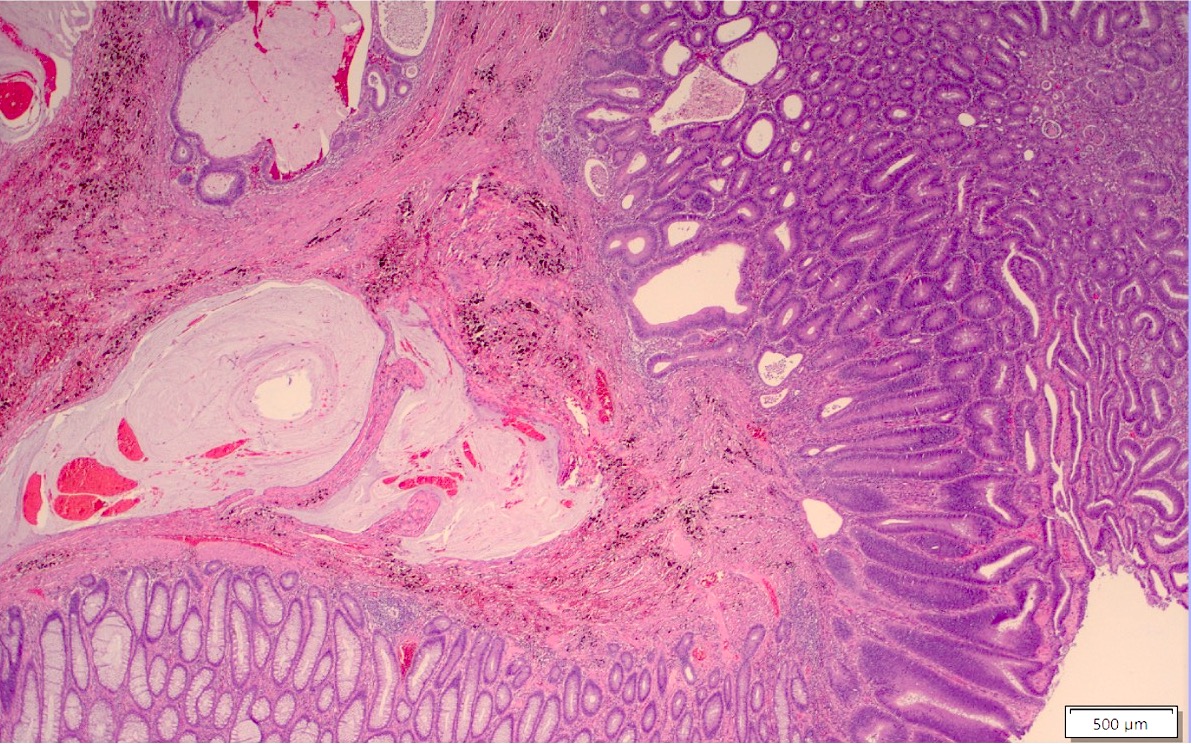
Microscopic (histologic) images
Contributed by Albina Joldoshova, M.D. and Naziheh Assarzadegan, M.D.
Molecular / cytogenetics description
- Sessile serrated adenoma more often shows high levels of microsatellite instability and MLH1 hypermethylation in sporadic cases (Am J Gastroenterol 2012;107:1315)
Sample pathology report
- Colon, ascending polyp, hot snare polypectomy:
- Invasive adenocarcinoma, moderately differentiated, arising in a tubular adenoma (see comment)
- Negative for lymphovascular space invasion
- Low tumor budding score
- Cauterized stalk margins negative for dysplasia or carcinoma
- Immunohistochemistry for mismatch repair proteins will be reported in an addendum
- Comment: Tumor invades into submucosa at the head of the polyp (depth on invasion is 0.5 mm). The distance to the deep margin is 2 mm. Complete excision of this lesion is considered adequate treatment; therefore, completeness of excision should be ensured clinically, if not already achieved.
Differential diagnosis
- Adenoma with pseudoinvasion (misplacement of benign or dysplastic glands) (Cancer 1974;33:206):
- Presence of dysplastic glandular epithelium of the mucosa beneath the muscularis mucosae in colonic polyps mimicking a submucosal invasion
- Usually occurs in large polyps (> 1 cm) (especially those with long stalks) and is mostly found in polyps of the sigmoid colon
- Overall, it has lobular architecture and crypts with smooth and rounded edges
- Nondysplastic or same grade of dysplasia as adenoma at the surface
- Usually surrounded by rim of lamina propria
- Absent desmoplastic stromal response
- Hemorrhage or hemosiderin deposition
- Sometimes acellular extracellular mucin associated with ruptured dilated mucinous cysts and inflammatory response may be noted; need to differentiate from an invasive mucinous carcinoma (colloid), which will have mucin pools with malignant cells, a feature lacking in pseudoinvasion
- Colonic adenomatous polyps involving submucosal lymphoglandular complexes (Am J Surg Pathol 2018;42:1083):
- Lymphoglandular complexes (LGCs) are lymphoid follicles, present in close apposition to lamina propria or muscularis mucosae or submucosa; rarely, colorectal adenomas involve submucosal lymphoglandular complexes, simulating invasive adenocarcinoma with associated extensive lymphoid response and presenting a diagnostic pitfall
- Tumor is contained within the lymphoid tissue and lack infiltrating single cells / small clusters, poorly formed, fused and irregular glands, solid tumor nests, desmoplastic reaction and lymphovascular invasion
- Localized colitis cystica profunda:
- Glandular, nondysplastic epithelium in submucosa
- Overlying mucosa: usually ulcerated or hyperplastic
- Usually rectal; seen with prolapse or after irradiation
Board review style question #1
Board review style answer #1
D. Tubular adenoma with pseudoinvasion. This represents a tubular adenoma with pseudoinvasion, which shows misplacement of dysplastic glandular epithelium into submucosa mimicking a submucosal invasion. Pseudoinvasion will show associated stromal hemorrhage, hemosiderin deposition and acellular extracellular mucin with ruptured dilated mucinous cysts. Answer A is incorrect because of the additional features of pseudoinvasion. Answer B is incorrect because tubular adenomas with invasive adenocarcinoma will show true invasion of neoplastic glands beyond the muscularis mucosa into the submucosa. Answer C is incorrect because abundant expression of extracellular mucin within the tumor is not shown.
Comment Here
Reference: Adenoma with invasive carcinoma
Comment Here
Reference: Adenoma with invasive carcinoma
Board review style question #2
Which of the following are poor prognostic factors for malignant colorectal polyp?
- Large polyp size
- High grade dysplasia
- High tumor budding, lymphovascular invasion, higher histologic grade, positive margin and submucosal invasion > 1 mm
- Villous component in adenomatous polyp
Board review style answer #2
C. High tumor budding, lymphovascular invasion, higher histologic grade, positive margin and submucosal invasion > 1 mm are the adverse prognostic factors for distant metastasis. Answer A is incorrect because while a risk factor for finding an invasive carcinoma is higher (46%) in larger colorectal polyps (> 2 cm), this doesn’t have an adverse prognostic factor for distant metastasis or local recurrence. Answer D is incorrect because a risk factor for finding an invasive carcinoma is higher in colorectal polyps with a more villous component. Answer B is incorrect because while high grade dysplasia has a 35% risk of having carcinoma (versus low grade dysplasia, which has only a 6% risk), it is not a poor prognostic indicator.
Comment Here
Reference: Adenoma with invasive carcinoma
Comment Here
Reference: Adenoma with invasive carcinoma