Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Clinical features | Diagnosis | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: George GV, Huber AR. Intestinal spirochetosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonspirochetosis.html. Accessed March 30th, 2025.
Definition / general
- Colonization of the colonic epithelium by the filamentous nontreponemal anaerobic spirochetes, Brachyspira aalborgi or Brachyspira pilosicoli
Essential features
- Colonization of the colonic epithelium by spirochetes of the Brachyspira species
- Most commonly asymptomatic but may present with diarrhea or abdominal pain / cramps
- Diagnosed by histologic examination of colorectal mucosal biopsies that demonstrate a basophilic fringe on the surface epithelium
- May be confirmed with silver stains (Warthin-Starry, Steiner) or Treponema pallidum immunohistochemistry
- Typically treated with metronidazole, if symptomatic; otherwise, may be observed
ICD coding
Epidemiology
- Human intestinal spirochetosis (HIS) was originally recognized in 1967; however, the pathogenicity is still unclear
- HIS has a global distribution and Brachyspira species have been detected on nearly every continent, with the exception of Antarctica
- Prevalence rate is highly variable and is not entirely clear from the current literature; however, there appears to be lower prevalence rates (ranging from 0.2% to 3.2%) among healthy people residing in developed countries and higher prevalence rates (ranging from 10.8% to 64.8%) in developing countries
- In developed nations, the prevalence rates are thought to be highest among men who have sex with men (MSM) and patients with HIV
- More common in men and patients in the fourth or fifth decades of life
- Although rare, it may occur in pediatric patients
- No confirmed seasonality
- References: Br Med J 1967;3:718, J Gastroenterol Hepatol 2022;37:1222, J Bacteriol 2019;201:e00465, Ann Clin Lab Sci 2020;50:386, Annals Diagn Pathol 2015;19:414, Pediatr Gastroenterol Hepatol Nutr 2019;22:193
Sites
- Any portion of the colon may be involved
- A small study noted a predilection for the right colon (Annals Diagn Pathol 2015;19:414)
Pathophysiology
- Pathogenesis, transmission and risk factors remain unclear
- It is debatable whether Brachyspira species represent a commensal or pathogenic organism
- Electron microscopy findings suggest that the spirochetes adhere to the brush border resulting in thickening of the border (creating a so called false brush border)
- Diarrhea is thought to result from the reduction in absorptive surface secondary to loss of microvilli
- References: Ann Clin Lab Sci 2020;50:386, Pediatr Gastroenterol Hepatol Nutr 2019;22:193, J Bacteriol 2019;201:e00465, J Gastroenterol Hepatol 2022;37:1222
Clinical features
- In most children and adults, human intestinal spirochetosis is asymptomatic and often an incidental histologic finding on endoscopic biopsy material
- In symptomatic patients, the 2 most common symptoms are diarrhea (often chronic and watery) (51%) and abdominal cramps or pain (46%)
- Other symptoms may include bloating, weight loss, constipation, nausea, alternating constipation / diarrhea or irritable bowel syndrome-like symptoms and rectal or perirectal bleeding
- Pediatric patients may develop severe symptoms
- Brachyspira pilosicoli has a broader host range including swine, birds, humans and nonhuman primates
- Known cause of diarrhea in pigs and chickens
- Usually asymptomatic in humans but may cause diarrhea, abdominal pain or perirectal bleeding
- Critically ill patients may have spirochetemia
- Brachyspira aalborgi has only been detected in humans, nonhuman primates and opossums
- Typically, not associated with histologic findings or gastrointestinal symptoms
- Some believe this is simply a commensal organism
- Some studies have found an association between human intestinal spirochetosis and juvenile polyps in children
- References: Ann Clin Lab Sci 2020;50:386, J Gastroenterol Hepatol 2022;37:1222, Pediatr Gastroenterol Hepatol Nutr 2019;22:193, J Bacteriol 2019;201:e00465
Diagnosis
- Gold standard for diagnosis is histologic examination of an endoscopic colon or rectal biopsy
- Noninvasive diagnostic methods are not currently routine
- Reference: J Gastroenterol Hepatol 2022;37:1222
Case reports
- 9 year old boy with recurrent abdominal pain (Arch Pathol Lab Med 2004;128:823)
- 38 year old man with worsening fatigue and dyspnea (Am J Med 2019;132:e654)
- 49 year old man with positive fecal occult blood test result (Clin Gastroenterol Hepatol 2022;20:e1226)
- 60 year old man with hepatitis C cirrhosis and progressive weight loss (Int J Surg Pathol 2014;22:709)
Treatment
- Metronidazole is the most commonly utilized antibiotic for symptomatic patients
- Symptoms will resolve in the majority of patients (81%); in the minority (5%) they will not
- Asymptomatic patients do not usually require treatment
- References: J Gastroenterol Hepatol 2022;37:1222, Ann Clin Lab Sci 2020;50:386
Gross description
- The majority of cases appear grossly normal on endoscopy; rarely, nonspecific erythematous lesions may be seen (Pediatr Gastroenterol Hepatol Nutr 2019;22:193, Ann Clin Lab Sci 2020;50:386)
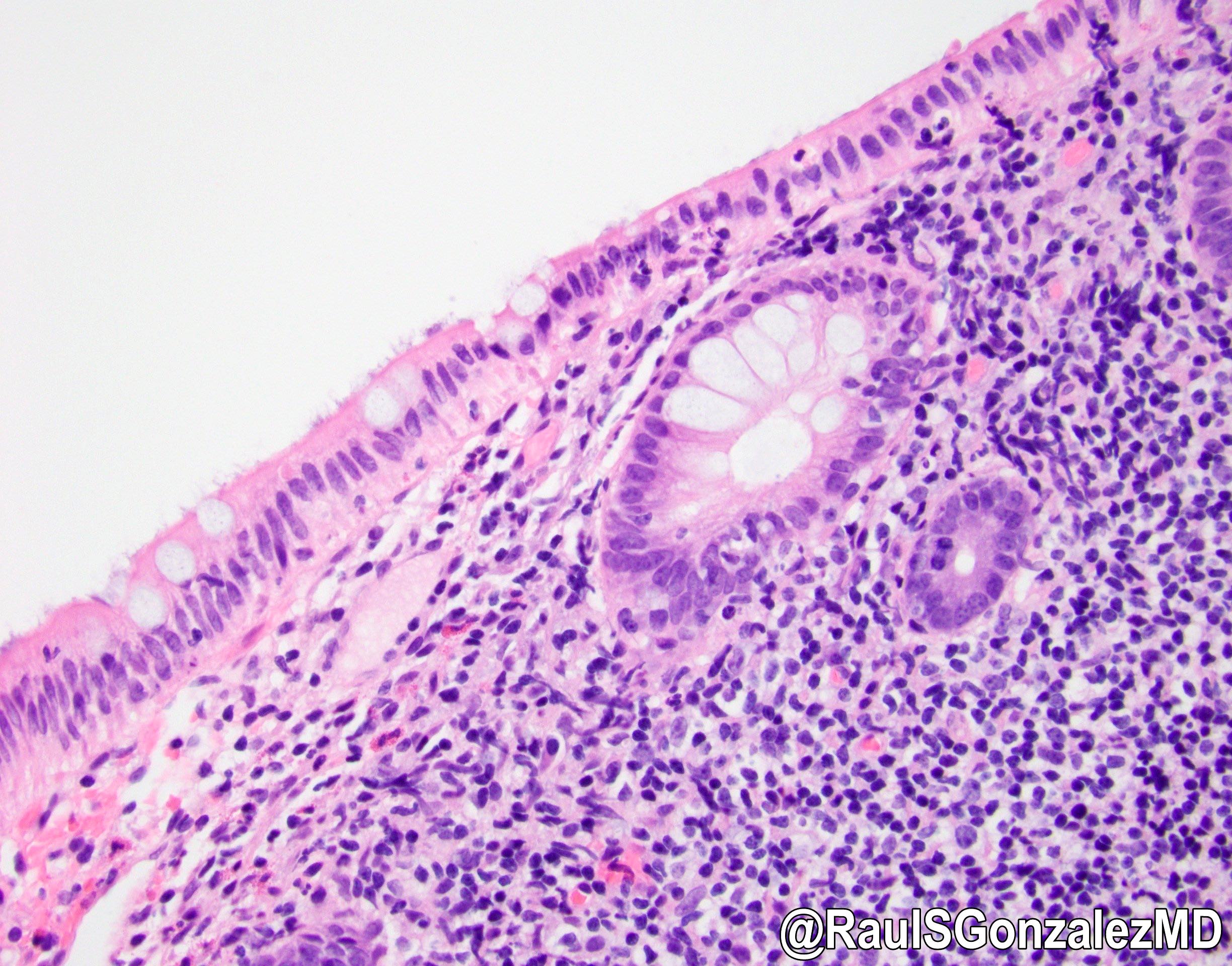
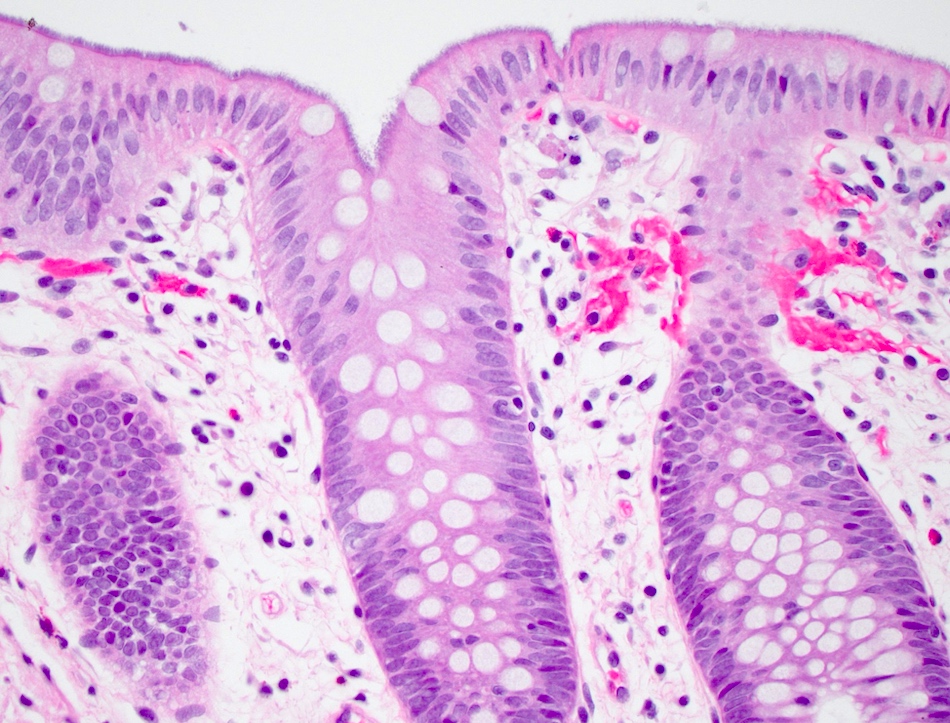
Microscopic (histologic) description
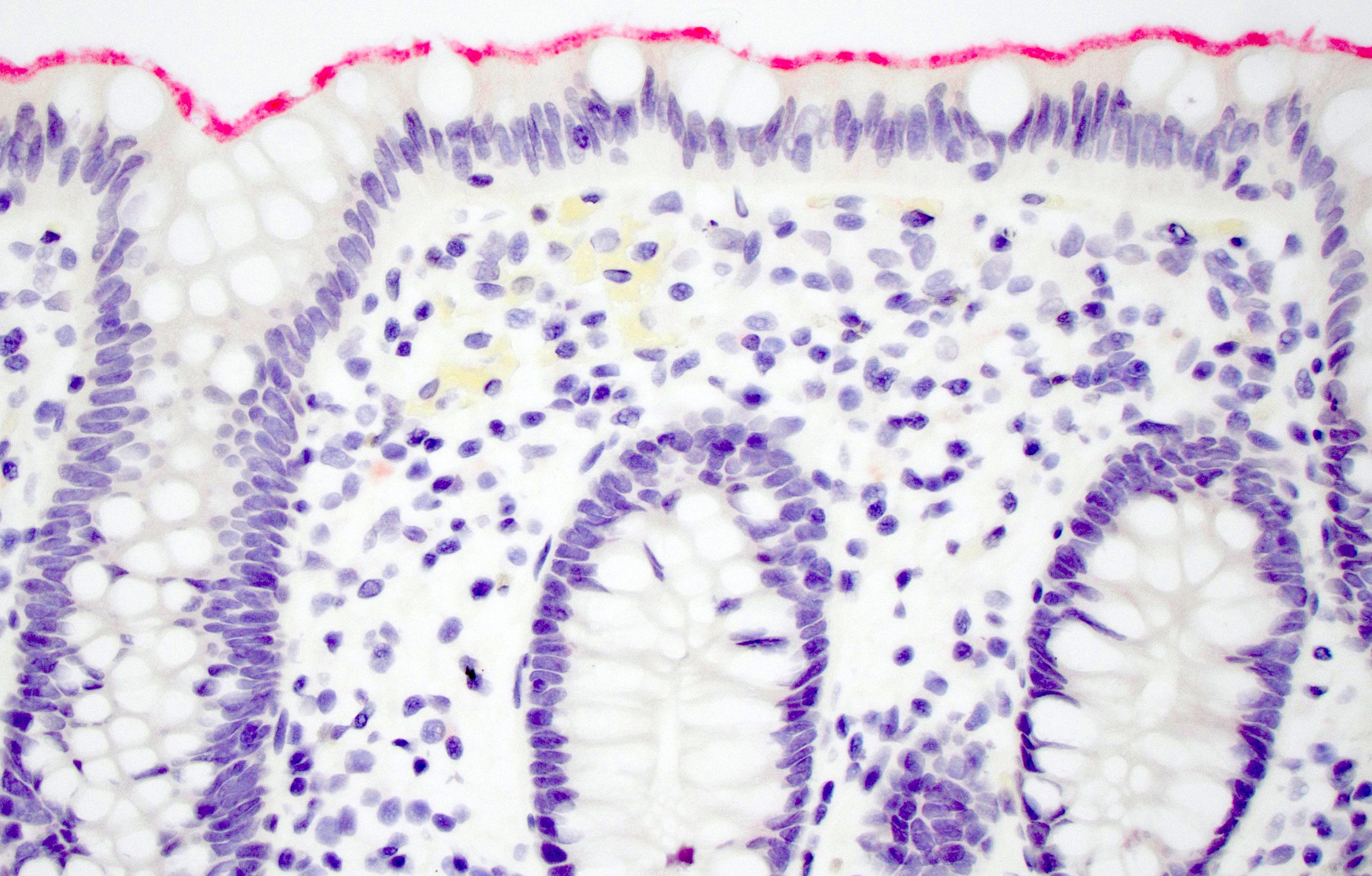
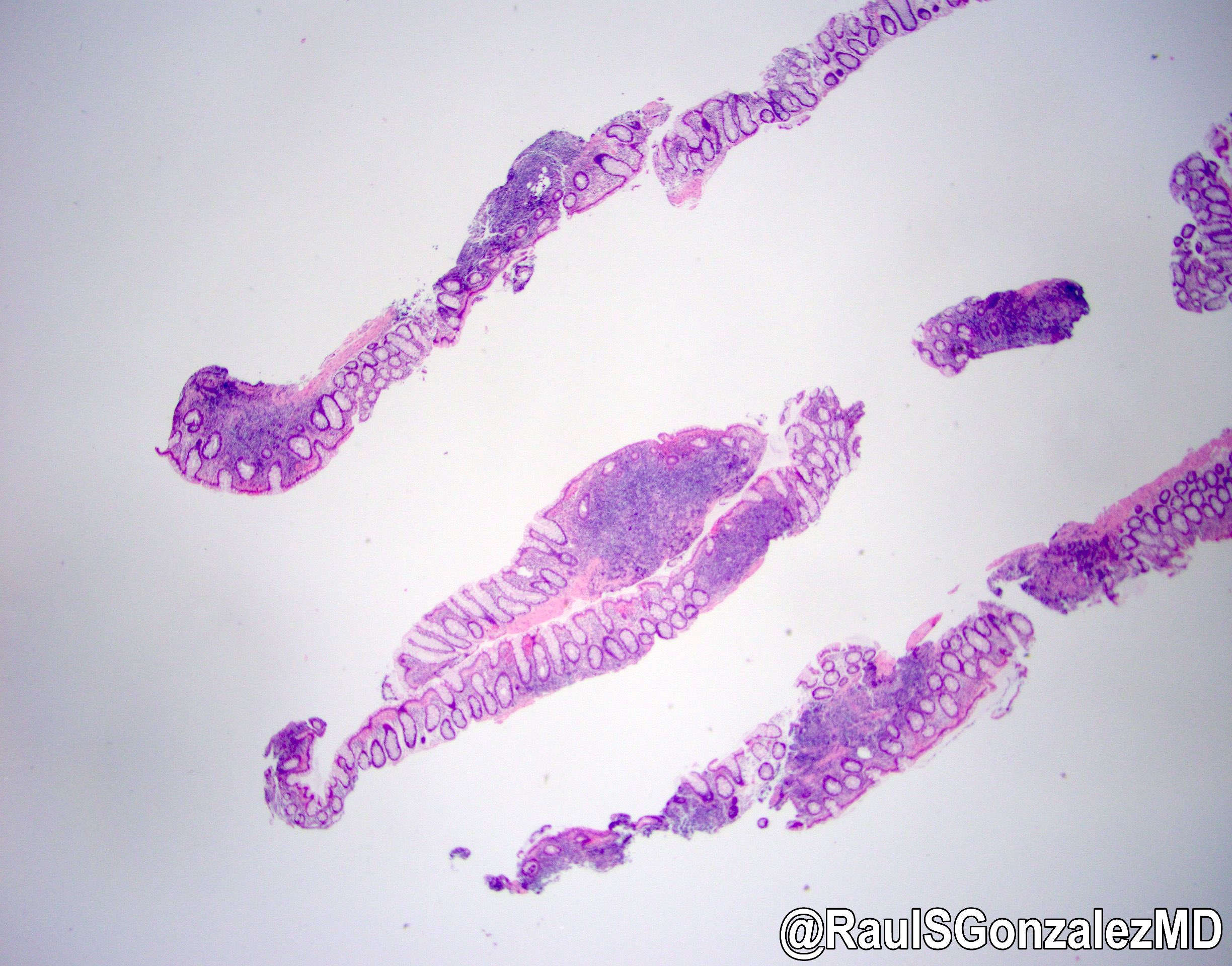
- The characteristic histologic feature of human intestinal spirochetosis is a blue fringe or fuzzy appearance of the surface colonic epithelium on H&E staining, which may be referred to as a so called false brush border, confluent forest or carpeting
- Rarely, there may be nonspecific lymphocytic, neutrophilic or eosinophilic inflammation in the lamina propria or epithelium; lymphoid aggregates or follicles may also be seen
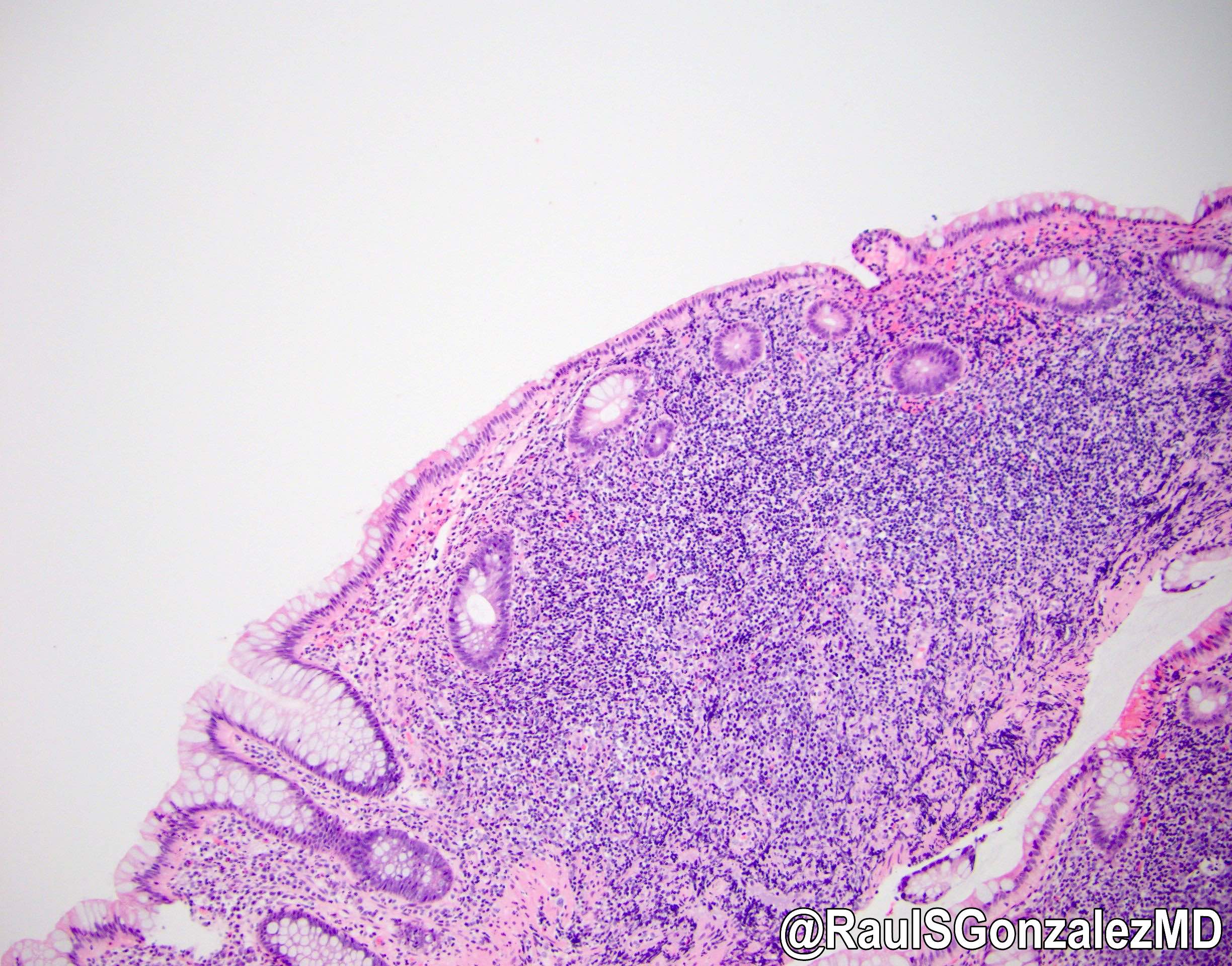
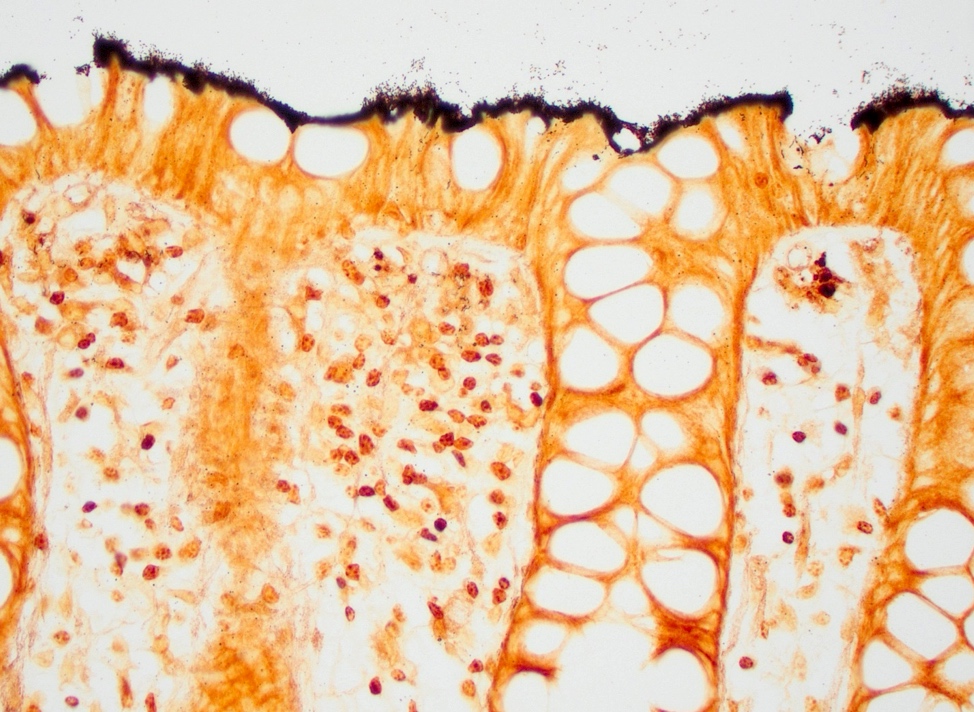
- Organisms may be highlighted by silver stains (Steiner, Warthin-Starry) or immunohistochemical stains for Treponema pallidum, which crossreacts with Brachyspira species
- Reference: Virchows Arch 2020;477:57, J Bacteriol 2019;201:e00465, J Gastroenterol Hepatol 2022;37:1222, Pediatr Gastroenterol Hepatol Nutr 2019;22:193, BMC Infect Dis 2021;21:721
Microscopic (histologic) images
Positive stains
- Organisms may be highlighted by silver stains (Steiner, Warthin-Starry) or immunohistochemical stains for Treponema pallidum, which crossreacts with Brachyspira species
Electron microscopy description
- Nontreponemal spirochetes are attached perpendicularly to the luminal border of enterocytes
- The head of the spirochetes anchors between microvilli, while the tail is directed towards the colonic lumen
- Creates a confluent forest of spirochetes on the surface epithelium, while the microvilli are reduced
- References: J Gastroenterol Hepatol 2022;37:1222, J Bacteriol 2019;201:e00465
Electron microscopy images
Sample pathology report
- Colon, random, biopsy:
- Intestinal spirochetosis (see comment)
- Comment: H&E stained sections demonstrate a basophilic fringe on the surface of the colonic epithelium that is highlighted by a Warthin-Starry stain for spirochetes. The findings are compatible with intestinal spirochetosis.
Differential diagnosis
- Prominent glycocalyx:
- Careful pathologic examination of the surface epithelium and use of special stains (silver or T. pallidum immunohistochemistry) (J Gastroenterol Hepatol 2022;37:1222)
- Enteroadherent Escherichia coli:
- Gram negative on tissue Gram stain
- Normal colon biopsy:
- Findings are subtle and could be missed; always look at the surface of the epithelium in random colon biopsies for the basophilic fringe
Additional references
Board review style question #1
A 50 year old man with chronic watery diarrhea had random colon biopsies taken during a colonoscopy, which demonstrated macroscopically normal mucosa throughout the colon. A representative H&E image of his colon biopsies is shown above, as well as a Warthin-Starry stain performed to confirm the morphologic impression. What is the most likely diagnosis?
- Enteroadherent Escherichia coli
- Intestinal spirochetosis
- Normal colonic mucosa
- Normal colonic mucosa with prominent glycocalyx
Board review style answer #1
B. Intestinal spirochetosis. The H&E image demonstrates the classic basophilic fringe on the surface epithelium, which is characteristic of intestinal spirochetosis. This is confirmed with the Warthin-Starry stain that highlights the organisms. The findings of intestinal spirochetosis may be subtle and appear like normal colonic mucosa. It is important to evaluate the surface epithelium for the presence of the spirochetes in random colon biopsies performed for diarrhea. Enteroadherent E. coli would be strongly gram negative, if performed.
Comment Here
Reference: Intestinal spirochetosis
Comment Here
Reference: Intestinal spirochetosis
Board review style question #2
Which of the following statements is true regarding human intestinal spirochetosis (HIS)?
- All patients diagnosed histologically with human intestinal spirochetosis should be treated with antibiotics
- A majority of patients with human intestinal spirochetosis are symptomatic
- The most common symptoms in symptomatic patients are diarrhea and abdominal pain / cramps
- The most commonly utilized treatment for symptomatic patients is clarithromycin
- The pathogenesis, transmission and risk factors for human intestinal spirochetosis are clearly understood and delineated
Board review style answer #2
C. The most common symptoms in symptomatic patients are diarrhea (which is commonly chronic and watery) and abdominal pain / cramps. Most patients with human intestinal spirochetosis diagnosed histologically are asymptomatic and do not require treatment but may be followed or observed. Metronidazole is the most commonly used antibiotic therapy in symptomatic patients. The pathogenesis, transmission and risk factors for human intestinal spirochetosis are still unclear.
Comment Here
Reference: Intestinal spirochetosis
Comment Here
Reference: Intestinal spirochetosis