Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Parsons DW, Hagen CE. Portal hypertensive colopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonportalhypertensivecolopathy.html. Accessed January 8th, 2025.
Definition / general
- Vascular ectasia of the colon that arises secondarily to liver cirrhosis and portal hypertension that may lead to gastrointestinal bleeding
Essential features
- Consequence of liver cirrhosis and portal hypertension
- Clinicopathologic condition characterized by alterations of colonic mucosa on endoscopy, including edema, erythema, prominent vasculature, telangiectatic vessels and angiodysplasia
- Histologic features may include lamina propria vascular ectasia with hyalinization, telangiectasias, hemorrhage, varying degrees of acute or chronic inflammation and mucosal edema
Terminology
- Portal hypertensive intestinal vasculopathy
- Portal colopathy
- Colopathy of portal hypertension
Epidemiology
- Generally reported in patients with portal hypertension and liver cirrhosis
- In the United States and Europe, cirrhosis most commonly occurs in the setting of chronic alcohol use (World J Gastroenterol 2005;11:3127)
- Infectious etiologies may be more common elsewhere; for instance, in Japan, hepatitis C infection is noted to be the predominant cause of portal hypertensive colopathy in cirrhotic patients (World J Gastroenterol 2005;11:3127)
- Other associations include hepatitis B infection and hepatosplenic schistosomiasis mansoni (Acta Cir Bras 2005;20:9, Mem Inst Oswaldo Cruz 1997;92:699)
- A study by Diaz-Sanchez et al. on the prevalence of portal hypertensive colopathy in liver transplant candidates demonstrated a ratio of M:F = 6:1, with an average age of 55 at the time of diagnosis (World J Gastroenterol 2009;15:4781)
Sites
- More common in the right colon and generally only affects the left colon after progression of right sided involvement (Hawaii Med J 2010;69:39, AJR Am J Roentgenol 1999;172:919)
Pathophysiology
- Pathogenic mechanisms underlying portal hypertensive colopathy are not well understood but it is thought that cirrhosis and portal hypertension are necessary prerequisites for the subsequent development of portal hypertensive colopathy
- In cirrhotic states, the liver accumulates an excess of fibrotic tissue resulting in an increased intrahepatic vascular resistance (JHEP Rep 2021;3:100316)
- Reduced flow through the portal vein manifests as increased pressure within the portal system and is termed portal hypertension (Am J Physiol Gastrointest Liver Physiol 2000;279:G7)
- Increased portal pressure is back transmitted to its venous tributaries, including the superior mesenteric vein responsible for venous drainage of the small bowel and right colon, as well as part of the stomach and pancreas
- Inferior mesenteric vein predominately drains the left colon and the splenic vein that drains the spleen, stomach and pancreas
- These mechanisms have been better described within the context of portal hypertensive gastropathy, an analogous condition in which veins of the stomach become dilated and congested secondary to portal hypertension (Nihon Rinsho 1998;56:2369)
- This back transmission of pressure leads to vascular congestion of the aforementioned veins and thereby contributes to splenomegaly often seen in cirrhotic states
- It also leads to congestive vasculature of the colon by way of the mesenteric veins (World J Gastroenterol 2020;26:6111)
- Liver cirrhosis also leads to decreased production of nitric oxide (NO), which functions as a potent vasodilator
- Decreased production of nitric oxide thus also contributes to increased resistance to flow within the hepatic vasculature and subsequent development of portal hypertension (Clin Liver Dis 2014;18:281)
Etiology
- Liver cirrhosis and portal hypertension are the primary causes of portal hypertensive colopathy
- Common etiologies for liver cirrhosis with portal hypertension include excessive alcohol consumption, hepatitis B and C and hepatosplenic schistosomiasis mansoni (World J Gastroenterol 2005;11:3127, Acta Cir Bras 2005;20:9)
Clinical features
- Clinical features are highly variable but presentation may include
- Bloody bowel movements
- Anorectal varices
- Anemia
- Variety of findings on endoscopy, including telangiectatic vessels, angiodysplasia, hyperemia and increased vascularization (Acta Cir Bras 2005;20:9, World J Gastroenterol 2009;15:4781)
- Some data suggest a significant association between portal hypertensive colopathy and the development of adenomatous polyps, as well as adenocarcinoma
- It is speculated that an abnormal microvascular environment may potentiate the growth of preneoplastic lesions (World J Gastroenterol 2009;15:4781)
- Diaz-Sanchez et al. reported that portal hypertensive colopathy patients were at greater risk for developing spontaneous bacterial peritonitis (World J Gastroenterol 2009;15:4781)
- It is thought that greater vascular permeability and mucosal damage lead to greater likelihood of bacterial translocation
- Systemic symptoms consistent with liver cirrhosis and portal hypertension are often concomitant (J Gastroenterol 2021;56:593, J Clin Exp Hepatol 2022;12:1215)
- Clinical threshold for portal hypertensive colopathy is often lowest in the setting of patients with known liver cirrhosis and portal hypertension but the diagnosis of portal hypertensive colopathy may also lead to the discovery of previously undiagnosed cirrhosis (J Surg Case Rep 2023;2023:rjad114)
Diagnosis
- Currently, there is no accepted standardized diagnostic criteria for portal hypertensive colopathy
- Diagnosis depends heavily on patient history and clinical presentation, in addition to endoscopic and histologic findings
Laboratory
- There are no laboratory tests currently that yield a definitive diagnosis of portal hypertensive colopathy
- However, Ito et al. found a statistically significant correlation between portal hypertensive colopathy and thrombocytopenia (World J Gastroenterol 2005;11:3127)
- The same study demonstrated a significant association between portal hypertensive colopathy and Child-Pugh classes B and C and thus the following labs and clinical findings may aid in the diagnosis of portal hypertensive colopathy: total bilirubin, albumin, international normalized ratio (INR), ascites and encephalopathy
Radiology description
- Bowel wall thickening and hyperemia may be appreciated on computed tomography (CT)
- When bowel wall abnormalities are seen on CT, they are typically appreciated as right sided colonic irregularities
- Dilated mesenteric vessels may also be observed on CT
- References: AJR Am J Roentgenol 1999;172:919, J Surg Case Rep 2023;2023:rjad114
Radiology images
Prognostic factors
- Prognosis may depend on etiology of cirrhosis and portal hypertension (Arq Gastroenterol 2013;50:153)
- Ito et al. found that worsening Child-Pugh scores and thrombocytopenia correlated with increased prevalence of portal hypertensive colopathy (World J Gastroenterol 2005;11:3127)
- It is thus thought that these metrics may be used to predict which patients may be at greater risk for complications, such as lower gastrointestinal (GI) bleeding
Case reports
- 34 year old man with cryptogenic hepatic cirrhosis, splenic vein thrombosis and IgA nephropathy (World J Gastroenterol 2007;13:5783)
- 43, 69 and 70 year old men with liver cirrhosis and sepsis of abdominal origin discovered to have findings consistent with portal hypertensive colopathy with subsequent development of phlegmonous colitis (BMC Gastroenterol 2009;9:94)
- 45 year old man with alcoholic cirrhosis presents with massive lower gastrointestinal bleed (Case Reports Hepatol 2012;2012:735906)
- 57 year old man with cirrhosis and portal hypertension who presented with idiopathic intussusception (Hawaii Med J 2010;69:39)
- 58 year old woman with anemia and chronic alcohol use diagnosed with portal hypertensive colopathy after endoscopy (J Surg Case Rep 2023;2023:rjad114)
- 78 year old man with idiopathic myelofibrosis complicated by portal hypertension diagnosed with portal hypertensive colopathy after increasing transfusion requirements (J Clin Pathol 2004;57:999)
Treatment
- Treatment options vary on clinical presentation but it is generally thought that addressing the portal hypertension may decrease the risk of developing lower gastrointestinal bleeds (Clin Liver Dis 2019;23:643)
- In the case of schistosomal portal hypertensive colopathy, Miranda et al. demonstrated a decrease of portal hypertensive colopathy findings on endoscopy and histology via splenectomy and gastric devascularization: 2 surgical interventions that reduce portal pressure by ~30% (Arq Gastroenterol 2013;50:153)
- Other treatment options may include
- Iron replacement therapy in the case of anemia
- Transfusions
- Portal pressure reducing agents, such as propranolol and octreotide
- Sclerotherapy
- Cryotherapy
- Hemostatic powders
- Argon plasma coagulation (APC)
- Vessel ligation
- Shunt surgery, including transjugular intrahepatic portosystemic shunt procedure (TIPS)
- Liver transplantation
Clinical images
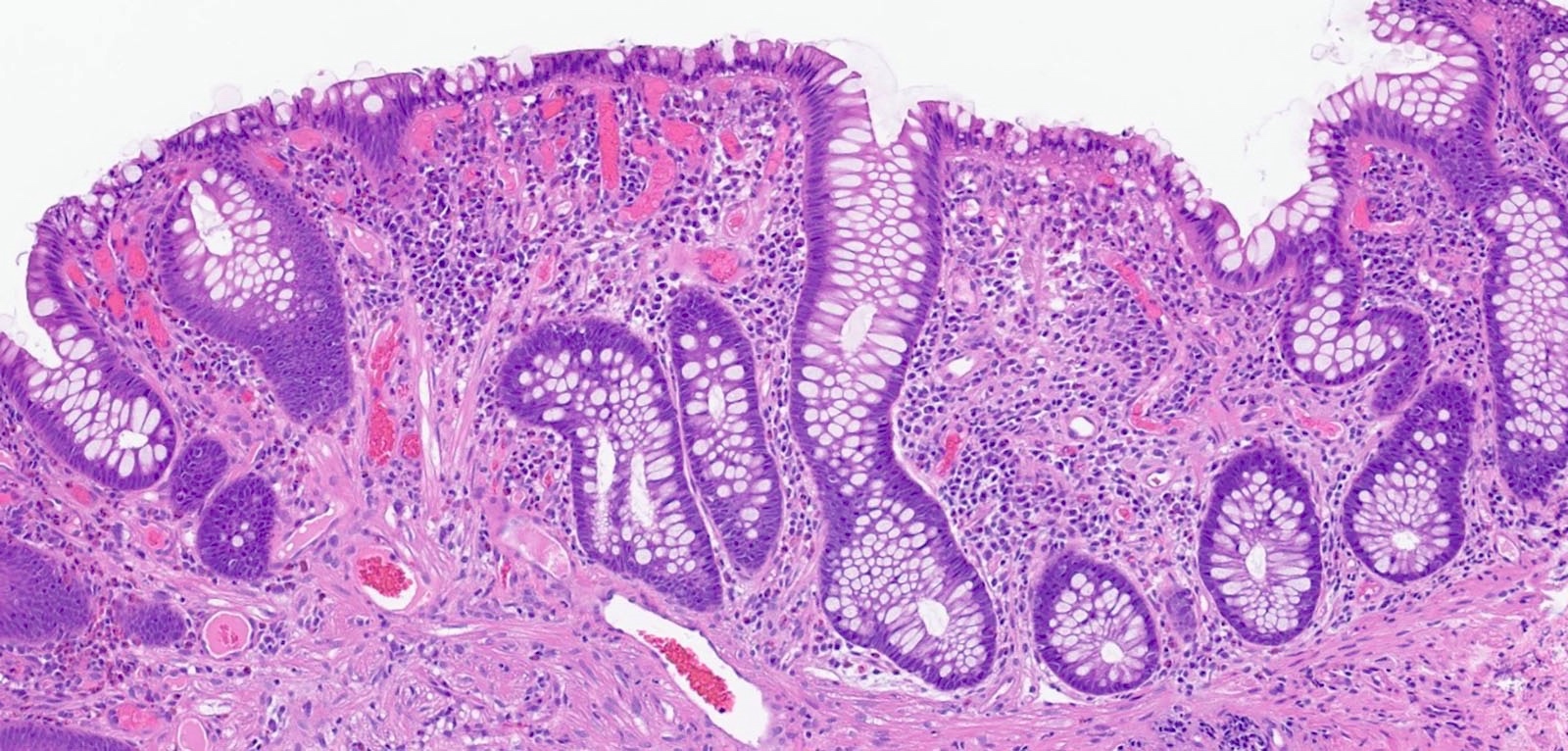
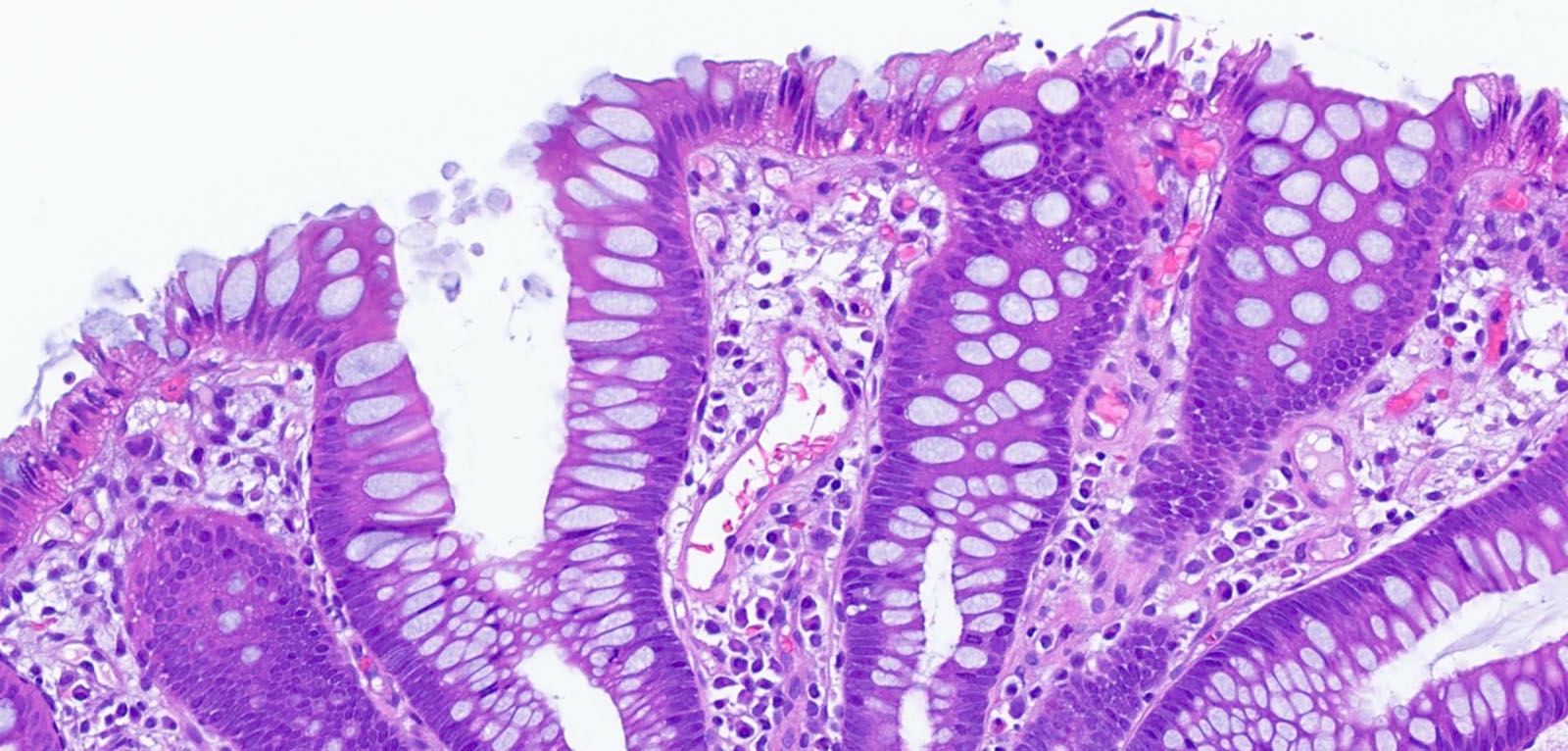
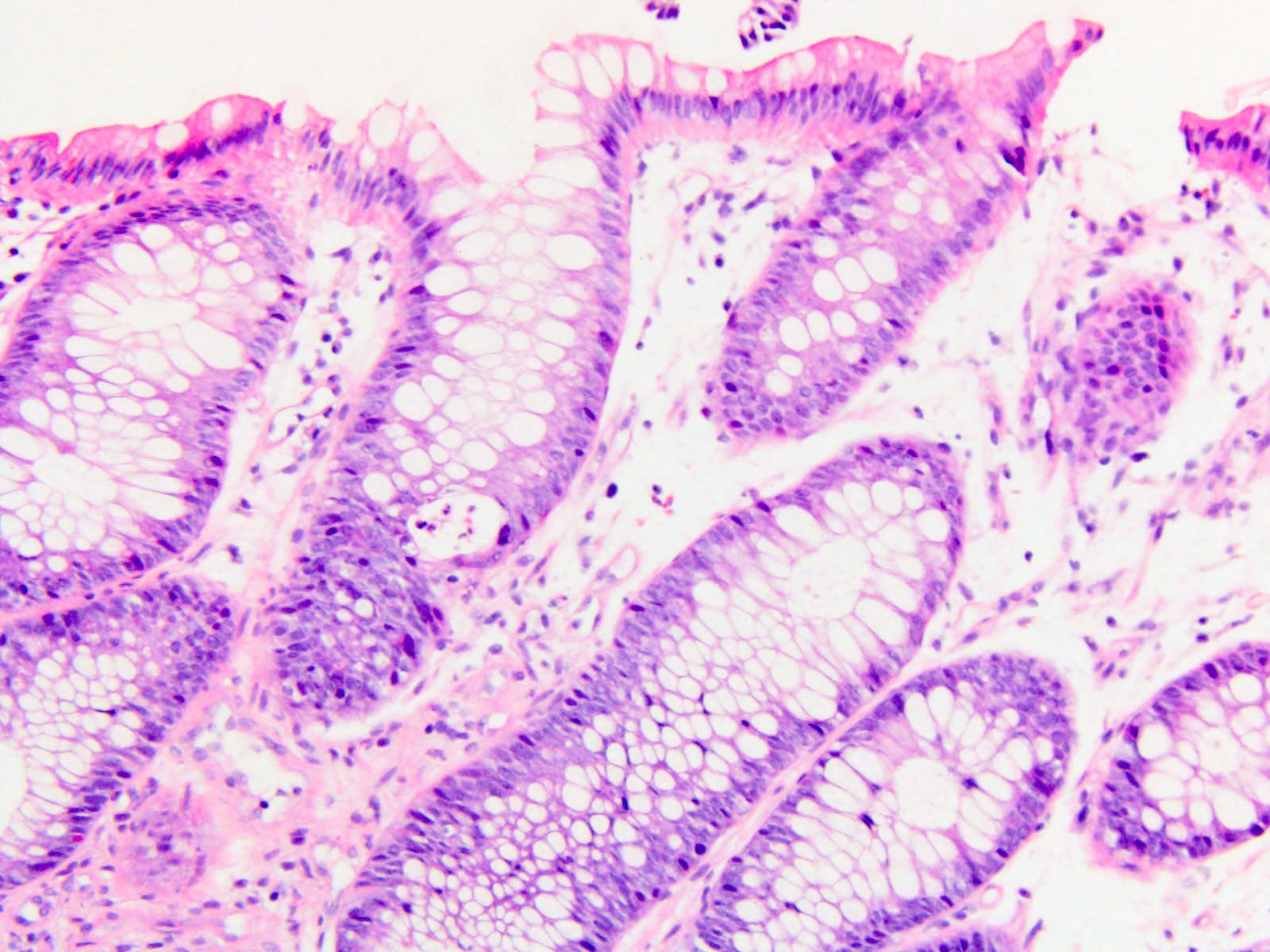
Microscopic (histologic) description
- Lamina propria vascular ectasia
- Mucosal edema
- Thickened, hyalinized lamina propria capillaries
- Varying degrees of active or chronic inflammation
- Hemorrhage
- Mucosal epithelial sloughing
- Telangiectasias
- Sclerosis / fibrosis
- References: Hawaii Med J 2010;69:39, Arq Gastroenterol 2013;50:153
Microscopic (histologic) images
Sample pathology report
- Colon, ascending, endoscopic biopsy:
- Fragments of colonic mucosa with telangiectasia and chronic inflammation consistent with portal hypertensive colopathy
- Colon, entire, endoscopic biopsy:
- Edema and vascular ectasia in otherwise normal colonic mucosa (see comment)
- Comment: The histology is nonspecific but the vascular changes are compatible with portal hypertensive colopathy in the appropriate clinical setting.
Differential diagnosis
- Hereditary hemorrhagic telangiectasia:
- Also known as Osler-Weber-Rendu disease
- Can present with mucocutaneous telangiectasias, gastrointestinal bleeding and portal hypertension secondary to shunting with tortuous and dilated hepatic arteries (GeneReviews: Hereditary Hemorrhagic Telangiectasia [Accessed 10 July 2024])
- Radiation enterocolitis:
- May have vascular ectasia and vascular hyalinization
- Correlation with history of radiation therapy
- Idiopathic myointimal hyperplasia of mesenteric veins:
- Tends to involve left colon of young males
- Thickened, hyalinized vessels can be present in the lamina propria
- Resection specimens show evidence of thickened mesenteric veins (Front Med (Lausanne) 2022;9:855335)
Board review style question #1
A 33 year old man with a medical history of chronic hepatitis C infection presents with bright red blood per rectum. His hemoglobin is found to be 10.6 (reference range: 13.2 -16.6) and albumin is 2.9 (reference range: 3.4 - 5.4). He is also noted to have several scattered telangiectasias on his chest and proximal arms. A colonoscopy is performed, which demonstrates an angiodysplastic-like lesion of his right colon, as well as a few telangiectatic vessels. Endoscopic biopsy is shown above. Which of the following is the most likely cause of his bleeding?
- Infectious enterocolitis
- Ischemic colitis
- Osler-Weber-Rendu syndrome
- Portal hypertensive colopathy
Board review style answer #1
D. Portal hypertensive colopathy. The patient's history of chronic hepatitis C infection point toward a possibility of liver cirrhosis. This possibility is further supported by low albumin levels, which may indicate reduced hepatic synthetic function. Given his anemia and bleeding symptoms in the context of liver cirrhosis, the most likely cause of his bleeding symptoms from the options listed is portal hypertensive colopathy. Moreover, the histology demonstrates telangiectatic vessels, which further supports the diagnosis of portal hypertensive colopathy.
Answer A is incorrect because infectious enterocolitis may be caused by a number of different pathogens, including bacterial organisms, parasites and viruses. Notably, patients will often present with fevers, abdominal pain, nausea, vomiting and diarrhea (DEN Open 2023;3:e242). Given this patient's clinical presentation and absence of aforementioned symptoms, infectious enterocolitis is less likely. Histologically, such infectious colitis typically has an acute self limited colitis pattern and lacks vascular ectasia.
Answer B is incorrect because ischemic colitis often clinically presents with sudden onset abdominal pain, diarrhea and hematochezia. Common associations include a history of atherosclerosis, hypotension, atrial fibrillation, prior valvular or coronary artery surgery or cocaine use. Histologic findings may include edema, crypt withering, hemorrhage of mucosa and submucosa, lamina propria hyalinization, granulation tissue, microvascular thrombi and areas of necrosis (World J Gastroenterol 2008;14:7302).
Answer C is incorrect because Osler-Weber-Rendu syndrome, also called hereditary hemorrhagic telangiectasia (HHT), is a rare autosomal dominant condition characterized by mucocutaneous telangiectasias and arteriovenous malformations (AVMs) of visceral organs. It can present with significant bleeding from a variety of sources, including the gastrointestinal tract and lungs. Clinically, it is diagnosed with the Curaçao criteria, which considers 4 criteria: recurrent epistaxis, mucocutaneous telangiectasias, AVMs of visceral organs and first degree relatives with similar symptoms. The patient above only meets 1 criterion (presence of mucocutaneous telangiectasias) and thus is unlikely to have HHT (QJM 2020;113:586).
Answer A is incorrect because infectious enterocolitis may be caused by a number of different pathogens, including bacterial organisms, parasites and viruses. Notably, patients will often present with fevers, abdominal pain, nausea, vomiting and diarrhea (DEN Open 2023;3:e242). Given this patient's clinical presentation and absence of aforementioned symptoms, infectious enterocolitis is less likely. Histologically, such infectious colitis typically has an acute self limited colitis pattern and lacks vascular ectasia.
Answer B is incorrect because ischemic colitis often clinically presents with sudden onset abdominal pain, diarrhea and hematochezia. Common associations include a history of atherosclerosis, hypotension, atrial fibrillation, prior valvular or coronary artery surgery or cocaine use. Histologic findings may include edema, crypt withering, hemorrhage of mucosa and submucosa, lamina propria hyalinization, granulation tissue, microvascular thrombi and areas of necrosis (World J Gastroenterol 2008;14:7302).
Answer C is incorrect because Osler-Weber-Rendu syndrome, also called hereditary hemorrhagic telangiectasia (HHT), is a rare autosomal dominant condition characterized by mucocutaneous telangiectasias and arteriovenous malformations (AVMs) of visceral organs. It can present with significant bleeding from a variety of sources, including the gastrointestinal tract and lungs. Clinically, it is diagnosed with the Curaçao criteria, which considers 4 criteria: recurrent epistaxis, mucocutaneous telangiectasias, AVMs of visceral organs and first degree relatives with similar symptoms. The patient above only meets 1 criterion (presence of mucocutaneous telangiectasias) and thus is unlikely to have HHT (QJM 2020;113:586).
Board review style question #2
Which of the following histologic features is most commonly associated with portal hypertensive colopathy?
- Architectural distortion
- Crypt abscesses
- Granuloma formation
- Vascular ectasia
Board review style answer #2
D. Vascular ectasia of the lamina propria is a common histologic finding in portal hypertensive colopathy (Hawaii Med J 2010;69:39, Arq Gastroenterol 2013;50:153).
Answer A is incorrect because architectural distortion of colonic crypts can be appreciated in several conditions, such as ulcerative colitis, Crohn’s disease and diversion colitis (bioRxiv 2023 Feb 3 [Preprint], Hum Pathol 1993;24:211).
Architectural distortion is not a histologic hallmark of portal hypertensive colopathy.
Answer B is incorrect because crypt abscesses may be observed in a number of conditions, including ulcerative colitis, self limited colitis and diversion colitis. However, crypt abscesses are not considered a histologic finding in portal hypertensive colopathy (World J Gastroenterol 2010;16:583, Hum Pathol 1993;24:211).
Answer C is incorrect because the presence of granulomas should raise suspicion for Crohn’s disease but granulomas may also form in response to the presence of parasitic ova. Granulomas are not considered a histologic finding in portal hypertensive colopathy (Trends Parasitol 2021;37:176, J Crohns Colitis 2017;11:3).
Comment Here
Reference: Portal hypertensive colopathy
Comment Here
Reference: Portal hypertensive colopathy