Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Shafi S, Esnakula AK. Idelalisib associated. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonidelalisib.html. Accessed April 2nd, 2025.
Definition / general
- Colitis caused by the use of idelalisib, a highly potent small molecule phosphoinositide 3 kinase δ (PI3Kδ) inhibitor approved for the treatment of chronic lymphocytic leukemia / small lymphocytic lymphoma (CLL / SLL) and follicular lymphoma
Essential features
- A triad of intraepithelial lymphocytosis, epithelial cell apoptosis and neutrophilic cryptitis in colonic biopsies with moderate to severe diarrheal symptoms along with clinical history of idelalisib therapy (Am J Surg Pathol 2015;39:1661)
- Many patients develop gastrointestinal symptoms during idelalisib therapy
- Diarrhea with enterocolitis is a common adverse effect of long term idelalisib therapy (Am J Surg Pathol 2015;39:1661)
Epidemiology
- Most of the patients with severe gastrointestinal toxicity are older adults (mean age is 65 years)
- M > F
- History of drug intake for an average of 7 months before severe symptom development (Future Oncol 2018;14:2265)
Sites
- Mostly affects the small intestine and colorectum
- Stomach and esophageal involvement can also be seen (Am J Surg Pathol 2015;39:1653)
Pathophysiology
- Diarrhea with enterocolitis is a common adverse effect of long term idelalisib therapy
- Clinically present with loose, watery and nonbloody stools
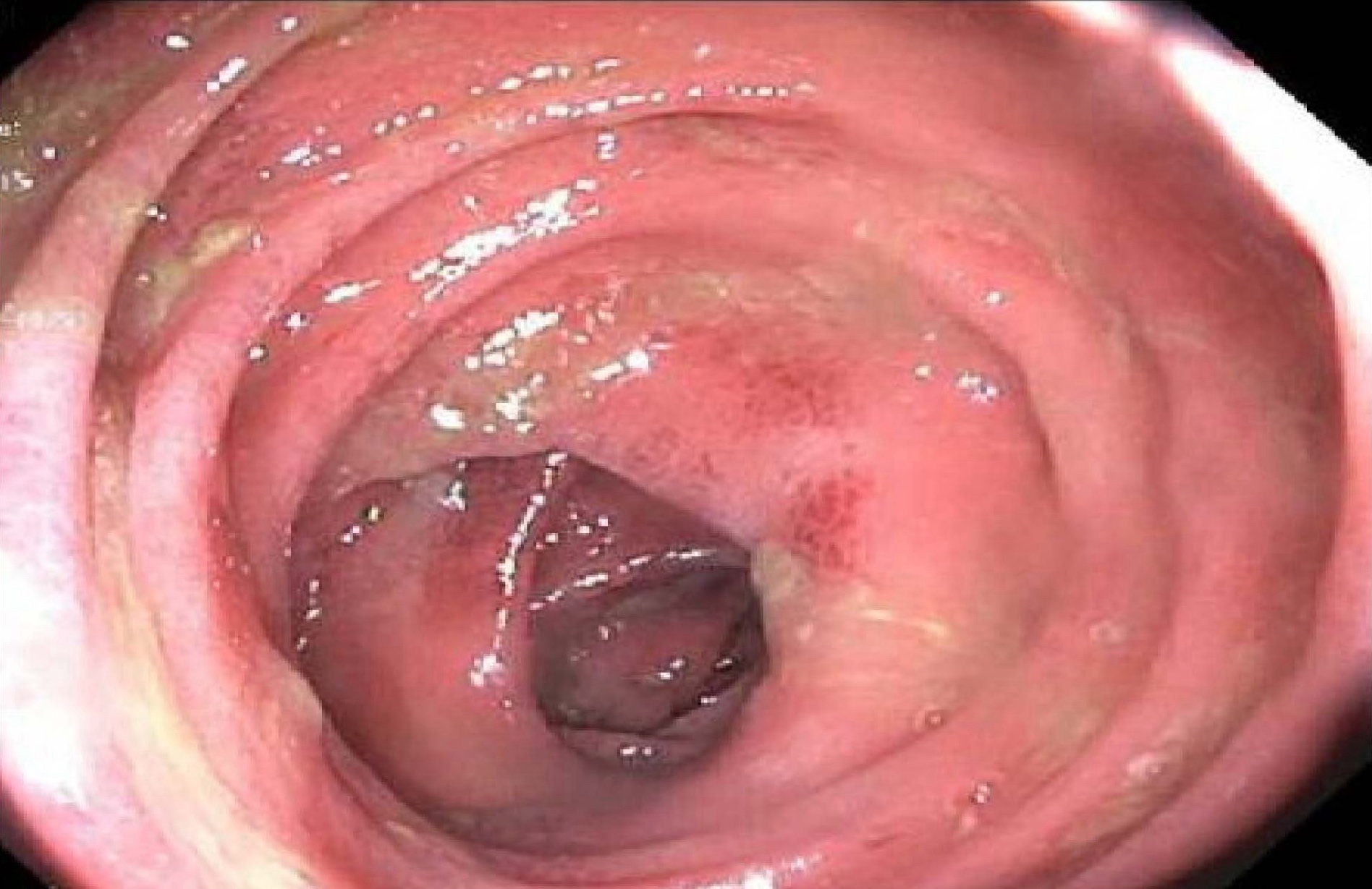
- Majority of patients who undergo a colonoscopy have endoscopically apparent colitis with erythema, congestion and granularity
- More severe cases can exhibit erosions or ulceration (Am J Surg Pathol 2015;39:1653)
Etiology
- Idelalisib (Zydelig) is a small molecule inhibitor of phosphoinositide 3 kinase δ (PI3Kδ) that was recently approved for treatment of relapsed B cell malignancies, including chronic lymphocytic leukemia and follicular lymphoma
- Median time for onset of severe grade 3 or 4 diarrhea is ~7 months (Am J Surg Pathol 2015;39:1653)
Clinical features
- Diarrhea, nausea, fatigue, cough, pyrexia, chills
- Rarely associated with transaminitis, pneumonitis
Diagnosis
- Physical examination including assessment of patient for fever, dizziness, abdominal pain / cramping and weakness (i.e., rule out risk for sepsis, bowel obstruction, dehydration)
- History of onset and duration of diarrhea
- Travel history to exclude infectious etiologies
- Description of number of stools and stool composition (e.g., watery, bloody, nocturnal)
- Medication profile to identify diarrheagenic agents
- Dietary profile to identify diarrheagenic foods (Leuk Lymphoma 2015;56:2779)
Laboratory
- Stool workup
- Occult blood determination
- Culture for enteric pathogens (Salmonella, Escherichia coli, Campylobacter, Clostridium difficile)
- Complete blood count, electrolytes and blood urea nitrogen / creatine (BUN:Cr) (grade 3: neutropenia, thrombocytopenia, anemia and alanine transaminase [ALT] or aspartate transferase [AST] elevation)
- Consider colonoscopy in selected cases (Leuk Lymphoma 2015;56:2779)
Radiology description
- Majority of patients who undergo a colonoscopy have endoscopically apparent colitis with erythema, congestion and granularity or ulceration
Prognostic factors
- Poor prognostic factors include fatal or severe diarrhea or colitis, hepatotoxicity, pneumonitis and intestinal perforation
- Adverse idelalisib events include pneumonia, pyrexia and febrile neutropenia (Leuk Lymphoma 2015;56:2779)
Case reports
- 40 year old woman with relapsed grade 2 follicular lymphoma presented with 3 days of vomiting, cramping abdominal pain and diarrhea (JAMA Oncol 2016;2:1361)
- 56 year old man with a history of relapsed follicular lymphoma presented with severe diarrhea and a skin eruption mimicking graft versus host disease 6 months after starting idelalisib (Clin J Gastroenterol 2017;10:142)
- 72 year old woman presented with abdominal pain, nonbloody diarrhea for 2 months and 15 lbs of weight loss (Ann Gastroenterol 2016;29:233)
Treatment
- Discontinue idelalisib
- Rule out infection
- Intravenous or oral rehydration if grade 3 diarrhea or colitis
- Budenoside or oral steroids (intravenous if orals are not tolerated)
- Diet modification recommendations such as plenty of fluids, 8 - 12 glasses a day of oral rehydration drinks, 5 - 6 small meals each day and low fat, high protein foods such as lean meat and eggs (Leuk Lymphoma 2015;56:2779)
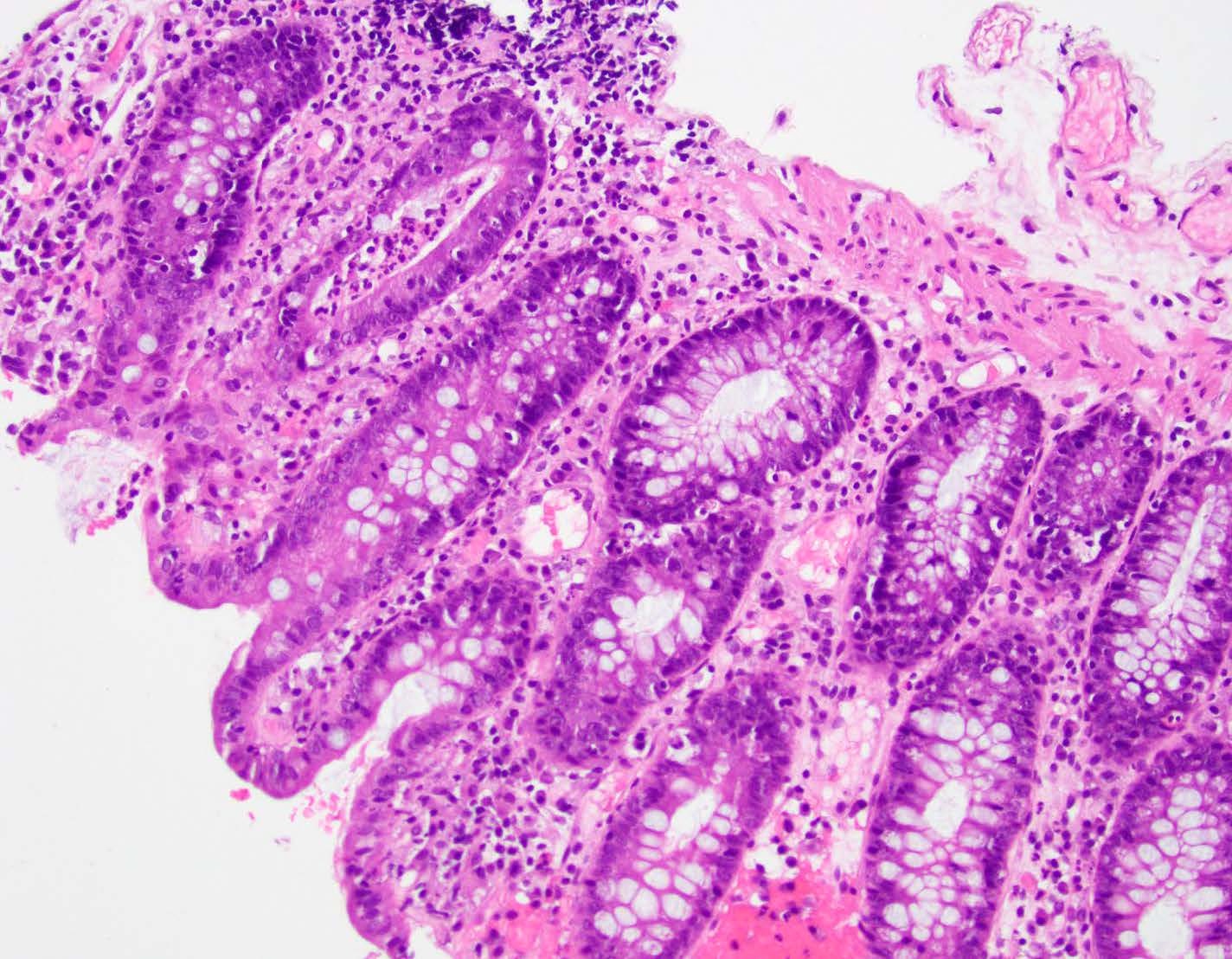
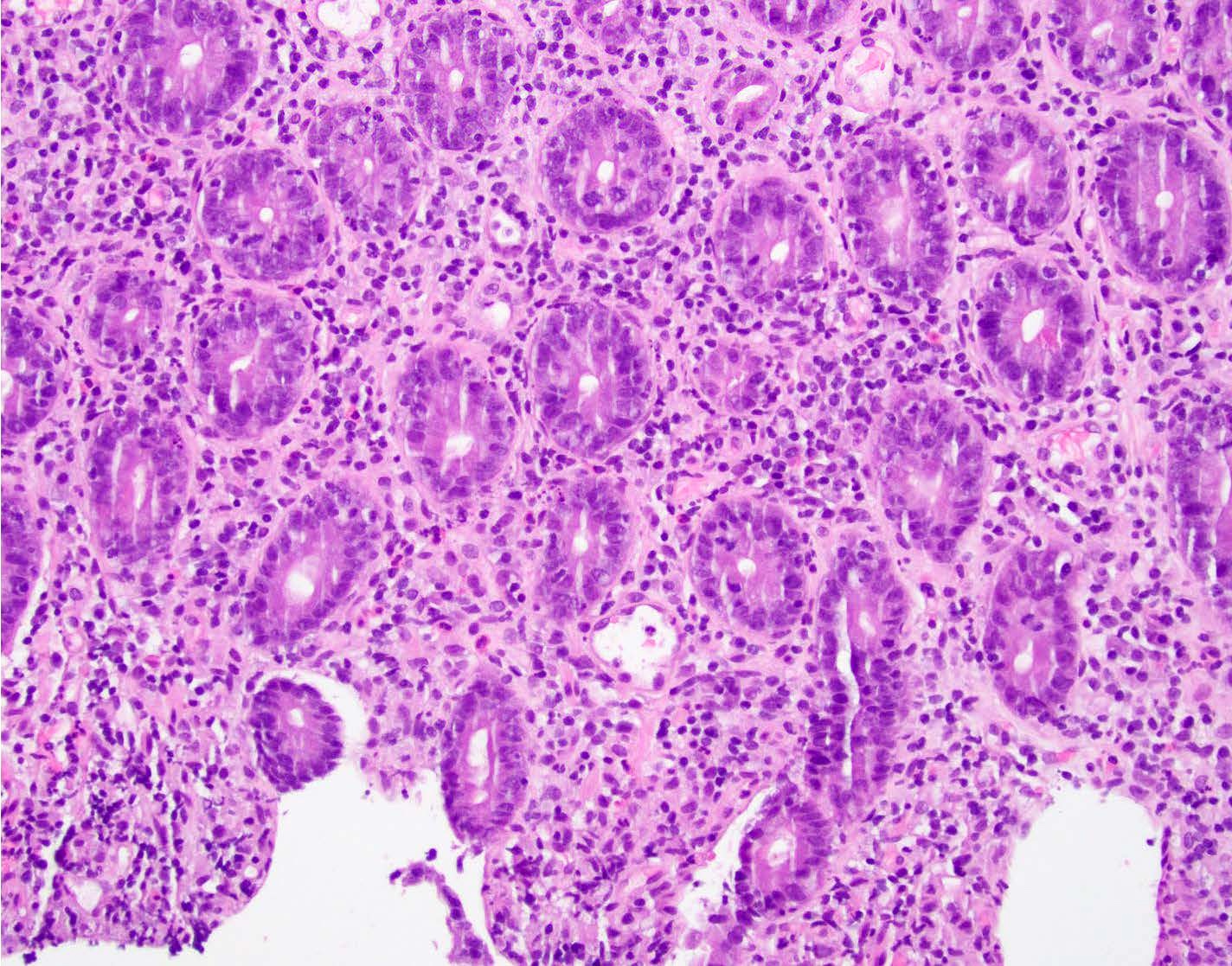
Microscopic (histologic) description
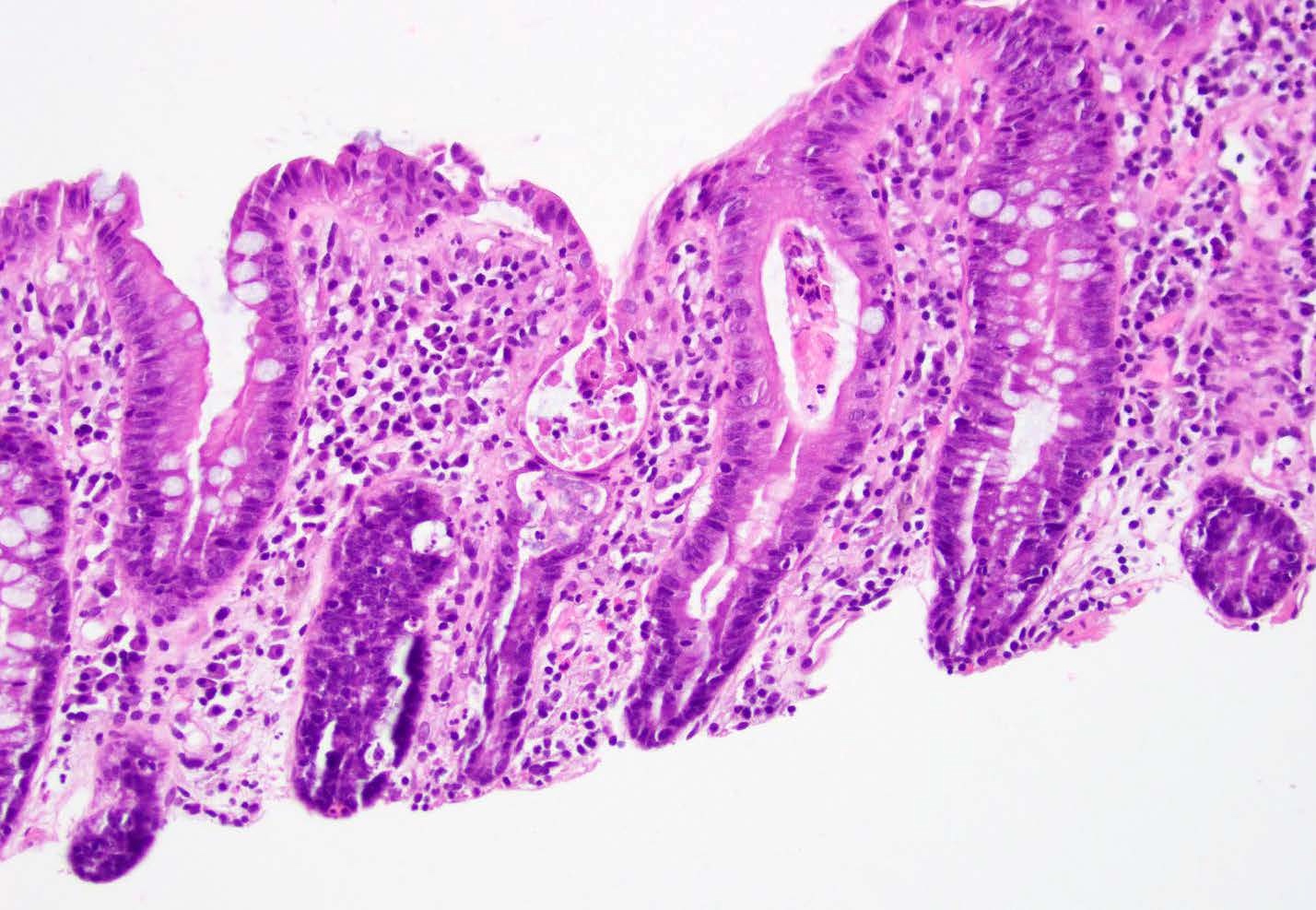
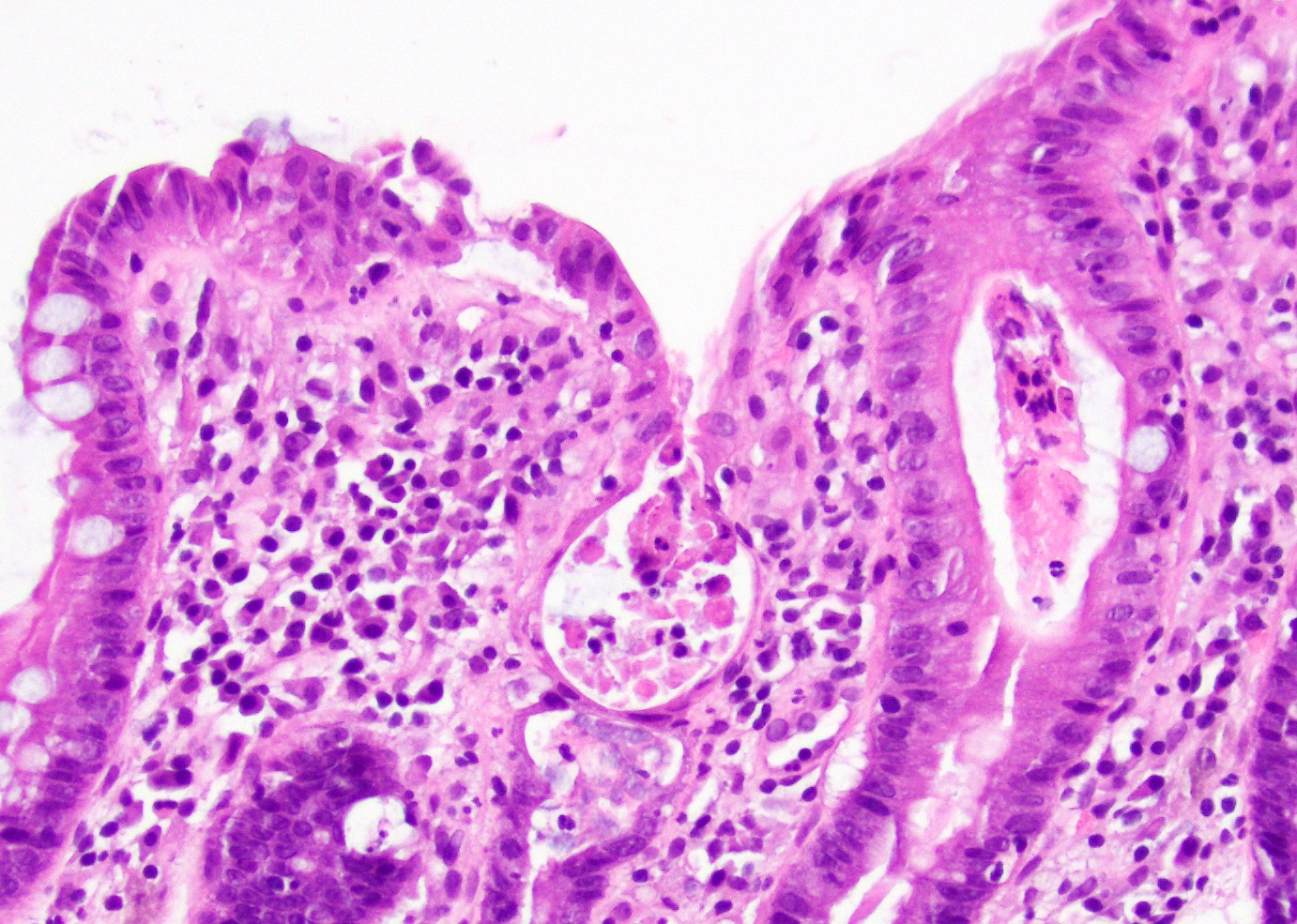
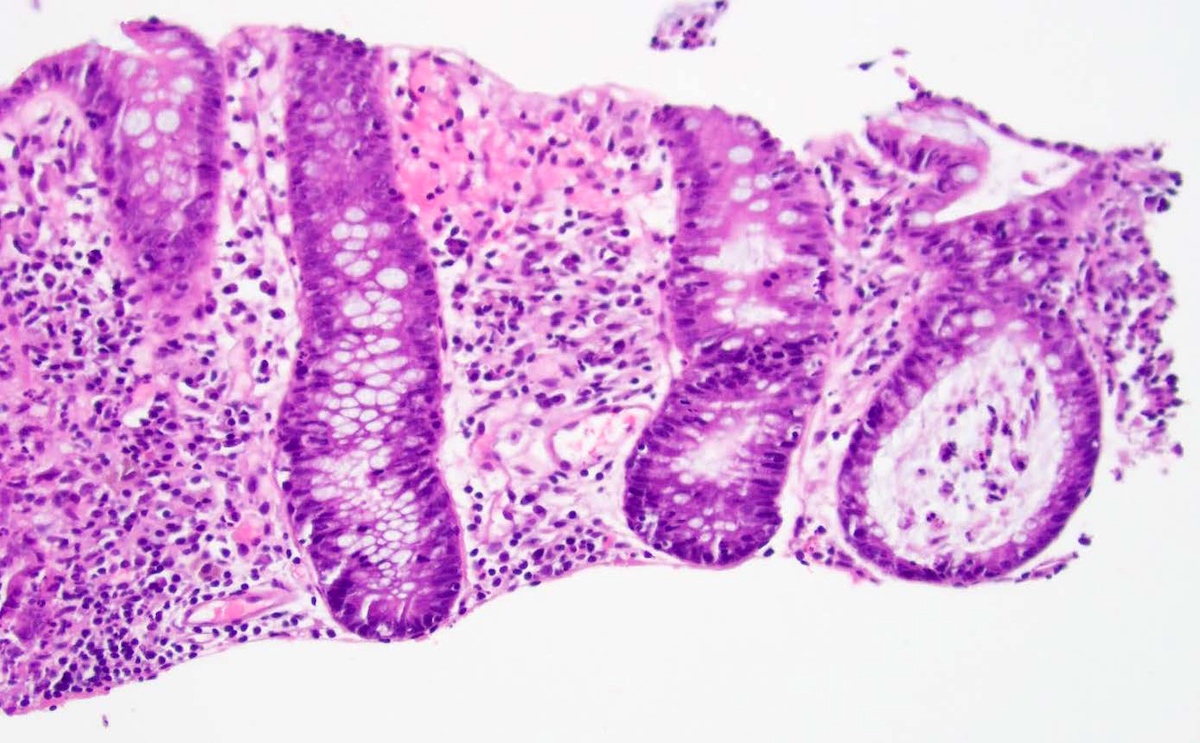
- Presence of intraepithelial lymphocytosis in both the crypts and surface epithelium
- Apoptotic crypt epithelial cells (sometimes numerous with large exploding apoptotic cells)
- Neutrophilic infiltration of the crypt epithelium with occasional crypt abscesses
- Minority show crypt architectural distortion in those patients that had a prolonged interval between symptom onset and colonoscopy
- Histologic patterns can be divided into 4 distinct morphological categories:
- Predominantly normal
- Apoptotic pattern without intensive inflammatory component
- Infectious colitis-like pattern characterized predominantly by inflammation with varying degrees of attenuated glands (apoptotic cells not a prominent feature)
- Mixed pattern with varying degrees of apoptotic cells, mixed inflammation or attenuated glands, with the most striking features of architectural distortion, mixed inflammation (including intraepithelial lymphocytes and neutrophils and increased eosinophils), crypt abscess / destruction and apoptosis
- References: Am J Surg Pathol 2015;39:1661, Am J Surg Pathol 2015;39:1653
Microscopic (histologic) images
Positive stains
- Intraepithelial lymphocytes are positive for CD8 and TCR alpha / beta (Am J Surg Pathol 2015;39:1653)
Negative stains
- CMV, adenovirus, HHV6 (Am J Surg Pathol 2015;39:1653)
Sample pathology report
- Left colon, biopsy:
- Colonic mucosa with mild acute cryptitis, mucosal eosinophilia, intraepithelial lymphocytes and prominent crypt apoptosis (see comment)
- Comment: The patient's clinical history of refractory follicular lymphoma and treatment with idelalisib are noted. The histologic findings are likely consistent with idelalisib associated colitis.
Differential diagnosis
- Graft versus host disease (GVHD):
- Additional clinical history of a lack of stem cell transplant is perhaps the most helpful in excluding GVHD (Am J Surg Pathol 2015;39:1653)
- Autoimmune enteropathy:
- Predominantly neutrophilic (versus eosinophilic) cryptitis and crypt abscesses, as well as a complete absence of goblet cells (Am J Surg Pathol 2015;39:1653)
- Inflammatory bowel disease (IBD):
- Crypt apoptosis is not typical for inflammatory bowel disease
- Presence of eosinophils within crypt abscesses and the finding of dilated, damaged crypts is more suggestive of a drug related process
- Chronic injury is absent or mild in idelalisib associated colitis
- Mild architectural distortion in the form of few branching crypts may be present but basal plasmacytosis, Paneth cell metaplasia and thickening with splaying of the muscularis mucosae are not observed (Am J Surg Pathol 2015;39:1653)
- Common variable immunodeficiency (CVID):
- May exhibit almost identical histologic features, although cryptitis is not typical for common variable immunodeficiency
- Common variable immunodeficiency demonstrates a paucity or complete absence of plasma cells (Am J Surg Pathol 2015;39:1653)
- Celiac disease:
- Presence of cryptitis and apoptosis are not typical for celiac disease and may help with this distinction (Am J Surg Pathol 2015;39:1653)
- Cytomegalovirus (CMV) and other infectious enterocolitides:
- Relatively mild chronic changes with comparatively prominent features of active injury may suggest an infectious colitis
- Increased eosinophils within the lamina propria and within crypt abscesses suggest a drug related process (Am J Surg Pathol 2015;39:1653)
Additional references
Board review style question #1
A 68 year old man was admitted for evaluation of chronic dehydration, diarrhea, abdominal pain and weight loss for > 1 month (~20 lbs). He has a history of relapsed follicular lymphoma and has been on Zydelig (idelalisib) for ~11 months. Which of the following favors idelalisib associated colitis over inflammatory bowel disease?
- Basal plasmacytosis
- Epithelial cell apoptosis
- Paneth cell metaplasia
- Splaying of muscularis mucosae
Board review style answer #1
B. Epithelial cell apoptosis. Crypt apoptosis is a common feature associated with idelalisib associated colitis and is less commonly seen in patients with inflammatory bowel disease.
Comment Here
Reference: Idelalisib associated colitis
Comment Here
Reference: Idelalisib associated colitis
Board review style question #2
A 56 year old man with a history of relapsed follicular lymphoma status postallogenic bone marrow transplant who developed severe diarrhea with a skin eruption mimicking graft versus host disease (GVHD) 6 months after starting idelalisib. Which of the following histological findings is indicative of idelalisib associated colitis?
- Basal plasmacytosis
- Increased eosinophils within the lamina propria and crypt abscesses
- Lack of apoptosis
- Severe chronic injury
Board review style answer #2
B. Increased eosinophils within the lamina propria and crypt abscesses. Idelalisib associated colitis closely mimics graft versus host disease and can be challenging to distinguish. The presence of prominent neutrophilic cryptitis and crypt abscesses can be helpful to favor idelalisib associated colitis.
Comment Here
Reference: Idelalisib associated colitis
Comment Here
Reference: Idelalisib associated colitis