Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Enteroaggregative E. coli (EAEC) | Shiga toxin producing E. coli (STEC) / enterohemorrhagic E. coli (EHEC) | Enteroinvasive E. coli (EIEC) | Enteropathogenic E. coli (EPEC) | Enterotoxigenic E. coli (ETEC) | Diffusely adherent E. coli (DEAC) | Adherent invasive E. coli (AIEC) | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ullah AM, Lee L. Escherichia coli. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonecoli.html. Accessed March 31st, 2025.
Definition / general
- Escherichia coli (E. coli) is a gram negative, facultative anaerobic, coliform, rod shaped bacterium
- It is a part of the normal flora of the intestine of humans and many warm blooded animals; it provides benefits such as production of vitamin K2 and a stable environment where more beneficial bacteria can prosper (Elife 2015;4:e05826)
- Most cases are transmitted through contaminated food and water
Essential features
- Most cases cause self limiting disease
- Treatment is supportive
Terminology
- Enteroaggregative E. coli (EAEC)
- Shiga toxin producing E. coli (STEC) / enterohemorrhagic E.coli (EHEC)
- Enteroinvasive E. coli (EIEC)
- Enteropathogenic E. coli (EPEC)
- Enterotoxigenic E. coli (ETEC)
- Diffusely adherent E. coli (DEAC)
- Adherent invasive E. coli (AIEC)
ICD coding
- ICD-10:
- B96.20 - unspecified Escherichia coli (E. coli) as the cause of diseases classified elsewhere, Escherichia coli (E. coli), NOS
- B96.21 - Shiga toxin producing Escherichia coli (E. coli) (STEC) O157 as the cause of diseases classified elsewhere
- B96.22 - other specified Shiga toxin producing Escherichia coli (E. coli) (STEC) as the cause of diseases classified elsewhere
- B96.23 - unspecified Shiga toxin producing Escherichia coli (E. coli) (STEC) as the cause of diseases classified elsewhere
- B96.29 - other Escherichia coli (E. coli) as the cause of diseases classified elsewhere, non-Shiga toxin producing E. coli
Enteroaggregative E. coli (EAEC)
- Pattern of adherence characterized by self agglutination, called aggregative adherence, in a stacking pattern
- Affects children (usually < age 2 years) and adults, immunocompromised and HIV+ (in developing and developed countries)
- Also immunocompetent and those without foreign travel
- EAEC adheres to intestinal mucosa and forms a mucoid biofilm
- Common cause of persistent watery diarrhea > 14 days (Clin Infect Dis 2006;43:402, J Infect Dis 1989;159:1061)
- Also fever, abdominal pain
- Laboratory: lactose fermenter, indole positive, citrate negative
- References: J Med Microbiol 2007;56:4, Lancet 1991;337:262, Koneman: Koneman's Color Atlas and Textbook of Diagnostic Microbiology, 6th Edition, 2005
Shiga toxin producing E. coli (STEC) / enterohemorrhagic E. coli (EHEC)
- Major foodborne pathogen (ground beef and salami, unpasteurized milk and juice, sprouts, lettuce)
- Also due to contact with cattle, swimming in contaminated waters
- Most common E. coli strain producing disease in the U.S.
- Serotype O157:H7 is most commonly isolated strain, infectious dose is 100 bacterial cells or less
- Due to verotoxin, Shiga-like toxin in O157:H7 strains
- Symptoms: abrupt onset of abdominal pain, vomiting and bloody diarrhea 3 - 4 days following ingestion with absence of fever
- Complications: up to 10% of patients, especially children under 15 years of age, may develop hemolytic uremic syndrome (HUS), usually 5 - 10 days after onset of diarrhea with up to 5% mortality rate
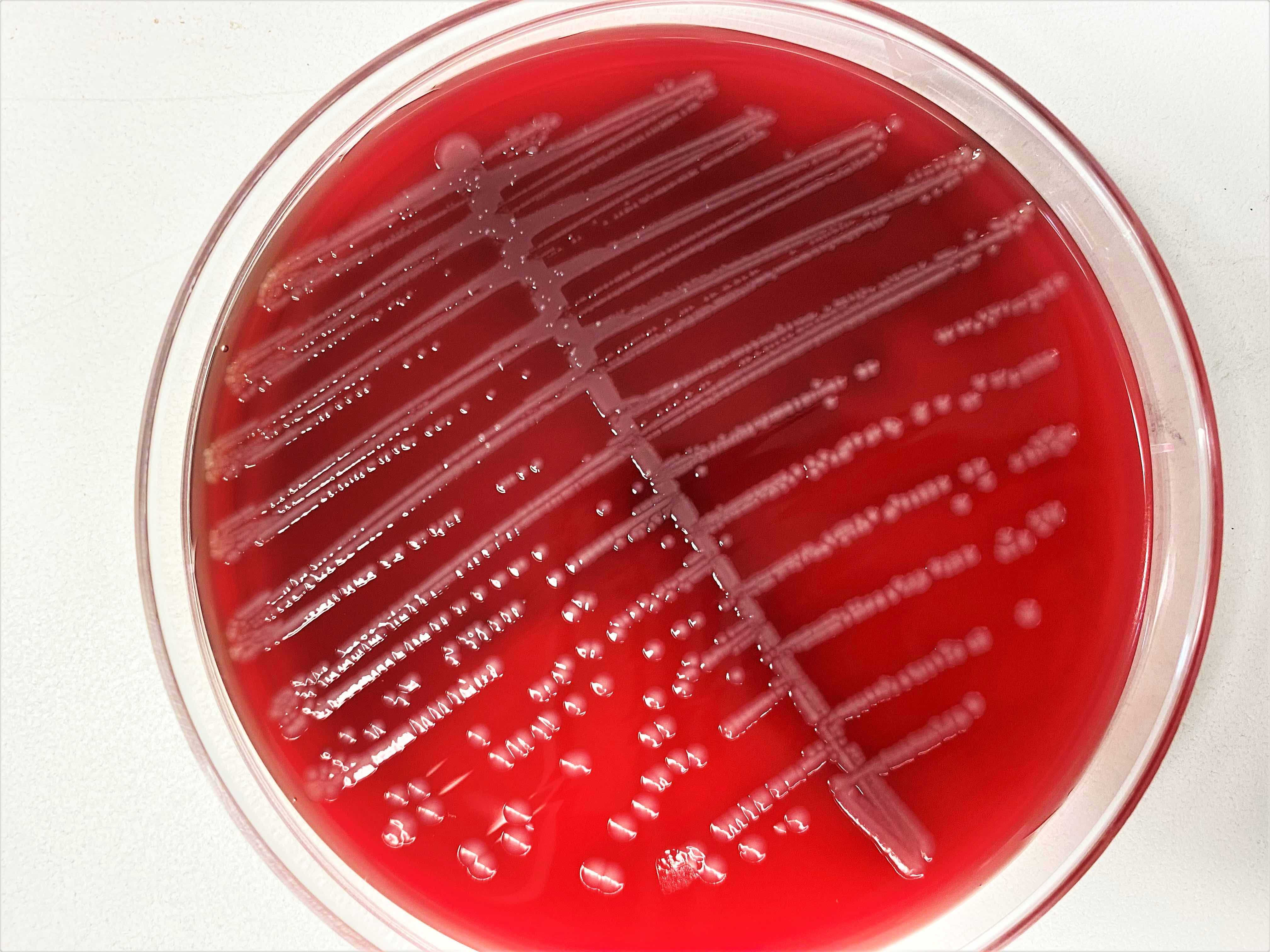
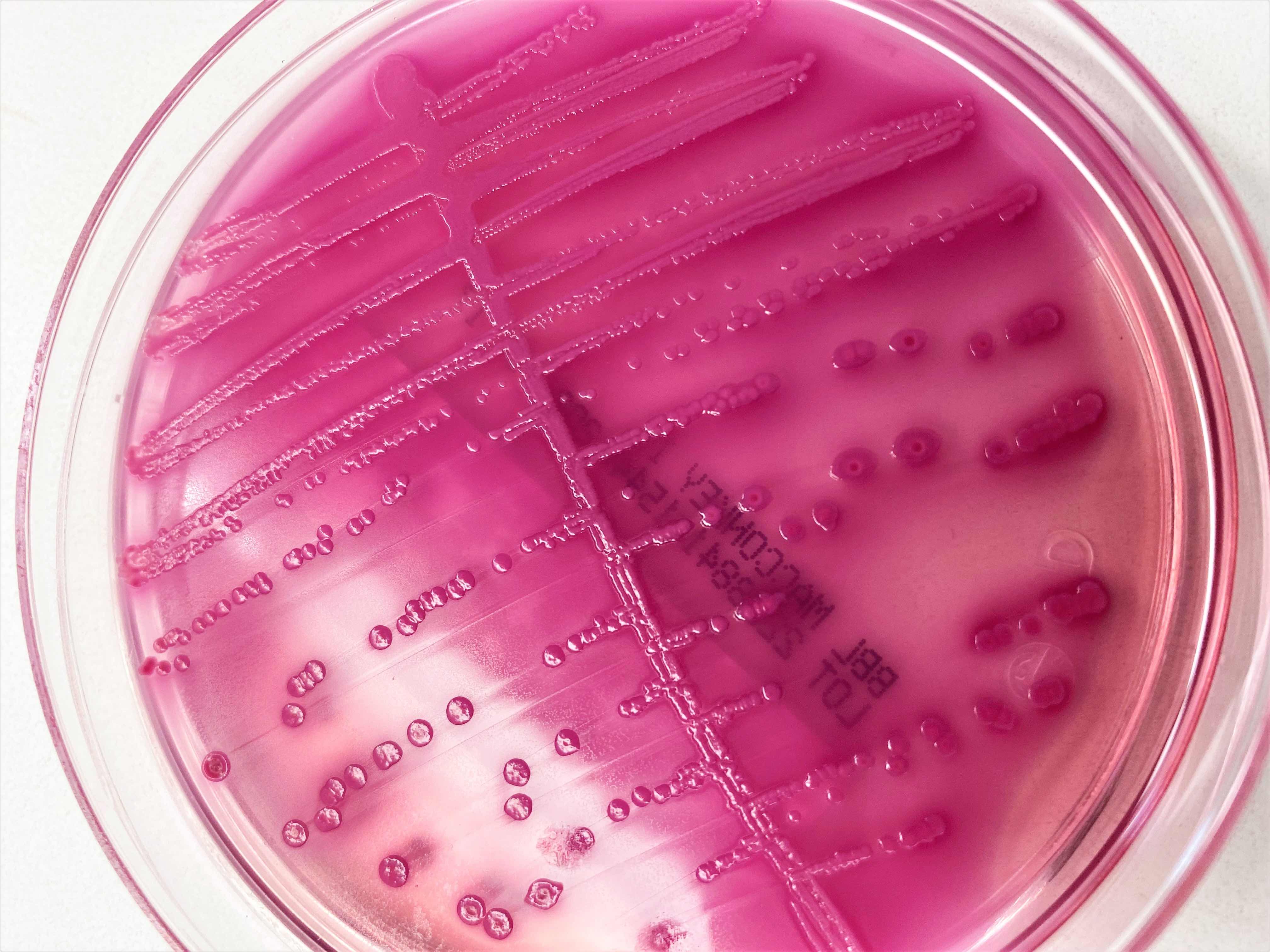
- Diagnosis: PCR, enzyme immunoassay or culture on sorbitol MacConkey agar (Mol Cell Probes 2006;20:31, J Clin Microbiol 2004;42:1652)
- Laboratory: lactose fermenter, indole positive, citrate negative, colorless growth (sorbitol nonfermenter) on sorbitol MacConkey
- Treatment
- Supportive therapy for HUS (platelets contraindicated), possibly with dialysis or plasmapheresis
- Avoid usage of antiemetic or antiperistaltic agents
- Antibiotics are not beneficial
- Microscopic description
- Necrosis of superficial mucosa, acute inflammation
- Necrotic foci may appear as pseudomembranous inflammation (usually not endoscopically visible)
- Cryptitis and crypt abscesses
- Hemorrhage and edema in lamina propria, capillary thrombosis
- References: Iowa State University: Enterohemorrhagic Escherichia coli and Other E. coli Causing Hemolytic Uremic Syndrome [Accessed 22 February 2023], Infect Immun 2007;75:4199, UpToDate: Shiga Toxin-Producing Escherichia coli - Clinical Manifestations, Diagnosis, and Treatment [Accessed 22 February 2023]
Enteroinvasive E. coli (EIEC)
- Causes dysentery-like syndrome with fever
- Due to contaminated food, water or person to person spread
- Endemic to developing nations with rare outbreaks in industrialized countries
- Reported outbreaks in the U.S. primarily affect children under 5 years of age (Ryan: Sherris Medical Microbiology, 5th Edition, 2010, Ryan: Sherris Medical Microbiology, 4th Edition, 2003)
- Infectious dose for healthy adults is 106
- Similar molecular features to Shigella, due to virulence plasmid that encodes determinants (specific adhesion, outer membrane protein) for entry into epithelial cells and dissemination from cell to cell (Infect Immun 2004;72:5080)
- Invades and destroys colonic epithelium
- Laboratory: lactose fermenter and nonfermenters; lysine decarboxilase negative; nonmotile
- Treatment: generally self limited; fluid replacement as necessary
- Trimethoprim / sulfamethoxazole (TMP SMX) or quinolones may reduce duration of diarrhea
- Micro description: bacterial invasion and destruction of colonic mucosa resulting in inflammation and ulceration
- References: Clin Microbiol Rev 1998;11:142, Am J Trop Med Hyg 2007;76:528, Todar: Todar's Online Textbook of Bacteriology, 2020
Enteropathogenic E. coli (EPEC)
- Some types of EPEC are known as diffusely adherent E. coli (DAEC)
- Major cause of infant diarrhea in developing countries
- Due to contaminated water and meat products
- Virulence mechanism is unrelated to excretion of typical E. coli enterotoxins; diarrhea and symptoms are caused by invasion of host cells (attachment and effacement) rather than by production of toxins
- Has pathogenicity island that encodes proteins which modulate the actin microtubule and intermediate filament networks to allow intimate attachment of bacteria to plasma membrane of infected enterocytes, forming attachment and effacing lesions (J Bacteriol 2006;188:3110)
- Also has large plasmid that contains a cluster of genes encoding bundle forming pili
- Infectious dose is 106 organisms
- Atypical cases lack bundle forming pili and are associated with prolonged diarrhea (Emerg Infect Dis 2006;12:597)
- Clinical features:
- Infantile diarrhea may lead to dehydration, electrolyte imbalance or death
- Watery or bloody diarrhea
- Up to 50% mortality rates in developing countries
- Treatment: self limited; antibiotics may not improve disease and may increase the risk of developing hemolytic uremic syndrome
- Micro description: effacement of brush border microvilli of enterocytes; no bacterial invasion but surface adherent organisms may be identifiable
- References: Food and Drug Administration: Bad Bug Book - Foodborne Pathogenic Microorganisms and Natural Toxins, 2nd Edition, 2012, Todar: Todar's Online Textbook of Bacteriology, 2020, Microbiology (Reading) 2004;150:527, Emerg Infect Dis 2002;8:508
Enterotoxigenic E. coli (ETEC)
- Annually causes 200 million diarrhea episodes and 170,000 to 380,000 deaths, due to contaminated food and water
- Most common cause of traveler's diarrhea (CDC: Enterotoxigenic E. coli (ETEC) [Accessed 15 March 2023])
- Also a leading cause of infant diarrhea in developing countries
- Emerging cause of diarrhea in the U.S. (Rev Environ Health 2008;23:135)
- Due to enterotoxins (heat labile [LT] and heat stable [ST]) produced by noninvasive bacteria that adhere to small intestine and produce cholera-like watery diarrhea
- Strains that can produce both enterotoxins cause more severe diarrhea
- Causes profuse watery diarrhea, abdominal cramping, fever, nausea
- Treatment: prophylaxis with rifaximin, careful food / beverage selection, rehydration
- Drugs vary based on current patterns of antimicrobial resistance; vaccines are currently being tested (Drugs 2006;66:303, Clin Vaccine Immunol 2012;19:1921)
- Micro description: often does not cause inflammation due to its noninvasive nature
- References: Clin Microbiol Rev 2006;19:583, Clin Microbiol Rev 2005;18:465, CDC: Enterotoxigenic E. coli (ETEC) [Accessed 22 February 2023]
Diffusely adherent E. coli (DEAC)
- Extremely heterogeneous group of potentially pathogenic E. coli, which are characterized by their diffuse adherence to epithelial cells
- DAEC isolates are detected not only in humans commonly in children of between 2 and 5 years of age but also in various groups of animals (dogs, calves, cattle, poultry, pigs)
- No diarrheal disease has been reported in adults but the latest data indicates a possible contribution of DAEC strains in the process of the development of colorectal cancer and Crohn's disease (CD) (Clin Microbiol Rev 2014;27:823, Advancements of Microbiology 2019;58:143)
- On the basis of adhesins, DAEC strains have been divided into 2 basic groups: typical DAEC (which binds to the hDAF receptor) and atypical DAEC (which does not bind the hDAF factor)
- DAEC are omitted in the routine diagnosis of infections of the digestive tract due to the huge genotypic diversity of these strains
- Optimum method for diagnosis of DEAC is still under active research; the lack of commonly available diagnostic methods hinders the correct identification of infections caused by DAEC and therefore, the possibility of treatment (BMC Microbiol 2013;13:22, Front Cell Infect Microbiol 2020;10:572951)
Adherent invasive E. coli (AIEC)
- Adherent invasive Escherichia coli (AIEC) pathobiont bacteria have the ability to adhere to and invade intestinal epithelial cells (IECs) as well as to survive and replicate within macrophages
- AIEC bacteria have been linked in the etiology of CD; however, active genetic research is ongoing in order to better establish this link and develop possible treatment modalities to prevent and limit AIEC colonization in CD patients (Int J Mol Sci 2020;21:3734)
Epidemiology
- In the U.S., most outbreaks have been reported in Minnesota, followed by Washington
- Route of transmission is foodborne; mainly by undercooked ground beef in EHEC (Emerg Infect Dis 2005;11:603)
- ETEC organisms are the principal cause of traveler's diarrhea and spread via contaminated food or water
- EIEC / EAEC organisms are bacteriologically similar to Shigella and are transmitted via food, water or by person to person contact
Sites
- Colon and rectum
Pathophysiology
- Depends on the strain of pathogenic E. coli
- Enteroaggregative E. coli
- EAEC adhere to epithelial cells
- EAEC attach to enterocytes via adherence fimbriae and are aided by dispersin, a bacterial surface protein that neutralizes the negative surface charge of lipopolysaccharide
- They also produce enterotoxins similar to Shigella enterotoxin and ETEC ST toxin (Curr Opin Gastroenterol 2005;21:4)
- Enterohemorrhagic E. coli / Shiga toxin producing E. coli (STEC)
- EHEC are classified as E. coli O157:H7 and non-O157:H7 serotypes
- Both serotypes produce Shiga-like toxins
- Hemolytic uremic syndrome (HUS) is caused by Shiga-like toxin which is absorbed by inflamed gastrointestinal mucosa into the circulation, where it alters endothelial cell function leading to platelet activation and aggregation
- Children and the elderly are at highest risk (Med Clin North Am 2013;97:681)
- Enteroinvasive E. coli
- EIEC do not produce toxins, they invade epithelial cells and cause acute self limited colitis (J Vet Sci 2022;23:e28)
- Enterotoxigenic E. coli
- ETEC produce LT toxin and ST toxin
- Both induce chloride and water secretion while inhibiting intestinal fluid absorption
- LT toxin activates adenylate cyclase and stimulates chloride secretion and simultaneously inhibits absorption
- ST toxins bind to guanylate cyclase and stimulate chloride secretion (Gut Microbes 2022;14:2055943)
- Enteroaggregative E. coli
Etiology
- Contaminated food and water
Clinical features
- EAEC organisms cause nonbloody diarrhea that may be prolonged in AIDS patients (Am J Trop Med Hyg 2010;83:158)
- EHEC causes symptoms similar to S. dysenteriae
- Causes large outbreaks of bloody diarrhea and HUS
- HUS includes microangiopathic hemolytic anemia and thrombocytopenia but no neurologic symptoms and no acute renal failure (Med Clin North Am 2013;97:681)
- EIEC is common among young children in developing countries
- Also causes traveler's diarrhea and diarrhea in both children and adults (J Vet Sci 2022;23:e28)
- ETEC causes traveler's diarrhea commonly in underdeveloped regions and children younger than 2 years of age are particularly susceptible
- Secretory, noninflammatory diarrhea, vomiting, dehydration and in severe cases, shock (Gut Microbes 2022;14:2055943)
Diagnosis
- Typically made by clinical findings and history of ingestion of contaminated food like undercooked meat
Laboratory
- Stool culture on sorbitol MacConkey agar (SMAC) or the variant cefixime potassium tellurite sorbitol MacConkey agar (CT SMAC)
- Colonies appear clear on SMAC due to their inability to ferment sorbitol, while sorbitol fermenting colonies of E. coli serotypes appear red
- E. coli DNA extraction method: DNA probes plus PCR techniques for detecting verocytotoxin (MMWR Recomm Rep 2009;58:1, StatPearls: Escherichia Coli [Accessed 1 June 2023])
Radiology description
- CT is usually preferred modality for radiological assessment (AJR Am J Roentgenol 2001;177:619)
- Shows severe diffuse colonic wall thickening, often with a target sign and pericolic stranding
- Involvement of bowel can be segmental or diffuse
Radiology images
Prognostic factors
- Disease is usually self limiting and patients recover on supportive therapy
Case reports
- 32 year old woman with infection due to Shiga toxin producing enterohemorrhagic Escherichia coli (EHEC) presenting as ischemic colitis (IDCases 2019;18:e00629)
- 36 year old woman with severe ulcerative colitis and Coronavirus disease 2019 followed by Escherichia coli 0157:H7 infection (Croat Med J 2021;62:634)
- 75 year old man with pseudomembranous colitis-like lesions associated with hemolytic uremic syndrome and neurological sequelae (BMJ Case Rep 2017;2017:bcr2016218586)
Treatment
- Treatment is mainly supportive
- Antibiotic use with STEC infections is not recommended (Clin Infect Dis 2016;62:1251)
Gross description
- EHEC: colonic mucosa is edematous and erythematous with multiple erosions
- Erosion may show adherent blood clots (Virulence 2013;4:366)
Microscopic (histologic) description
- EAEC, EIEC, ETEC
- No significant microscopic changes
- EHEC
- Foci of epithelial cell damage / necrosis with pyknotic nuclei, vacuolated cytoplasm
- Areas of hemorrhage within lamina propria
Positive stains
- E. coli are gram negative bacilli
Electron microscopy description
- Transmission electron microscopy, in cases of EHEC, shows pyknotic nuclei, damaged membranes and cytoplasmic vacuolization of colonic epithelial cells
Sample pathology report
- Left colon, colectomy:
- Colonic mucosa with focal active colitis, surface erosions and focal areas of hemorrhage (see comment)
- Comment: Focal active colitis pattern is a nonspecific histologic finding that may be seen in association with a variety of conditions. The most common clinical diagnoses rendered upon follow up of patients with a focal active colitis pattern include acute self limited / infectious colitis, irritable bowel syndrome, Crohn's disease, ischemic colitis, antibiotic associated colitis, NSAID related colitis, diverticular disease associated colitis, etc.
Differential diagnosis
- Ischemic colitis:
- Negative culture for E. coli; no significant history
- Other infective colitis:
- Negative culture for E. coli
Additional references
Board review style question #1
Which E. coli strain has been implicated as a possible precursor to the development of colorectal cancer?
- Adherent invasive E. coli (AIEC)
- Diffusely adherent E. coli (DEAC)
- Enteropathogenic E. coli (EPEC)
- Enterotoxigenic E. coli (ETEC)
- Shiga toxin producing E. coli (STEC)
Board review style answer #1
B. Diffusely adherent E. coli (DEAC). Diffusely adherent E. coli (DEAC) found in colons of Crohn's disease and colorectal cancer (CRC) patients have been found to harbor the daaC and afaBC genes. The afa1 positive strains isolated from these patients demonstrate adherence and invasion into various epithelial cells and also induce the increased mRNA expression of VEGF (vascular endothelial growth factor), which promotes angiogenesis in tumors. Multiple other genes and the proinflammatory effect of DEAC adhesions on intestinal epithelium has also been associated with the development of Crohn's disease and CRC according to multiple studies (Gastroenterology 2004;127:80, Advancements of Microbiology 2019;58:143, World J Gastrointest Pathophysiol 2014;5:213). No other strain of E. coli has been associated with the development of CRC.
Comment Here
Reference: Escherichia coli
Comment Here
Reference: Escherichia coli
Board review style question #2
A 45 year old woman with chronic kidney disease status post renal transplant presents to the emergency department with vomiting, bloody diarrhea and dehydration. In light of the recent E. coli O157:H7 outbreak, you suspect E. coli colitis. What is the gold standard for diagnosis?
- Cefixime potassium tellurite sorbitol MacConkey agar (CT SMAC)
- Horse blood agar
- Thayer Martin Agar (VPN agar)
- Thiosulfate citrate bile salts sucrose agar (TCBS)
Board review style answer #2
A. Cefixime potassium tellurite sorbitol MacConkey agar (CT SMAC). Cefixime potassium tellurite sorbitol MacConkey agar (CT SMAC) is a modified form of MacConkey sorbitol agar (SMAC) that contains selective agents cefixime and tellurite. Cefixime inhibits the growth of other enteric organisms, such as Proteus spp. and potassium tellurite inhibits non-O157 Shiga toxin producing E. coli (STEC). The use of CT SMAC has been associated with increased cultural sensitivity for the isolation of E. coli O157:H7. Therefore, it is recommended by the American Society of Microbiology and Centers for Disease Control and Prevention (CDC) for use as a primary isolation medium for E. coli O157:H7 in community acquired diarrhea (Versalovic: Manual of Clinical Microbiology, 10th Edition, 2011). The mechanism includes the production of pink colonies by E. coli strains other than O157:H7 through the fermentation of D sorbitol, whereas the colonies of CT SMAC are colorless after overnight incubation due to the lack of D sorbitol fermentation (ThermoFisher: MacConkey Sorbitol Agar w/ Cefixime and Tellurite [Accessed 15 March 2023).
Comment Here
Reference: Escherichia coli
Comment Here
Reference: Escherichia coli