Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez RS. Ipilimumab associated colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncolitisipilimumab.html. Accessed April 1st, 2025.
Definition / general
- Colitis caused by use of the anti-CTLA4 medication, ipilimumab
Essential features
- Colitis is a somewhat common side effect of ipilimumab
- Can be mild (diarrhea) or severe (perforation, death)
- Histology: increased intraepithelial lymphocytes, increased apoptosis, cryptitis
Epidemiology
- Occurs in up to 29% of patients taking ipilimumab, an immunologic agent used for melanoma and other malignancies (Melanoma Res 2015;25:321)
Sites
- Can affect entire gastrointestinal tract, even liver (Am J Surg Pathol 2015;39:1075)
Pathophysiology
- Causes dysregulation of gastrointestinal mucosal immunity
Clinical features
- Diarrhea, colitis
Radiology description
- Mesenteric vessel engorgement and bowel wall thickening (Am J Roentgenol 2013;200:W468)
Prognostic factors
- Side effects are dose dependent, schedule related and cumulative (Scientifica (Cairo) 2013;2013:857519)
Case reports
- 52 year old man with perforating ipilimumab associated colitis (J Surg Case Rep 2014;2014:rju010)
Treatment
- Steroids are usually effective but anti-TNF agents or surgery may be required for severe cases (Dig Dis Sci 2016;61:2132)
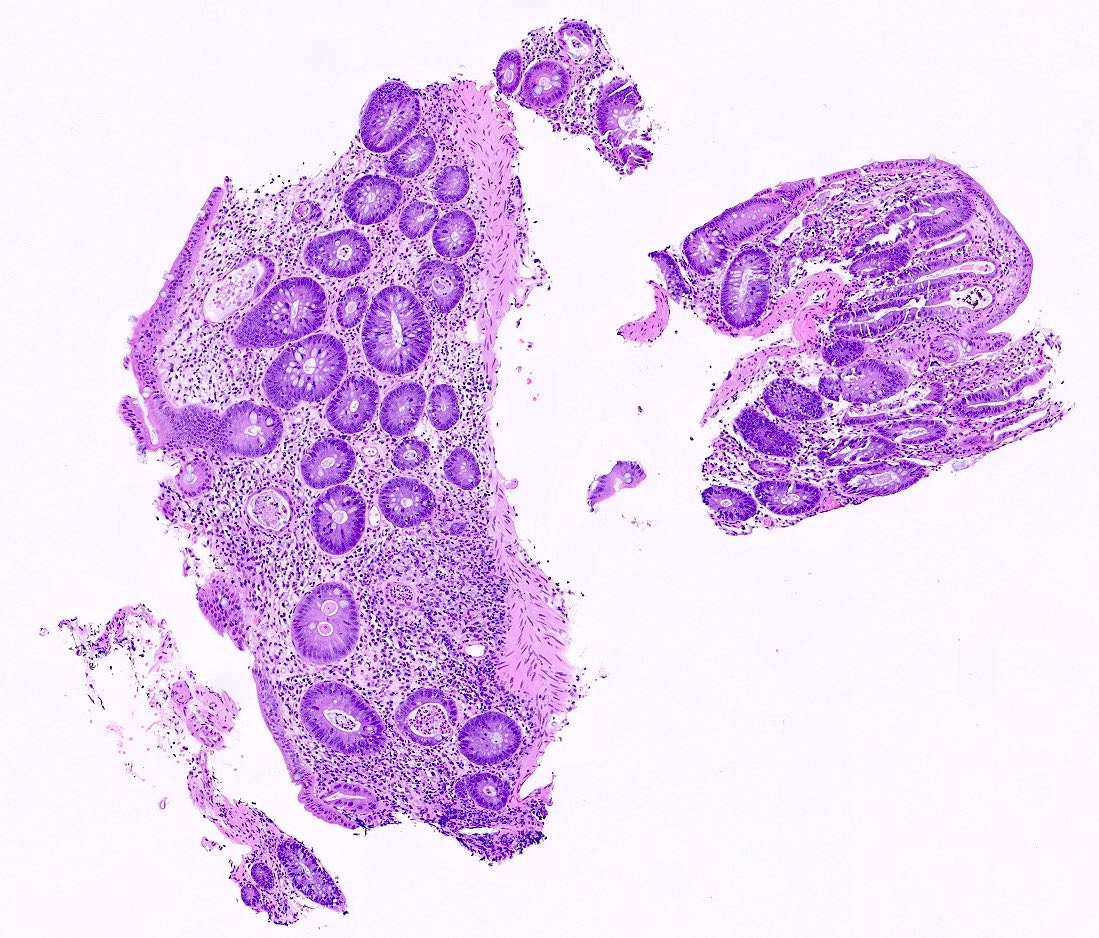
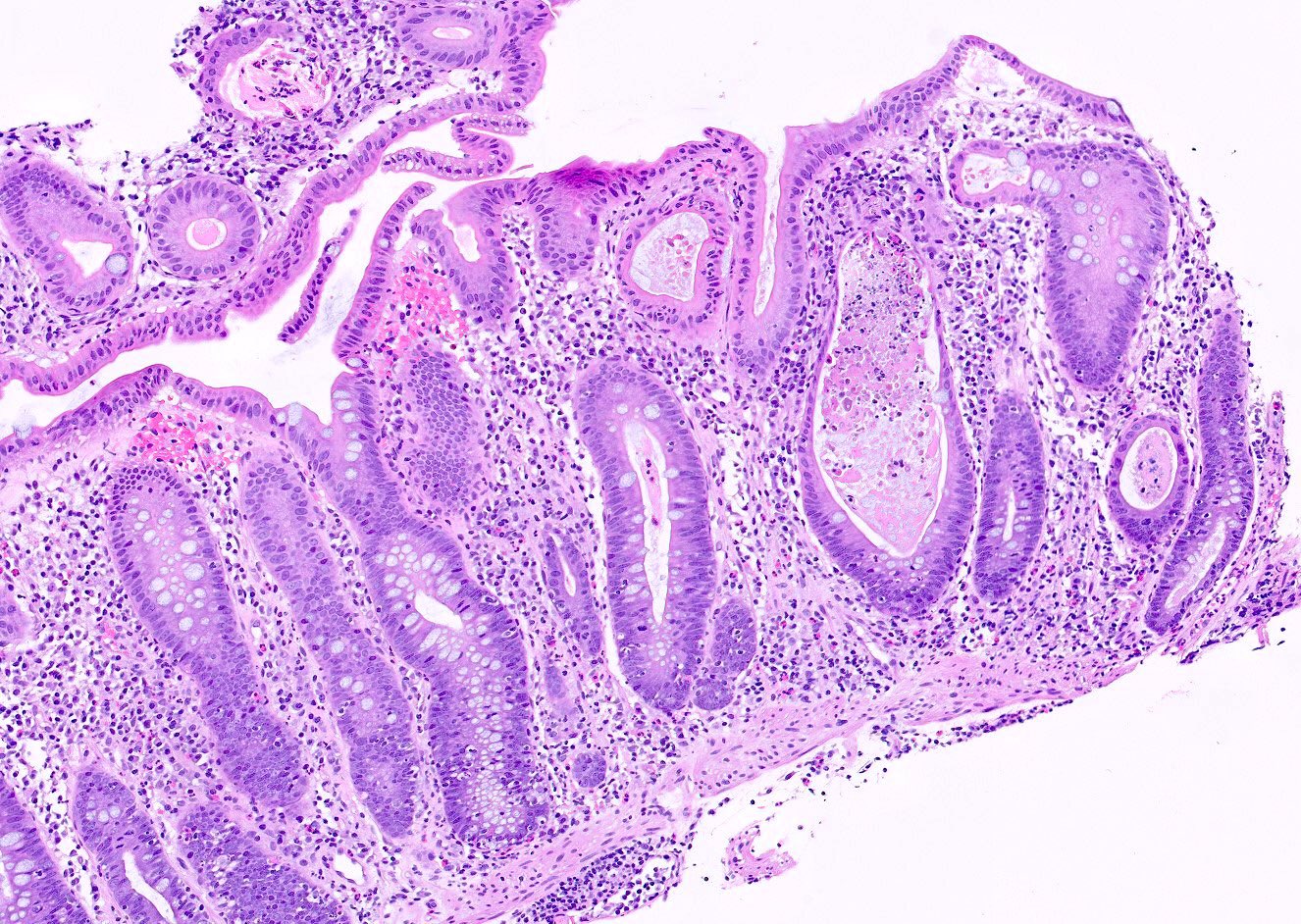
Microscopic (histologic) description
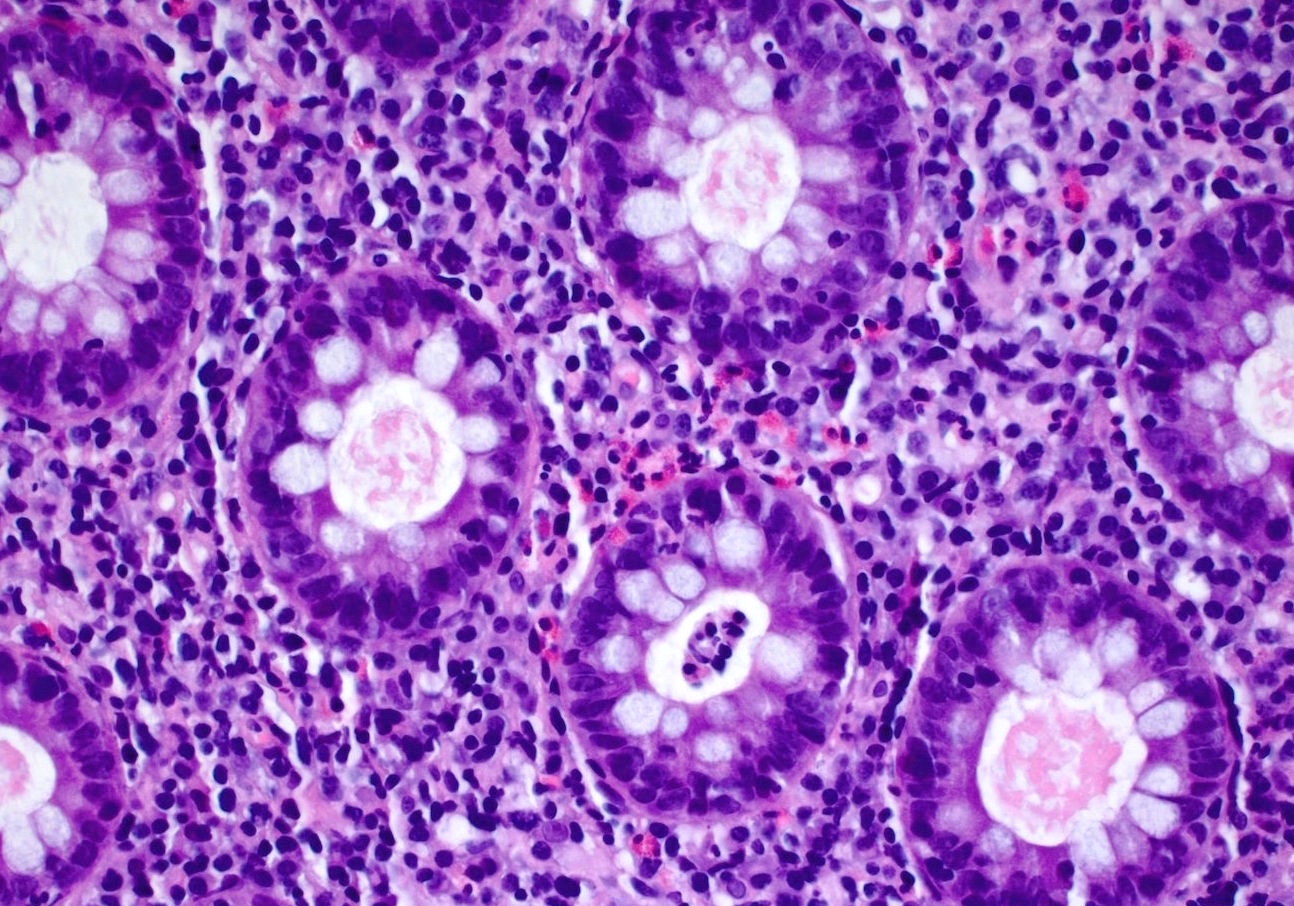
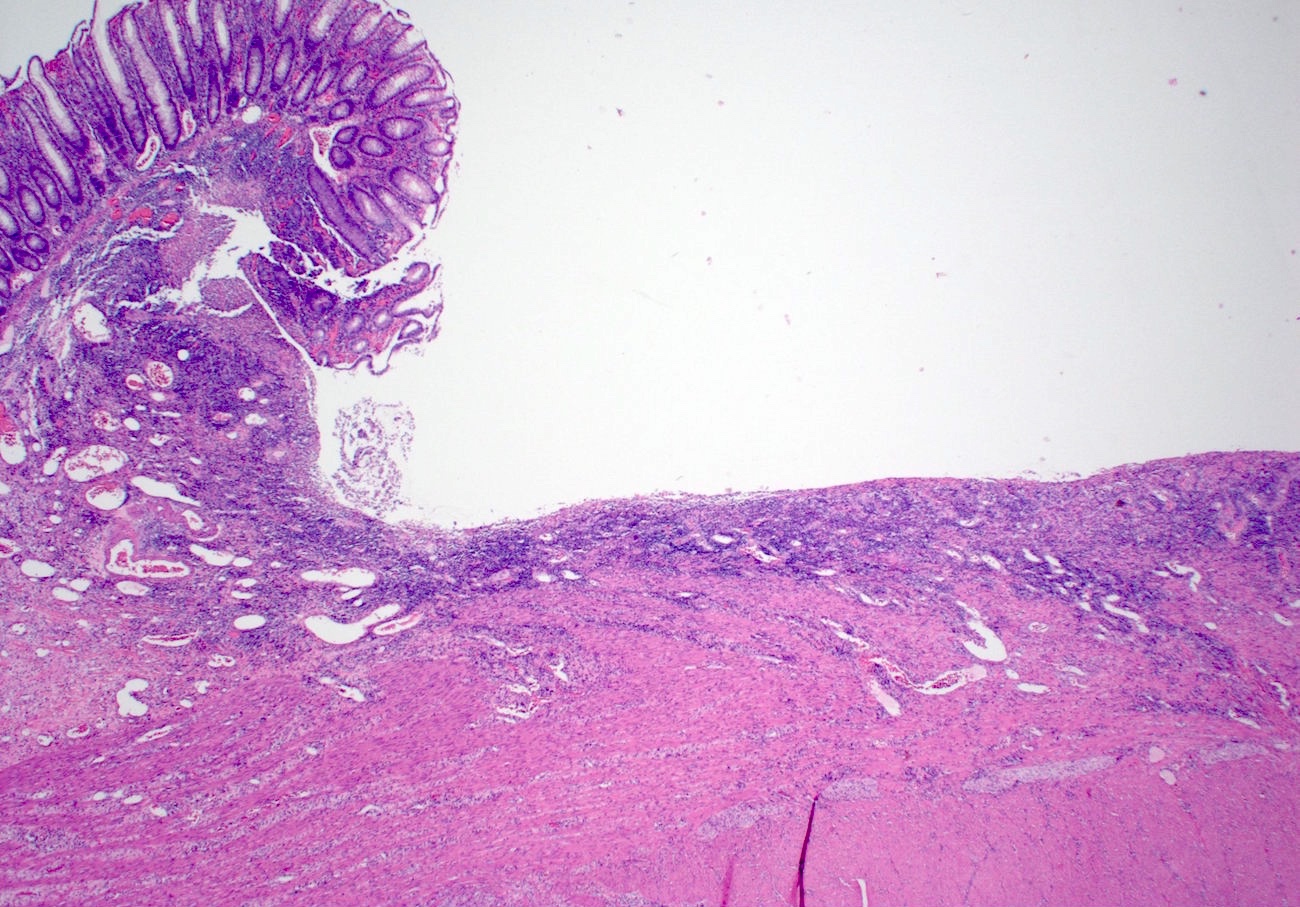
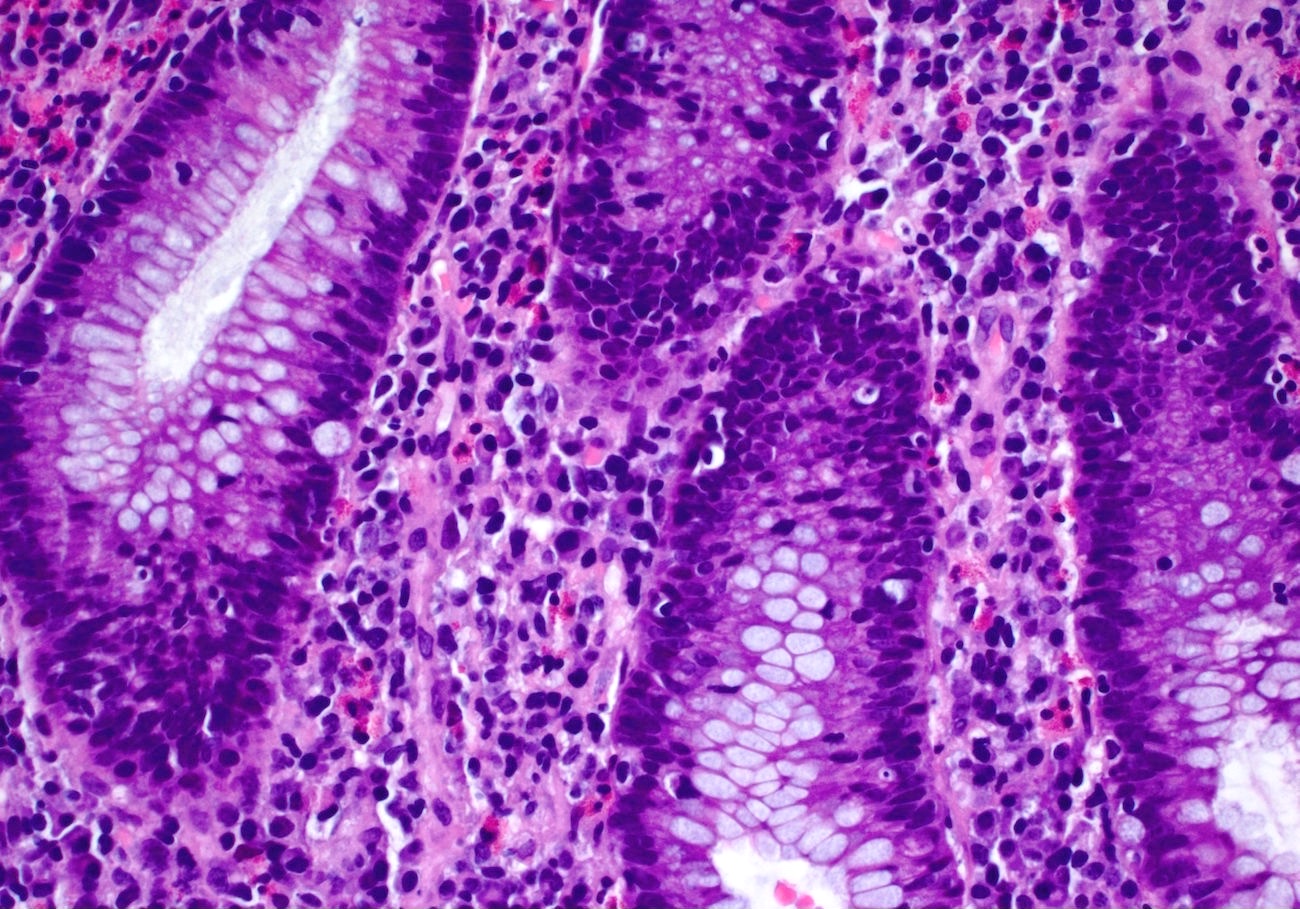
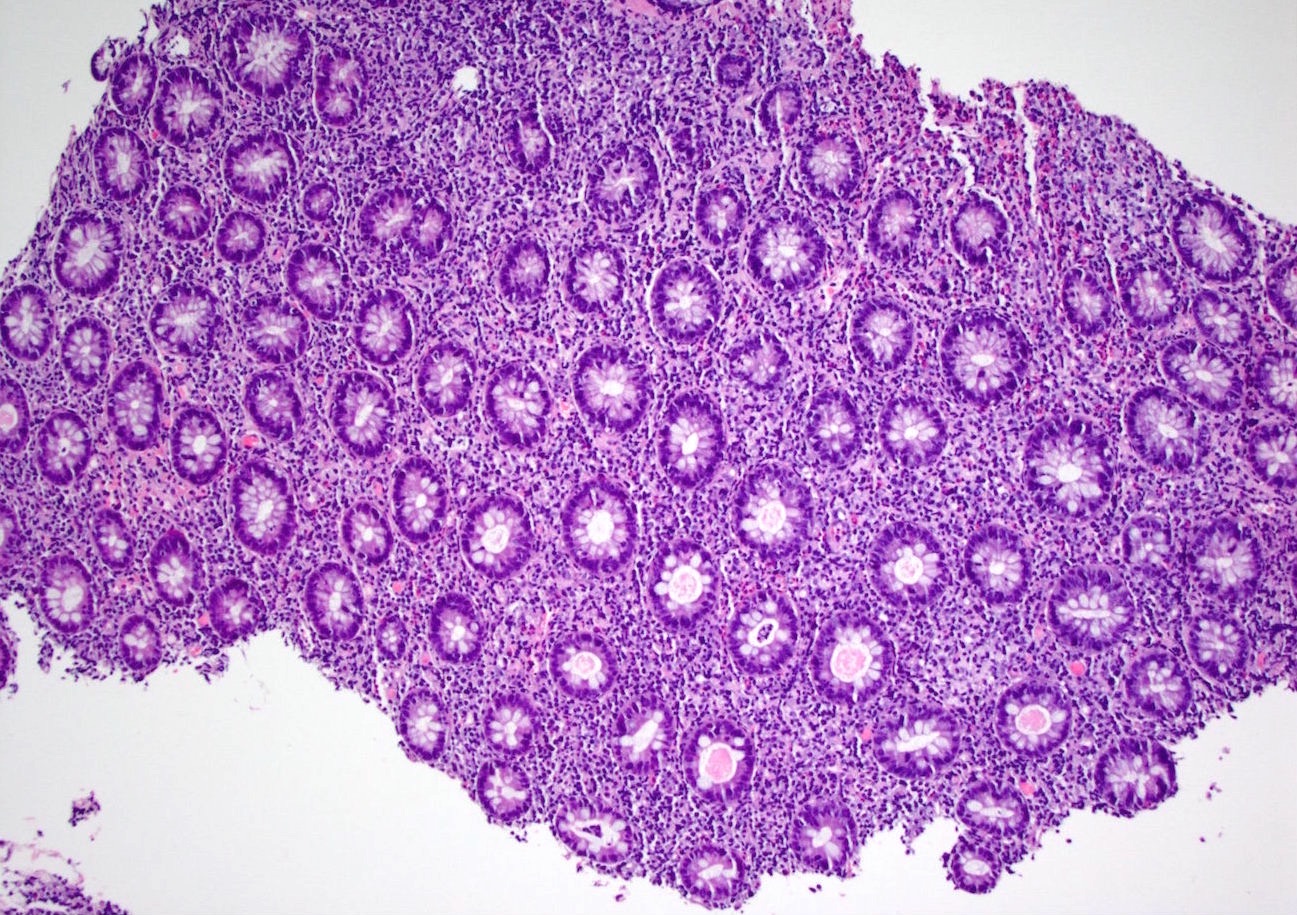
- Lymphoplasmacytic expansion of lamina propria; increased apoptosis and intraepithelial lymphocytes; cryptitis and crypt elongation (Am J Surg Pathol 2008;32:1130)
- Severe cases may show ulceration/perforation, pseudopolyp formation and crypt dilation, without lymphocytosis or apoptosis (J Clin Gastroenterol 2013;47:781)
Microscopic (histologic) images
Sample pathology report
- Sigmoid colon, biopsy:
- Colonic mucosa with mild acute inflammation, expanded lamina propria, increased intraepithelial lymphocytes and focally increased apoptosis (see comment)
- Comment: The patient's use of ipilimumab is noted. The findings are most consistent with ipilimumab associated colitis.
Differential diagnosis
- Inflammatory bowel disease:
- Less apoptosis; signs of chronicity
- Idelalisib associated colitis:
- Also caused by immune modulation (PI3K inhibitor); similar histology; history probably necessary for distinction (Am J Surg Pathol 2015;39:1661)
- Anti-PD1 associated colitis:
- Also caused by immune modulation; similar histology; history probably necessary for distinction (Am J Surg Pathol 2017;41:643)
Board review style question #1
Which of the following is true about gastrointestinal tract injury secondary to ipilimumab use?
- It can cause ulceration and perforation
- It is an extremely rare side effect
- It only occurs in the colon
- The main histologic findings are Paneth cell metaplasia and a thickened basement membrane
Board review style answer #1
Board review style question #2
A 55 year old man with a history of metastatic melanoma presents with diarrhea and undergoes colonoscopy, which finds musical erythema. A biopsy is taken, with histology shown above. What is the most likely diagnosis?
- Ipilimumab induced colitis
- Lymphocytic colitis
- Segmental colitis associated with diverticulosis
- Ulcerative colitis
Board review style answer #2