Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Differential diagnosisCite this page: Bansal N. Candida. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncandida.html. Accessed April 1st, 2025.
Definition / general
- Candida colonies are normal commensals of the gastrointestinal tracts and rarely pathogenic in gut
- Candida infections are usually seen in immunocompromised and debilitated patients due to concurrent chronic diseases, malnutrition, use of immunosuppressive drugs or old age (Int J Contemporary Medical Research 2017;4:76)
- In immunocompetent patients, low pH, regular use of antacids as well as hyperglycemia can cause the yeast to break through the intestinal mucosal barrier and lead to invasive candidiasis and candidemia (Dtsch Arztebl Int 2009;106:837)
Essential features
- Candida colonies are normal commensals of gastrointestinal tracts
- Infections are usually seen in immunocompromised and debilitated patients
- Factors favoring fungal proliferation include: regular antacid use, which lowers pH; use of antibiotics, which diminish useful bacteria; and hyperglycemia, as seen with diabetes
- Candida usually causes mucosal lesions; rarely perforations
- Esophagus is the most commonly affected site in GI
- Gold standard test for diagnosis is culture
- Antifungals are treatment of choice
ICD coding
- B37.8 - Candidiasis of other sites
Epidemiology
- Patients usually middle aged to elderly, with an average age of 65 years
Sites
- Most commonly affected organ is the esophagus, followed by the stomach, the small intestine and the large intestine (Medicine (Baltimore) 1972;51:367, Nihon Shokakibyo Gakkai Zasshi 1986;83:2341)
Pathophysiology
- Under normal conditions, there is homeostasis between C. albicans and the host; however, if the balance is disrupted by low pH, regular use of antacids or hyperglycemia, the yeast can break through the intestinal mucosal barrier and cause invasive candidiasis and candidemia (Dtsch Arztebl Int 2009;106:837)
Etiology
- Candida albicans most commonly; rarely C. tropicalis, C. parapsilosis and C. kefyr (Emerg Med (Los Angel) 2015;5:264)
Diagrams / tables
Clinical features
- Invasive Candida infections are characterized by fever and shock along with low blood pressure, abdominal pain, rigors, an elevated heart rate, respiratory distress and multiorgan failure (Emerg Med (Los Angel) 2015;5:264)
Diagnosis
- Histopathology showing fungal hyphae and spores
- Gold standard is culture for fungi
Laboratory
- Eosinophilia
- Positive fungal culture
- Elevated levels of proinflammatory cytokine IL17 (Curr Opin Microbiol 2011;14:386)
Radiology description
- With intestinal perforation, chest Xray and Xray abdomen in erect view demonstrate gas under right hemidiaphragm
Prognostic factors
- Prognosis of Candida peritonitis is very poor in critically ill surgical patients, with a mortality rate between 52% and 75% (Curr Opin Crit Care 2007;13:195)
- Risk factors associated with increased mortality in Candida peritonitis include: extremes of age, upper GI tract infection as well as patient comorbidities, such as cardiac insufficiency, cirrhosis, diabetes mellitus, renal failure and multiorgan failure (Medicine (Baltimore) 2011:90:69)
Case reports
- 50 year old man diagnosed with acute peritonitis caused by a gastrointestinal perforation (J Clin Diagn Res 2012;6:1564)
- 50 year old man with invasive gastric candidiasis causing perforation and peritonitis (J Krishna Inst Med Sci Univ 2015;4:183)
- 54 and 62 year old women who developed systemic candidiasis (World J Emerg Surg 2013;8:38)
Treatment
- The antifungal agents for Candida peritonitis include polyenes, azoles, echinocandins and flucytosine
- Azoles are fungistatic against most Candida species, whereas the polyenes and echinocandins are fungicidal
- Fluconazole is recommended for patients without prior azole exposure and not at high risk, such as elderly, diabetic and cancer patients (Clin Infect Dis 2009;48:503, Perit Dial Int 2009;29 Suppl 2:S161)
Gross description
- Candida tends to cause mucosal lesions and produce ulcers of varying configuration, mucosal flecks, sloughed mucous membranes, polypoid masses and segmental lesions (J Clin Pathol 1992;45:806)
- With perforation, bowel may be covered by a thick, black, serosal exudate (Acta Paediatr 2003;92:258)
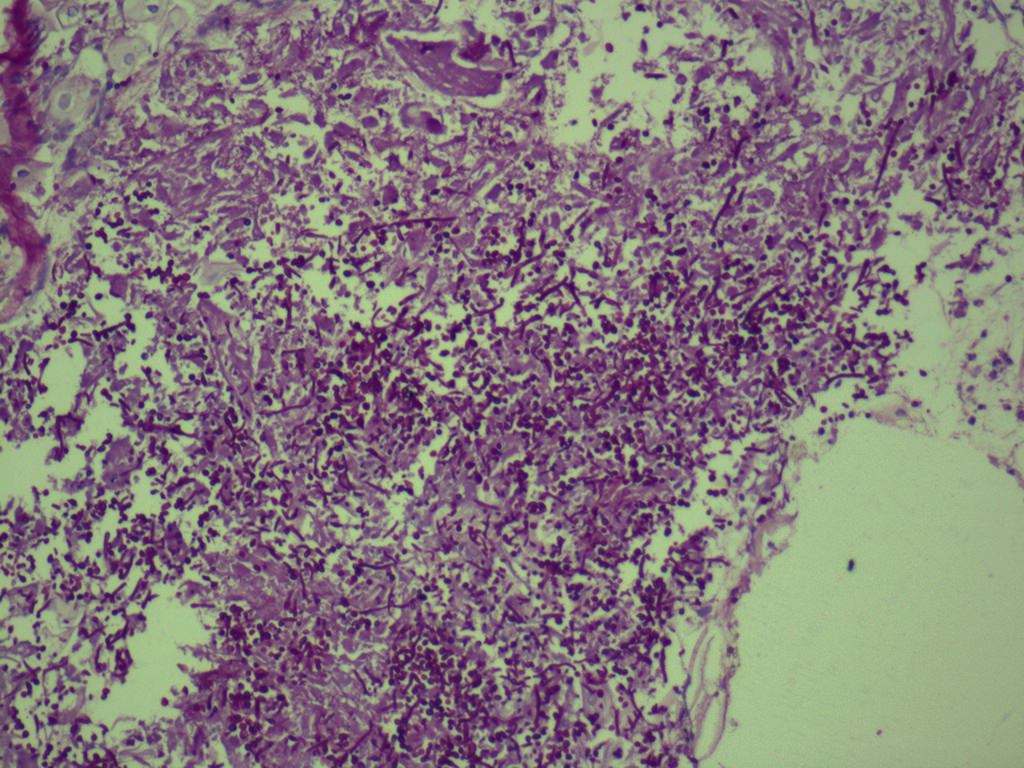
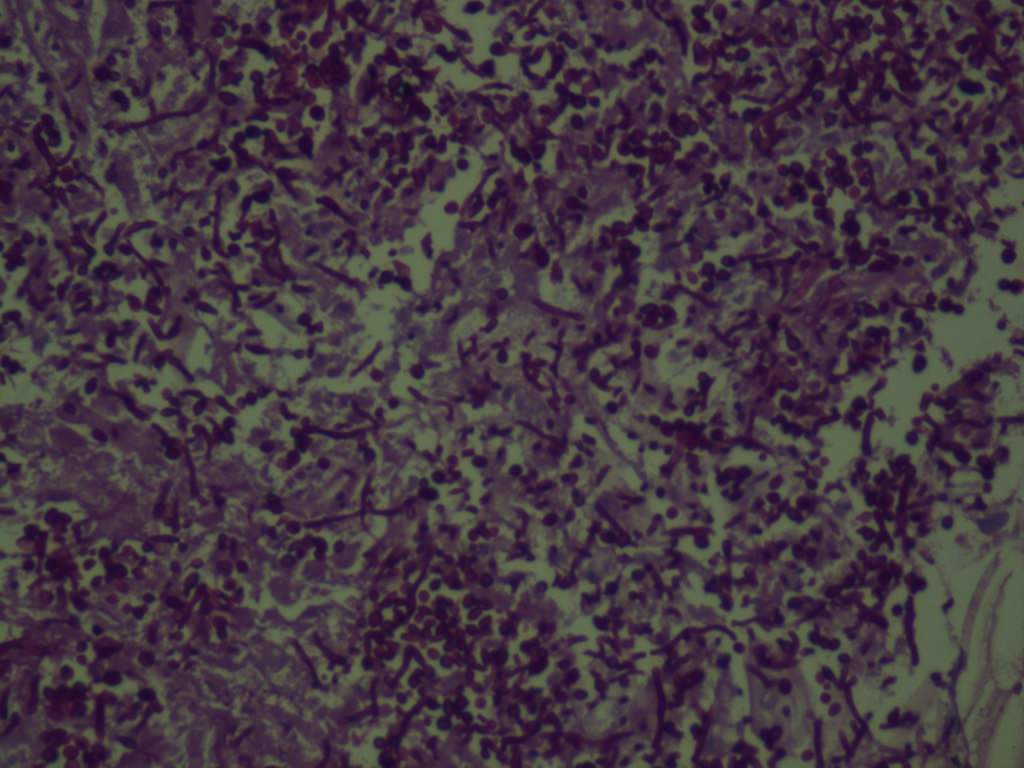
Microscopic (histologic) description
- Ulcer slough with eosinophils and neutrophils
- Classical budding hyphae and spores of Candida admixed with ulcer slough
Microscopic (histologic) images
Cytology description
- Fungal spores and hyphae
Negative stains
Differential diagnosis
- Other fungal infections
- Mucormycosis: broad aseptate hyphae
- Basidiobolomycosis: broad septate; thin walled fungal hyphae