Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Poor prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Differential diagnosisCite this page: Bansal N. Basidiobolomycosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonbasidio.html. Accessed April 2nd, 2025.
Definition / general
- Basidiobolomycosis is a rare fungal infection caused by environmental saprophyte Basidiobolus ranarum
- It is a member of the order Entomophthorales of the class zygomycetes
- The zygomycetes include two fungal orders:
- Mucorales, involving mainly immunocompromised patients, and
- Entomophthorales, which causes infection in immunocompetent individuals (J Korean Surg 2012;83:325)
- Basidiobolomycosis is endemic in tropical and subtropical regions of Africa, Latin America, Middle East and Asia (Curr Pediatr Res 2013;17:1)
- It mainly involves skin and subcutaneous tissue and rarely infects the gastrointestinal tract
- First case of visceral basidiobolomycosis (GIB) was reported in 1964 (Trans R Soc Trop Med Hyg 1964;58:242)
Essential features
- Basidiobolomycosis is a rare fungal infection caused by Basidiobolus ranarum
- Causes infection in immunocompetent individuals
- Is endemic in tropical and subtropical regions
- Mainly involves skin and subcutaneous tissue, visceral involvement is rare
- Infection is caused by ingestion of contaminated food or use of contaminated toilet paper
- Abdominal pain and fever are most common presenting features
- Histology shows broad septate thin walled fungal hyphae with the Splendore-Hoeppli phenomenon
- Culture is gold standard for diagnosis
- Treatment: combined surgery and medical therapy with antifungals
- Prognosis poor in pediatric patients
ICD coding
- B46.8 - other zygomycoses
Epidemiology
- Ages 18 months to 80 years; male to female ratio of 11:1
- Mean age 37 years (Clin Infect Dis 2012;54:1685)
Sites
- Mostly cause chronic infection in the skin and subcutaneous tissue
- May cause infection in the stomach, small intestine, colon and liver
Pathophysiology
- Infection is acquired by ingestion of infected food (e.g., people with pica) and using contaminated papers for cleaning the skin (e.g., toilet papers)
- Possibly due to ranitidine, which can decrease gastric acidity and allow fungal survival after gastric passing (Iran J Med Sci 2015;40:90)
- Smoking can decrease mucosal WBC function and facilitate fungal infection by B. ranarum (Clin Infect Dis 2012;54:1685)
Etiology
- Basidiobolus ranarum
Clinical features
- Abdominal pain and fever are most common presenting features (J Med Microbiol 2012;61:1770)
- Other features include constipation, diarrhea, gastrointestinal bleeding, mucoid stool and rarely perforated appendicitis (Case Rep Surg 2011;2011:685460)
Diagnosis
- Based on characteristic histopathology findings of fungal hyphae (the Splendore-Hoeppli phenomenon) and culture of B. ranarum from the tissue specimen
- The gold standard for definite diagnosis is culture
- Macroscopically, colonies are yellowish gray in color with a waxy appearance and many radial folds (J Med Microbiol 2012;61:1770)
Laboratory
- Eosinophilia and high ESR (erythrocyte sedimentation rate)
- Elevated levels of cytokines such as IL4, IL10, TNFα (TH2 type cytokines) (J Clin Microbiol 2001;39:2360)
Radiology description
- Colorectal mass is the most common finding, followed by hepatic mass or small bowel mass (Abdom Imaging 2015;40:246)
- Bowel wall thickening was noticed in 25% of the reported cases, whereas bowel perforation or abscess was less commonly seen (Afr J Paediatr Surg 2015;12:193)
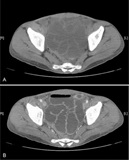
Radiology images
Poor prognostic factors
- Pediatric age group at presentation
- Delayed treatment
Case reports
- 4 year old girl with visceral basidiobolomycosis, an unusual fungal infection of viscera (Afr J Paediatr Surg 2015;12:193)
- 34 year old woman with perforated appendicitis with gastrointestinal basidiobolomycosis (Surg Infect (Larchmt) 2014;15:339)
- 36 year old man with diffusely thickened small bowel with edematous change (Medicine (Baltimore) 2015;94;e1430)
Treatment
- Combined surgery and antifungal treatment for a variable period of time (6 months to 2 years) (J Pediatr Surg 2012;47:949)
- Itraconazole, an antifungal agent is the most common drug used
Gross description
- Fungus involves the nonmucosal layers such as submucosa and subserosa of the GI tract, hence endoscopic biopsies, which are superficial and small, usually fail to detect the fungal hyphae (Saudi Med J 2013;34:1068)
Gross images
Microscopic (histologic) description
- Marked infiltration of eosinophils
- Mixed infiltration of PMN leukocytes and granulomatous inflammation
- Thin wall and broad hyphae surrounded by eosinophilic material, which are easily seen by hematoxylin and eosin staining; however periodic acid-Schiff (PAS) and gomori methenamine silver (GMS) can intensify the fungal wall staining
- Zygospores which are very similar to trophozoites of amoeba (Clin Infect Dis 2001;32:1448)
Microscopic (histologic) images
Cytology description
- Broad septate thin walled fungal hyphae along with eosinophils
Differential diagnosis
- Eosinophilic gastroenteritis: no fungal hyphae
- Other granulomatous lesions: no broad septate fungal hyphae