Table of Contents
Definition / general | Essential features | ICD coding | Sites | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ahmed S, Haroon S. Focal active colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonactivecolitis.html. Accessed March 27th, 2025.
Definition / general
- Focal active colitis (FAC) is a histologic term that denotes the presence of focal neutrophil infiltration within the colonic crypts or epithelium (Biomedicines 2023;11:2631)
- Nonspecific diagnosis that encompasses infectious (acute self limited) colitis and noninfectious active colitis
Essential features
- Focal active colitis (FAC) is characterized by a single focus or multiple foci of neutrophilic infiltration of the crypts with an otherwise unremarkable colonic mucosa; the crypt architecture is well preserved with no evidence of chronic injury (Cureus 2020;12:e8140)
- FAC can be seen in the setting of acute self limited infectious colitis, evolving inflammatory bowel disease (IBD), ischemic colitis, Clostridium difficile colitis, drug induced or chemical injury, irritable bowel syndrome and bowel preparation artifact (Cureus 2020;12:e8140)
- Incidence of Crohn's disease (CD) in adults presenting with FAC is relatively low and varies between 0 and 13%, whereas the incidence of infectious type colitis has been demonstrated to be nearly 50% (Cureus 2020;12:e8140)
- In pediatric patients, a 24% rate of IBD is seen with FAC; however, when patients with associated terminal ileal inflammation were excluded, the rate dropped to 11% (similar to the rates of adults) (Hum Pathol 2018;74:164)
- FAC remains a diagnostic challenge; one must incorporate the patient's presenting history, medications and findings on endoscopy to help narrow the differential diagnosis
ICD coding
- ICD-11: 1A40.0 - gastroenteritis or colitis without specification of origin
Sites
- Colon
Clinical features
- Diarrhea, nausea, abdominal cramps, increased flatulence (Cureus 2020;12:e8140)
Diagnosis
- Diagnosed on colonoscopic biopsy
Prognostic factors
- Prognosis depends upon the underlying cause whether it is infectious or inflammatory bowel disease
Case reports
- Teenage girl with orbital myositis associated with focal active colitis (Childs Nerv Syst 2012;28:641)
- 82 year old woman presented with complaints of diarrhea, nausea, abdominal cramping, increased flatulence, anorexia and weight loss for the past 3 months (Cureus 2020;12:e8140)
Treatment
- Treatment of underlying etiology, such as inflammatory bowel disease, irritable bowel syndrome or infectious colitis
Microscopic (histologic) description
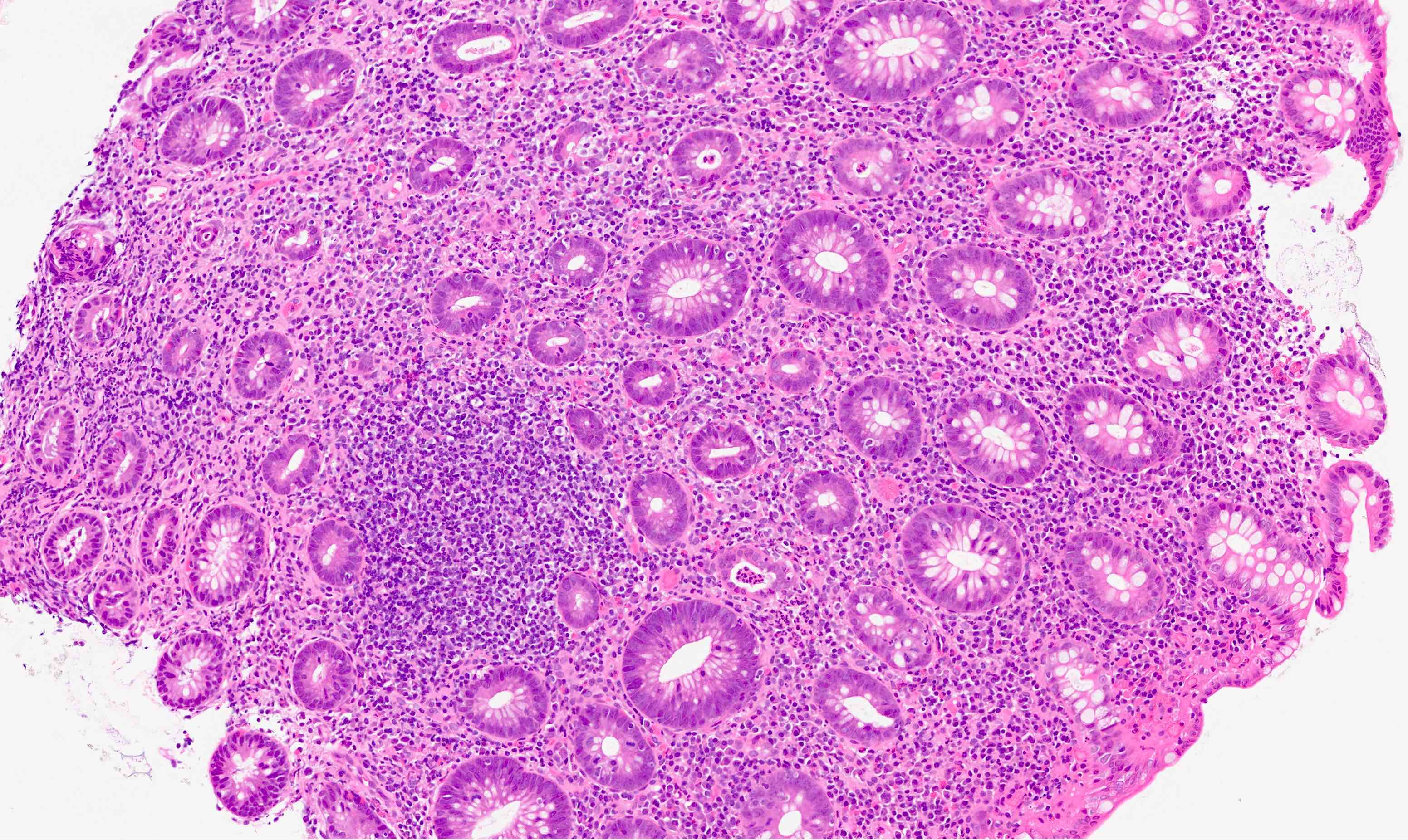
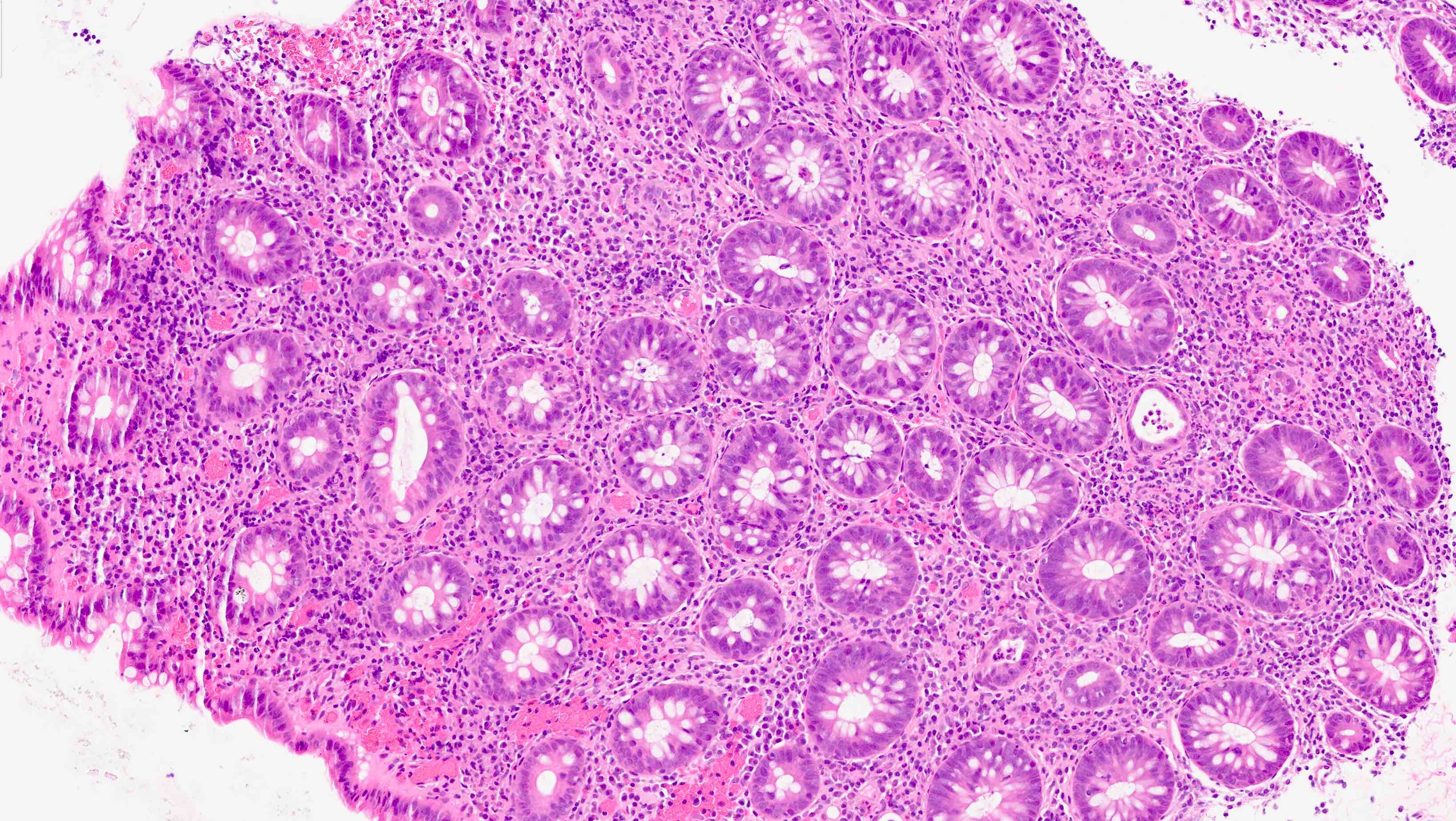
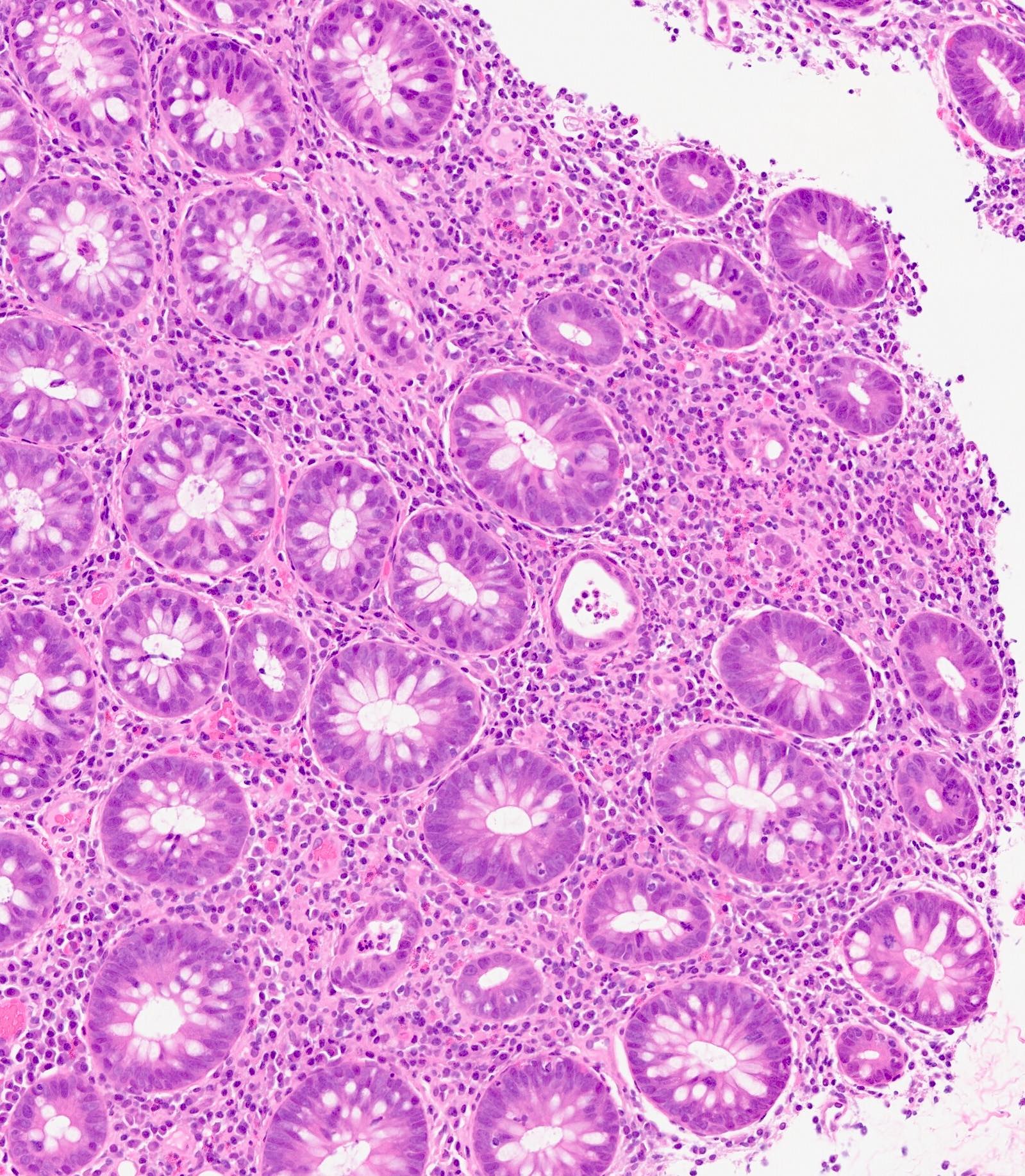
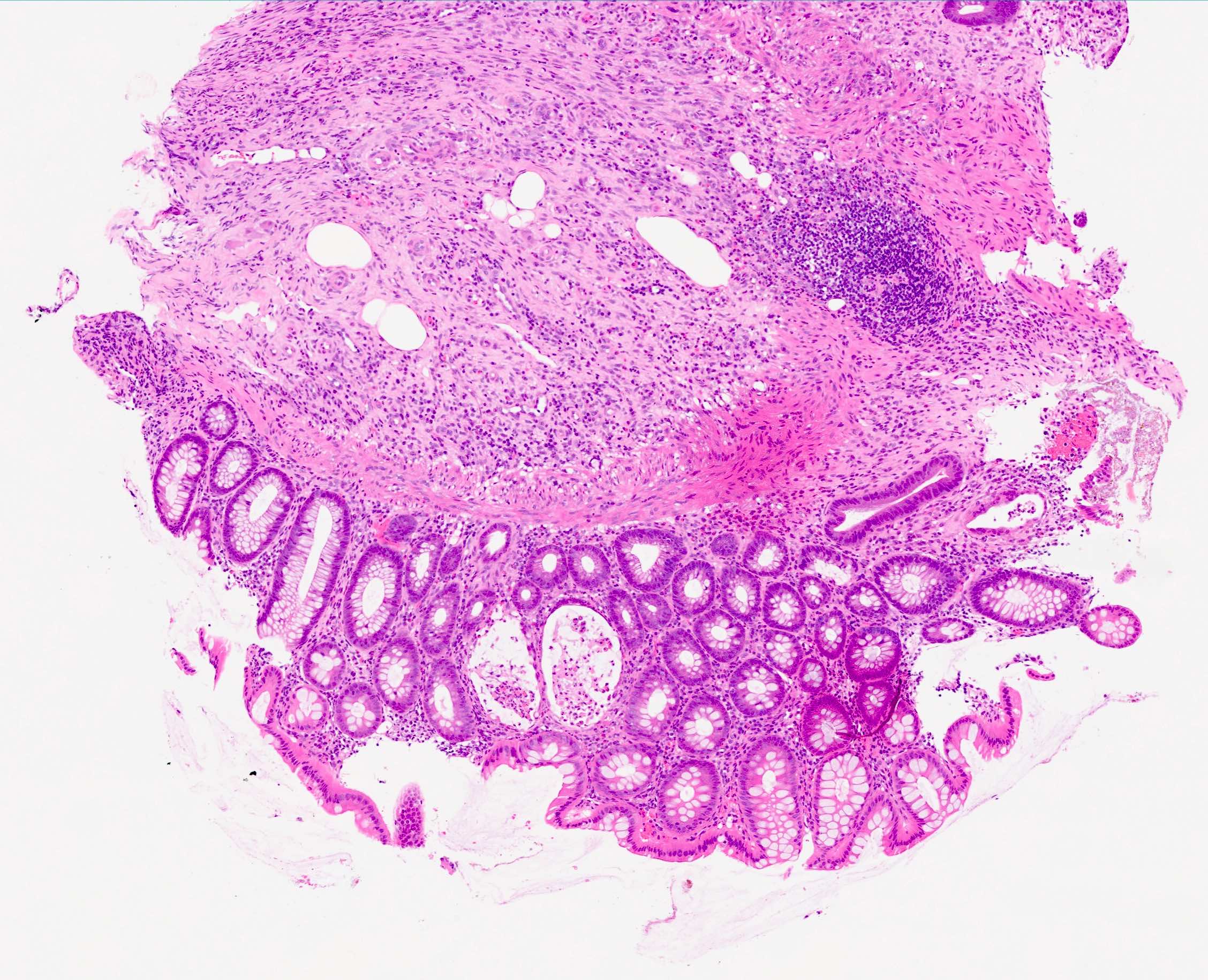
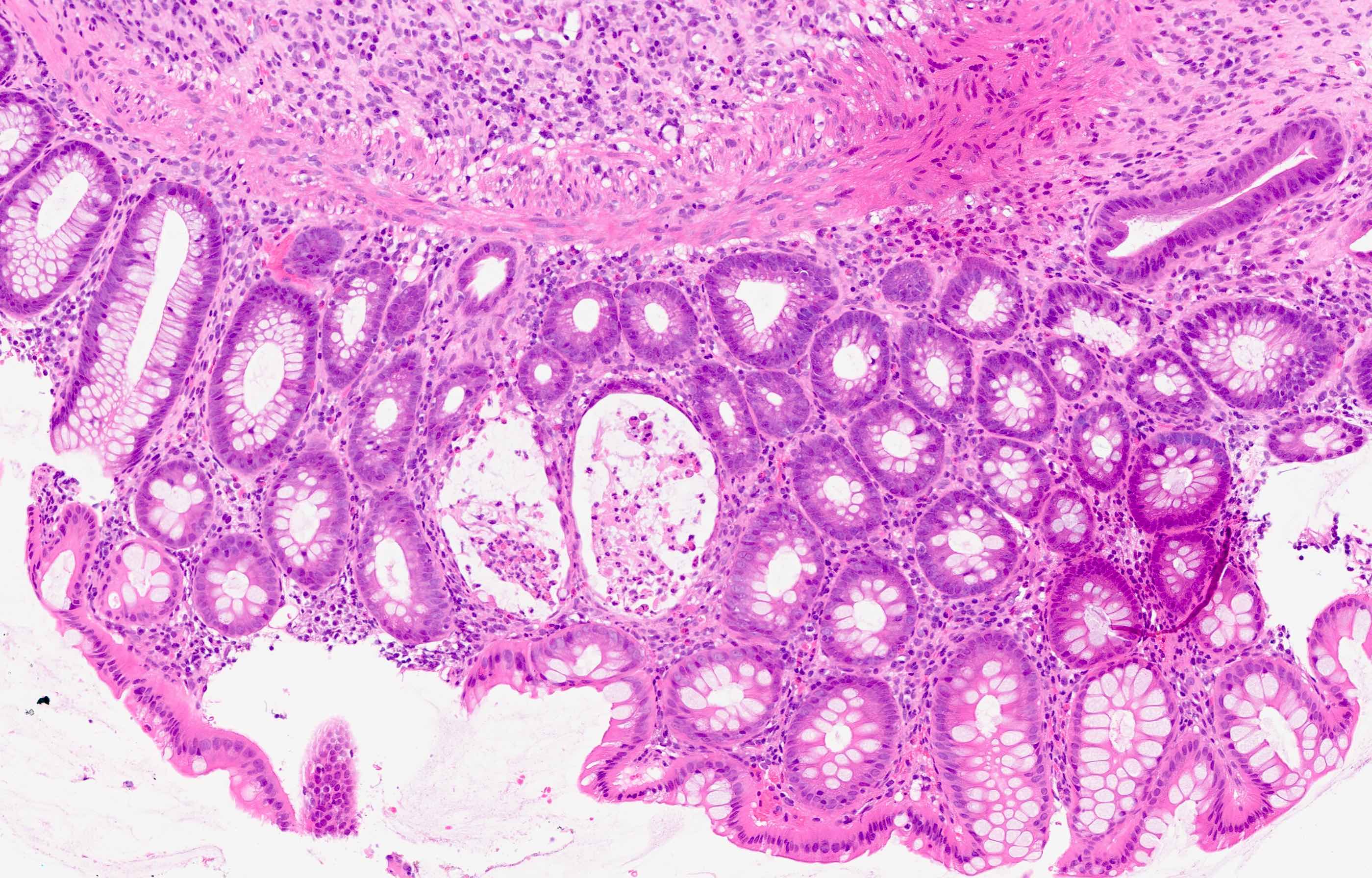
- Neutrophil mediated surface epithelial injury, neutrophils within epithelial cells (cryptitis) or within crypt lumina (crypt abscess) (Biomedicines 2023;11:2631)
- Expansion of lamina propria with neutrophils and eosinophils
- Well preserved crypt architecture
Microscopic (histologic) images
Sample pathology report
- Colon, biopsy:
- Focal active colitis (see comment)
- Comment: The differential diagnosis for focal active colitis includes infectious process, medication associated injury (e.g., nonsteroidal anti-inflammatory drugs) or emerging inflammatory bowel disease. Histologic features of chronic injury are not seen. Negative for viral cytopathic effect and granulomata.
Differential diagnosis
- Acute self limiting colitis:
- Abundant superficial acute inflammation, cryptitis and crypt abscess without features of chronicity
- Early onset inflammatory bowel disease:
- Especially in pediatric population
- Ileal involvement
- Granulomas may be present
- Drug related colitis:
- Can have various patterns injury
- Increased epithelial apoptosis
- May show increased eosinophils (Br J Clin Pharmacol 2003;56:477)
- Increased intraepithelial lymphocytes
- Ischemic colitis:
- Ulceration and mucosal necrosis
- Lamina propria hyalinization
- Acute inflammatory exudate
- Crypt withering and crypt loss
Additional references
Board review style question #1
A 55 year old man presented with diarrhea, abdominal discomfort and flatulence. Colonoscopy shows patchy erythematous areas in the left colon. Endoscopic biopsy is taken and it shows the histology above. Which of the following statements is the most likely morphological diagnosis?
- Focal active colitis
- Lymphocytic colitis
- Pseudomembranous colitis
- Ulcerative colitis
Board review style answer #1
A. Focal active colitis. Focal active colitis is the correct answer as there is focal cryptitis and crypt abscess formation. The crypt architecture is intact. Answer B is incorrect because there are no increased intraepithelial lymphocytes. Answer C is incorrect because pseudomembranous colitis typically has necroinflammatory exudate on the surface. Answer D is incorrect because crypt distortion is typically seen in ulcerative colitis of patients of this age range.
Comment Here
Reference: Focal active colitis
Comment Here
Reference: Focal active colitis
Board review style question #2
A 17 year old boy presented with bloody diarrhea and elevated fecal calprotectin. He had granulomata on upper GI biopsy and colonoscopic biopsy showed focal active colitis. Which of the following is the most likely underlying diagnosis?
- Crohn's disease
- Lymphocytic colitis
- Pseudomembranous colitis
- Ulcerative colitis
Board review style answer #2
A. Crohn's disease is the correct answer because in the pediatric population, inflammatory bowel disease can just present by focal active colitis, even though the architecture is intact. Answer B is incorrect because lymphocytic colitis has increased intraepithelial lymphocytes. Answer C is incorrect because pseudomembranous colitis shows inflammatory exudate on the mucosal surface. Answer D is incorrect because ulcerative colitis doesn't show granulomas on upper GI biopsies.
Comment Here
Reference: Focal active colitis
Comment Here
Reference: Focal active colitis