Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Perveze I, Yin F. COVID-19 associated colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colonCOVID19colitis.html. Accessed March 30th, 2025.
Definition / general
- Colonic mucosal damage associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection
Essential features
- Gastrointestinal symptoms seen in up to 50% of coronavirus disease 2019 (COVID-19) patients (Am J Gastroenterol 2020;115:766, Lancet Gastroenterol Hepatol 2020;5:667, BMJ Open Gastroenterol 2021;8:e000578, Gut 2020;69:997)
- SARS-CoV-2 RNA detected in more than 40% of fecal samples in COVID-19 patients (BMJ Open Gastroenterol 2021;8:e000578)
- Potential fecal - oral transmission (Nat Rev Gastroenterol Hepatol 2021;18:269)
- Common clinical presentation: nausea, vomiting, diarrhea, abdominal discomfort and hematochezia (Gastroenterology 2020;159:81, Am J Gastroenterol 2020;115:766, Clin Gastroenterol Hepatol 2020;18:2378, World J Gastroenterol 2020;26:2323)
- Common endoscopic findings: ischemic-like colopathy, ulcer, lower GI bleeding and erythema (BMJ Open Gastroenterol 2021;8:e000578)
- Common histopathologic findings: ischemic colitis with necrosis, submucosal venous microthrombi, withered crypts, erosion / ulceration, focal edema, nonspecific acute inflammation, lamina propria lymphohistiocytic or eosinophilic infiltrate, increased crypt apoptotic bodies, mild architectural distortion and pneumatosis intestinalis; may resemble pseudomembranous colitis (Case Rep Gastroenterol 2021;15:408, BMJ Open Gastroenterol 2021;8:e000578, Arch Pathol Lab Med 2021 May 7 [Epub ahead of print])
ICD coding
Epidemiology
- WHO declared the COVID-19 outbreak, caused by SARS-CoV-2, a global pandemic
- Primarily affecting the respiratory system, COVID-19 can also lead to gastrointestinal symptoms
- Common comorbidities: hypertension, diabetes mellitus, chronic cardiac disease, chronic respiratory disease, chronic renal disease (Clin Gastroenterol Hepatol 2020;18:2378, BMJ Open Gastroenterol 2021;8:e000578)
Pathophysiology
- SARS-CoV-2 binds to the angiotensin converting enzyme 2 (ACE2) receptor through its surface spike protein for host entry
- ACE2 receptor is highly expressed in the intestinal epithelial cells
- Potential mechanisms for COVID-19 associated colitis:
- Altered microbiota homeostasis
- Enterocyte damage
- Release of virulent proteins or toxins
- Hypercoagulable state (Intest Res 2020 Nov 6 [Epub ahead of print], Acta Med Indones 2021;53:96)
Etiology
- SARS-CoV-2, an enveloped positive stranded RNA virus related to the severe acute respiratory syndrome (SARS) virus and the Middle East respiratory syndrome (MERS) virus
Clinical features
- Common clinical presentation:
- Anorexia (26.8%)
- Diarrhea (12.5%)
- Nausea and vomiting (10.2%)
- Abdominal discomfort (9.2%) (Gastroenterology 2020;159:81)
- Gastrointestinal symptoms typically develop within 1 week of onset of COVID-19 infection
- Diffuse abdominal pain / tenderness, metabolic acidosis and hypotension indicate worsening clinical course and potential need for surgical intervention
Diagnosis
- SARS-CoV-2 RNA detection in upper respiratory tract specimens
- SARS-CoV-2 RNA detection in fecal specimens
- Electron microscopy showing SARS-CoV-2 viral particles in colorectal tissue
- Histopathologic evaluation of the gastrointestinal biopsy and resection specimens
- SARS-CoV-2 RNA ISH and immunohistochemical stain on formalin fixed, paraffin embedded (FFPE) sections (Arch Pathol Lab Med 2021 May 7 [Epub ahead of print], Clin Infect Dis 2020 Jul 8 [Epub ahead of print])
Laboratory
- Elevation of prothrombin time and international normalized ratio (INR)
- D dimer > 1,850 ng/mL and presence of at least 1 gastrointestinal symptom were independently associated with major endoscopic abnormalities (BMJ Open Gastroenterol 2021;8:e000578)
- Elevation of liver function test (aspartate aminotransferase [AST], alanine aminotransferase [ALT]) (Am J Gastroenterol 2020;115:766)
Radiology description
- Enhanced CT showed mild dilatation of the colon with diffuse wall thickening and surrounding inflammation (Cureus 2021;13:e13236, Am J Trop Med Hyg 2021;104:1655)
- Computed tomography angiography (CTA) showed pneumatosis intestinalis and mesenteric stranding, highlighting the thromboembolic complications in COVID-19 (Rev Esp Enferm Dig 2020;112:583)
Case reports
- 7 week old boy with COVID-19 and necrotizing enterocolitis-like pneumatosis intestinalis (Pediatr Infect Dis J 2021;40:e85)
- 17 year old boy with trisomy 21 diagnosed with SARS-CoV-2 related ischemic colitis (Pediatr Dev Pathol 2021 May 28 [Epub ahead of print])
- 38, 55 and 74 year old men with cases of COVID-19 disease with colonic manifestations (Am J Gastroenterol 2020;115:948)
- 44 year old man, hospitalized for COVID-19 associated pneumonia, developed pneumatosis intestinalis (BMJ Open Gastroenterol 2020;7:e000434)
- 45 year old man and 68 year old woman with COVID-19 associated ischemic enterocolitis (Am J Trop Med Hyg 2021;104:1655)
- 56, 68 and 76 year old men with COVID-19 pneumonia developed severe colon ischemia (Rev Esp Enferm Dig 2020;112:784)
- 62 year old woman with low rectal cancer treated with low anterior rectal resection, complicated with SARS-CoV-2 infection, late colonic ischemia and colovaginal fistula (Chirurgia (Bucur) 2020;115:677)
- 66 year old man with severe COVID-19 pneumonia and ischemic colitis (Am J Trop Med Hyg 2021;104:63)
- 67 and 68 year old men with severe COVID-19 pneumonia complicated by hematochezia (Case Rep Gastroenterol 2021;15:408)
- 73 year old man presented with COVID-19 disease and ischemic colitis (Am J Emerg Med 2020;38:2758.e1)
- 82 year old woman with COVID-19 infection presenting as acute intestinal ischemia (Korean J Gastroenterol 2020;76:164)
Treatment
- Supportive care, bowel rest and close observation
- Surgical intervention is indicated if there is evidence of perforation, infarction and necrosis (Am J Emerg Med 2020;38:2758.e1)
Microscopic (histologic) description
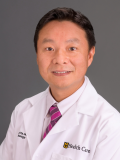
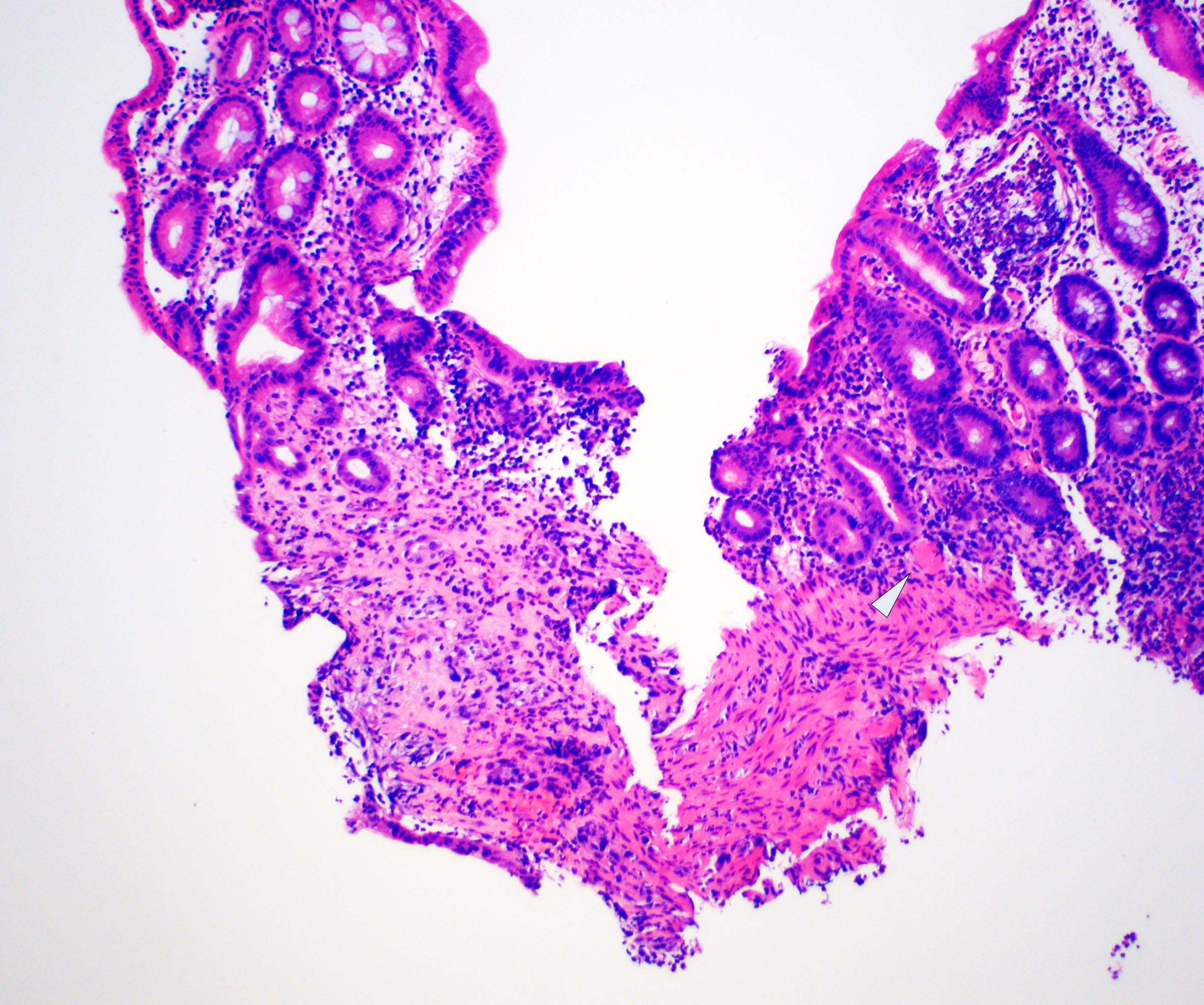
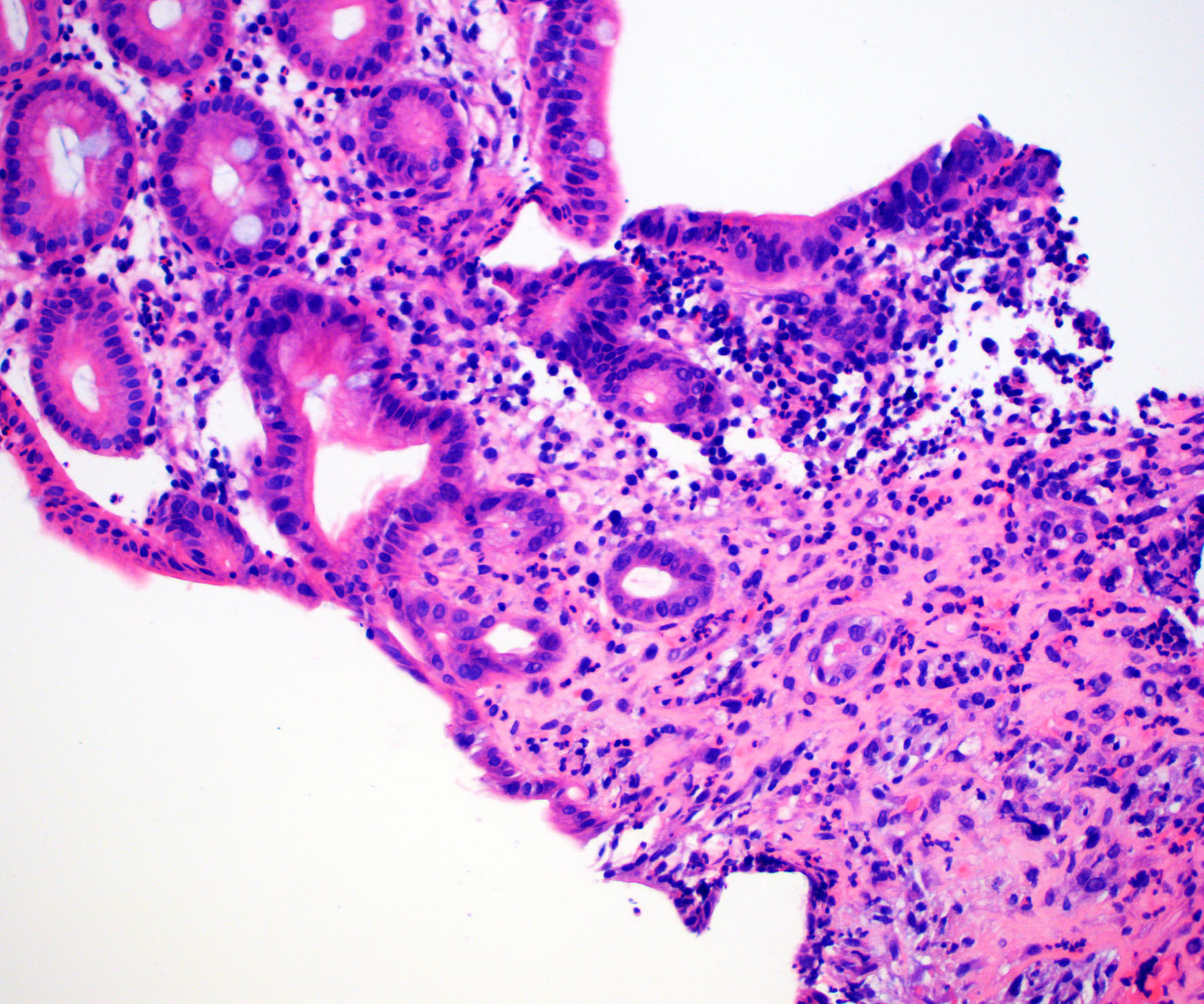
- Ischemic colitis pattern of injury most common:
- Withered crypts
- Hyalinized stroma
- Erosion / ulceration
- Coagulative necrosis
- Microhemorrhages
- Microthrombi and vascular congestion
- Other nonspecific histopathologic findings:
- Focal edema
- Nonspecific acute inflammation
- Lamina propria lymphohistiocytic or eosinophilic infiltrate
- Increased crypt apoptotic bodies (Arch Pathol Lab Med 2021 May 7 [Epub ahead of print])
- Mild architectural distortion
- Pneumatosis intestinalis
- Pseudomembranous colitis-like presentation
Microscopic (histologic) images
Positive stains
- SARS-CoV-2 immunohistochemical stain (Clin Infect Dis 2020 Jul 8 [Epub ahead of print])
- SARS-CoV-2 in situ hybridization (ISH) (Arch Pathol Lab Med 2021 May 7 [Epub ahead of print])
Electron microscopy description
- Multiple SARS-CoV-2 viral particles in the colonic submucosal venous endothelial cells (Intensive Care Med 2020;46:2081)
Sample pathology report
- Colon, biopsy:
- Ischemic colitis consistent with clinical history of SARS-CoV-2 infection
Differential diagnosis
- Inflammatory bowel disease (IBD):
- Personal or family history of IBD or other autoimmune disorders
- Onset tends to be subacute to chronic
- Marked architectural distortion and prominent acute inflammation
- Ischemic colitis, NOS:
- Noninfectious colitis
- Watershed areas most commonly affected
- Clinical correlation essential
- Medication associated mucosal damage:
- History of medication (such as NASID) use
- May present as chronic mucosal injury pattern
- Acute infectious colitis (other than COVID-19):
- Caused by bacteria or virus
- Acute cryptitis, crypt abscess
- May present with ischemic injury pattern
- Bacterial culture, PCR and sequencing diagnostic
Board review style question #1
A 71 year old man with a medical history of diabetes mellites type 2, coronary artery disease and morbid obesity was hospitalized for COVID-19 pneumonia. On day 3 of hospital stay, he developed left sided abdominal pain and hematochezia. Endoscopy showed mucosal erosions and ulceration at the splenic flexure. A representative photomicrograph of the biopsy is shown. Which is the most likely diagnosis?
- COVID-19 associated colitis
- Diverticulitis
- Inflammatory bowel disease
- Mesenteric ischemia
- Pseudomembranous colitis
Board review style answer #1
A. COVID-19 associated colitis. The biopsy reveals colonic mucosa with focal epithelial mucin depletion, withered crypts, mildly hyalinized stroma, mucosal microthrombi and patchy acute inflammatory infiltrate. In the current clinical setting (patient with COVID-19 pneumonia followed by abdominal pain and hematochezia), this is most compatible with COVID-19 associated ischemic colonic mucosal injury. Clinical correlation is essential.
Comment Here
Reference: COVID-19 associated colitis
Comment Here
Reference: COVID-19 associated colitis
Board review style question #2
What is the most common histologic feature of COVID-19 associated colitis?
- Basal lymphoplasmacytosis and crypt architectural distortion
- Eosinophilic cryptitis and abscess
- Intraepithelial lymphocytosis
- Pseudomembrane material composed of fibrin, mucin, neutrophils and inflammatory debris
- Withered crypts, lamina propria hyalinization and microthrombi
Board review style answer #2
E. Withered crypts, lamina propria hyalinization and microthrombi. The most common histologic feature of COVID-19 associated colitis is ischemic colitis pattern, including withered crypts, lamina propria hyalinization and microthrombi.
Comment Here
Reference: COVID-19 associated colitis
Comment Here
Reference: COVID-19 associated colitis