Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tauziede-Espariat A. Medulloblastoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumormedulloblastoma.html. Accessed January 14th, 2025.
Definition / general
- 4 genetically defined groups and 4 histologically defined groups (Nature 2017;547:311)
- Genetically defined: (a) WNT (for wingless integration site) activated, (b) SHH (sonic hedgehog) activated (either TP53 mutant or TP53 wild type), non-WNT / non-SHH, either (c) medulloblastoma group 3 or (d) medulloblastoma group 4 (Nature 2017;547:311)
- Histologically defined: classic, desmoplastic / nodular, medulloblastoma with extensive nodularity and large cell / anaplastic medulloblastoma (Neuropathol Appl Neurobiol 2002;28:257)
- Classic is more common in childhood and desmoplastic / nodular in infants and adults (Neuropathol Appl Neurobiol 2002;28:257)
Essential features
- Small, round undifferentiated cells with mild to moderate nuclear pleomorphism (Neuropathol Appl Neurobiol 2002;28:257)
- High mitotic count (Neuropathol Appl Neurobiol 2002;28:257)
- Cerebellum and paratentorial brain, fourth ventricle (Neuropathol Appl Neurobiol 2002;28:257)
Epidemiology
- Medulloblastoma is the most common CNS embryonal tumor of childhood and is second only to pilocytic astrocytoma for all intracranial neoplasms (Acta Neuropathol 2012;123:473)
- Classic medulloblastoma (Acta Neuropathol 2012;123:473)
- Non-WNT / non-SHH tumors or WNT activated
- Midline location
- Desmoplastic / nodular medulloblastoma (Acta Neuropathol 2012;123:473)
- Cerebellar hemispheres and midline
- Bimodal age distribution
- Gorlin syndrome: nevoid basal cell carcinoma syndrome
- SHH activated
- Favorable outcome in young children compared to nondesmoplastic
- Medulloblastoma with extensive nodularity (Acta Neuropathol 2012;123:473)
- Closely related to desmoplastic medulloblastoma
- SHH activated
- Predominantly occurs in infants
- Excellent outcome
- Large cell / anaplastic medulloblastoma (Acta Neuropathol 2012;123:473)
- Undifferentiated cells with marked nuclear pleomorphism, prominent nucleoli, cell wrapping and high mitotic count and apoptotic counts
- Associated with all genetic variants but more common in SHH activated and in group 3
Sites
- Fourth ventricle or cerebellar parenchyma
Clinical features
- Signs and symptoms of increased intracranial pressure (headache, nausea, vomiting)
Diagnosis
- Diagnosis of medulloblastoma requires histologic examination of tumor tissue and molecular genetic analyses
- Integrated pathology diagnosis that includes both morphologic subtype and molecular subgroup along with any additional molecular data is recommended (Pediatr Dev Pathol 2022;25:23)
Radiology description
- Solid, intensely contrast enhancing masses on CT and MRI (Neurochirurgie 2021;67:6)
Prognostic factors
- 3 prognostic subgroups (high risk, low risk and standard risk) depending on (Neuro Oncol 2021;23:1163)
- Clinical findings: age at diagnosis, presence or absence of metastases at diagnosis, extent of resection of the tumor (Neuro Oncol 2021;23:1163)
- Histopathological findings: histological group (large cell / anaplastic = poor prognosis; desmoplastic / nodular = good prognosis), presence of tumor cells in the cerebrospinal fluid (Neuro Oncol 2021;23:1163)
- Biological / molecular findings: immunohistochemical / genetic subgroup (non-WNT / non-SHH = groups 3 and 4 having a poor prognosis; WNT activated = good prognosis), SHH activated TP53 mutation (associated with a poorer prognosis), MYC / MYCN amplification (associated with a poorer prognosis) (Neuro Oncol 2021;23:1163)
Case reports
- 2 year old boy who presented with a midline cerebellar mass (Neuropathology 2016;36:372)
- 4 year old boy with a cerebellar hemispheric mass (Pediatr Blood Cancer 2016;63:1128)
- 6 year old boy with a mass lesion located in the upper middle cerebellum (J Neuropathol Exp Neurol 2021;80:205)
Treatment
- Depends on risk stratification
- Total resection
- Chemotherapy and radiation therapy
- Reference: J Neurooncol 2022;157:37
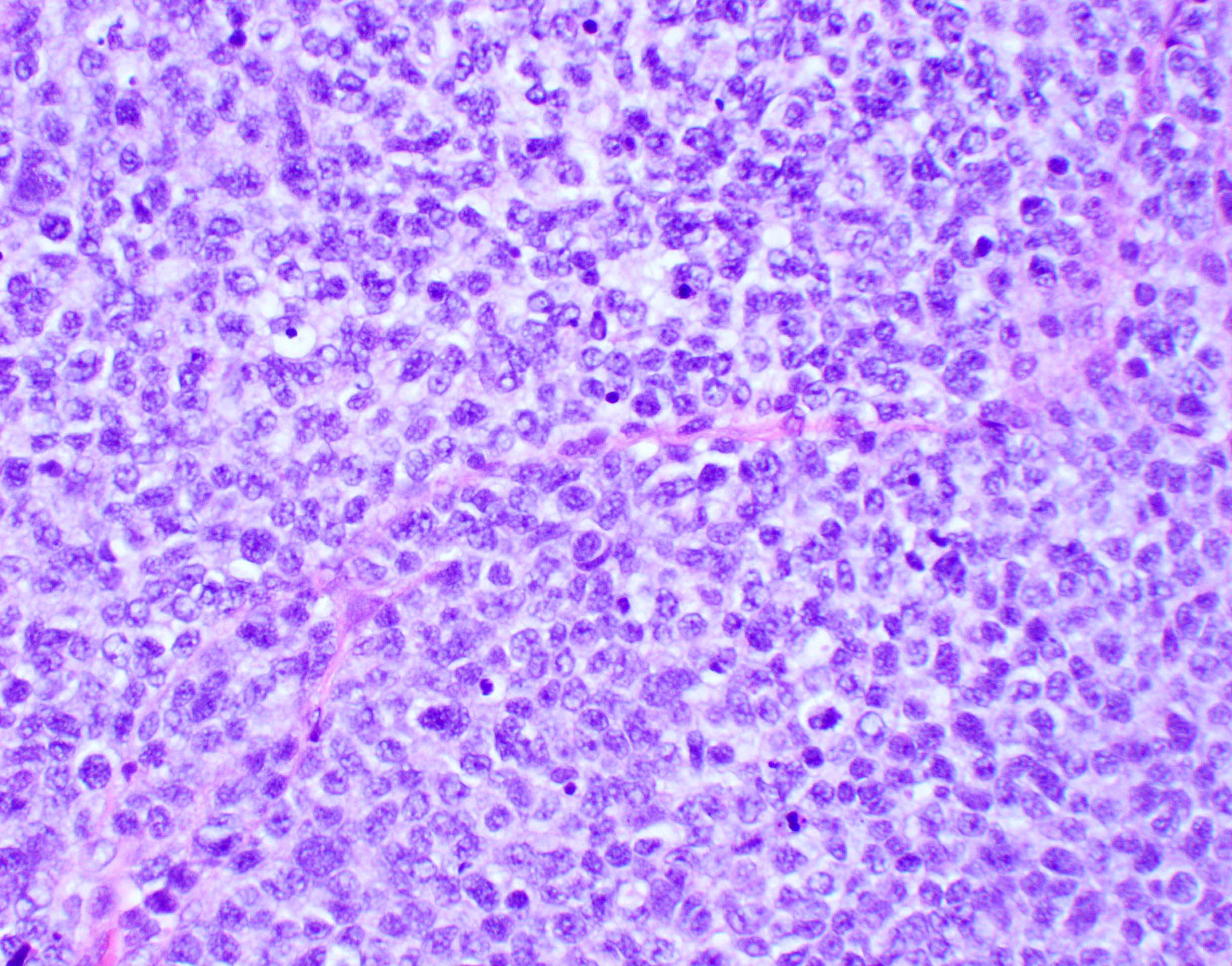
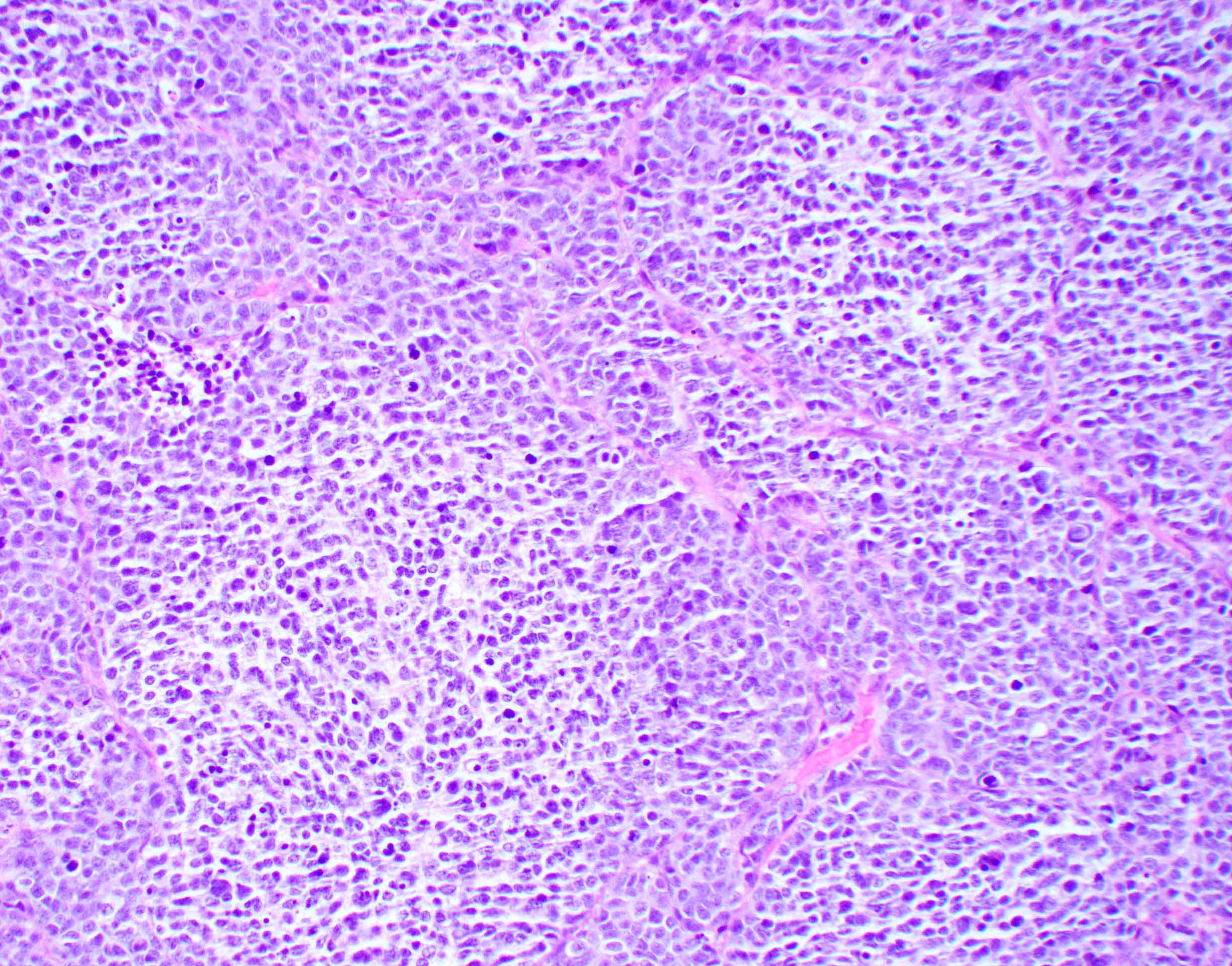
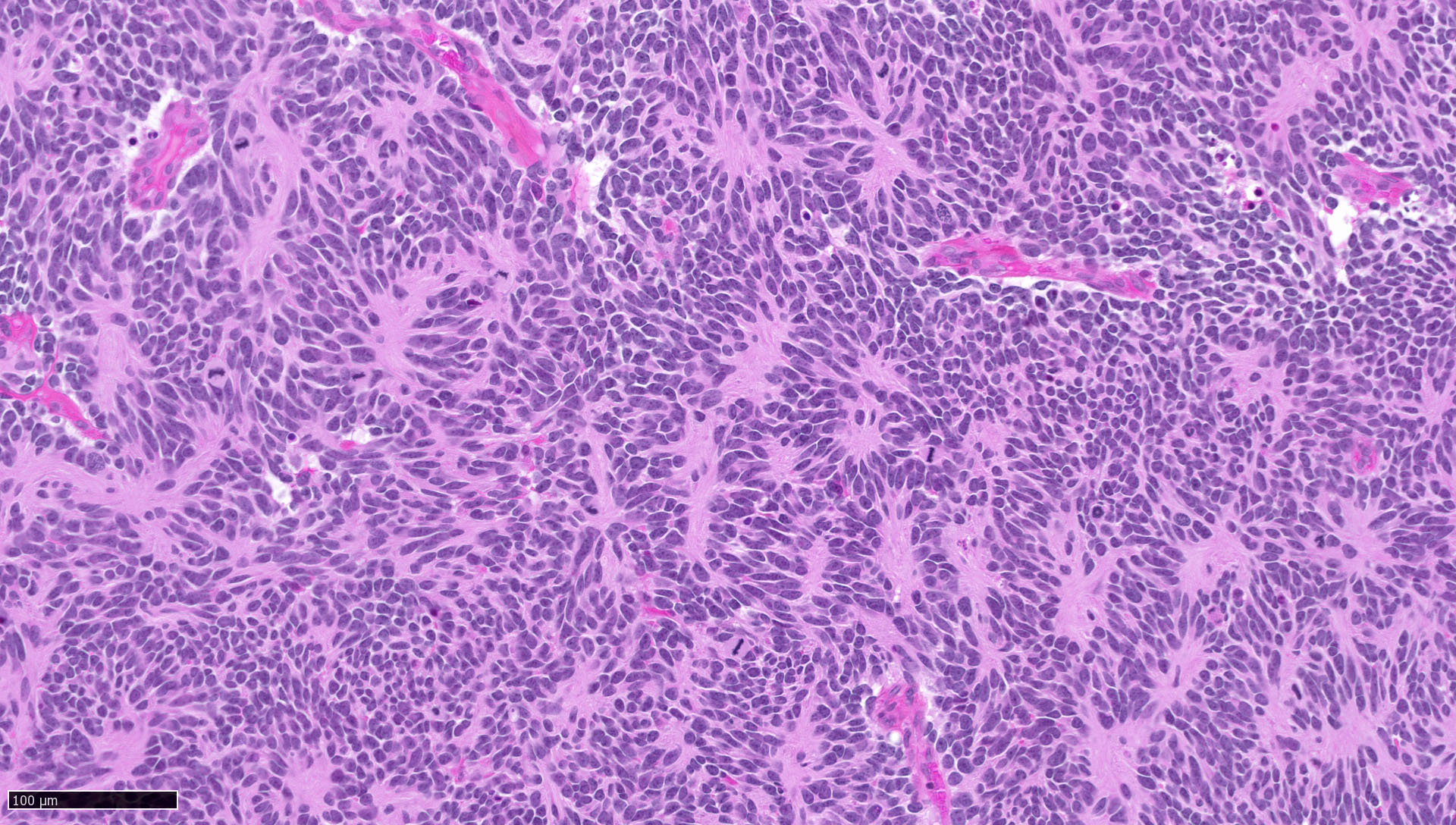
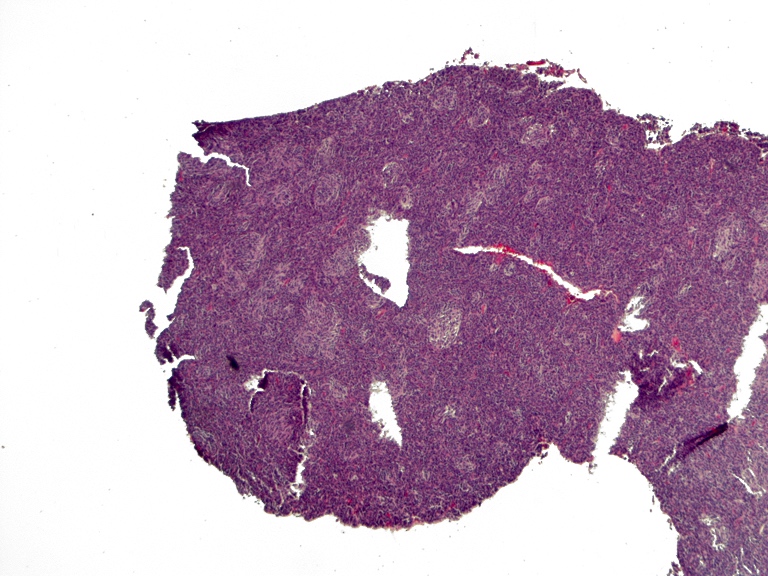
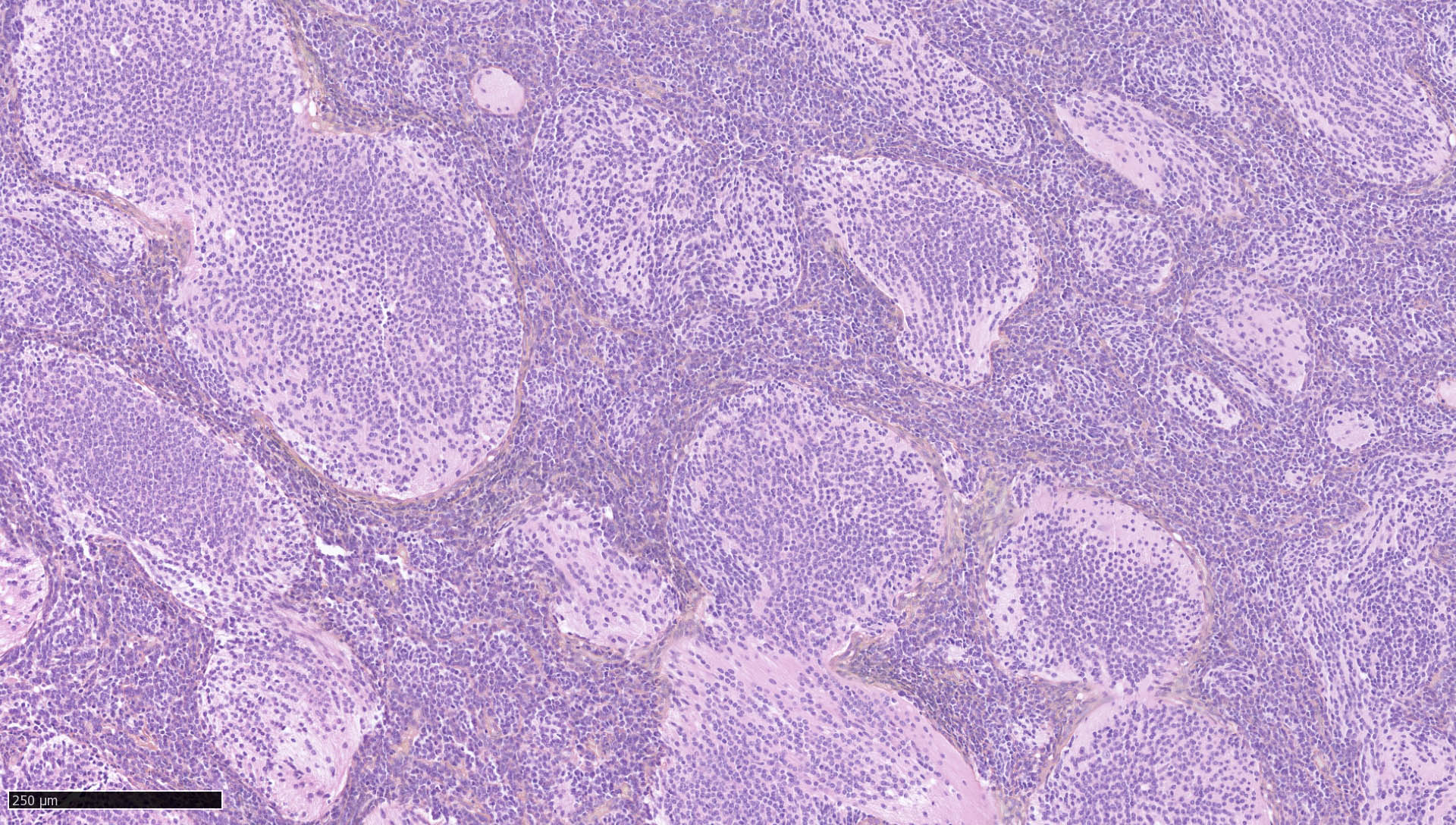
Microscopic (histologic) description
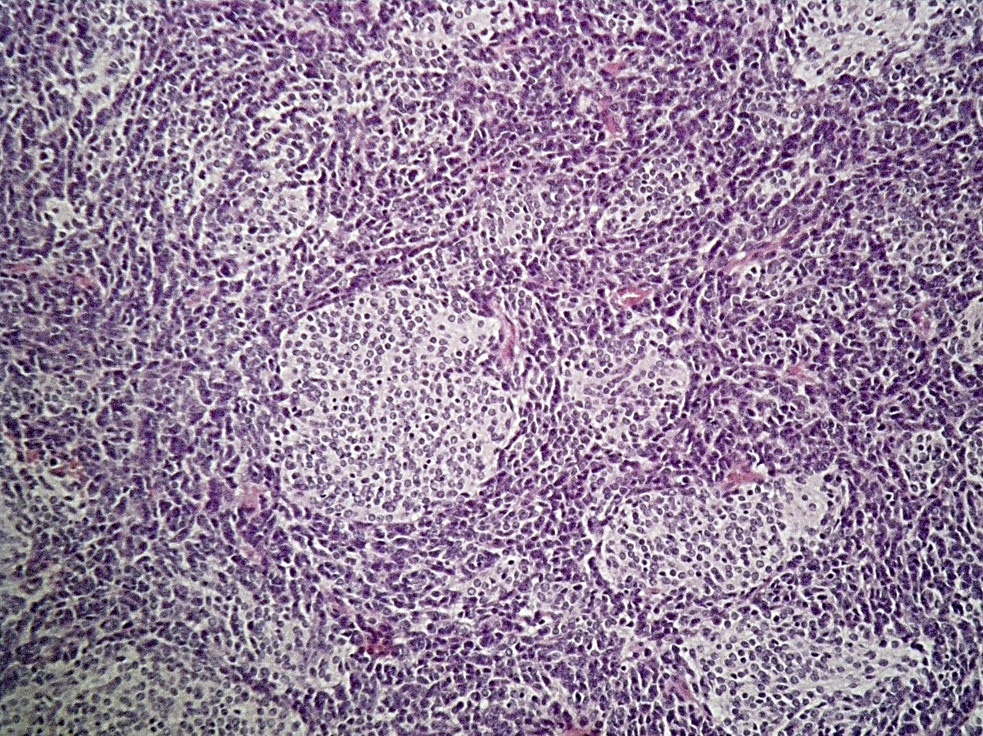
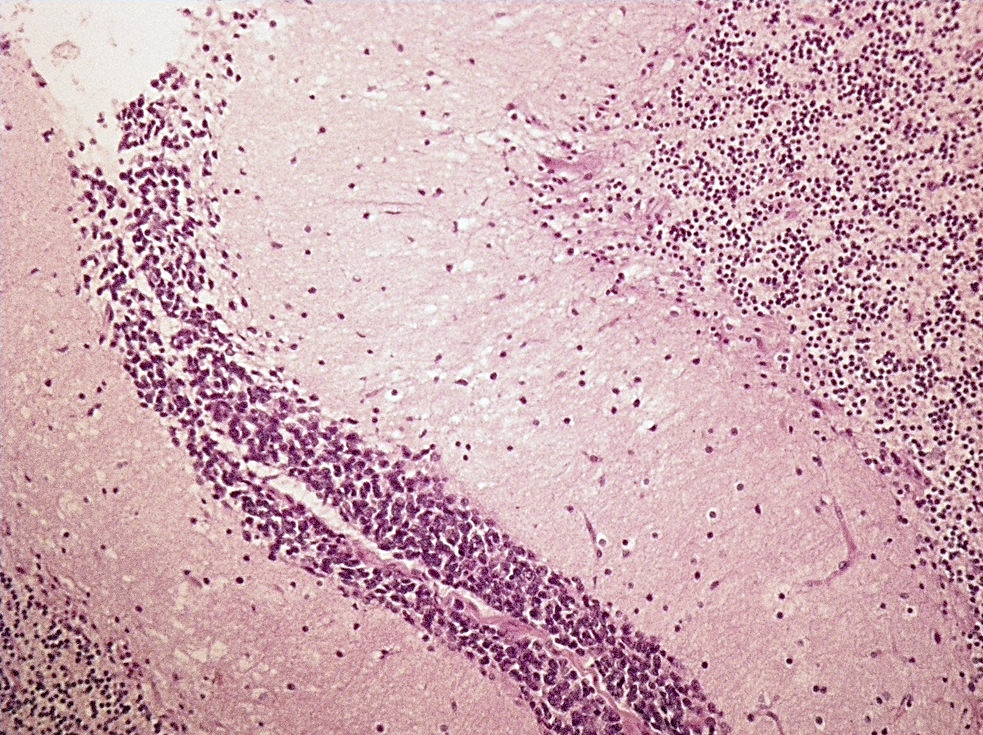
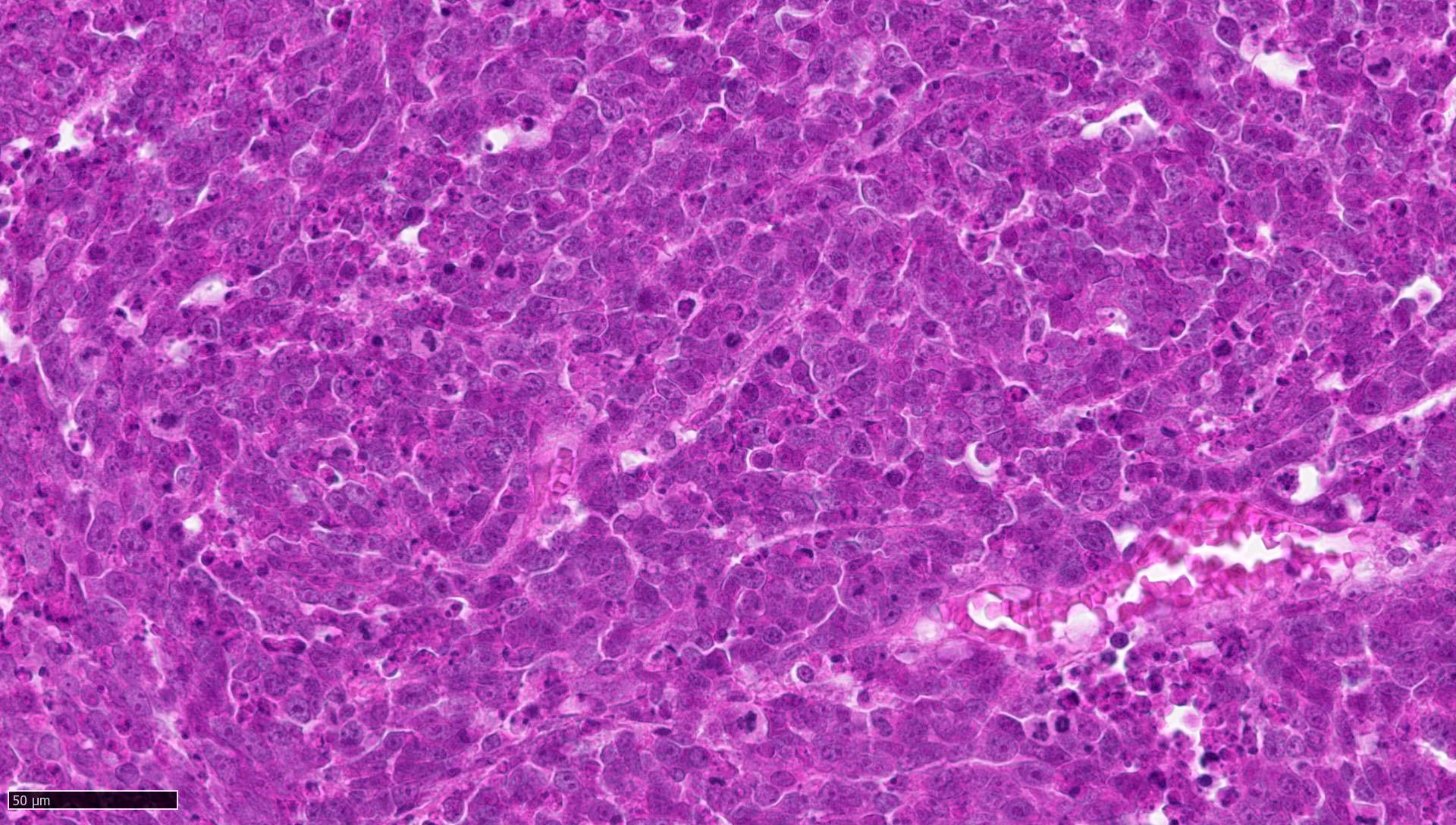
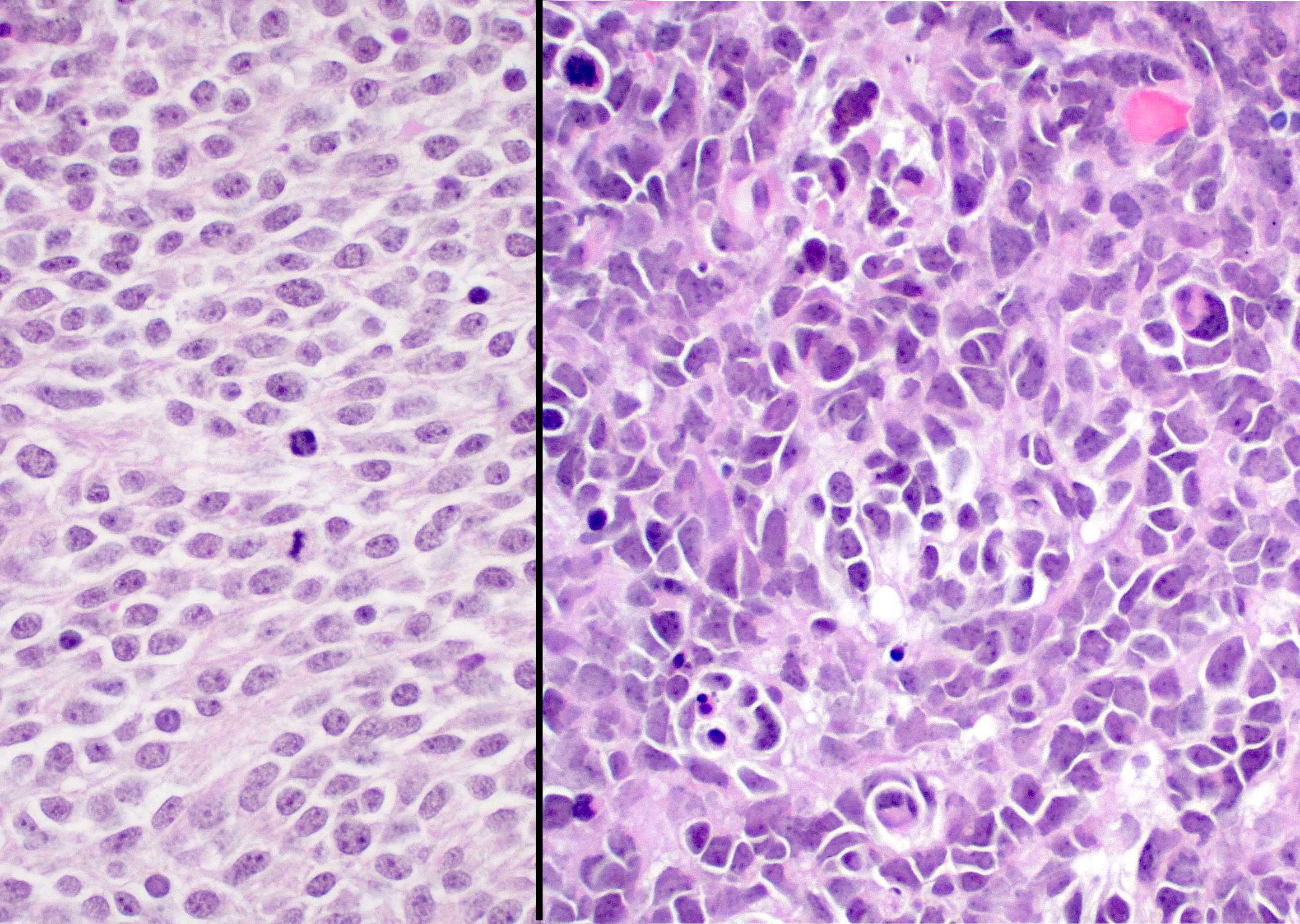
- Classic medulloblastoma (Neuropathol Appl Neurobiol 2002;28:257)
- Small, blue, round cell tumor
- Syncytial arrangement of densely packed undifferentiated cells (embryonal cells)
- Mitosis with apoptotic bodies
- Homer Wright rosettes
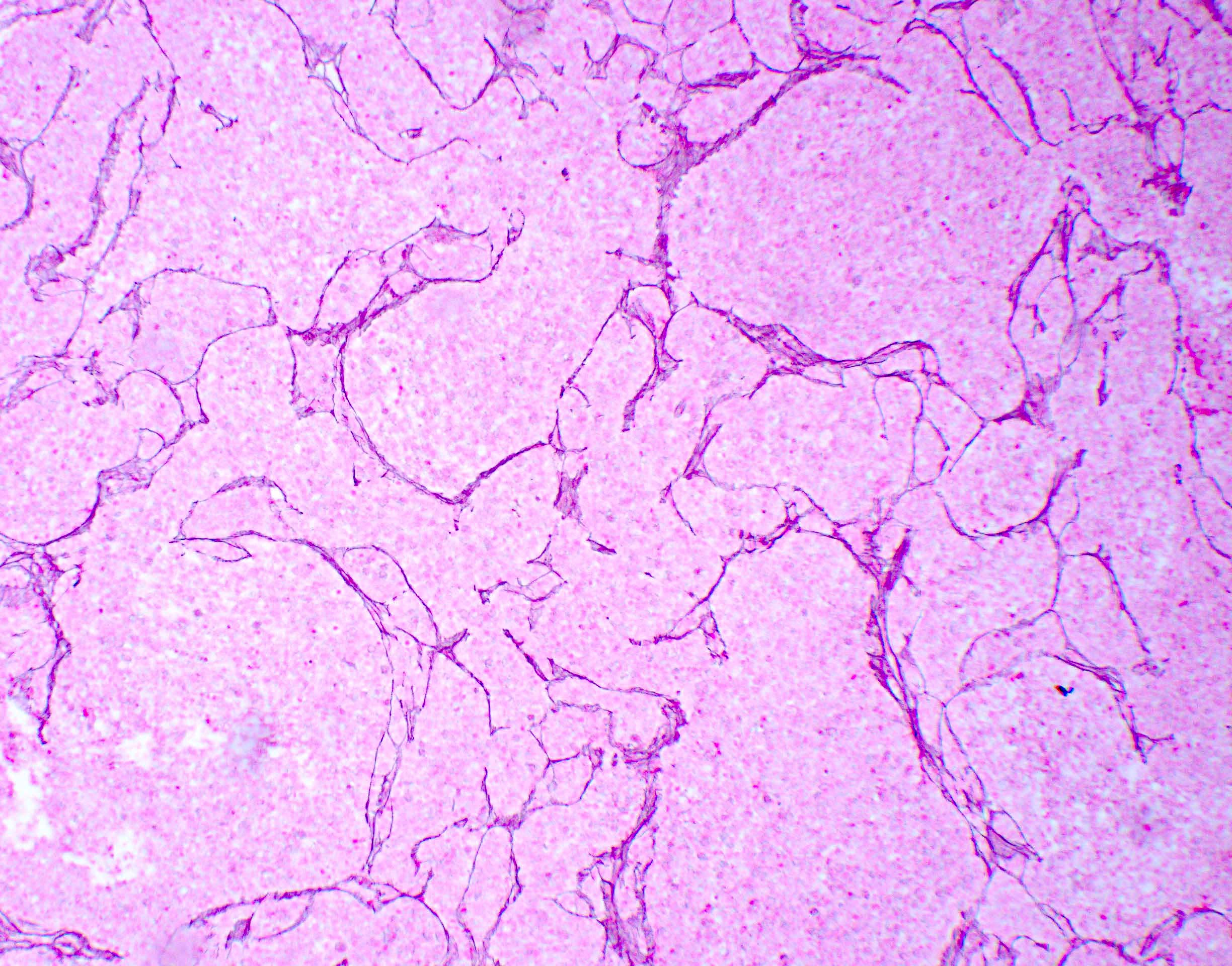
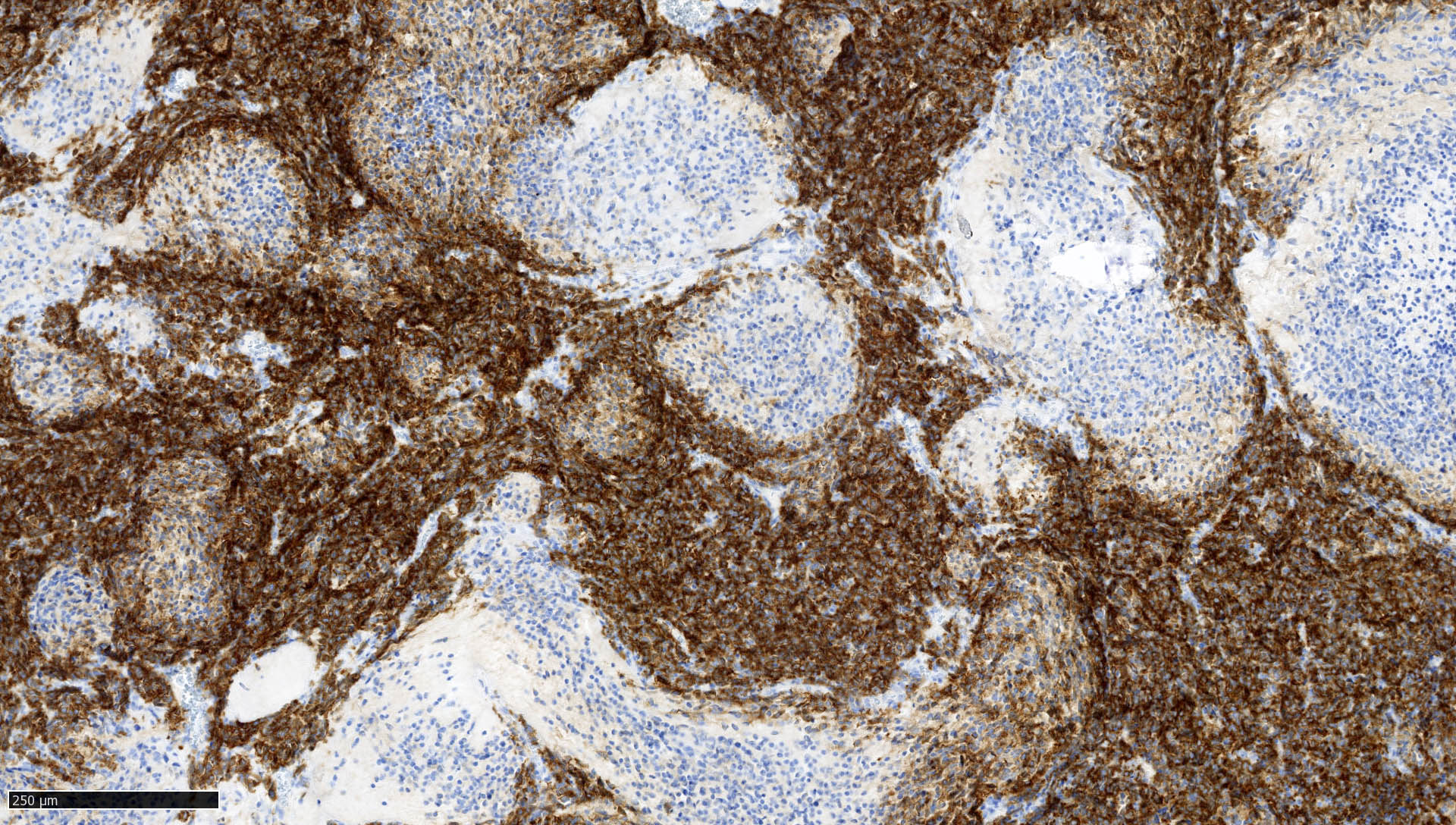
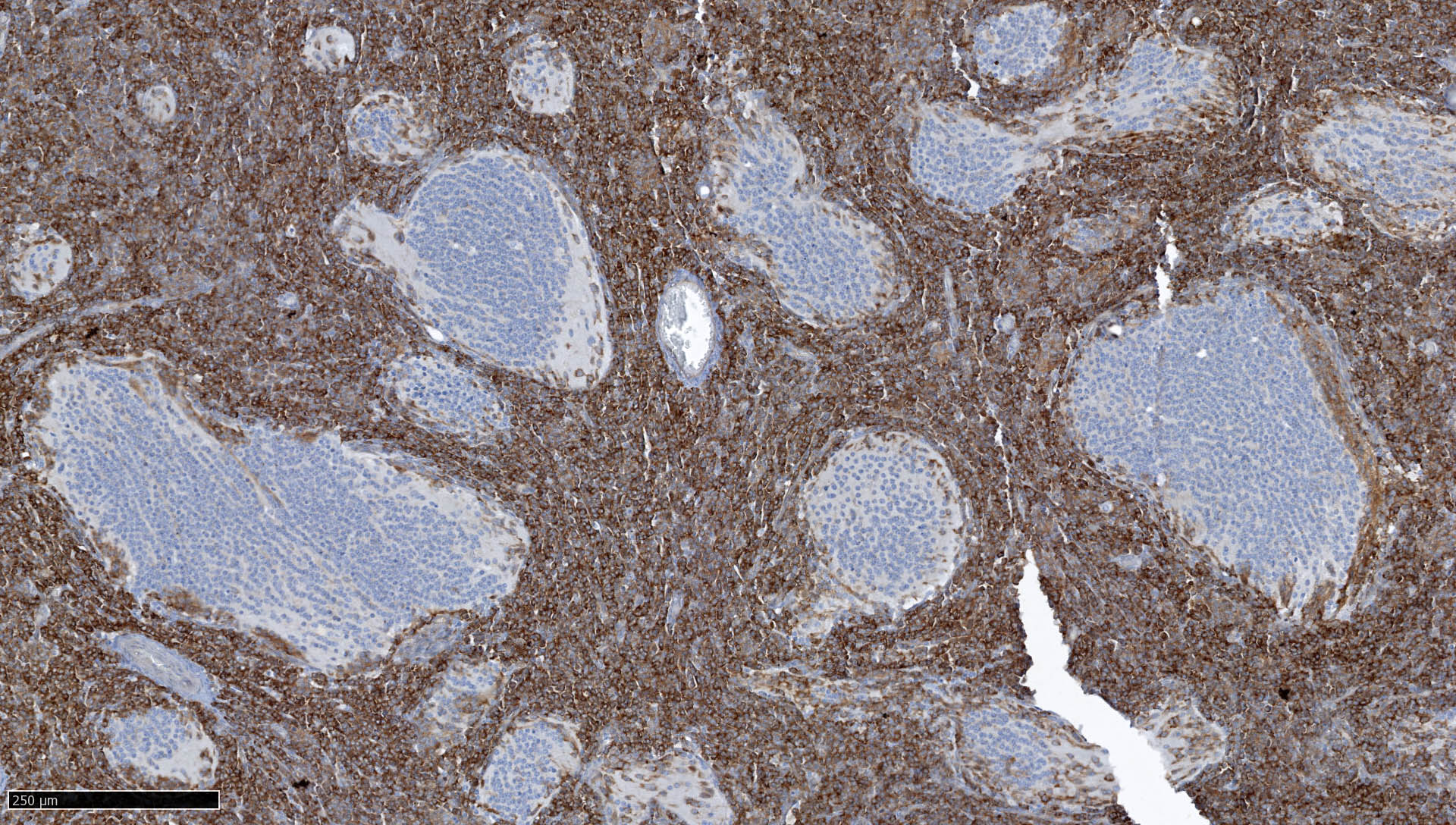
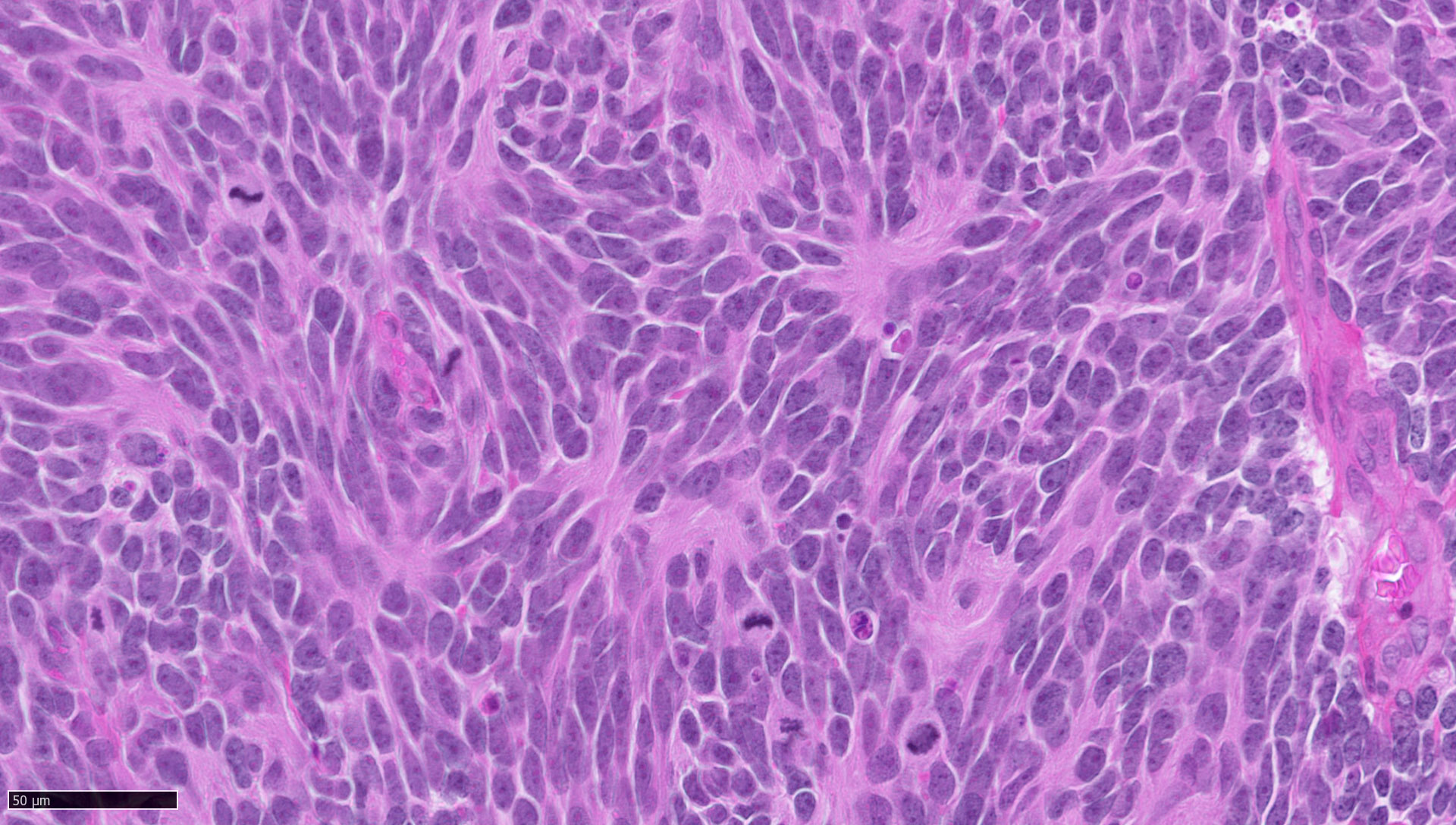
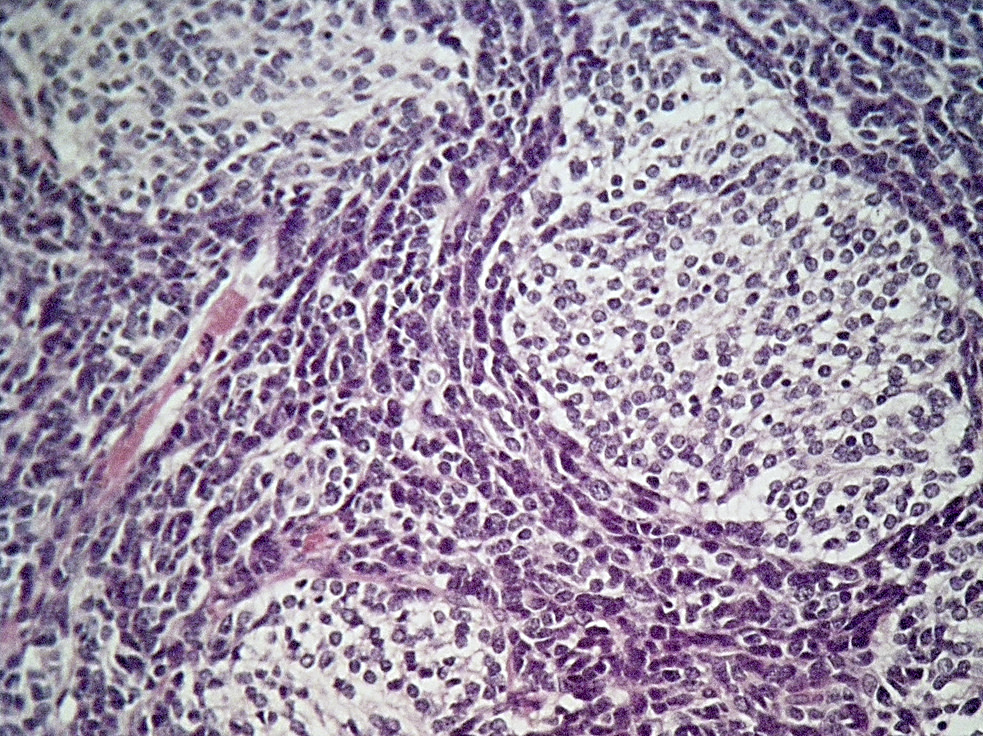
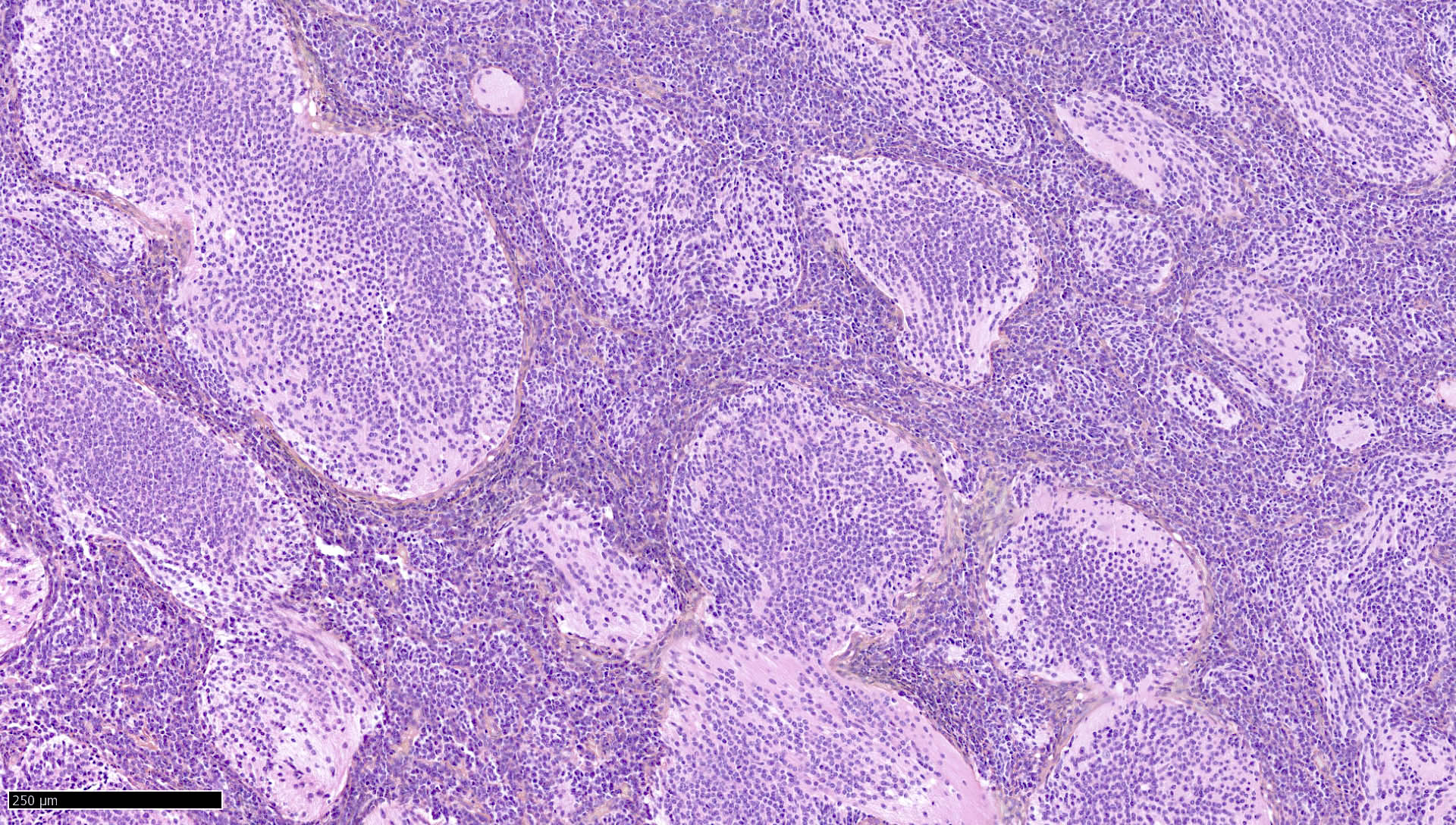
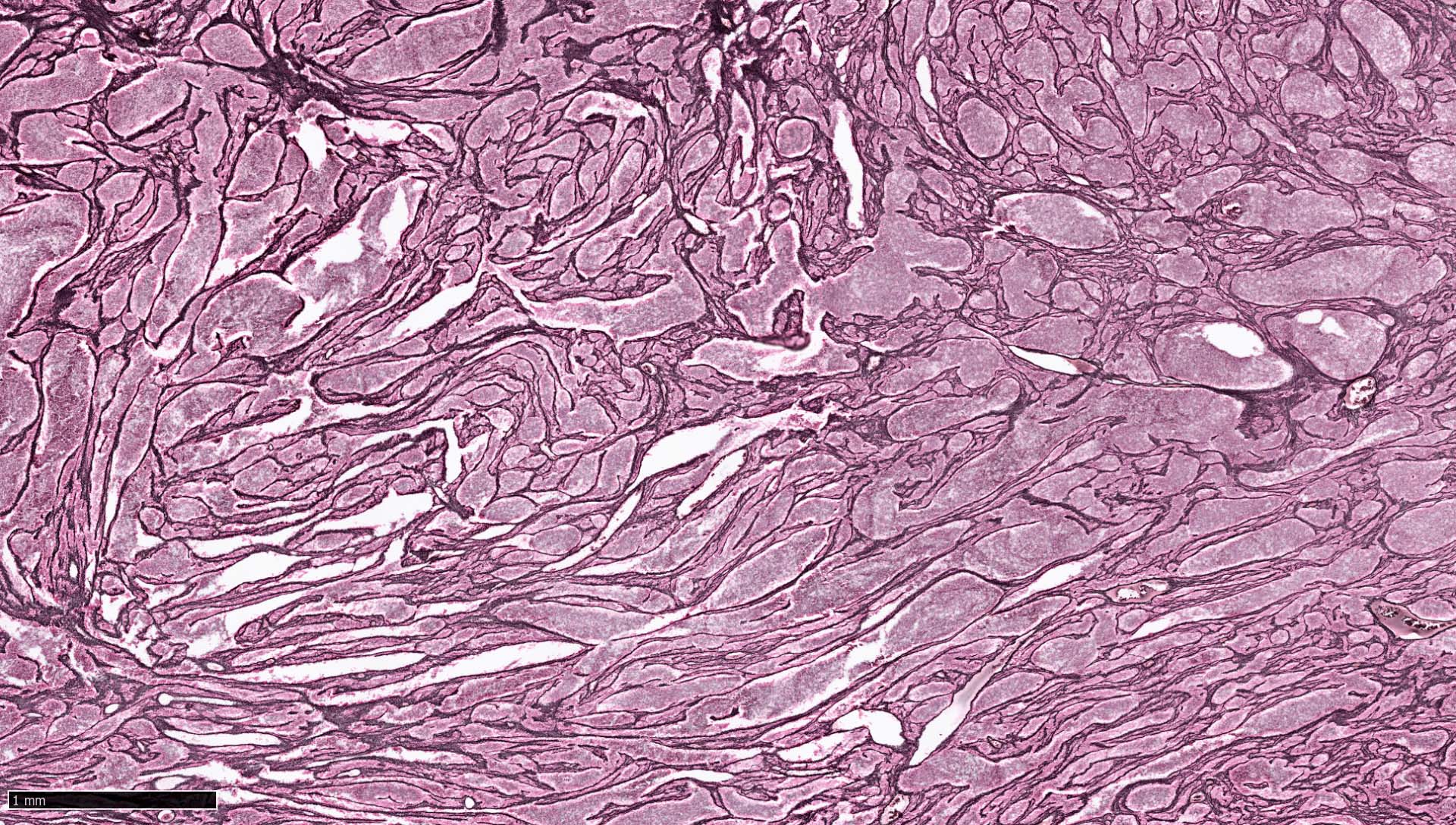
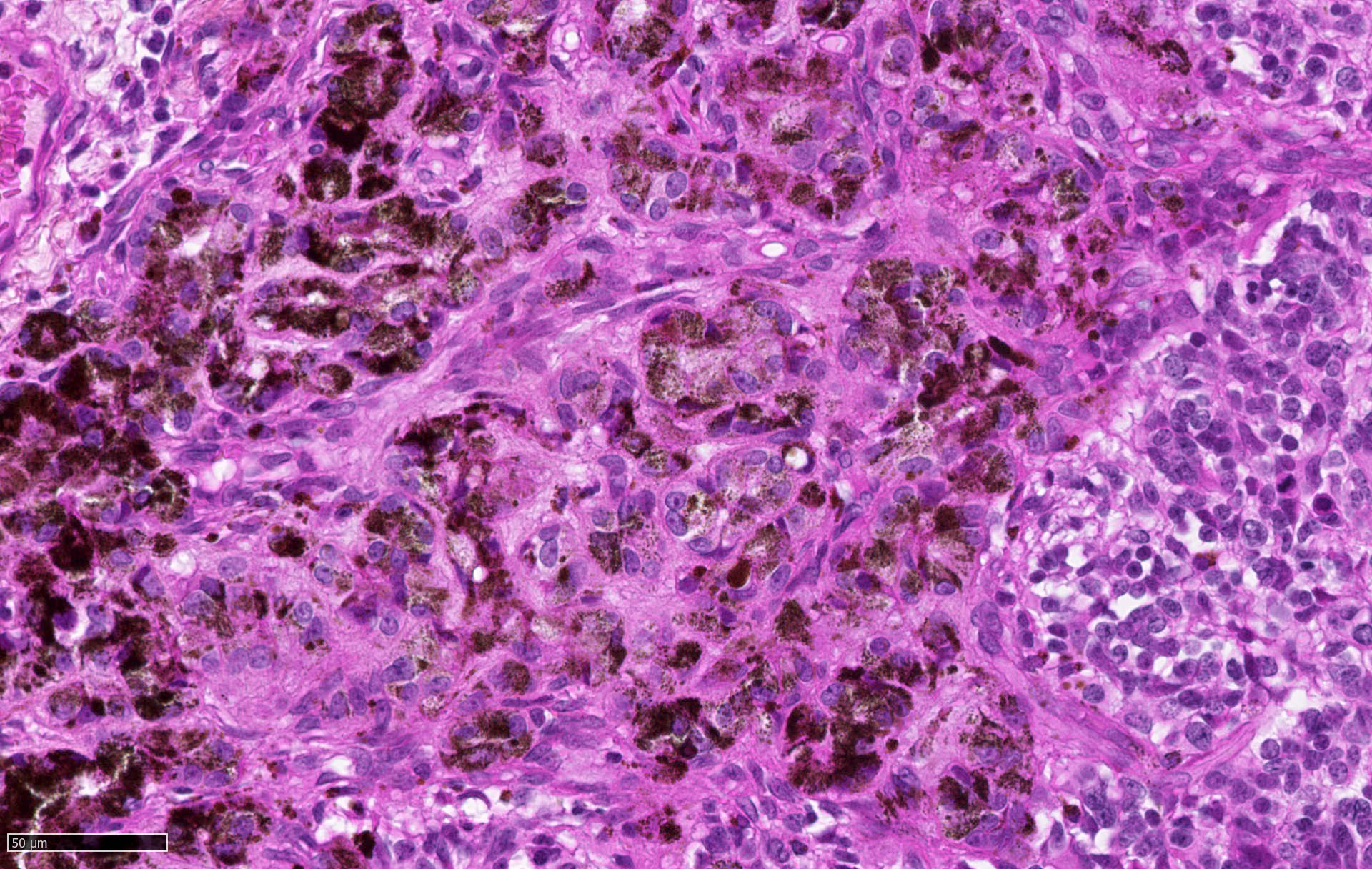
- Desmoplastic / nodular medulloblastoma (Neuropathol Appl Neurobiol 2002;28:257)
- Densely packed, undifferentiated cells with hyperchromatic and pleomorphic nuclei that produce dense intercellular reticulin fiber network with nodular reticulin free zones
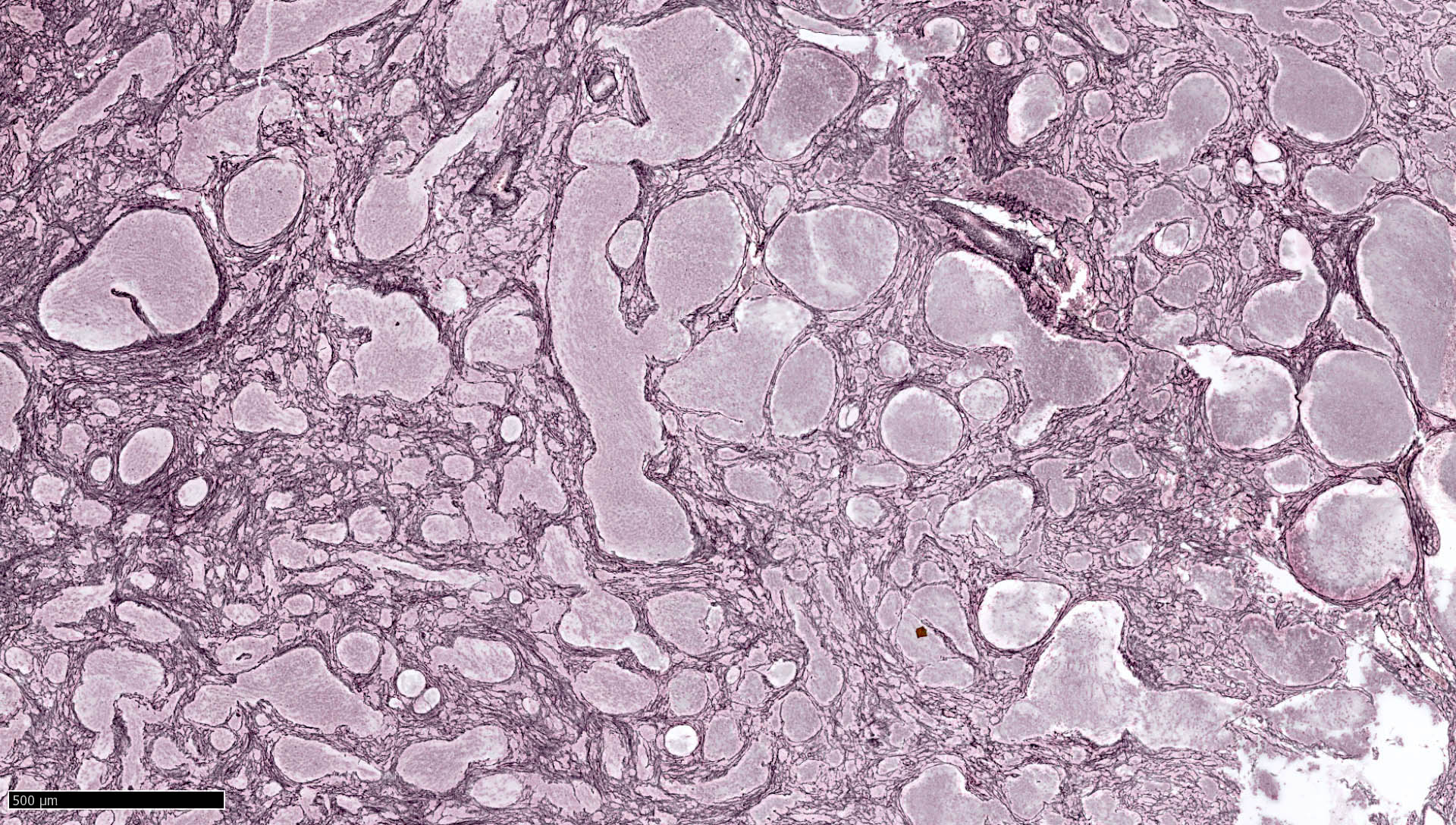
- Medulloblastoma with extensive nodularity (Neuropathol Appl Neurobiol 2002;28:257)
- Expanded lobular architecture due to reticulin free nodular zones becoming enlarged and rich in neuropil-like tissue
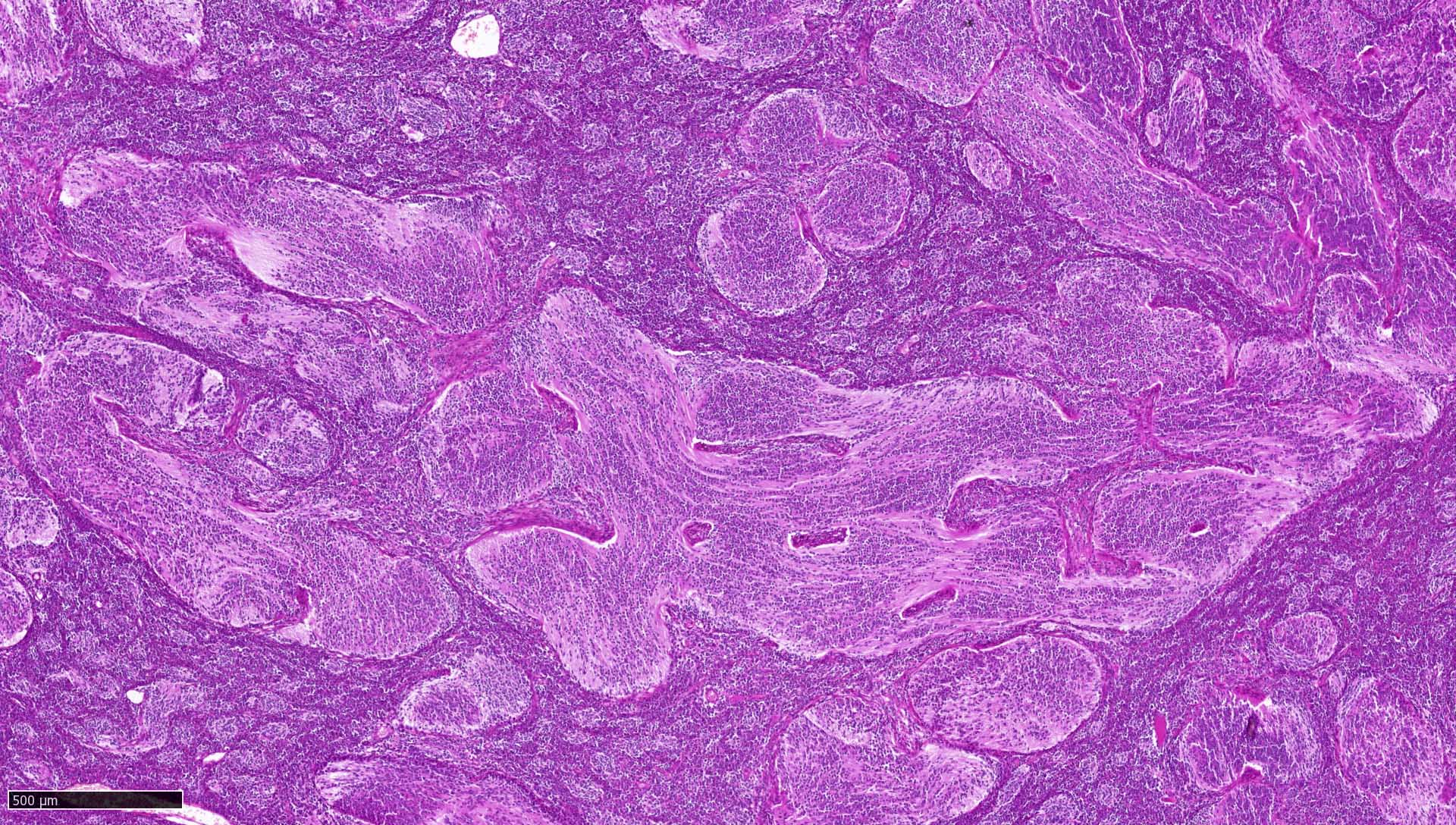
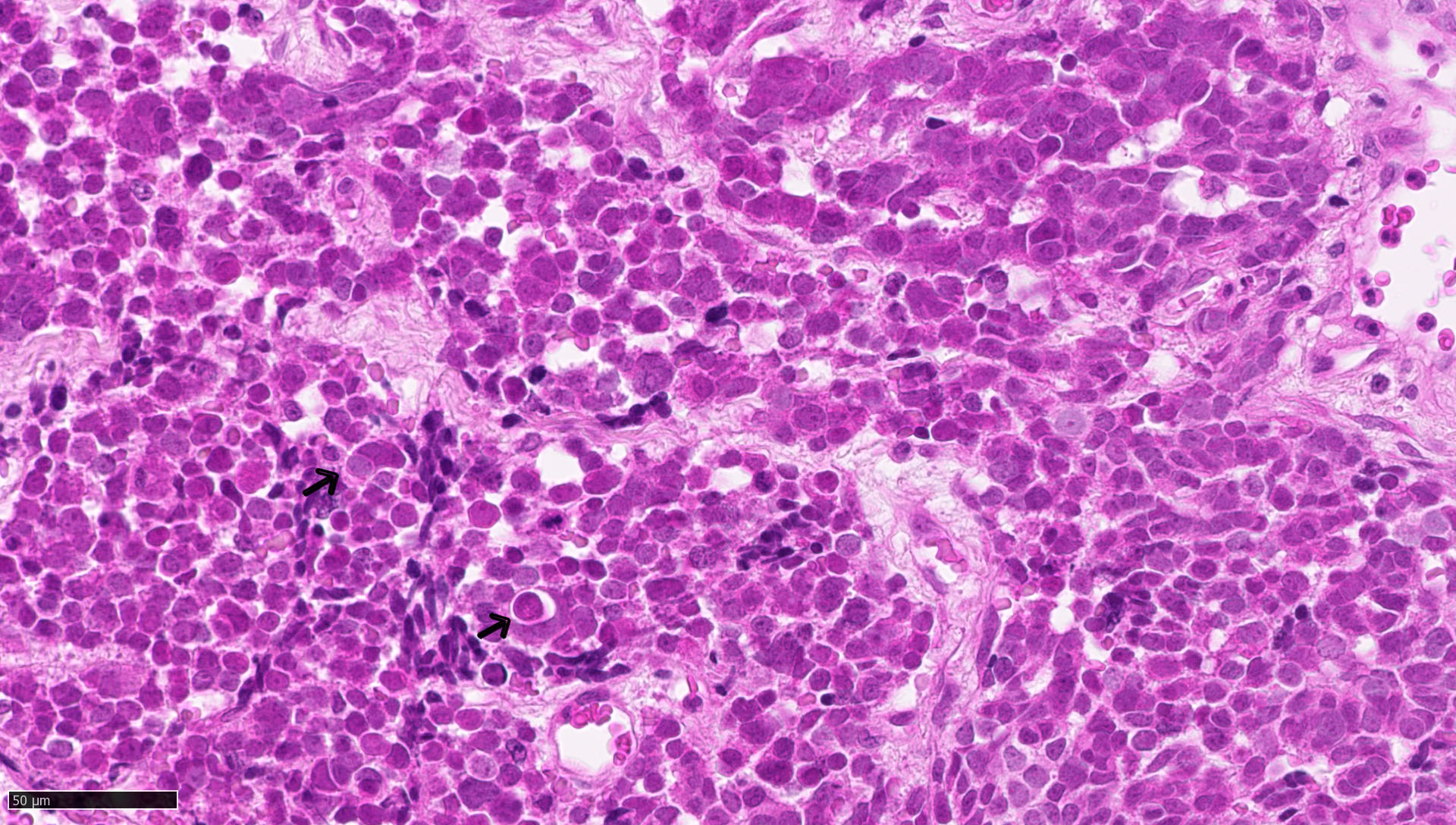
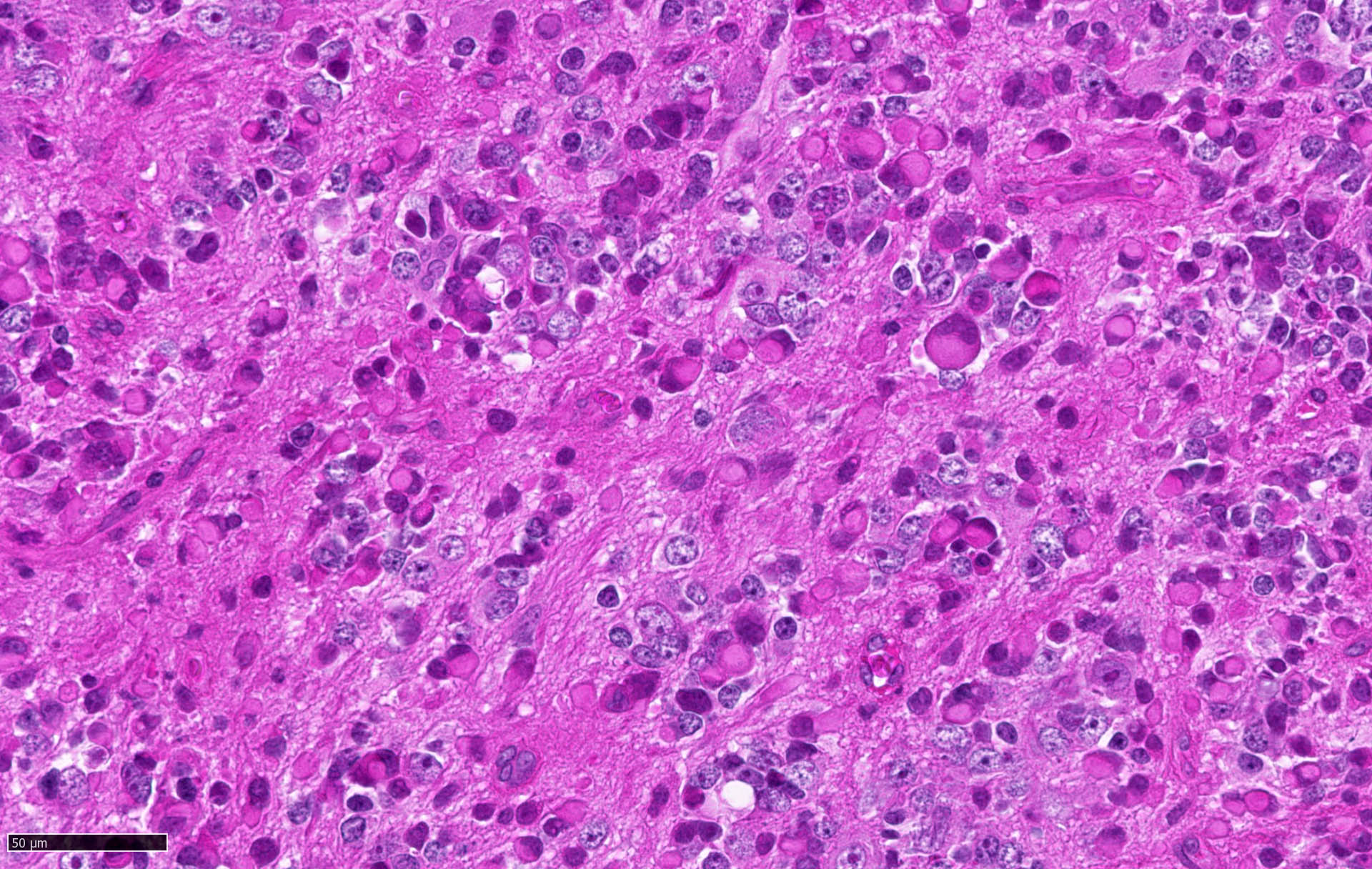
- Large cell / anaplastic medulloblastoma (Neuropathol Appl Neurobiol 2002;28:257)
- Anaplasia with marked nuclear pleomorphism, high mitotic count and high apoptotic count
- Nuclear molding and cell wrapping
- Medulloblastomas with melanotic or myogenic differentiations (Neuropathol Appl Neurobiol 2002;28:257)
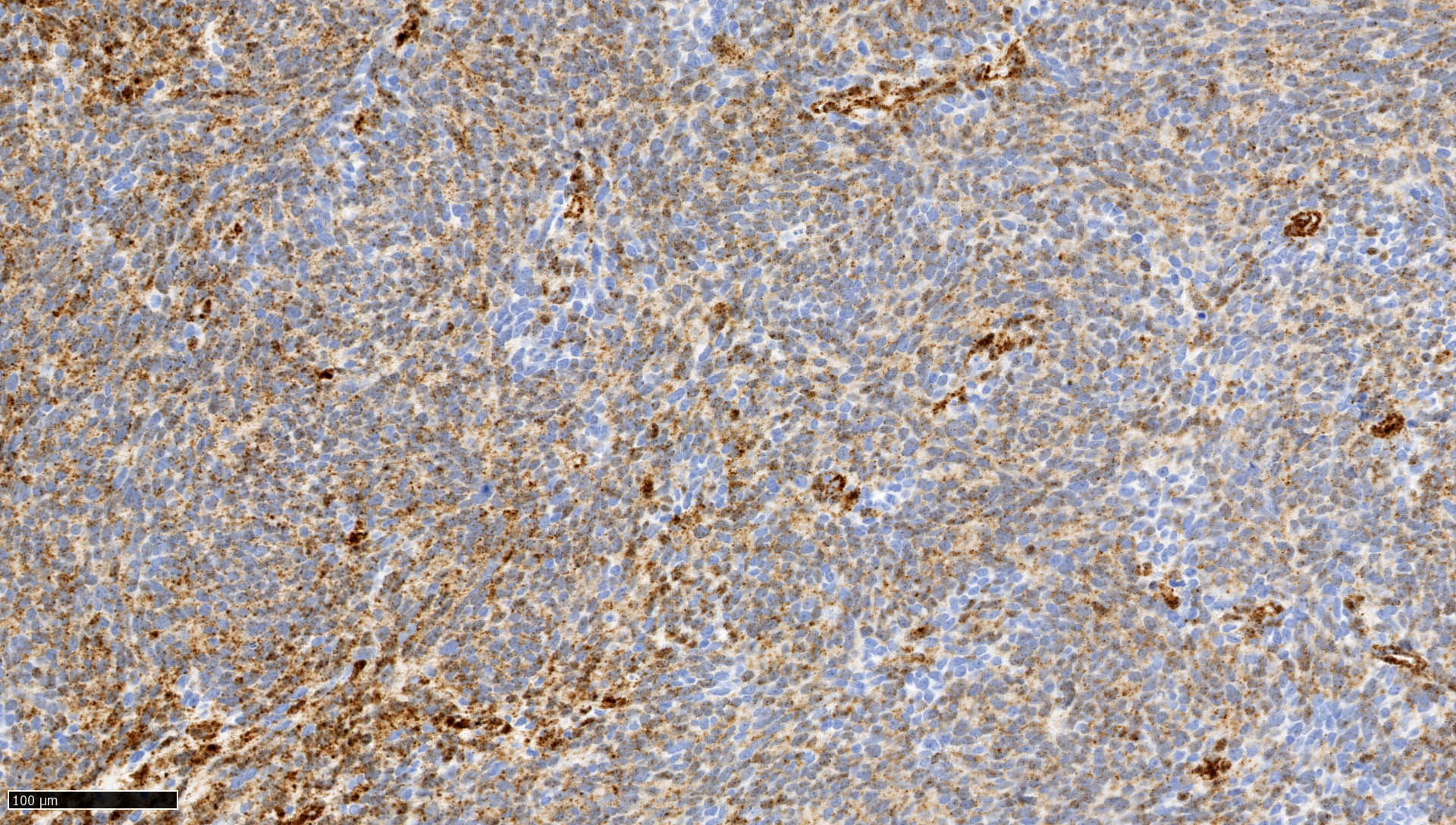
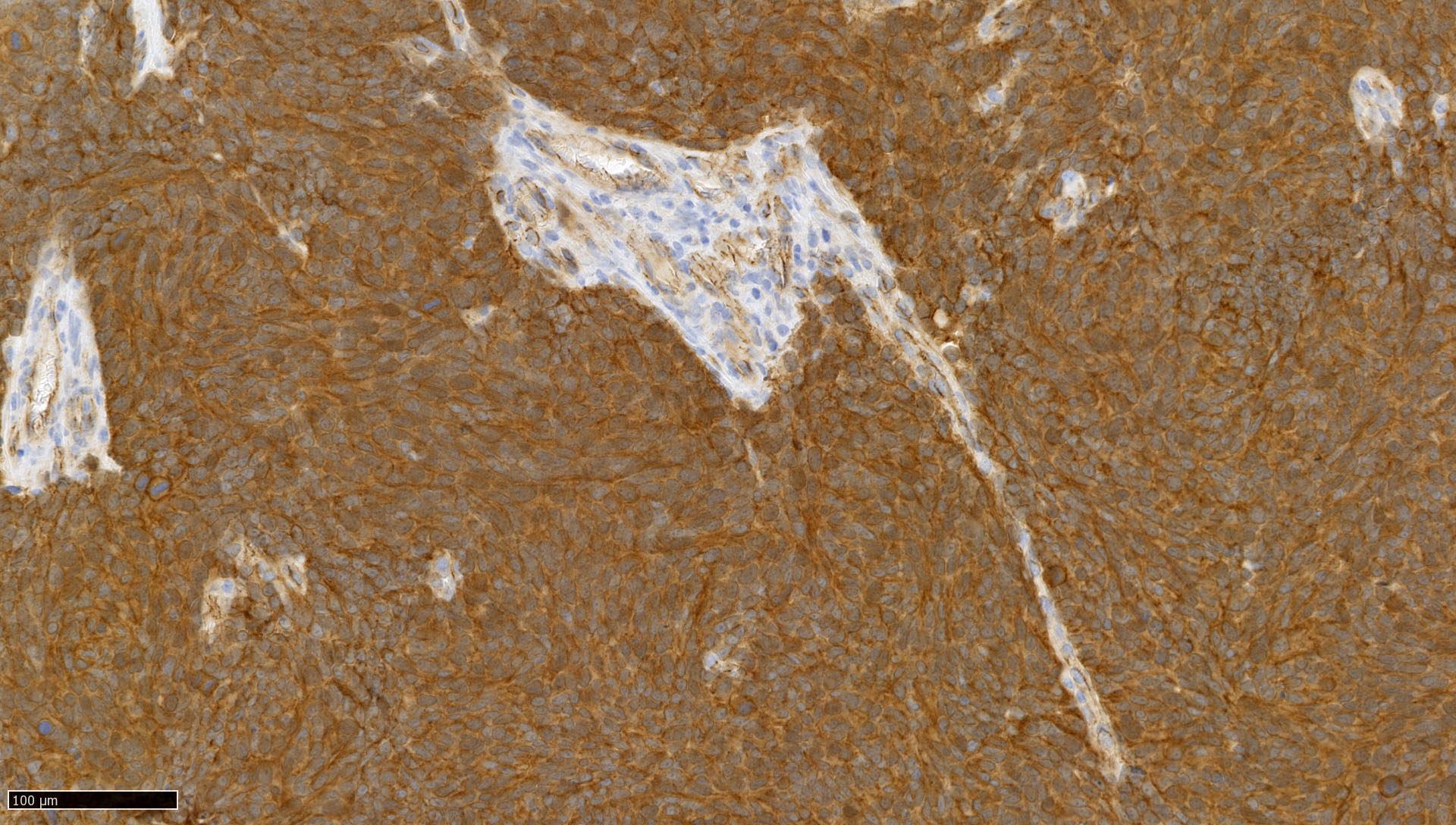
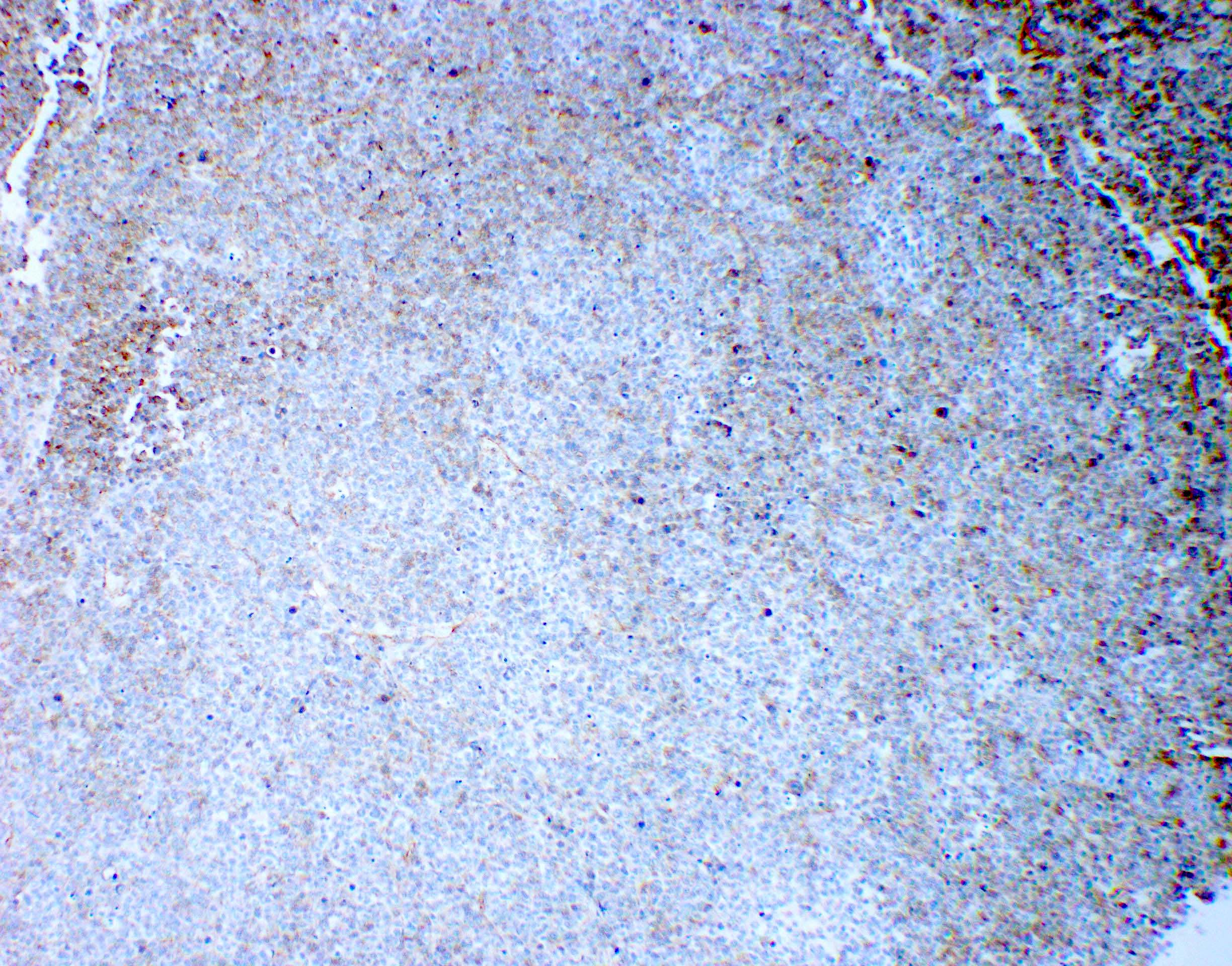
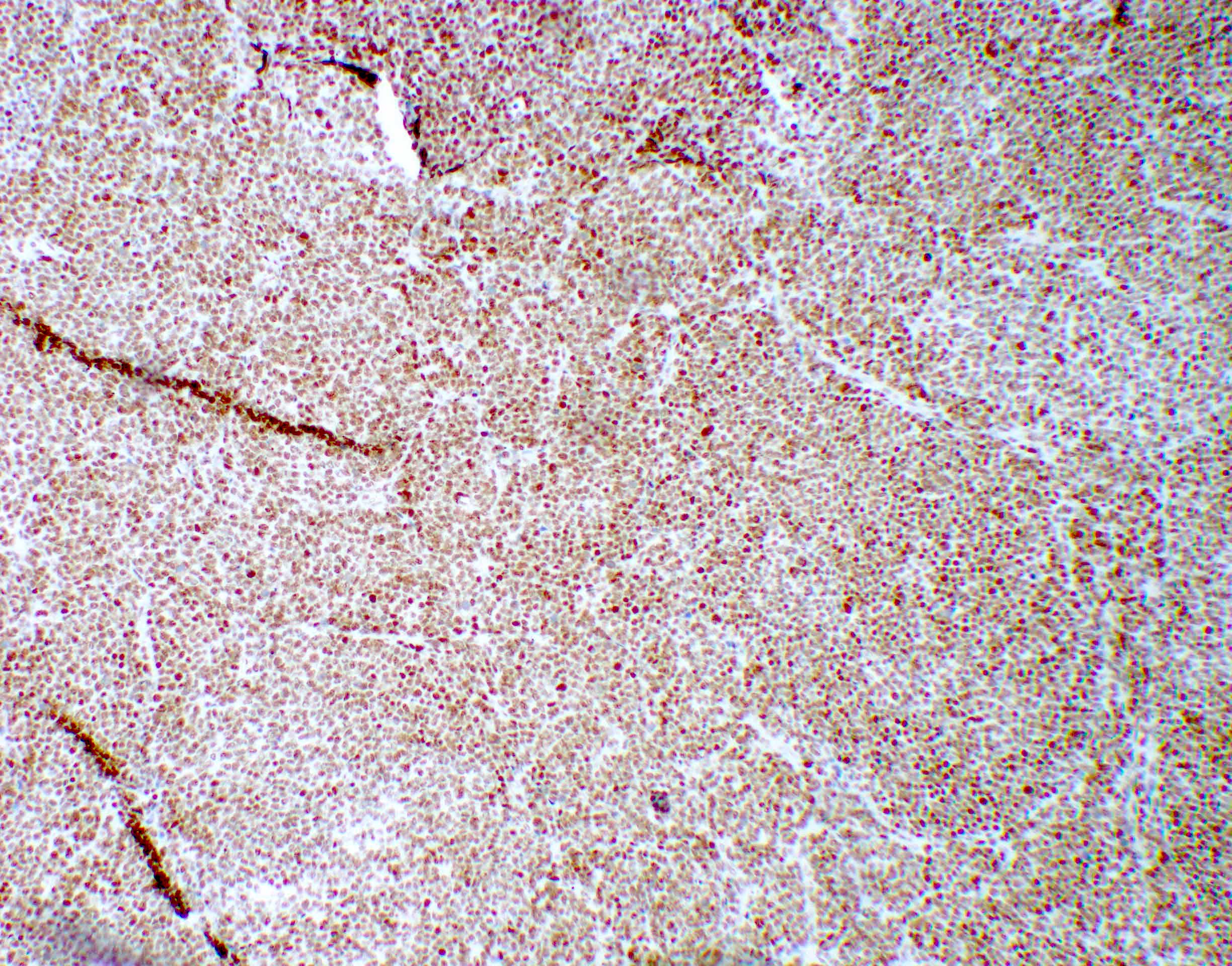
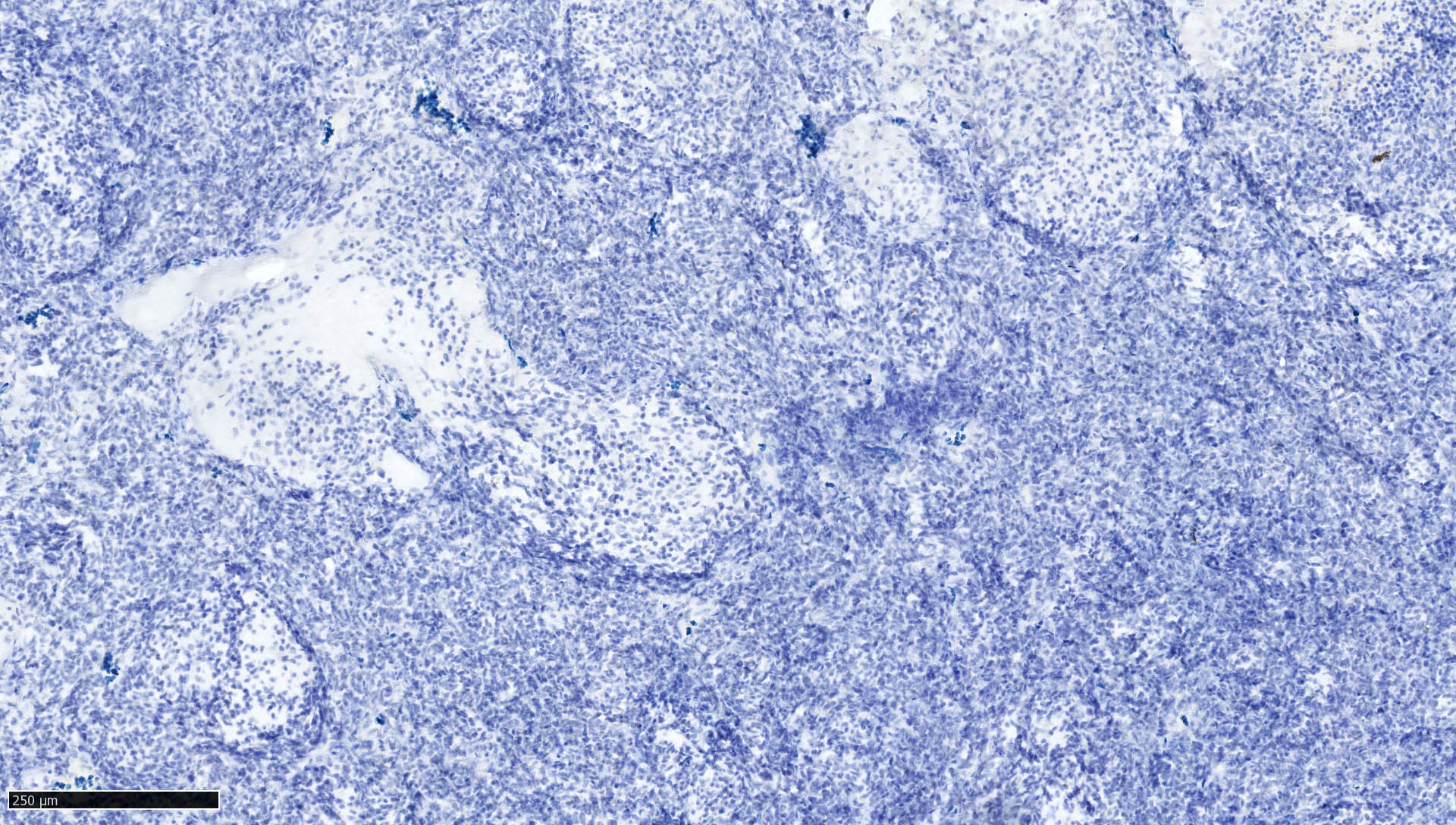
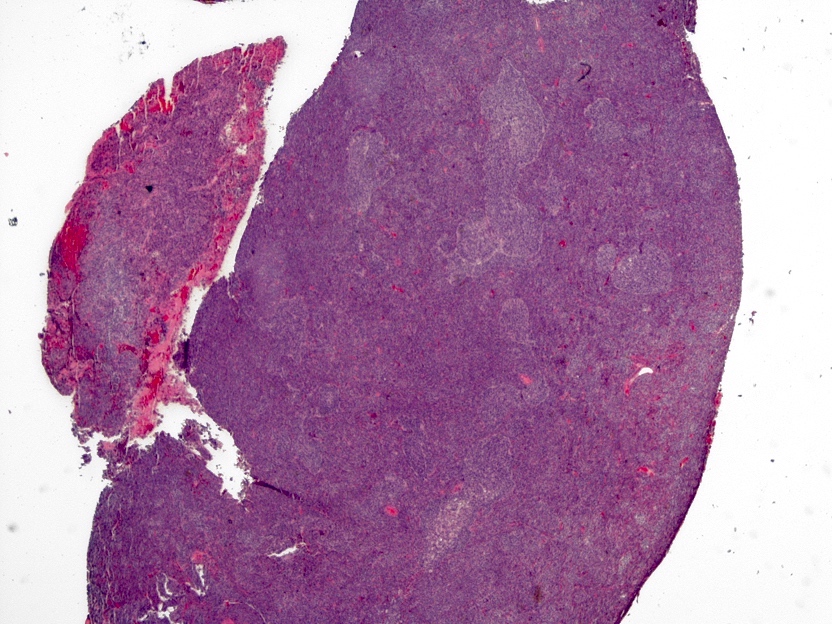
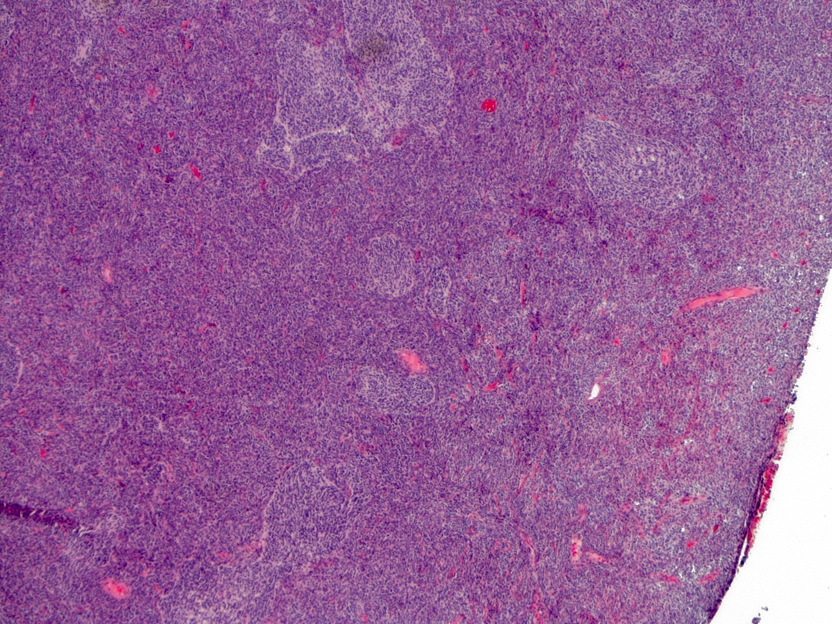
Microscopic (histologic) images
Contributed by Arnault Tauziede-Espariat, M.D., John DeWitt, M.D., Ph.D., Meaghan Morris, M.D., Ph.D.,
Nirupama Singh, M.D., Ph.D. and Eman Abdelzaher, M.D., Ph.D.
Genetically defined
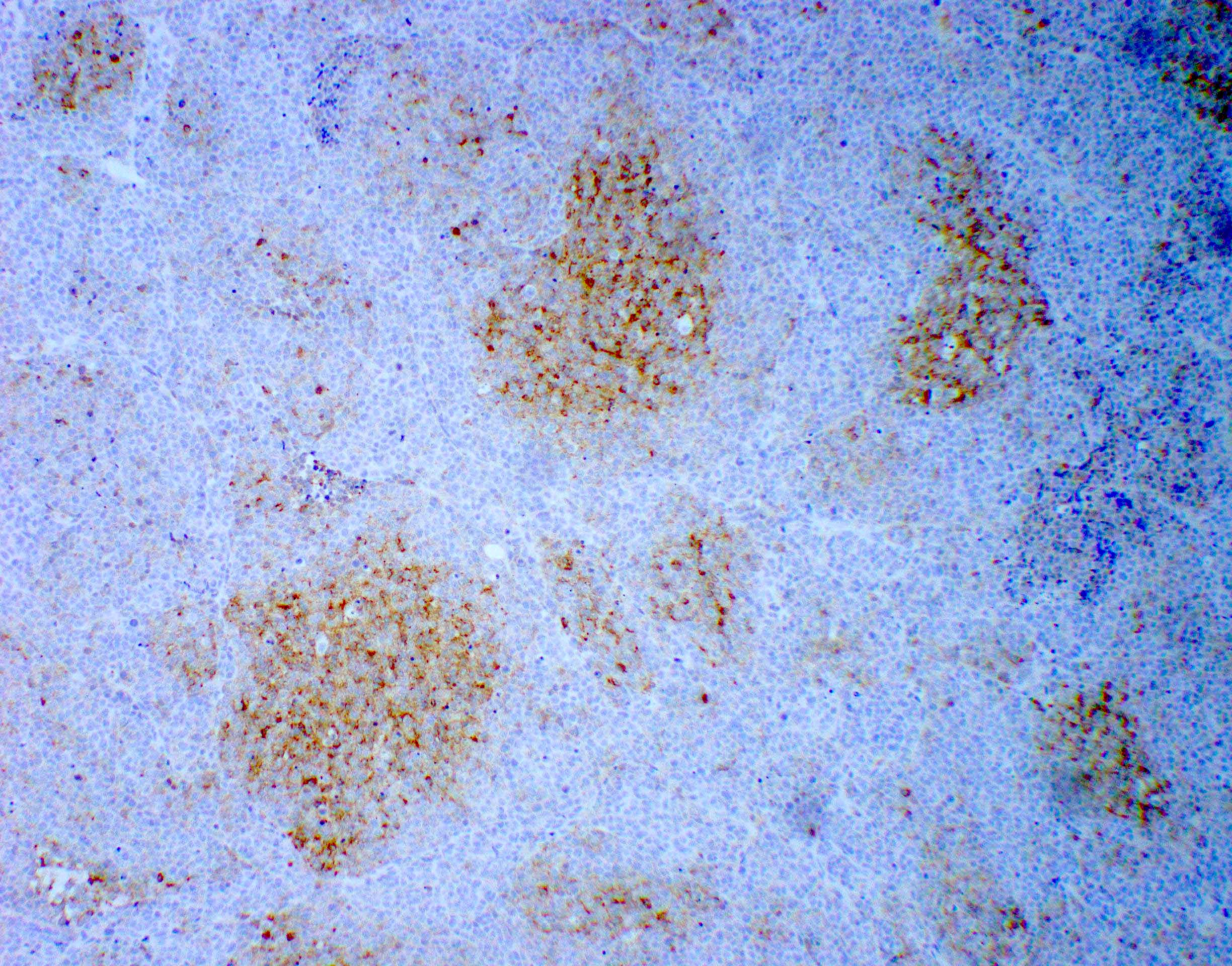
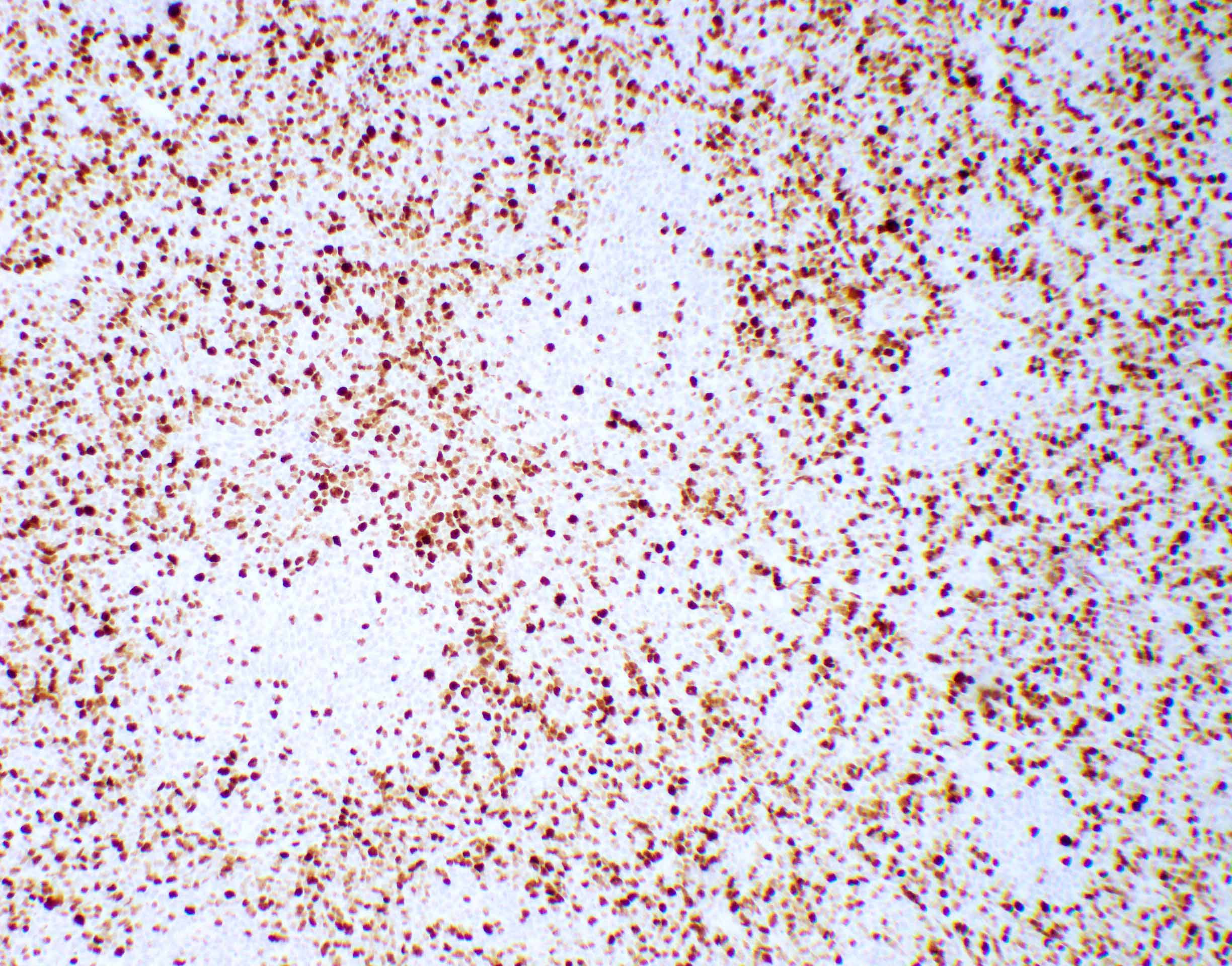
WNT (for wingless integration site) activated
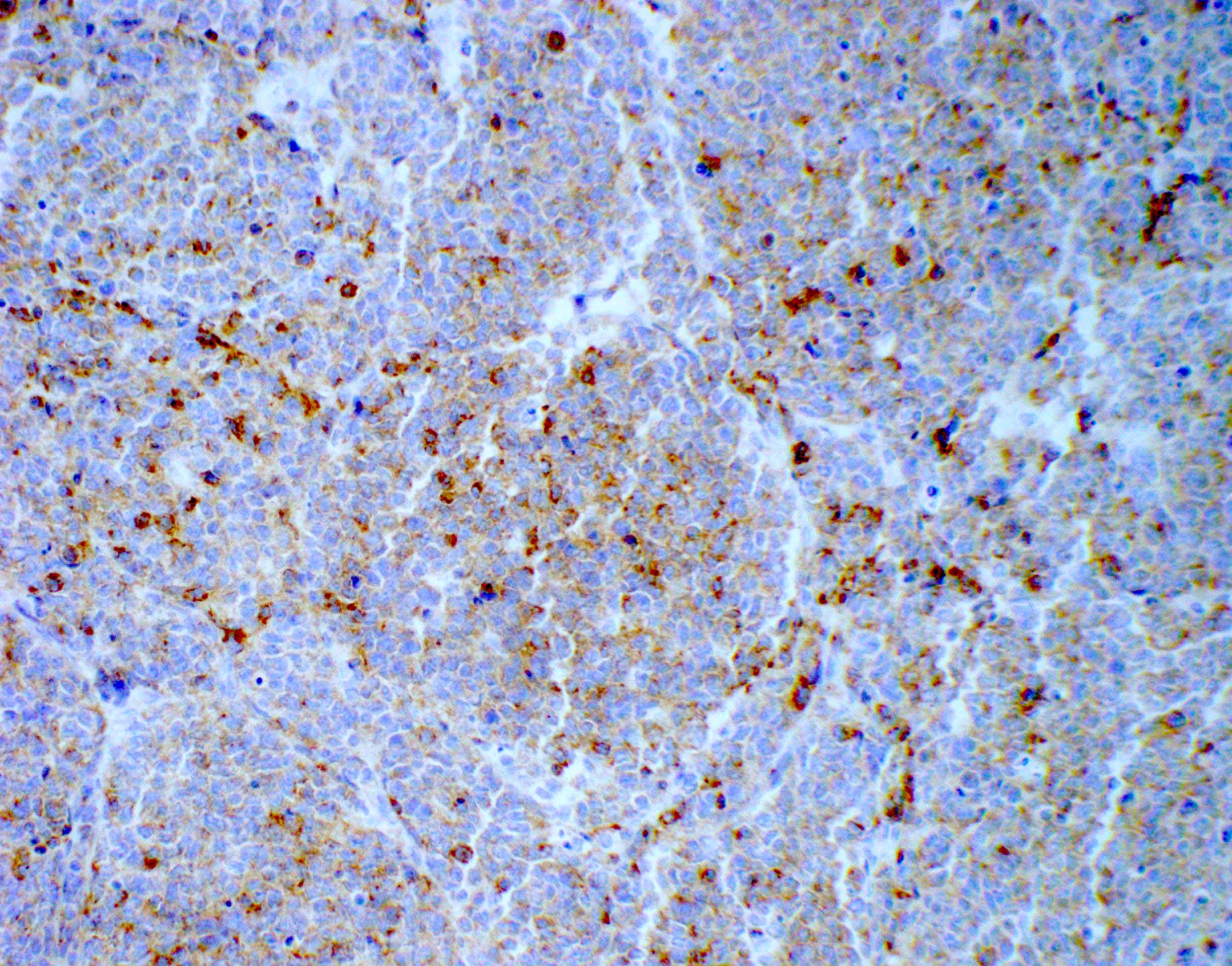
SHH (sonic hedgehog) activated (either TP53 mutant or TP53 wild type)
Histologically defined
Classic
Desmoplastic / nodular medulloblastoma
Medulloblastoma with extensive nodularity
Large cell / anaplastic medulloblastoma
Special morphology
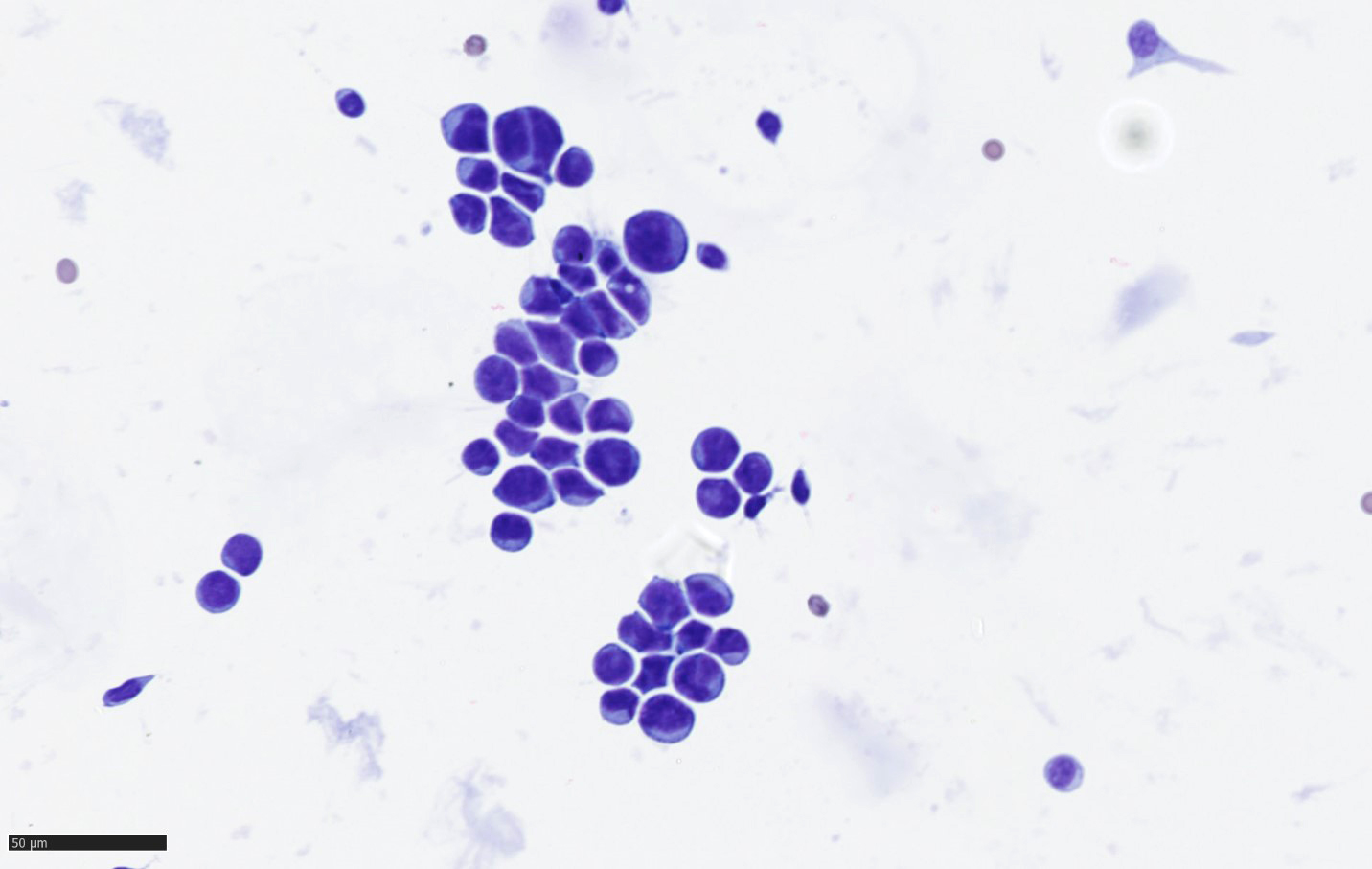
Cytology description
- Clusters of tumor cells with hyperchromatic nuclei
Positive stains
- Synaptophysin, NeuN
- Nuclear SMARCB1 / INI1 and SMARCA4 are retained
- Medulloblastoma with melanocytic differentiation: HMB45, MelanA
- Medulloblastoma with myogenic differentiation: desmin and myogenin
- Reference: Neuropathol Appl Neurobiol 2002;28:257
Negative stains
- GFAP rarely positive in tumor cells
- LIN28A
- References: Acta Neuropathol 2012;124:875, Acta Neuropathol 1985;67:1
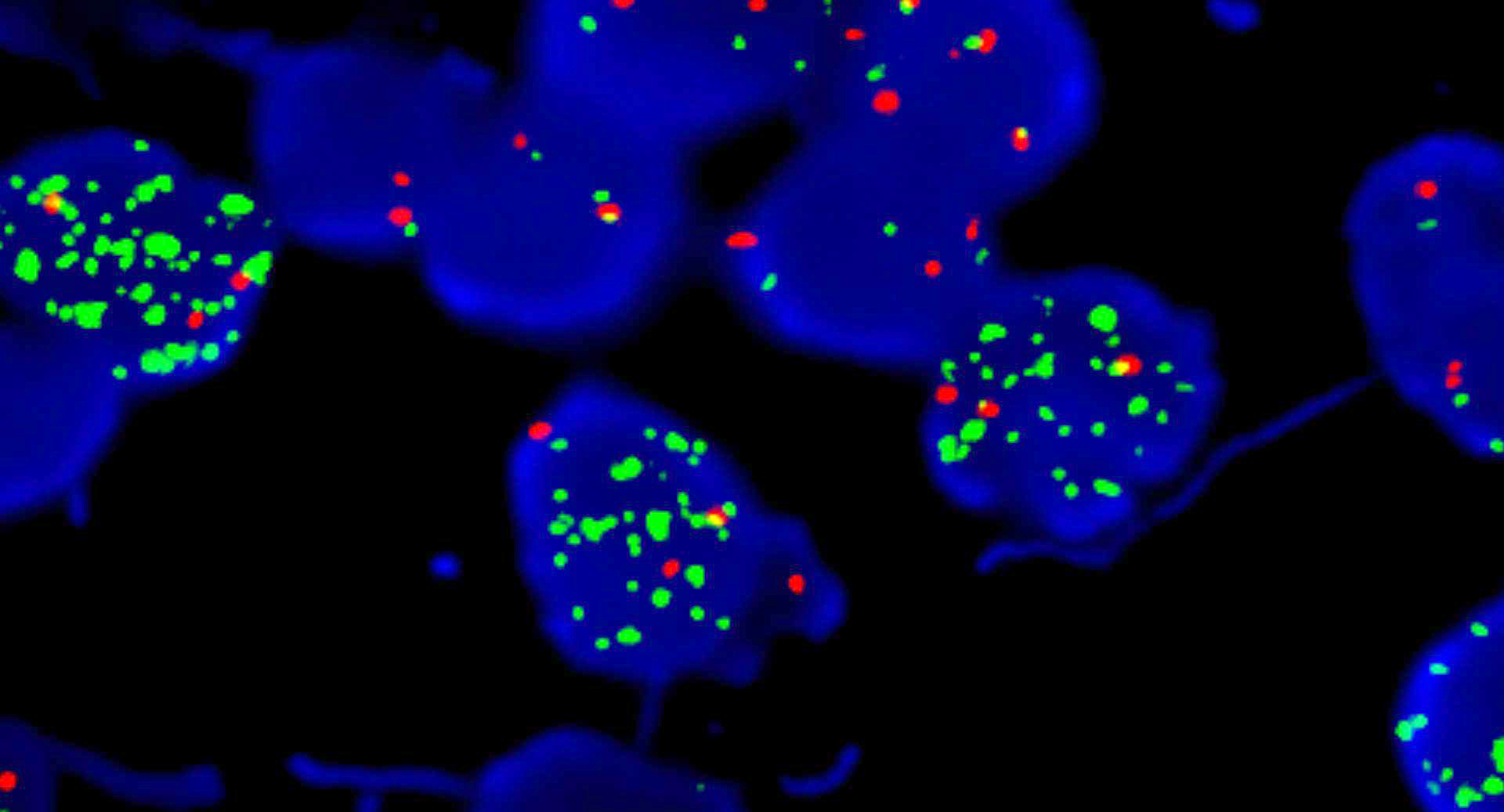
Molecular / cytogenetics description
- Genetic subgroups may be presumed due to immunohistochemical markers (Am J Surg Pathol 2021;45:558)
| Genetic subgroups | Immunohistochemical markers | |||||
| GAB1 | OTX2 | p75 NGFR | Filamin A | |||
| WNT activated | + n | - | + n and c / - | + n | - | + c |
| Non-WNT / non-SHH (groups 3 and 4) | - | - | - | + n | - | - |
| SHH activated | - (only c and m) | + c | + n and c | - | + c | + c |
Sample pathology report
- Brain, cerebellar tumor, resection:
- Classic medulloblastoma (see comment)
- Comment: Medulloblastoma, WNT activated, CNS WHO Grade 4
- Molecular pathology findings
- CTTNB1 p.Ser33Cys mutation
- Monosomy 6
Differential diagnosis
- Ependymoma:
- GFAP positive, synaptophysin negative
- Embryonal tumors with multilayered rosettes:
- LIN28A positive
- Atypical teratoid / rhabdoid tumor:
- INI1 loss
- CNS tumor with BCOR internal tandem duplication (ITD):
- BCOR positive
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true of medulloblastomas?
- Medulloblastomas, SHH activated show YAP1 and OTX2 immunoreactivities
- Medulloblastomas, WNT activated show YAP1 and GAB1 immunoreactivities
- Medulloblastomas, non-WNT / non-SHH show OTX2 expression
- Beta catenin cytoplasmic expression is specific of medulloblastomas, WNT activated
- p53 overexpression is specific of medulloblastomas, SHH activated
Board review style answer #2
C. Medulloblastomas, non-WNT / non-SHH show OTX2 nuclear expression. Answers A and D are incorrect because medulloblastomas, SHH activated show YAP1 and GAB1 immunoreactivities and beta catenin nuclear expression is specific of medulloblastomas, WNT activated. Answer B is incorrect because medulloblastomas, WNT activated show YAP1 immunoreactivity without GAB1 expression. Answer E is incorrect because p53 overexpression is evidenced in cases of Li-Fraumeni syndrome. Medulloblastomas, SHH activated are frequent in Li-Fraumeni syndrome but other histomolecular subtypes are possible.
Comment Here
Reference: Medulloblastoma
Comment Here
Reference: Medulloblastoma