Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Intraoperative frozen / smear cytology images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Multz RA, Ahrendsen JT. Diffuse astrocytoma, MYB or MYBL1 altered. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumordiffuseastrocytomamyb.html. Accessed November 28th, 2024.
Definition / general
- Glial neoplasm with infiltrative growth pattern and composed of monomorphic cells with alterations in either MYB or MYBL1 (CNS WHO grade 1)
Essential features
- Low grade diffuse glial neoplasm (CNS WHO grade 1)
- MYB or MYBL1 alteration detected by molecular or cytogenetic testing
- Often associated with long term seizures refractory to medical management
- Absence of histological features of anaplasia
Terminology
- Diffuse astrocytoma, MYB altered
- Diffuse astrocytoma, MYBL1 altered
- Not recommended
- Isomorphic astrocytoma
- Isomorphic diffuse glioma
ICD coding
- ICD-O: 9421/1 - diffuse astrocytoma, MYB or MYBL1 altered
- ICD-10: C71.9 - malignant neoplasm of brain, unspecified
- ICD-11: 2A00.0Y & XH6PH6 - other specified gliomas of brain & astrocytoma, NOS
Epidemiology
- Typically arises in children (median age is 7.2 years for MYB altered and 5.0 years for MYBL1 altered) (Cancer Cell 2020;37:569)
- Accounts for ~2% of pediatric low grade gliomas and < 0.5% of all brain tumors (Cancer Cell 2020;37:569)
- Not all patients undergo resection as children, so the age range at surgery can be variable (4 - 50 years) (Acta Neuropathol 2020;139:193)
Sites
- Majority occur in supratentorial locations (~90% overall; 58.7% cortex, 26.1% white matter / deep gray nuclei), with rare cases in the brainstem (Acta Neuropathol 2019;138:1091, Cancer Cell 2020;37:569, Childs Nerv Syst 2023;39:2509)
- Most common location is the temporal lobe (42%) (Acta Neuropathol 2020;139:193)
Pathophysiology
- Structural rearrangements in MYB or MYBL1 result in their overexpression and tumorigenesis (Acta Neuropathol 2010;120:731, Acta Neuropathol 2020;139:193)
Etiology
- Unknown
Clinical features
- Typically, patients have a long term history of epilepsy, often beginning in childhood, that is refractory to medical management (Acta Neuropathol 2020;139:193)
- Can also present with symptoms of increased intracranial pressure or cranial nerve deficits (Acta Neuropathol 2019;138:1091)
Diagnosis
- Brain imaging (computed tomography [CT] / magnetic resonance imaging [MRI])
- Surgical biopsy / resection
Radiology description
- On MRI, lesions are T2 / FLAIR hyperintense, T1 hypointense, typically do not show contrast enhancement and lack diffusion restriction (Acta Neuropathol 2020;139:193)
- Well defined borders, with cortical tumors showing some lobulation and brainstem tumors appearing slightly more infiltrative (Acta Neuropathol 2019;138:1091)
Radiology images
Prognostic factors
- Overall, patients have a good prognosis, with one study reporting a 10 year progression free survival of 89.6% and an overall survival of 95.2% (Acta Neuropathol 2019;138:1091)
- One study found that patients with MYBL1 altered tumors were more likely to progress than those with MYB altered tumors (Cancer Cell 2020;37:569)
- For patients with epilepsy, 90% become seizure free after surgery and the remainder experience decreased seizure frequency (Acta Neuropathol 2020;139:193)
Case reports
- 14 month old boy with pontine MYB altered diffuse glioma (Childs Nerv Syst 2023;39:2509)
- 21 month old girl with cerebellar MYBL1 altered diffuse glioma (Acta Neuropathol 2022;144:385)
- 5 year old boy with right temporo-occipital brain mass (Neuroradiol J 2023;36:232)
Treatment
- Surgical resection of the tumor may be curative for the patient's epilepsy or may greatly reduce the severity / frequency of seizures (Acta Neuropathol 2020;139:193)
Gross description
- Soft, friable, tan-gray to tan-white tissue
Frozen section description
Intraoperative frozen / smear cytology images
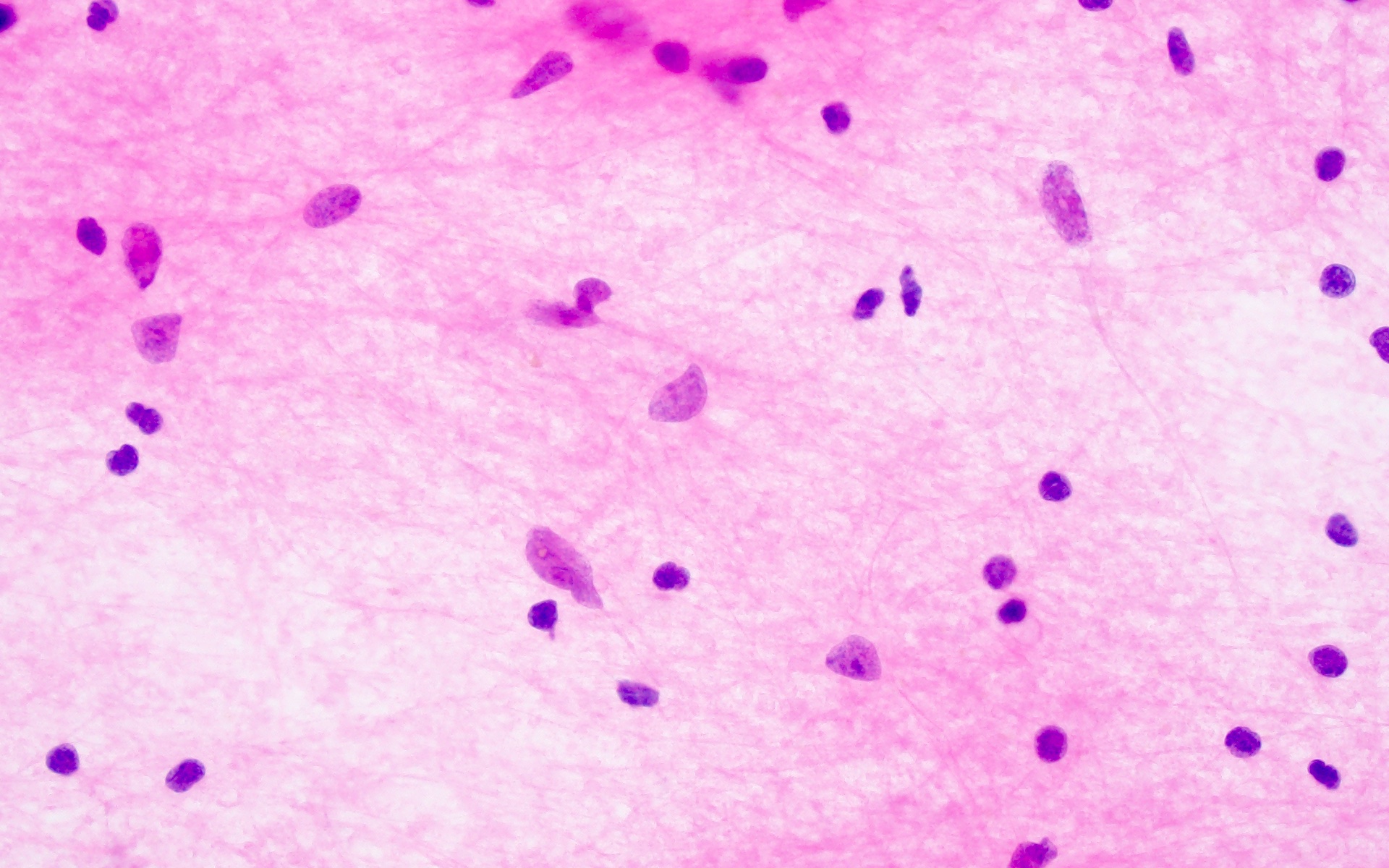
Microscopic (histologic) description
- Mildly hypercellular, infiltrative lesion composed of monomorphic glial cells
- May see secondary structure formation or microcystic changes
- Rare to virtually absent mitotic activity
- No evidence of tumor necrosis or microvascular proliferation
- Reference: Acta Neuropathol 2020;139:193
Microscopic (histologic) images
Cytology description
Positive stains
- GFAP
- Ki67 low (< 1%) (Acta Neuropathol 2004;107:381)
- ATRX (retained nuclear expression, wild type pattern)
Negative stains
- Olig2
- IDH1 R132H
- p53 (rare cells with weak expression, wild type pattern)
- EMA
- CD34 (Acta Neuropathol 2020;139:193)
- MAP2 (Acta Neuropathol 2004;107:381)
Molecular / cytogenetics description
- Structural alterations in MYB or MYBL1, creating fusion proteins (most common fusion partners are PCDHGA1, MMP16 and MAML2) (Acta Neuropathol 2020;139:193)
- MYB::QKI fusion rarely found, as this fusion is much more common in angiocentric glioma (Acta Neuropathol 2019;138:1091)
- MYB / MYBL1 copy number alterations (amplifications or deletions) can also be encountered (Acta Neuropathol 2020;139:193)
- By definition, no mutations in IDH or H3 genes
Molecular / cytogenetics images
Sample pathology report
- Brain, left temporal lobe, resection:
- Diffuse astrocytoma, MYB altered, CNS WHO grade 1
Differential diagnosis
- Astrocytoma, IDH mutant:
- Angiocentric glioma:
- Composed of bland spindle cells with unique condensation around blood vessels
- EMA positive (dot-like or ring-like)
- Almost all with MYB::QKI fusion (amplification / deletion or MYB::QKI fusion) but typically do not show alterations in MYBL1
- Diffuse low grade glioma, MAPK pathway altered:
- Ganglioglioma:
Additional references
Board review style question #1
A 7 year old with intractable seizures is found to have a 2.2 cm ovoid, T2 hyperintense, T1 hypointense mass on magnetic resonance imaging (MRI). He undergoes resection of this mass, which shows a mildly hypercellular, infiltrative lesion composed of monomorphic glial cells that do not surround blood vessels. The tumor cells are positive for GFAP and negative for Olig2 and EMA. What gene is most likely altered in this tumor?
- IDH1
- MN1
- MYB
- TERT promoter
- TSC2
Board review style answer #1
C. MYB. The histology is that of a low grade infiltrating glioma that lacks Olig2 expression and occurs in a child, all consistent with a diagnosis of diffuse astrocytoma, MYB or MYBL1 altered. Answer B is incorrect because MN1 is an alteration seen in astroblastoma, which typically shows rosette or papillary architecture. Answer A is incorrect because mutations in IDH1 are seen in adult type diffuse gliomas (which do not typically occur in patients this young) and tumor cells are positive for both GFAP and Olig2. Answer E is incorrect because TSC2 mutations are associated with subependymal giant cell astrocytoma (SEGA), which will show a circumscribed lesion composed of large and often pleomorphic or multinucleated astrocytic cells. Answer D is incorrect because alterations in TERT promoters are typically encountered in glioblastoma and oligodendroglioma, both of which would show Olig2 immunoreactivity, typically occur in older patients and would display more prominent hypercellularity and atypia.
Comment Here
Reference: Diffuse astrocytoma, MYB or MYBL1 altered
Comment Here
Reference: Diffuse astrocytoma, MYB or MYBL1 altered