Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3 | Board review style question #4 | Board review style answer #4Cite this page: Burns DK. Tuberculosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstuberculosis.html. Accessed March 31st, 2025.
Definition / general
- An infectious / inflammatory process within the central nervous system (CNS) that can involve the meninges, brain parenchyma or both, and is typically composed of areas of cheese-like (caseous) necrosis, lymphocytes, macrophages and multinucleated giant cells reacting to the presence of Mycobacterium tuberculosis
- Less commonly, the inflammatory infiltrates can contain a significant number of neutrophils, particularly in acute cases
Essential features
- Leptomeningeal or localized parenchymal infections that occur via hematogenous dissemination of inhaled M. tuberculosis
- This can occur at the time of initial infection or later in the course of more chronic, established infections
- Infection occurs when M. tuberculosis is inhaled and interacts with pulmonary alveolar macrophages
- Low level bacteremia is present during the early stages of infection, during which time seeding of the leptomeninges or brain parenchyma can occur
- Bacteremia can persist in patients with progressive disease or recur in patients with reactivation of latent infection
- Radiographic imaging can provide important clues to the correct diagnosis
- Classical features of leptomeningeal disease include prominent basilar leptomeningeal enhancement, sometimes associated with infarcts in deep gray and white matter of the cerebral hemispheres
- Parenchymal lesions (tuberculomas or less commonly, tuberculous abscesses) present as solitary or multiple mass lesions, most commonly in the cerebral hemispheres in adults or in the cerebellum in children, often associated with ring enhancement
- Identification of M. tuberculosis bacilli in cerebrospinal fluid or in biopsies of parenchymal lesions via acid fast stains or culture or the identification of M. tuberculosis related DNA sequences by PCR or similar nucleic acid amplification techniques is required for a definitive diagnosis
Terminology
- Diagnostic terms include tuberculous meningitis, meningeal tuberculosis and tuberculomas
ICD coding
- ICD-10:
- A17 - tuberculosis of the nervous system
Epidemiology
- Tuberculosis (TB) remains a leading cause of morbidity and mortality, with an estimated 10.6 million cases noted worldwide in 2021 and an estimated 1.6 million deaths during the same year (WHO: Global Tuberculosis Report 2022 [Accessed 6 April 2023])
- The number of newly diagnosed TB cases increased by 3.6% between 2020 and 2021, reversing a steady decline in new cases noted over the preceding 2 decades
- CNS tuberculosis is estimated to occur in ~1% of all TB cases
- Children and HIV positive individuals account for a disproportionate number of cases of CNS TB
Sites
- Clinically apparent infections can develop within the leptomeninges (TB meningitis) or as localized, space occupying lesions within the parenchyma of the brain or spinal cord (tuberculomas or less commonly, tuberculous abscesses)
- Tuberculomas may also occur in the leptomeninges, dura and extradural spaces
- TB meningitis and tuberculomas may coexist
- TB spondylitis (Pott disease) involving the thoracic or lumbosacral vertebrae, although not strictly a CNS infection, can also cause significant neurological disease when the compromised vertebrae collapse and lead to mechanical injury of the spinal cord (J Spinal Cord Med 2011;34:440)
Pathophysiology
- Infection with M. tuberculosis occurs when individuals inhale airborne droplets that contain viable bacilli
- Droplets measuring < 5 μm in diameter reach pulmonary alveoli, where bacilli come into contact with alveolar macrophages
- In the presence of alveolar surfactant protein A, mycobacterial surface proteins known as pathogen associated molecular patterns bind to receptors expressed on alveolar macrophages, including CD44, Fc, mannose, immunoglobulin, complement and Toll-like receptors (Front Cell Infect Microbiol 2021;10:618414, Semin Immunol 2014;26:471, Microbes Infect 2001;3:37)
- Binding of the mycobacteria to these receptors facilitates phagocytosis of the bacilli and fusion of engulfed microorganisms with lysosomes (Front Cell Infect Microbiol 2021;10:618414)
- These interactions also trigger the generation of multiple chemokines and cytokines that activate, in turn, a host T helper cell mediated immune response and the formation of granulomas with varying degrees of caseating necrosis
- During the initial phase of the host response, a low level bacteremia occurs before the mycobacteria are completely contained within macrophages and dissemination of the organisms to other oxygen rich sites, including the CNS, can occur (Clin Microbiol Rev 2008;21:243)
- Host reaction to mycobacterial antigens is complex, containing elements that promote inactivation and killing of the bacilli, as well as additional elements that paradoxically allow M. tuberculosis to evade the host immune response (Semin Immunol 2014;26:471)
- Although most mycobacteria are eventually well contained in immunocompetent hosts, a small number of organisms may remain viable even while sequestered in macrophages, resulting in continuous remodeling of granuloma (Front Cell Infect Microbiol 2021;10:618414)
- Reactivation of latent infection, with release of microorganisms sequestered within macrophages, can occur whenever the host's normal immune response is compromised, as in instances of malnutrition, HIV or iatrogenic immunosuppression (Front Cell Infect Microbiol 2021;10:618414)
- As in the case of bacteremia occurring in the early stages of M. tuberculosis infection, hematogenous dissemination of organisms can also occur during such periods of reactivation
- Circulating cytokines, particularly TNFa, appear to play a role in increasing blood - brain barrier permeability and allowing mycobacteria to gain access to the CNS, where organisms may find their way to the meninges, brain parenchyma or spinal cord (Front Cell Infect Microbiol 2021;10:618414, Clin Microbiol Rev 2008;21:243)
- Microglia appear to be the major target for mycobacteria that gain access to the CNS (Clin Microbiol Rev 2004;17:942, Clin Microbiol Rev 2008;21:243)
- Within the CNS M. tuberculosis interacts with surface receptors on resident microglia; among these, the CD14 appears to play a particularly important role in the ingestion of mycobacteria by microglial cells (Infect Immun 1995;63:1598)
- M. tuberculosis infected microglia release a host of cytokines and chemokines, including TNFa, IL6, IL1b and CXCL10; IL1 and IL10 production, in contrast, is inhibited, particularly with more virulent strains of M. tuberculosis (Clin Microbiol Rev 2008;21:243, Neurochem Int 2004;44:381)
- Interactions between M. tuberculosis and resident microglia trigger a sequence of cellular events to those seen in the infection of pulmonary alveolar macrophages, resulting in the formation of single or multiple granulomas termed Rich foci, named after the work of Dr. Arnold Rich at The Johns Hopkins Hospital (Bull Johns Hopkins Hosp 1933;52:5)
- Depending upon their location, rupture of Rich foci release mycobacteria into the subarachnoid space or CNS parenchyma, resulting in the development of meningitis or localized parenchymal infections, respectively (J Neurol Sci 2021;421:117278)
Etiology
- Although a number of different mycobacterial species can cause human infection, virtually all cases of CNS TB are caused by Mycobacterium tuberculosis, a nonmotile, strictly aerobic bacillus
- Cell wall of M. tuberculosis is rich in lipids, including mycolic acid, cord factor and wax D, which confer a significant degree of resistance to lysosomal bactericidal activity within macrophages (J Neurol Sci 2021;421:117278)
- Characterized by a slow generation time in vivo and in vitro, with positive cultures often taking 4 - 6 weeks to develop (J Neurol Sci 2021;421:117278)
Clinical features
- Tuberculous meningitis
- Most common form of CNS tuberculosis (70 - 80% of cases) (J Neurol Sci 2021;421:117278)
- Highest risk in children and in patients with histories of immunosuppression, malnutrition or alcohol abuse (Clin Neuroradiol 2019;29:3, Afr Health Sci 2011;11:116)
- Presents with nonspecific prodromal phase that includes low grade fever, fatigue, weight loss and night sweats
- Prodromal phase is followed by more classical signs of meningitis, including headache, neck stiffness, photophobia, altered mental status and seizures; meningeal signs typically develop more slowly than those in pyogenic bacterial meningitis but may present more acutely, particularly in children
- Cranial nerve (CN) deficits are common, particularly abnormalities involving CN VI, CN II and less commonly CN III and CN IV (Curr Opin Neurol 1994;7:191, Afr Health Sci 2011;11:116, J Neurol Sci 2021;421:117278. Clin Microbiol Rev 2008;21:243)
- Additional neurological abnormalities, including hemiplegia and a variety of movement disorders, may develop owing to vasculitis involving penetrating lenticulostriate arteries (Curr Opin Neurol 1994;7:191, Afr Health Sci 2011;11:116, J Neurol Sci 2021;421:117278)
- Tuberculoma
- May occur independently or in association with tuberculous meningitis
- Multifocal, supratentorial lesions are more common in adults; solitary and infratentorial lesions are more common in children (J Neurol Sci 2021;421:117278, Postgrad Med J 1999;75:133)
- Clinical manifestations include headache and focal neurological deficits, the latter determined by the location of the lesion(s)
- Tuberculous abscess
- Far less common that tuberculoma
- May be solitary or multifocal (Arch Neurol 1978;35:148, Clin Microbiol Rev 2008;21:243)
- Manifestations similar to those seen with tuberculomas, albeit more rapidly progressive (Afr Health Sci 2011;11:116)
Diagnosis
- Diagnosis of CNS TB is dependent on a combination of clinical findings (see above), radiographic imaging studies and laboratory evaluation of cerebrospinal fluid (CSF) or CNS biopsies
- Evidence of tuberculous infection elsewhere (e.g., lung) provides a very important clue to the possibility of CNS TB in patients with neurological abnormalities
Laboratory
- Includes assessment of CSF protein and glucose levels, CSF cytology and identification of M. tuberculosis in CSF or tissue biopsies via acid fast stains, isolation of M. tuberculosis in culture and identification of bacterial nucleic acids and antigens and measurement of adenosine deaminase and tuberculostearic acid in CSF
- CSF profiles in TB meningitis typically include a lymphocytic pleocytosis, elevated protein levels and decreased glucose levels (Clin Microbiol Rev 2008;21:243, Curr Opin Neurol 1994;7:191, Clin Neuroradiol 2019;29:3)
- Protein levels may range from 0.5 to 3 g/L, while CSF glucose levels are usually < 45 mg/dL (or below 40 - 60% of serum glucose levels) (Clin Neuroradiol 2019;29:3)
- While a lymphocytic pleocytosis is most commonly seen, in a minority of patients, a neutrophilic pleocytosis may be present, either early in the course of the disease or shortly after initiation of antituberculous antibiotics (Clin Microbiol Rev 2008;21:243, Acta Cytol 1982;26:678)
- CSF profiles in parenchymal tuberculomas are nonspecific in the absence of concomitant leptomeningeal disease
- Cytological evaluation of CSF in suspected CNS TB cases is imperative, not only to characterize any inflammatory cells but to exclude leptomeningeal carcinomatosis, the latter being an important differential diagnostic consideration in suspected TB meningitis
- Morphological identification of M. tuberculosis in CSF or in smears or histological sections of tissue biopsies using the Ziehl-Neelson or Kinyoun acid fast stain (AFB) continues to play a key role in the diagnosis of CNS TB (Clin Microbiol Rev 2008;21:243)
- Centrifugation of large volumes (10 - 20 mL) of CSF with AFB staining of the resultant sediment has been shown to improve the sensitivity of detection of M. tuberculosis in CSF samples to 91% (J Clin Pathol 1953;6:241)
- Isolation of M. tuberculosis from cultures of CSF or tissues remains the gold standard in the diagnosis of CNS TB; isolation of M. tuberculosis in culture has the additional benefit of enabling laboratories to test for drug sensitivity, an important consideration with the emergence of drug resistant strains of the organism (Clin Microbiol Rev 2008;21:243)
- Because M. tuberculosis grows slowly in vitro, treatment decisions must usually be made before culture results are available (J Neurol Sci 2021;421:117278)
- Molecular diagnosis of CNS TB, specifically the detection of M. tuberculosis associated nucleic acids by a variety of nucleic acid amplification (NAA) tests has supplemented traditional staining and culture in the diagnosis of CNS TB and offers the special advantage of yielding positive results more rapidly than AFB staining or cultures (J Neurol Sci 2021;421:117278)
- Reported sensitivities of commercially available NAA assays range from 56 - 100%, with diagnostic specificities ranging from 96 - 100% (Clin Microbiol Rev 2008;21:243)
- NAA assays continue to evolve, with newer forms offering greater sensitivity and ease of use than earlier generation tests; although a positive NAA assay provides useful diagnostic information, as with any laboratory test, a negative assay does not exclude the possibility of TB
- Detection of M. tuberculosis associated antibodies and antigens in CSF is used in some laboratories, with reported sensitivities ranging from 52 - 94% and specificities ranging from 96 - 100% (Clin Microbiol Rev 2008;21:243)
- Measurement of adenosine deaminase and tuberculostearic acid in CSF have also been used in the evaluation of suspected CNS TB, albeit much less widely than traditional morphology, culture and NAA assays (Clin Microbiol Rev 2008;21:243)
Radiology description
- Imaging of the brain (computerized tomography [CT] and magnetic resonance imaging [MRI]) is extremely important in the evaluation of patients with suspected TB meningitis or tuberculoma(s)
- Radiographic imaging in cases of suspected CNS TB should include evaluation of the entire neuroaxis
- Contrast enhanced MRI is generally superior to CT in terms of both specificity and sensitivity in the diagnosis of CNS TB (Clin Neuroradiol 2019;29:3)
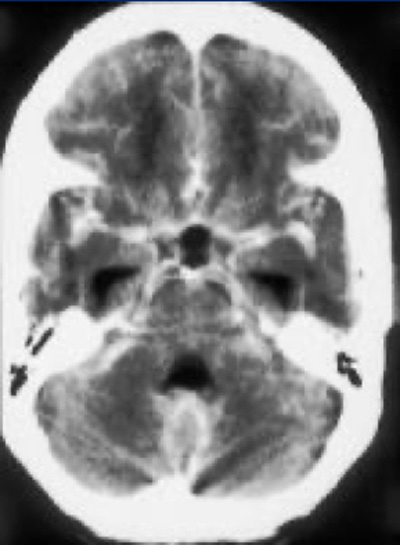
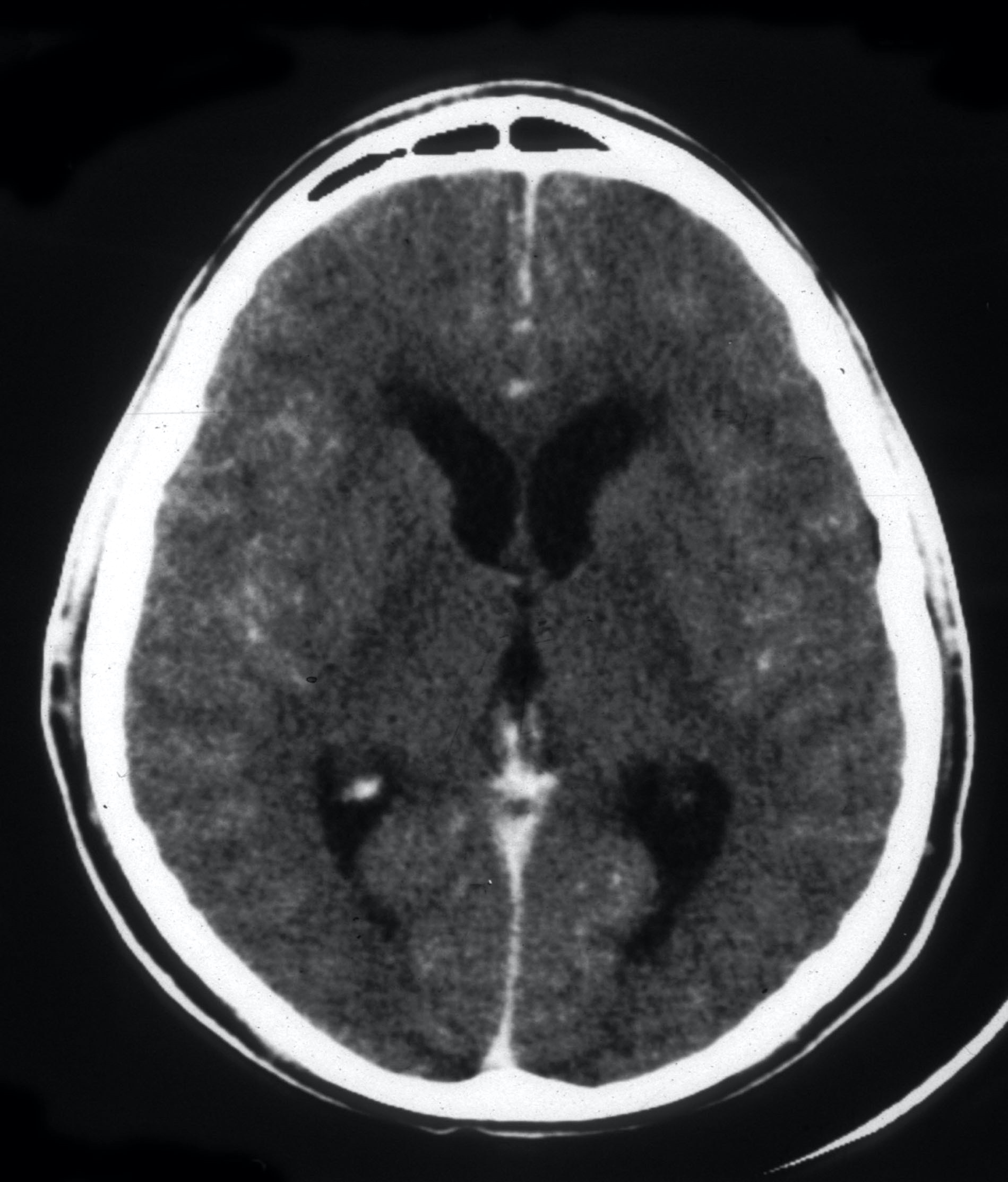
- Important radiographic features of TB meningitis area basal meningeal enhancement, hydrocephalus and cerebral infarcts (particularly in the basal ganglia, anterior thalamus and internal capsules) (Clin Neuroradiol 2019;29:3, Radiol Res Pract 2015;2015:202806)
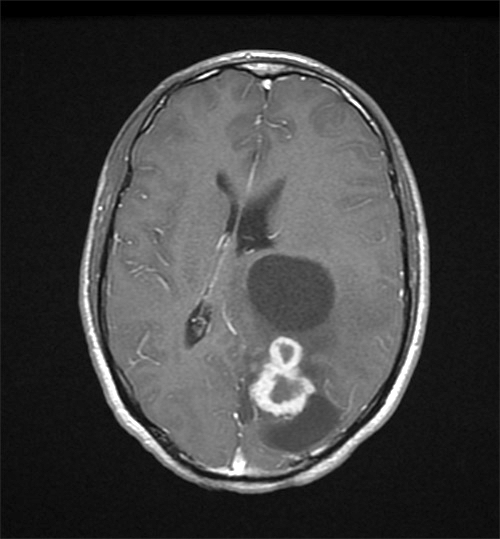
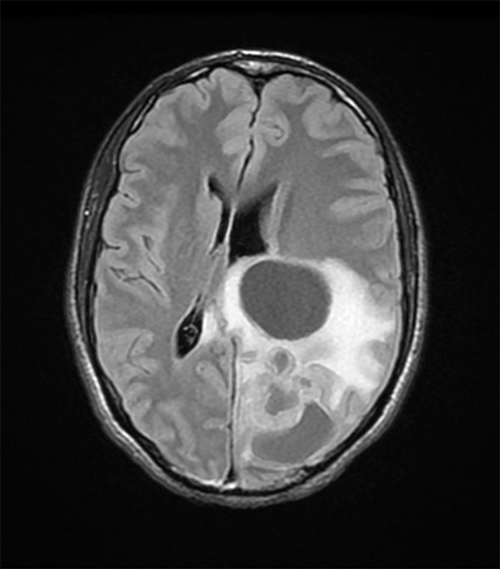
- Parenchymal tuberculomas may be solitary or multiple and may be associated with meningitis
- Radiographic appearance varies with the age of the lesion, the presence or absence of caseous necrosis (see histology below) and the presence or absence of calcification
- CT features of tuberculomas include areas of low density associated with peripheral ring enhancement and edema; calcification may be seen in older lesions, producing a characteristic target sign (Radiol Res Pract 2015;2015:202806)
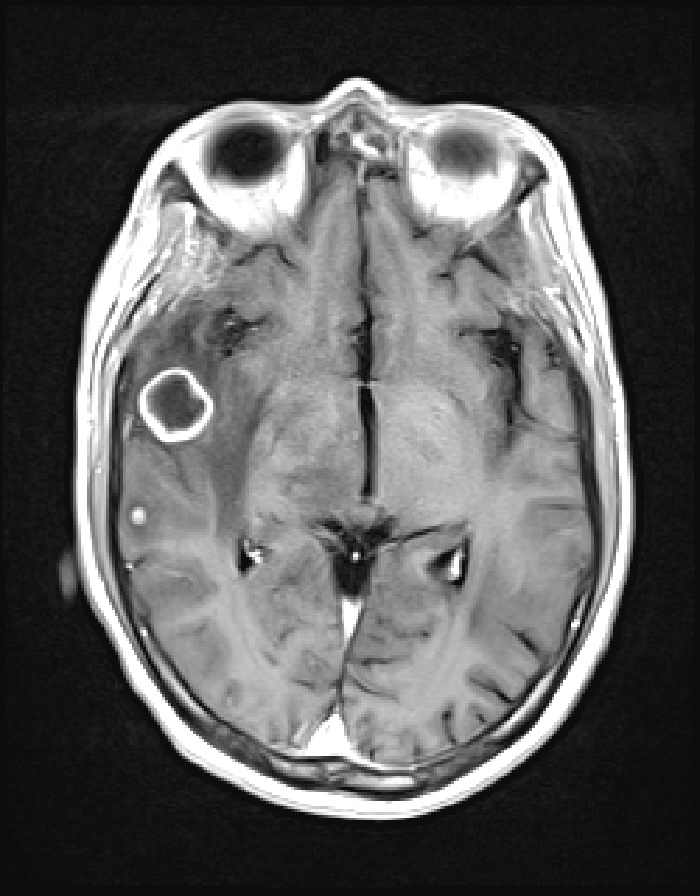
- MRI scans of caseating tuberculomas reveal areas of iso or hypointensity surrounded by a hyperintense rim in nonenhanced T1 weighted images; areas of peripheral ring enhancement are commonly seen after administration of gadolinium (Clin Imaging 2020;68:263)
- MRI scans of noncaseating tuberculomas reveal areas of hypointensity in noncontrast enhanced T1 weighted images, with a pattern of homogenous enhancement following the administration of gadolinium (Clin Neuroradiol 2019;29:3)
- These lesions appear iso or hyperintense in T2 weighted images (Clin Imaging 2020;68:263)
- Tuberculous abscesses may be solitary or multiple and have radiographic appearances quite similar to those seen in pyogenic bacterial abscesses, namely central hypo or isointensity associated with ring enhancement and regional edema
Radiology images
Prognostic factors
- In cases of TB meningitis, the clinical stage of disease at the time of presentation, as defined by the British Medical Research Council (MRC) criteria, is the single most important predictor of mortality and long term neurologic sequelae (Lancet 1948;1:582, Cochrane Database Syst Rev 2016;4:CD002244, Clin Microbiol Rev 2008;21:243)
- Mortality in patients with TB meningitis with MRC stage III disease (clouding of sensorium, focal neurological deficits, seizures, involuntary movements) ranges from 50 to 70%, while the outlook in patients with MRC stage I disease is considerably better, with a reported mortality of 18% (Am J Trop Med Hyg 1998;58:28, Clin Microbiol Rev 2008;21:243)
- Additional indictors of a poor prognosis in TB meningitis include (Postgrad Med J 1999;75:133):
- Extremes of age (i.e., infants and elderly patients)
- Malnutrition
- Chronic alcoholism
- Immunosuppression
- Hydrocephalus
- Markedly elevated CSF protein
- Very low CSF glucose levels
- In patients with tuberculoma, the presence of coma and evidence of miliary disease on chest Xray has been associated with a poor prognosis (J Pak Med Assoc 2004;54:83)
Case reports
- 2 year old previously healthy girl with a fatal case of TB meningitis (Pediatr Rep 2022;14:175)
- 19 year old woman with TB meningitis presented with progressive motor weakness in the absence of sensory abnormalities (Cureus 2017;9:e1222)
- 28 year old previously healthy woman with TB meningitis presented with intermittent fever, generalized limb weakness, dysphagia and visual hallucinations (Malays J Med Sci 2017;24:119)
- 38 year old woman who developed tuberculoma during the course of TB meningitis (Przegl Epidemiol 2013;67:23)
- 69 year old man with symptomatic tuberculoma (IDCases 2019;17:e00582)
Treatment
- Prompt treatment of CNS TB, particularly TB meningitis, is critical (J Neurol Sci 2021;421:117278)
- Most cases of CNS TB can be treated medically, although surgery may be indicated in certain patients (see below)
- Medical therapy includes (Clin Microbiol Rev 2008;21:243, J Neurol Sci 2021;421:117278)
- Intensive phase of 4 antituberculous antibiotics administered over a 2 month period
- Continuation phase of 2 antituberculous antibiotics administered over an additional 7 to 10 months
- Glucocorticoids
- Immune reconstitution inflammatory syndrome (IRIS) has been reported in ~33% of patients receiving antituberculous therapy and may be associated with significant clinical deterioration (J Neurol Sci 2021;421:117278)
- Emergence of multidrug resistant strains of M. tuberculosis may complicate medical treatment
- Neurosurgical intervention may be indicated in patients with hydrocephalus, in patients with tuberculomas with elevated intracranial pressure and in patients with spinal cord compression (Afr Health Sci 2011;11:116)
- Surgical treatment of tuberculomas has become much less common with the advent of effective medical therapy
Gross description
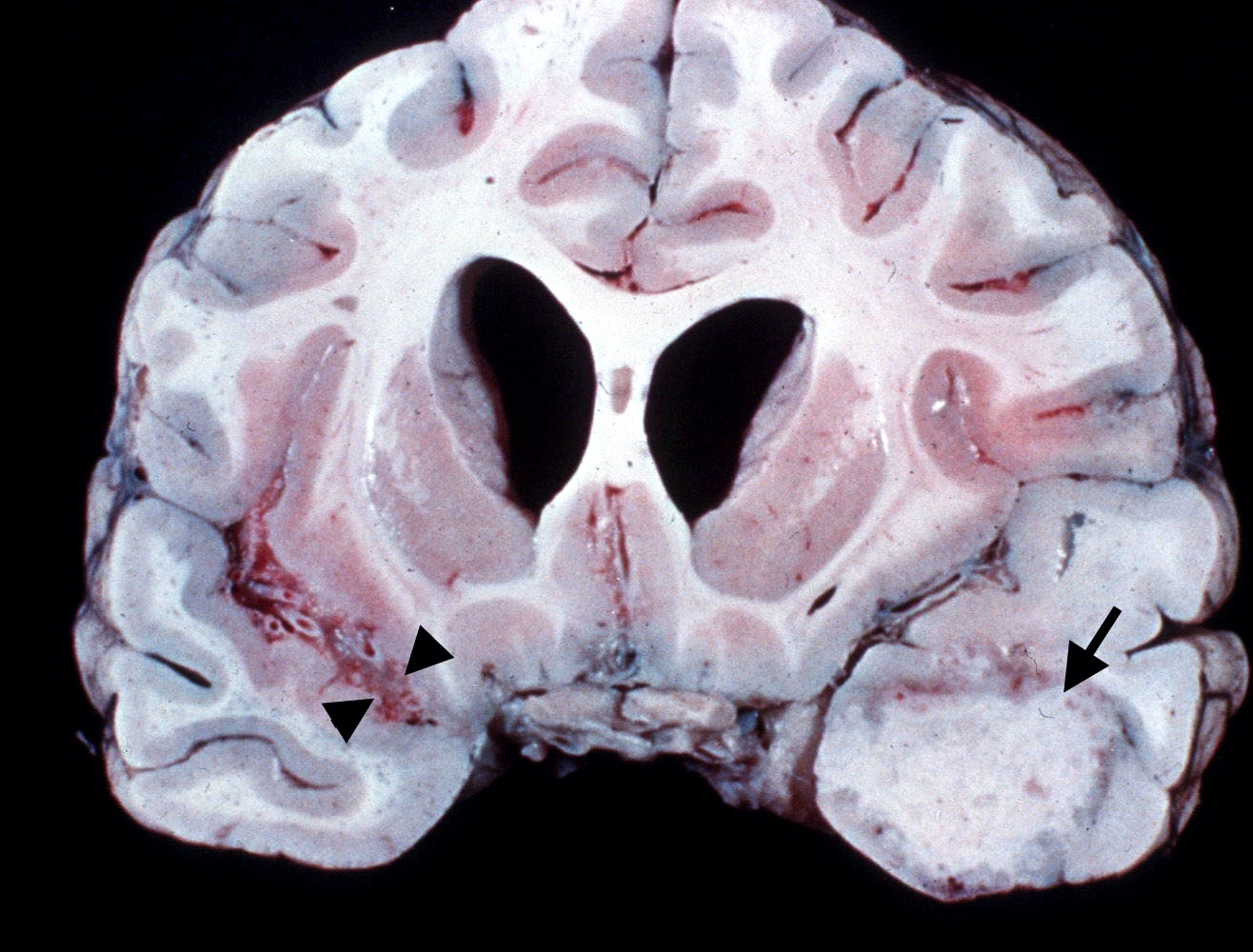
- Tuberculous meningitis is characterized by a dense leptomeningeal, grayish, occasionally gelatinous exudate that is typically most pronounced in the basal leptomeninges beneath the ventral diencephalon (Curr Opin Neurol 1994;7:191, Postgrad Med J 1999;75:133, Neurol India 1970;18:86)
- Exudate typically surrounds the optic chiasm and adjacent leptomeningeal vessels, including branches of the distal internal carotid, proximal middle cerebral and vertebrobasilar arteries
- Foci of necrosis are common in areas of the brain supplied by branches of the circle of Willis and the vertebrobasilar system (Curr Opin Neurol 1994;7:191, Postgrad Med J 1999;75:133)
- Hydrocephalus, usually of the communicating type, is often present, owing to obstruction of the flow of CSF in the basal cisterns (Curr Opin Neurol 1994;7:191, Clin Neuroradiol 2019;29:3)
- Tuberculomas are space occupying, well circumscribed, encapsulated lesions that range in diameter from a few millimeters to several centimeters (Postgrad Med J 1999;75:133, Clin Neuroradiol 2019;29:3, Clin Microbiol Rev 2008;21:243)
- In adults, they are most commonly seen near gray-white junctions in the supratentorial compartment, while infratentorial tuberculomas are more common in pediatric patients (Radiol Clin North Am 1995;33:753, Clin Imaging 2020;68:263)
- Centers of larger tuberculomas contain friable, gray areas of caseous (cheese-like) necrosis
- Tuberculomas may extend through the cortex into the leptomeninges to produce tuberculous leptomeningitis; rupture into the ventricular system may also occur, resulting in life threatening ventriculitis (Int J Mycobacteriol 2016;5:231)
- Localized tuberculomas can also occur in the leptomeninges, dura mater and epidural space
Gross images
Frozen section description
- Frozen sections on suspected tuberculomas should be performed with careful attention to barrier protection and minimalization of aerosols, owing to the risk of contamination of cryostats and other equipment in the pathology laboratory and the risk of exposing laboratory workers to M. tuberculosis
- In particular, the use of pressurized coolants should be scrupulously avoided in the preparation of frozen sections in cases of suspected tuberculoma
- Frozen sections of tuberculomas have been reported to demonstrate areas of necrosis, epithelioid macrophages and giant cells (NMC Case Rep J 2014;1:33)
- Specimens of tuberculomas submitted for frozen section are often quite small and may lack specific diagnostic features
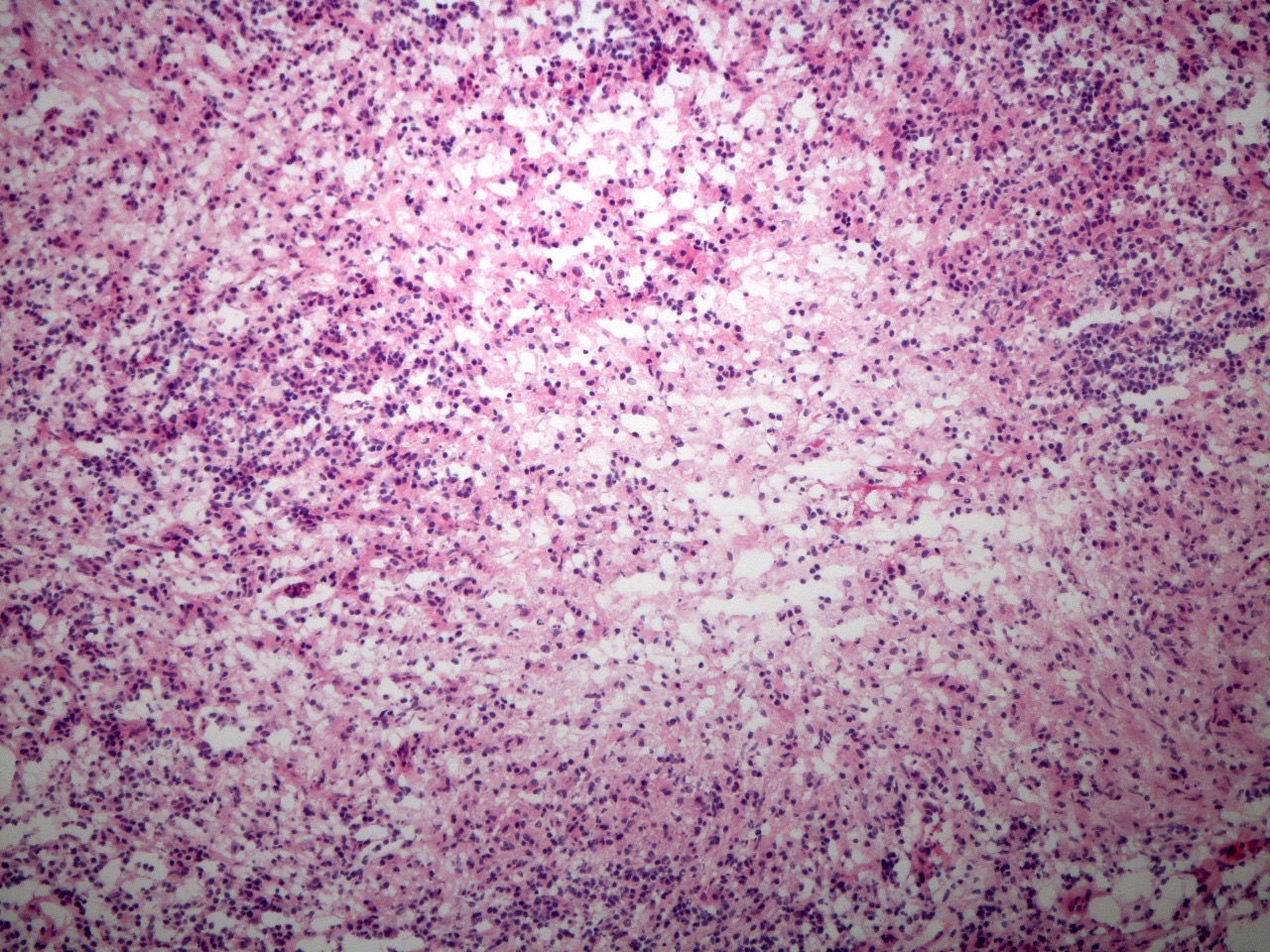
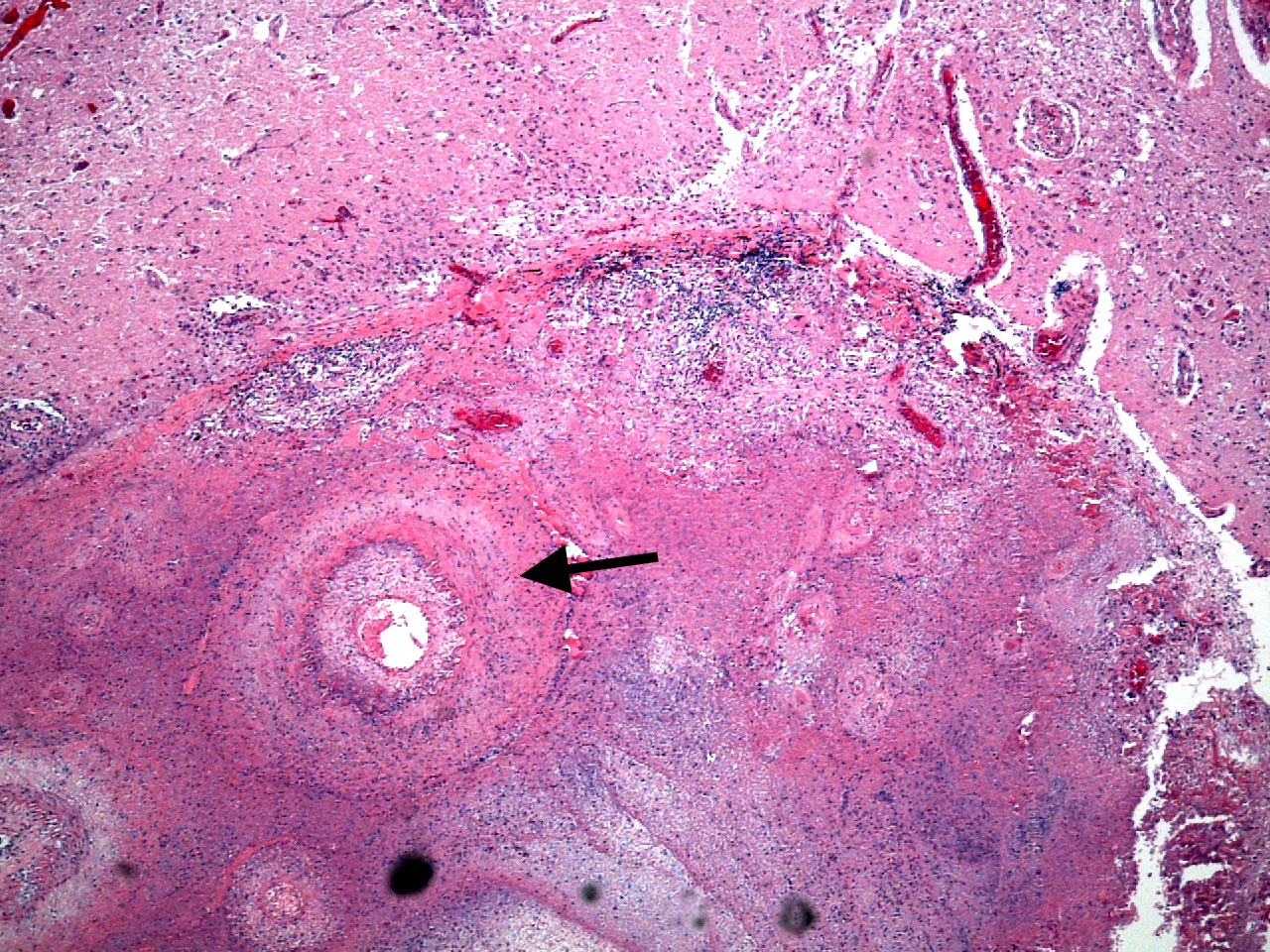
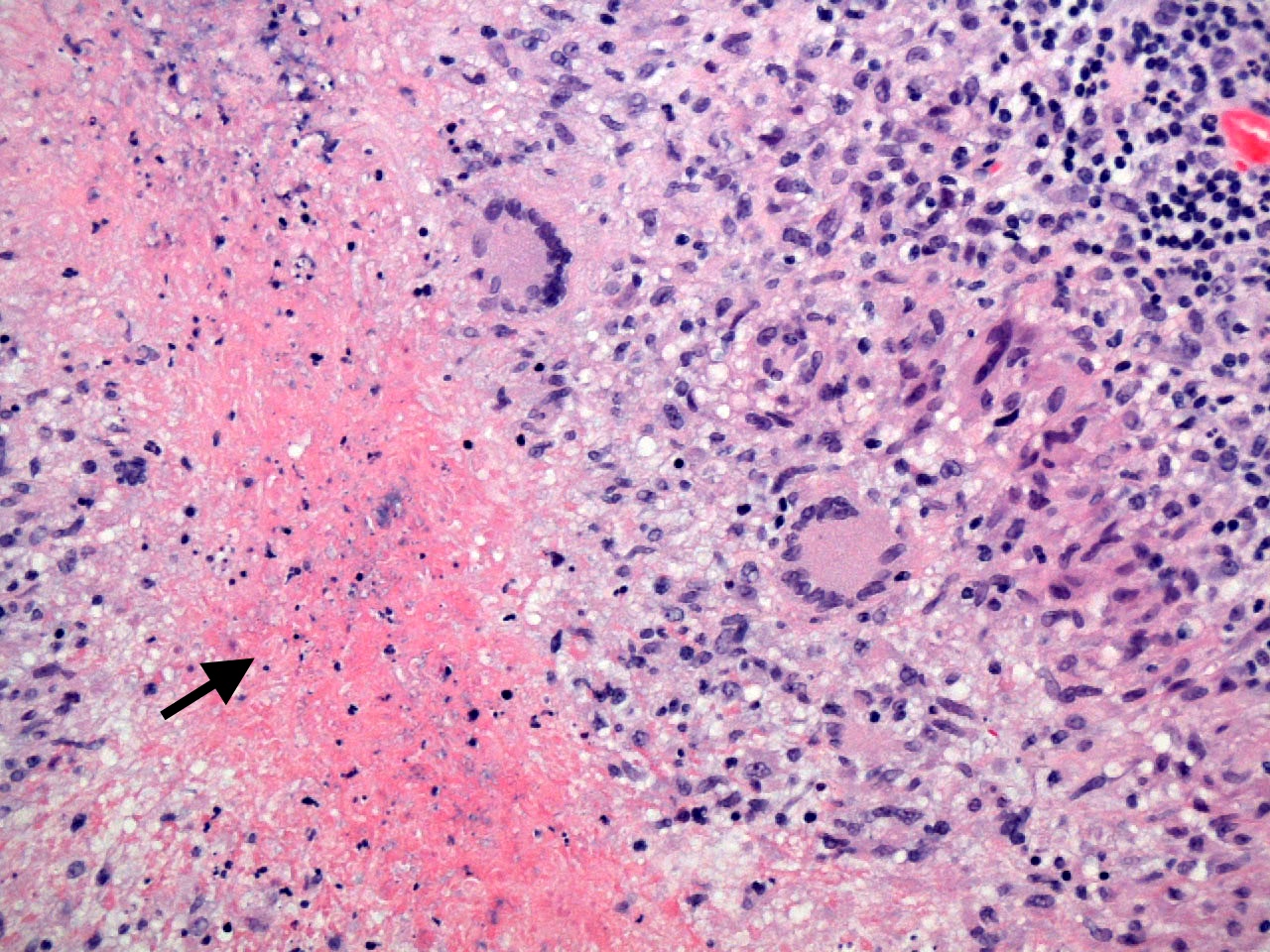
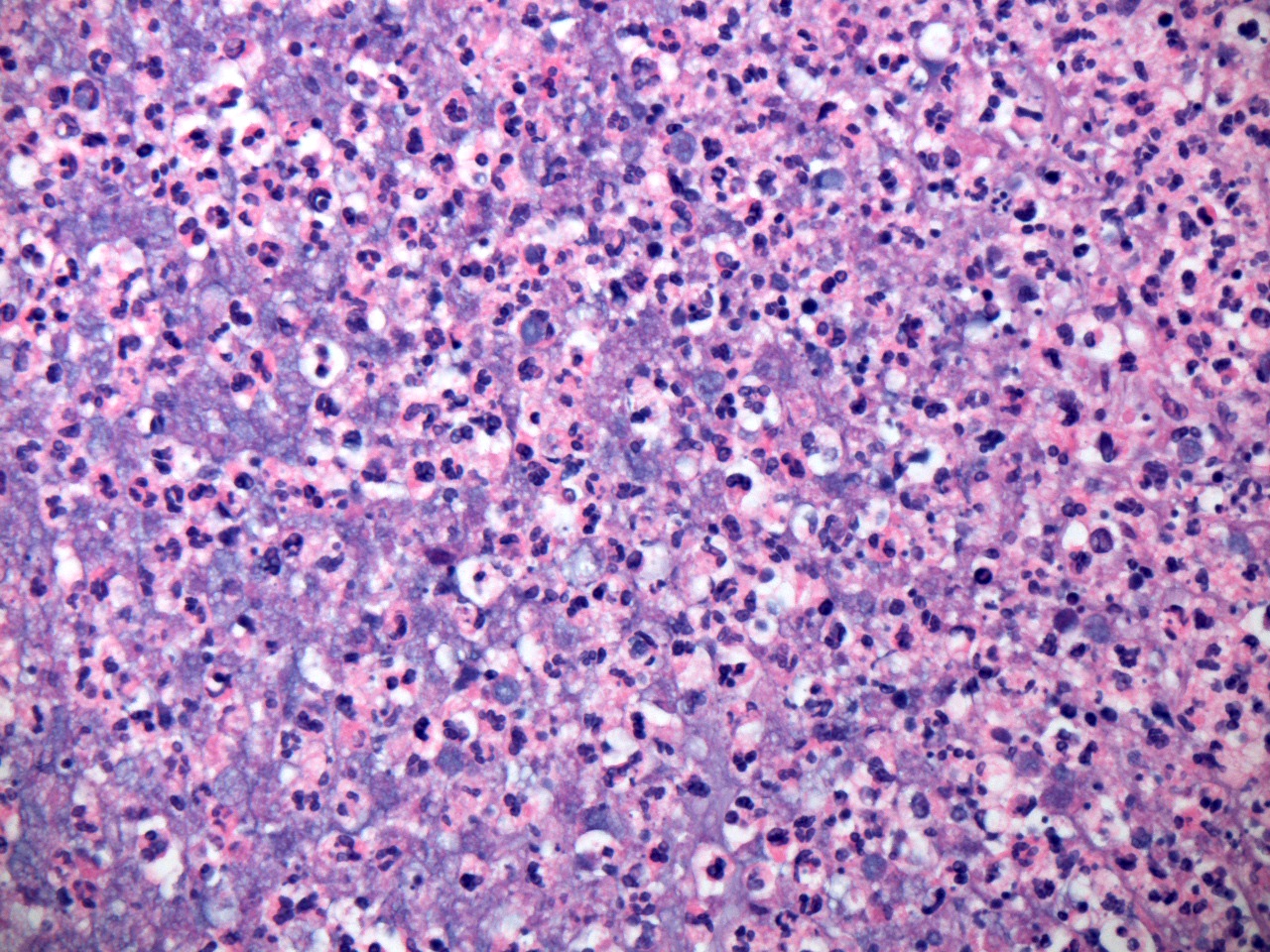
Microscopic (histologic) description
- Histological hallmark of M. tuberculosis infection is granulomatous inflammation, characterized by the presence of epithelioid macrophages and multinucleated giant cells that accumulate in response to the poorly digestible, waxy, mycolipid rich wall of the organism
- Areas of caseous necrosis typically develop in areas of granulomatous inflammation over time, reflecting the development of cell mediated immunity and delayed hypersensitivity to M. tuberculosis associated antigens (Antimicrob Agents Chemother 2003;47:833)
- Inflammatory reaction in the subarachnoid space in cases of TB meningitis is associated with the development of proliferative changes in the intima of regional vessels, particularly in penetrating arteries originating from the distal internal carotid arteries, middle cerebral arteries and other components of the circle of Willis (Clin Neuroradiol 2019;29:3)
- Progressive intimal arterial proliferation leads to ischemic damage in the territories supplied by the affected vessels
Microscopic (histologic) images
Cytology description
- Cytological studies in cases of CNS TB are most commonly undertaken in the evaluation of CSF samples
- In such cases, the standard cytological profile is that of a pleocytosis with a predominance of lymphocytes, although neutrophils may be seen in the earlier stage of disease (Acta Cytol 1982;26:678, Clin Microbiol Rev 2008;21:243, Clin Neuroradiol 2019;29:3, Acta Cytol 1982;26:678)
- As noted previously (see Laboratory above), cytological evaluation of CSF for the presence of malignant cells should always be undertaken to exclude the possibility of leptomeningeal carcinomatosis, an important differential diagnostic consideration in suspected TB meningitis
- As in the case of frozen sections, the preparation of smears from fresh, potentially infectious tissue obtained intraoperatively in suspected CNS TB cases is discouraged and if undertaken, should always be done with the same precautions used in preparing frozen sections
- Although little has been published about the cytological features of tuberculomas, reports of fine needle aspirations of tuberculomas in other sites have noted the presence of granulomas with epithelioid macrophages (Acta Cytol 1999;43:191)
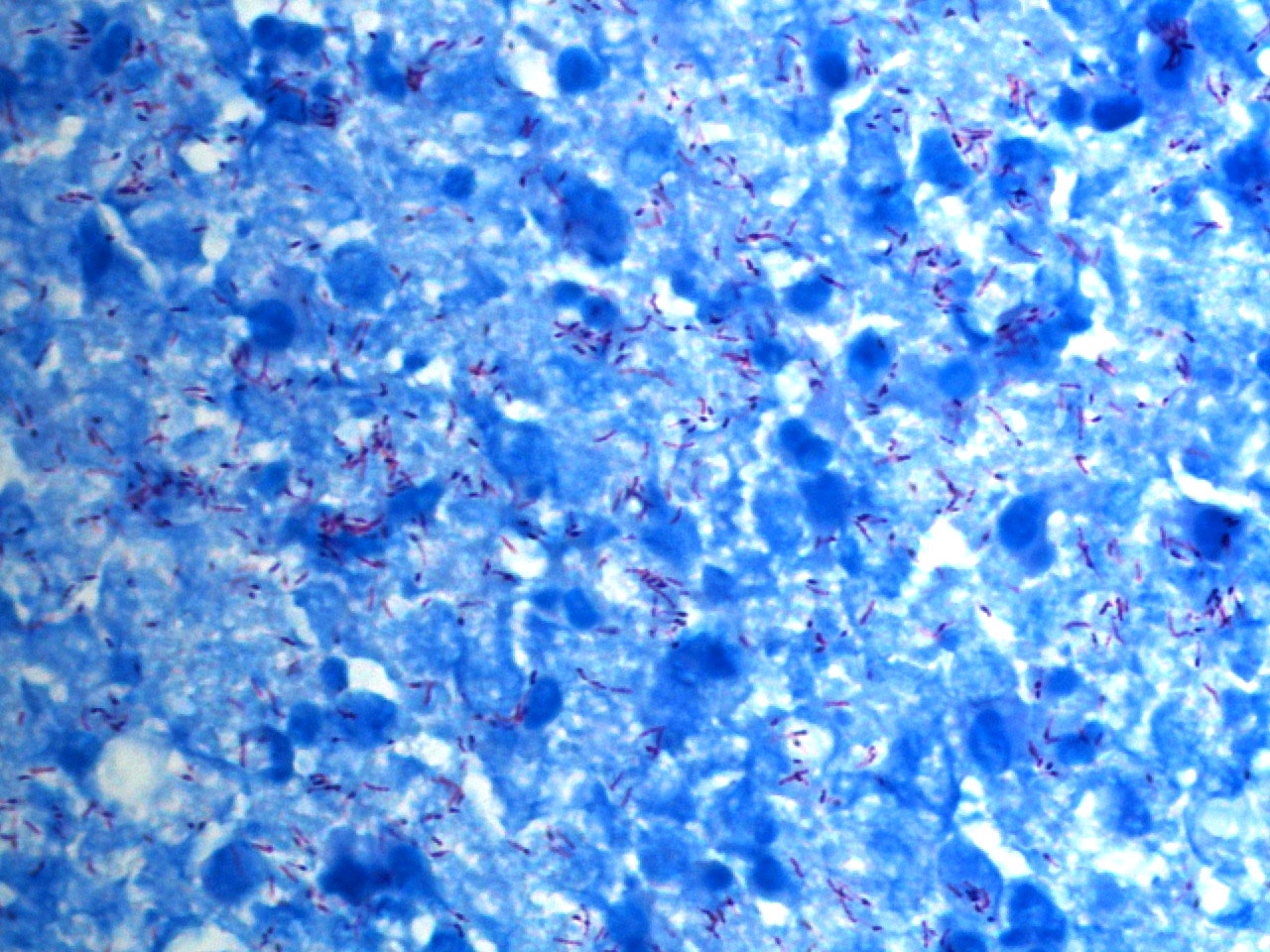
Positive stains
- Acid fast stains, notably variations of the Ziehl-Neelsen and Kinyoun stains, are the stains of choice for demonstrating M. tuberculosis (Clin Microbiol Rev 2008;21:243)
- Fluorescent stains, including auramine-rhodamine, will also highlight acid fast bacilli (J Ayub Med Coll Abbottabad 2018;30:159, Henry Ford Hosp Med Bull 1962;10:287)
- Although fairly sensitive and therefore useful for screening, auramine based stains are less specific for mycobacteria than are acid fast stains; positive specimens should always be evaluated with acid fast stains and wherever possible, confirmed by culture (Mikrobiyol Bul 2003;37:131)
Sample pathology report
- Brain, left parietal lobe, resection:
- Necrotizing granulomatous inflammation with acid fast bacilli, compatible with tuberculoma
- Brain, autopsy:
- Granulomatous leptomeningitis with caseous necrosis, proliferative vasculopathy and acid fast bacilli, compatible with tuberculous meningitis
Differential diagnosis
- A large number of infectious and noninfectious entities may mimic TB meningitis and intraparenchymal tuberculomas (Clin Neuroradiol 2019;29:3)
- Differential diagnoses in suspected TB meningitis include
- Bacterial (pyogenic) meningitis:
- CSF characterized by neutrophilic pleocytosis
- Fungal meningitis:
- CSF profile may be similar to that seen in TB meningitis
- Diagnosis dependent upon identification of specific pathogen
- Nontuberculous mycobacterial meningitis:
- Generally associated with immunosuppression, CD4 counts of < 50 cells/μl
- Neurobrucellosis:
- Identification of anti-Brucella antibodies in CSF is both sensitive and specific
- Neurosarcoidosis:
- May be associated with cranial nerve VII dysfunction, pituitary involvement
- Documentation of elevated ACE or IL2 receptor levels may be of diagnostic value
- Neurosyphillis:
- Identification of antitreponemal antibodies or treponemal DNA in CSF is of diagnostic value
- Viral meningitis / meningoencephalitis:
- Mononuclear pleocytosis, normal glucose
- Definitive diagnosis based on identification of specific antiviral antibodies on viral nucleic acid in CSF
- Leptomeningeal carcinomatosis:
- Malignant cells detected in CSF
- CSF profile may include elevated protein and very low glucose levels
- Bacterial (pyogenic) meningitis:
- Differential diagnoses in suspected tuberculoma(s) and tuberculous abscess include
- Bacterial (pyogenic) abscess:
- Predominance of neutrophils, identification of bacteria in Gram stains or by culture
- Localized fungal disease:
- Usually associated with granulomatous or lymphocytic inflammatory response, although neutrophils may be present in some (e.g., coccidioidomycosis)
- Organisms highlighted with appropriate silver stains (e.g., Gomori methenamine silver)
- Cerebral toxoplasmosis:
- Identification of organism in biopsies or detection of T. gondii DNA via PCR is necessary for definitive diagnosis
- Serological studies are of less value, particularly in immunosuppressed patients
- Neurocysticercosis:
- Identification of organism in biopsies
- Malignant neoplasms (glioma, metastatic carcinoma, CNS lymphoma):
- Identification of neoplastic cells in biopsies
- Bacterial (pyogenic) abscess:
Board review style question #1
A 53 year old man presents for evaluation of intermittent fever and a persistent headache. Neurological examination reveals evidence of decreased visual acuity and bilateral lateral gaze paralysis. An MRI scan reveals communicating hydrocephalus and evidence of meningeal enhancement, most pronounced in the basilar leptomeninges. Which one of the following is the most likely diagnosis in this patient?
- Acute bacterial meningitis
- Cryptococcal meningitis
- Leptomeningeal carcinomatosis
- Tuberculous meningitis
- Viral meningoencephalitis
Board review style answer #1
D. Tuberculous meningitis.
The combination of a cranial nerve VI (abducens) palsy, optic pathway damage, basilar leptomeningeal enhancement and communicating hydrocephalus is highly suggestive of tuberculous meningitis. Identification of M. tuberculosis via microscopy or culture, identification of M. tuberculosis associated nucleic acid via nucleic acid amplification techniques or identification of M. tuberculosis associated antigens in cerebrospinal fluid is necessary for a definitive diagnosis.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis
Board review style question #2
Which one of the following proteins plays the most important role in the ingestion of M. tuberculosis by CNS microglial cells?
- CD4
- CD14
- CD68
- IL1
- IL10
Board review style answer #2
B. CD14.
The CD14 receptor has been identified as a critical surface receptor that facilitates ingestion of M. tuberculosis by microglia. Answers A and C are incorrect because while CD68 immunoreactivity is typically seen in CNS granulomas in a variety of different conditions, including TB, neither the CD68 nor the CD4 receptor have been shown to play a specific role in the binding to or ingestion of M. tuberculosis by microglia. Answers D and E are incorrect because IL1 and IL10 production are decreased in M. tuberculosis infected microglia.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis
Board review style question #3
Which one of the following has been associated with a poor prognosis in patients with TB meningitis?
- British MRC stage I disease
- High CSF glucose levels
- Hydrocephalus
- Low CSF protein levels
- Middle age
Board review style answer #3
C. Hydrocephalus. Of the factors listed, only the presence of hydrocephalus has been associated with a poor prognosis in TB meningitis. The remaining answers are incorrect because other conditions associated with a poor prognosis include disease in either the very young or the very elderly, a very low CSF glucose, a very high CSF protein and severe clinical disease (MRC stage III disease). Malnutrition, immunosuppression and chronic alcoholism have also been associated with a poor prognosis.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis
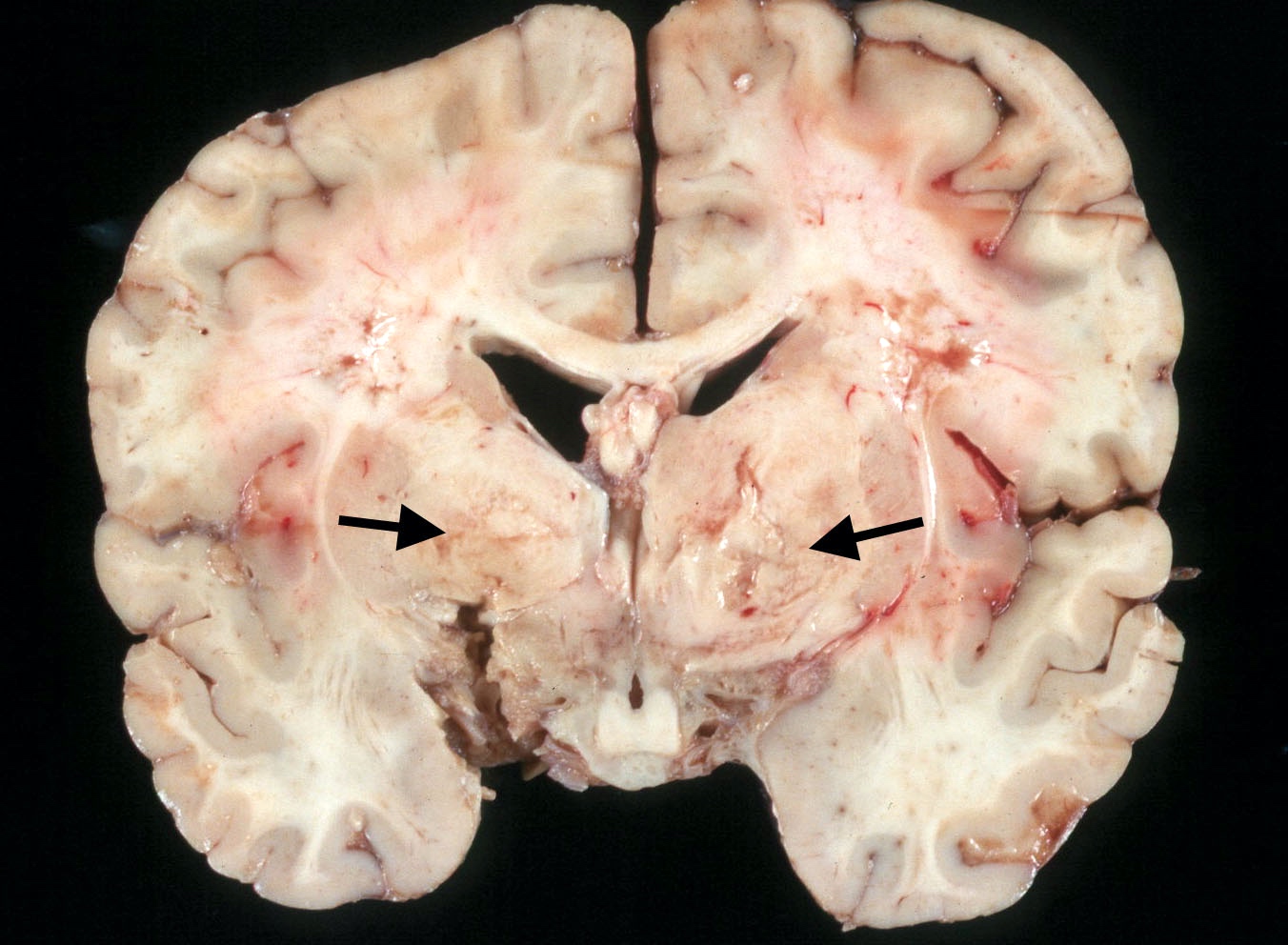
Board review style question #4
A 5 year old child was found unresponsive at home. A family member stated that the child had had intermittent fevers and irritability prior to becoming unresponsive. An elderly uncle who lived with the family had also been ill, with a history of fever, coughing and weight loss. Emergency medical personnel were unable to detect a pulse and began cardiopulmonary resuscitation. The child was taken to a nearby emergency, where advanced life support measures were unsuccessful. The case was referred to the medical examiner's office, where an autopsy was performed. A coronal section of the patient's brain is shown in the image above. What is the most likely cause of the lesions in the basal ganglia indicated by the arrows?
- Contiguous spread of leptomeningeal infection
- Embolic occlusion of vessels in the circle of Willis
- Hematogenous dissemination of microorganisms
- Obstruction of the flow of cerebrospinal fluid
- Vasculitis of lenticulostriate arteries
Board review style answer #4
E. Vasculitis of lenticulostriate arteries. The lesions in the basal ganglia are recent infarcts caused by injury to penetrating lenticulostriate arteries originating in the region of the circle of Willis. The tuberculous exudate, particularly conspicuous at the base of the brain in this patient, is characteristically associated with inflammation (vasculitis) and proliferative changes in regional vessels, with resultant compromise of arterial lumens and infarcts in territories supplied by these vessels.
Comment Here
Reference: Tuberculosis
Comment Here
Reference: Tuberculosis