Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognosis and treatment | Case reports | Gross images | Microscopic (histologic) images | Positive stains | Electron microscopy images | Differential diagnosisCite this page: Cohen M. Progressive multifocal leukoencephalopathy (PML) and other JC virus infections. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnspml.html. Accessed March 31st, 2025.
Definition / general
- Until recently, central nervous system infections with JC virus presented as a progressive, multifocal, demyelinating / degenerative white matter process within patients with chronic lymphoproliferative disorders
- Even today, progressive multifocal leukoencephalopathy and JC virus infection are often thought as being one and the same process
- However, in recent years, major changes in the understanding of these infections include:
- White matter disease may be nonprogressive, unifocal and inflammatory
- Neuronal infection is seen commonly in patients with white matter disease and may also be seen in isolation
- Reversal of the underlying predisposing immunosuppressed state (which is still the only effective therapy) may be accompanied by paradoxical worsening of the central nervous system disease, referred to as PML-IRIS (immune reconstitution inflammatory syndrome)
Terminology
- Progressive multifocal leukoencephalopathy (PML), JC virus granule cell neuronopathy (JCV GCN), JC virus encephalopathy (JCVE), progressive multifocal leukoencephalopathy - immune reconstitution inflammatory syndrome (PML-IRIS), JC virus granule cell neuronopathy - immune reconstitution inflammatory syndrome (GCN-IRIS)
Epidemiology
- Initially described as a rare complication of B cell lymphoproliferative disorders, JC virus infections affect ~5% of AIDS patients (although infections in patients treated with combined antiretroviral therapy are milder than those seen prior to implementation of these regimens)
- Patients with autoimmune diseases receiving monoclonal antibody therapies, especially patients with multiple sclerosis being treated with natalizumab (~400 patients reported to date, MAbs 2009;1:583)
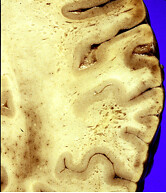
Sites
- Progressive multifocal leukoencephalopathy may affect the white matter anywhere within the central nervous system and has a distinct predilection for the cortical / subcortical interface
- JC virus granule cell neuronopathy selectively infects the granule cells of the cerebellum, while JC virus encephalopathy selectively infects cerebrocortical neurons
Pathophysiology
- Once the JC virus is reactivated (see below), it gains access to the central nervous system, where it lytically infects oligodendroglial cells, nonlytically infects astrocytes and may infect neurons either in combination with glial cells or by themselves (Discov Med 2011;12:495, PLoS Pathog 2012;8:e1003014)
Etiology
- Although primary infections with JC virus may lead to development of central nervous system disease, most cases are felt to be secondary to reactivation of dormant virus residing within the kidney, bone marrow or brain
- ~50% of population is serologically positive for JC virus, which is usually acquired asymptomatically in childhood
- Although often thought of as a disease of profoundly immunosuppressed individuals, JC virus central nervous system infection may occur in patients with minimal or even occult immunosuppression
- Some investigators believe that the fundamental reactivating process is B cell dysregulation, which is in turn usually but not always a result of loss of T cell surveillance
Clinical features
- Due to the wide range of nervous system structures which may be involved, the clinical manifestations may be protean (resembling Proteus in having a varied nature)
- However, PML is characterized by behavioral and cognitive abnormalities along with gait abnormalities, motor weakness, visual field deficits, speech and language deficits and incoordination
- JC virus granule cell neuronopathy presents with cerebellar dysfunction, including ataxia and dysmetria
- JC virus encephalopathy presents with global cerebrocortical dysfunction accompanied by seizures (Cleve Clin J Med 2011;78:S8)
Diagnosis
- Diagnosis of progressive multifocal leukoencephalopathy is made using a combination of clinical features, imaging findings and either CSF PCR for JC virus or demonstration of viral infection on brain biopsy
- Newer ultrasensitive techniques for CSF PCR have demonstrated greater than 95% sensitivity although this may be lower in patients with more modest immunosuppression
- In such cases, a brain biopsy may be needed to establish a definitive diagnosis although many cases may be treated as probable PML using only clinical and imaging features (Neurology 2013;80:1430)
Laboratory
- Most HIV+ patients with PML have CD4 lymphocyte counts less than 200 cells per cubic millimeter but ~10% have CD4 counts greater than 200/mm3
- CSF all counts are usually less than 20 per cubic millimeter
- CSF PCR for JC virus is the most useful laboratory diagnostic test but is not 100% sensitive (see above, J Clin Virol 2008;43:247, J Med Microbiol 2009;58:253)
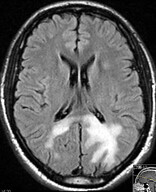
Radiology description
- CT scans show hypointense lesions within the affected white matter of patients with PML
- MRI demonstrates hyperintense lesions on T2 and FLAIR weighted images
- Faint, typically peripheral located contrast enhancement may be seen in ~5% of cases although this increases to 15% in patients with HIV associated PML and 40%% in patients with natalizumab associated PML
- Latter is often monofocal, with frontal lobe lesions predominating
- PML-IRIS, regardless of the initial predisposing condition, is characterized by prominent enhancement secondary to the reconstituted inflammatory response (Neurology 2012;79:1041)
Radiology images
Prognosis and treatment
- No specific effective therapy for JC virus - survival depends entirely on the ability to reverse the immunosuppressed state
- Overall, 1/3 of patients die, 1/3 have severe neurological deficits, 1/3 recover with minimal to moderate neurological deficits (Neurology 2009;73:1551, J Virol 2011;85:7256)
- Paradoxical worsening of symptoms (referred to as the immune reconstitution inflammatory syndrome) appears to be controllable (paradoxically) with corticosteroid therapy (high dose, short term)
Case reports
- 49 year old woman with multiple sclerosis (MS) and lesion suspicious of progressive multifocal leukoencephalopathy (PML) (Neurology 2011;77:2010)
- 61 year old man with treated follicular lymphoma and cerebellar mass (Case of the Week #265)
- 74 year old man with psoriasis who developed PML after fumaric acid treatment (N Engl J Med 2013;368:1657)
PML-IRIS:
- 23 year old man with simultaneous PML-IRIS after discontinuation of natalizumab (Neurology 2012;78:1390)
- 38 year old woman with PML-IRIS and treated with brentuximab (Neurology 2012;79:2075)
- 49 year old woman with maraviroc and JC virus associated immune reconstitution inflammatory syndrome (N Engl J Med 2014;370:486)
PML, possibly in combination with JC virus granule cell neuronopathy:
- 83 year old woman with progressive hemiataxia, tremor and infratentorial lesions (Neurology 2011;77:e7)
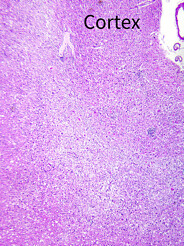
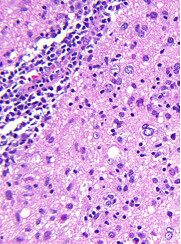
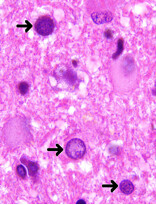
Microscopic (histologic) images
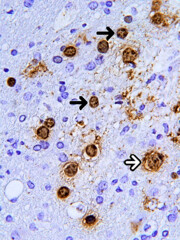
Positive stains
- In situ hybridization demonstrating JC viral DNA indicates viral infection
- All commercially available antibodies raised against SV40 antigen cross react with JC virus and confirm the active stage of the virus cycle
- Some antibodies are not sensitive enough to be used on paraffin embedded formalin fixed sections so care must be used in the evaluation of these preparations
Differential diagnosis
- On biopsy, principal differential diagnostic considerations include noninfectious demyelination and theoretically glioma (as a result of misinterpretation of enlarged atypical viral nuclei)
- Attention to the preserved nuclear to cytoplasmic ratio should prevent the latter, while careful scrutiny for viral inclusions should prevent the former