Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Afzal S, Zaman S, Minhas MK. Primary amebic meningoencephalitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnspam.html. Accessed March 31st, 2025.
Definition / general
- Primary amebic meningoencephalitis (PAM) is a rare, waterborne central nervous system (CNS) infection caused by the free living amoeba Naegleria fowleri
Essential features
- Waterborne CNS infection caused by N. fowleri, with rapid onset and a high mortality rate
- Characteristic organism has a single nucleus, vacuolated cytoplasm and is highlighted by Wright-Giemsa stain on cerebrospinal fluid (CSF) smears or on histology H&E stained slides
Terminology
- Naegleriasis
ICD coding
- ICD-10: B60.2 - naegleriasis
Epidemiology
- PAM is a very rare disease, with 3.7 cases/year reported worldwide (range: 0 - 16/year)
- Occurs more commonly in warmer regions and in the warmer months of spring and summer
- Mostly affects younger male children, with a median age of 12 years
- References: StatPearls: Amebic Meningoencephalitis [Accessed 14 September 2023], J Assoc Physicians India 2015;63:69, Clin Infect Dis 2021;73:e19
Sites
- Naegleria penetrates the olfactory mucosa and migrates into the central nervous system through the cribriform plate
- In the brain, the organism multiplies and causes hemorrhagic necrosis of brain parenchyma and secondary involvement of the meninges (Microbiology (Reading) 2012;158:791)
Pathophysiology
- N. fowleri occurs in 3 forms
- Inactive cyst form: 7 - 12 μm spherical, incredibly resistant structure that can survive in low temperatures of winter
- Transitory flagellate form: 10 - 16 μm pear shaped with 2 flagella, thrives at 27 - 37 °C; this is not the reproductively active or pathogenic form
- Trophozoite form: ~22 μm long and 7 µm wide, long, slender, reproductively active form that can cause infection; trophozoites grow at 35 - 46 °C
- Trophozoites are in the infective stage, which invades the central nervous system after nasal inoculation with amoebas, disrupting the olfactory mucosa
- 2 primary mechanisms are noted for brain damage
- Contact independent
- N. fowleri causes the devastation of the host cell and nervous system indirectly by secreting several proteins, including phospholipases, cysteine proteases, neuraminidases, phospholipolytic enzymes and acid hydrolases
- N. fowleri also induces formation of reactive oxygen species in its host, leading to host cell injury
- Contact dependent
- N. fowleri has a surface sucker-like structure called a food cup, which enables them to digest brain tissue; the formation of these food cups is carried out by Nfa1 and Nf actin, which mediate the phagocytic activity of N. fowleri
- References: StatPearls: Naegleria [Accessed 14 September 2023], Biomolecules 2021;11:1320, Antimicrob Agents Chemother 2015;59:6677, Clin Exp Pharmacol Physiol 2020;47:199
- Contact independent
Etiology
- PAM is caused by N. fowleri, which is a waterborne, free living amoeba that survives in temperatures between 30 °C and 45 °C (StatPearls: Amebic Meningoencephalitis [Accessed 14 September 2023])
- Mostly affects children and young adults with freshwater exposure (J Assoc Physicians India 2015;63:69)
- Recreational freshwater or unchlorinated water used for swimming and usage of infected water for nasal irrigation are also risk factors (Lancet Infect Dis 2020;20:27)
- Disease is rapidly progressive with high mortality rate (Biomolecules 2021;11:1320)
Clinical features
- Disease usually develops within 1 - 7 days after exposure (J Assoc Physicians India 2015;63:69)
- Clinical symptoms can be divided into early and late (J Pediatric Infect Dis Soc 2015;4:e68)
- Early: flu-like symptoms only
- Headache, nausea, vomiting, fever, fatigue and earache
- Late: CNS involvement
- Lethargy, nuchal rigidity, anorexia, irritation, confusion, photophobia, seizures, cranial nerve abnormalities, blurred vision and coma
- Early: flu-like symptoms only
Diagnosis
- Case definition as per Centers for Disease Control and Prevention (CDC) requirements
- Organism in CSF, biopsy, tissue specimen
- Nucleic acid in CSF or biopsy
- Antigen in CSF or biopsy
- References: J Assoc Physicians India 2015;63:69, Clin Infect Dis 2021;73:e19
Laboratory
- Can be diagnosed using microscopic methods, CSF culture, amoebic antigen detection and direct detection of parasite DNA by RT PCR
- CBC shows leukocytosis, predominantly neutrophils
- Increased opening pressure for CSF with increased red blood cell count
- Leukocytosis in CSF (neutrophil predominant); increased proteins and decreased glucose in CSF
- CSF reveals many neutrophils along with pseudopod forming, actively motile N. fowleri amoeba trophozoites, highlighted by Wright-Giemsa or trichrome special stains
- N. fowleri can be cultivated in nonnutrient / low nutrient agar plate or in a Nelson growth medium
- RT PCR can help determine exact genus and species (ITS1 oligonucleotide sequence of Naegleria spp.) (J Water Health 2023;21:972)
- References: Biomolecules 2021;11:1320, J Water Health 2023;21:972, J Pediatric Infect Dis Soc 2015;4:e68, Am J Trop Med Hyg 2017;97:1600
Radiology description
- Nonspecific changes on CT scan, with brain edema being most common
- Hydrocephalus and obliteration of basal cisterns is also seen on CT scan
- MRI of the brain shows the presence of single or multiple space occupying lesions with ring enhancement
- References: AJR Am J Roentgenol 1998;171:809, StatPearls: Amebic Meningoencephalitis [Accessed 14 September 2023], BMC Infect Dis 2021;21:1251
Case reports
- 13 year old boy presented with headache and fever (IDCases 2021;25:e01208)
- 25 year old woman presented with headache, lethargy and coma (Pathol Int 1999;49:468)
- 44 year old man presented with fever as well as worsening headache and generalized weakness (Case Rep Infect Dis 2020;2020:4925819)
- 73 year old man presented with fever, neck pain, seizures and altered sensorium (Indian J Crit Care Med 2012;16:34)
Treatment
- As the disease is rare and rapidly fatal, there are no clinical trials to determine optimal treatment regimens
- Generally, amphotericin B is recommended both intravenously and intrathecally
- Considering high disease mortality, a combination of drugs is usually used
- Amphotericin in combination with fluconazole, azithromycin, miltefosine and posaconazole has been noted to be effective
- Recently it has been demonstrated that amphotericin B and nystatin conjugated with silver nanoparticles are very effective in disease models
- Administration of dexamethasone reduces intracranial pressure, cerebral edema and brain damage caused by hyperinflammation
- References: Exp Parasitol 2018;187:1, StatPearls: Amebic Meningoencephalitis [Accessed 14 September 2023], Biomolecules 2021;11:1320, ACS Chem Neurosci 2016;7:1178
Gross description
- Done on autopsy
- Brain shows extensive areas of hemorrhage and necrosis
- Cortex of brain is edematous
- Leptomeningeal purulent exudate may be noted
- Reference: AJNR Am J Neuroradiol 2006;27:1217
Frozen section description
- Frozen section not performed as PAM usually presents clinically with features of an infection
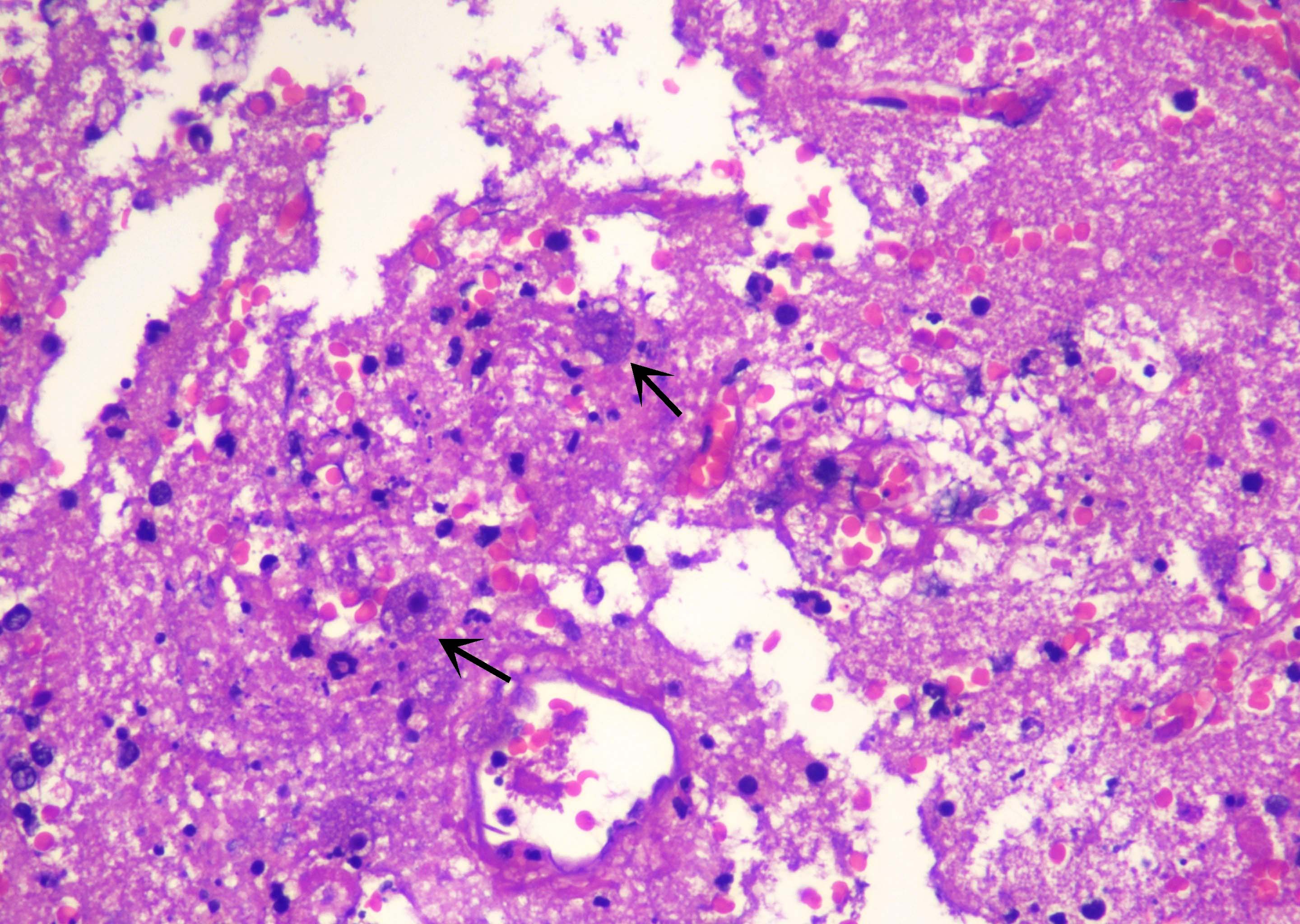
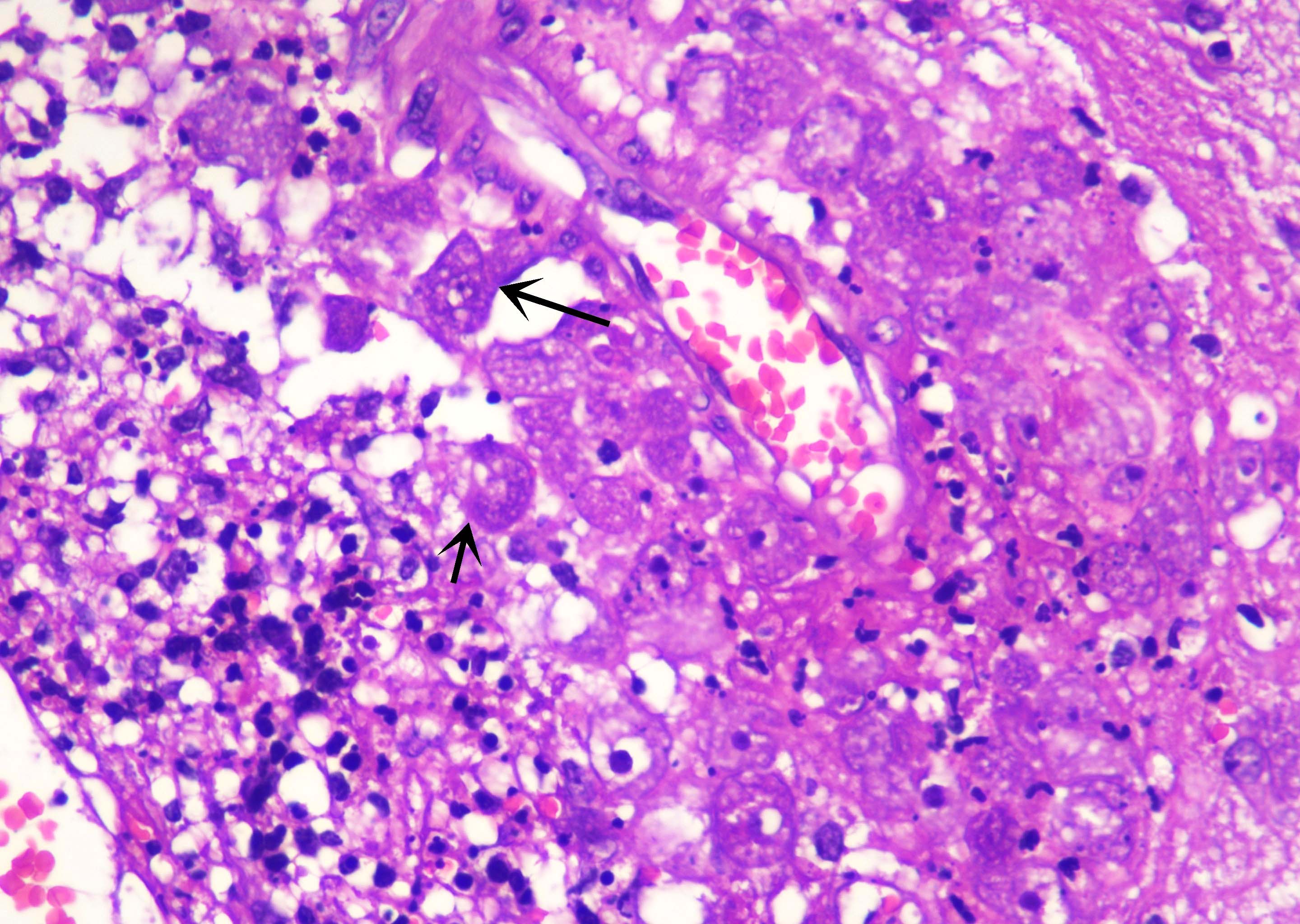
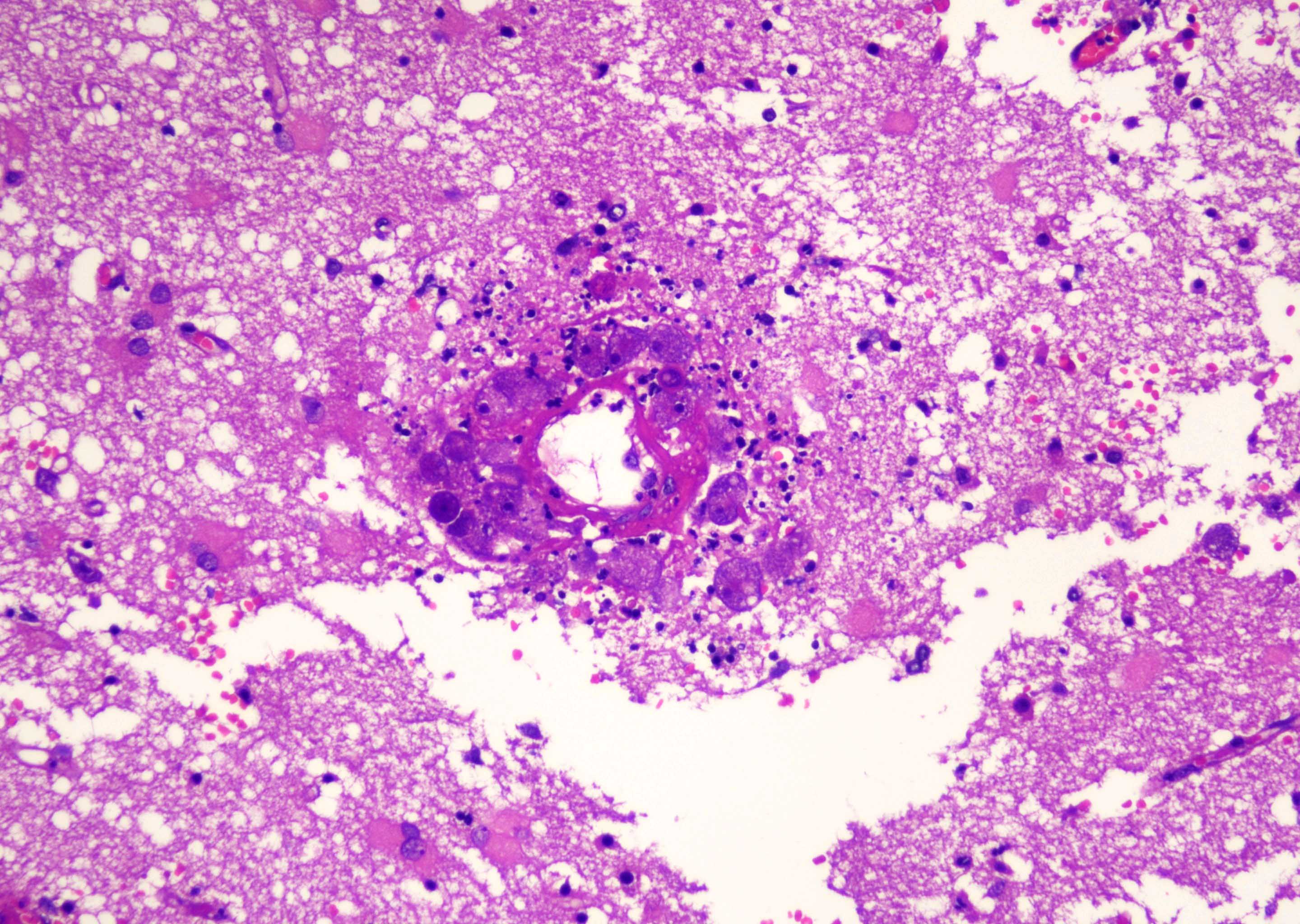
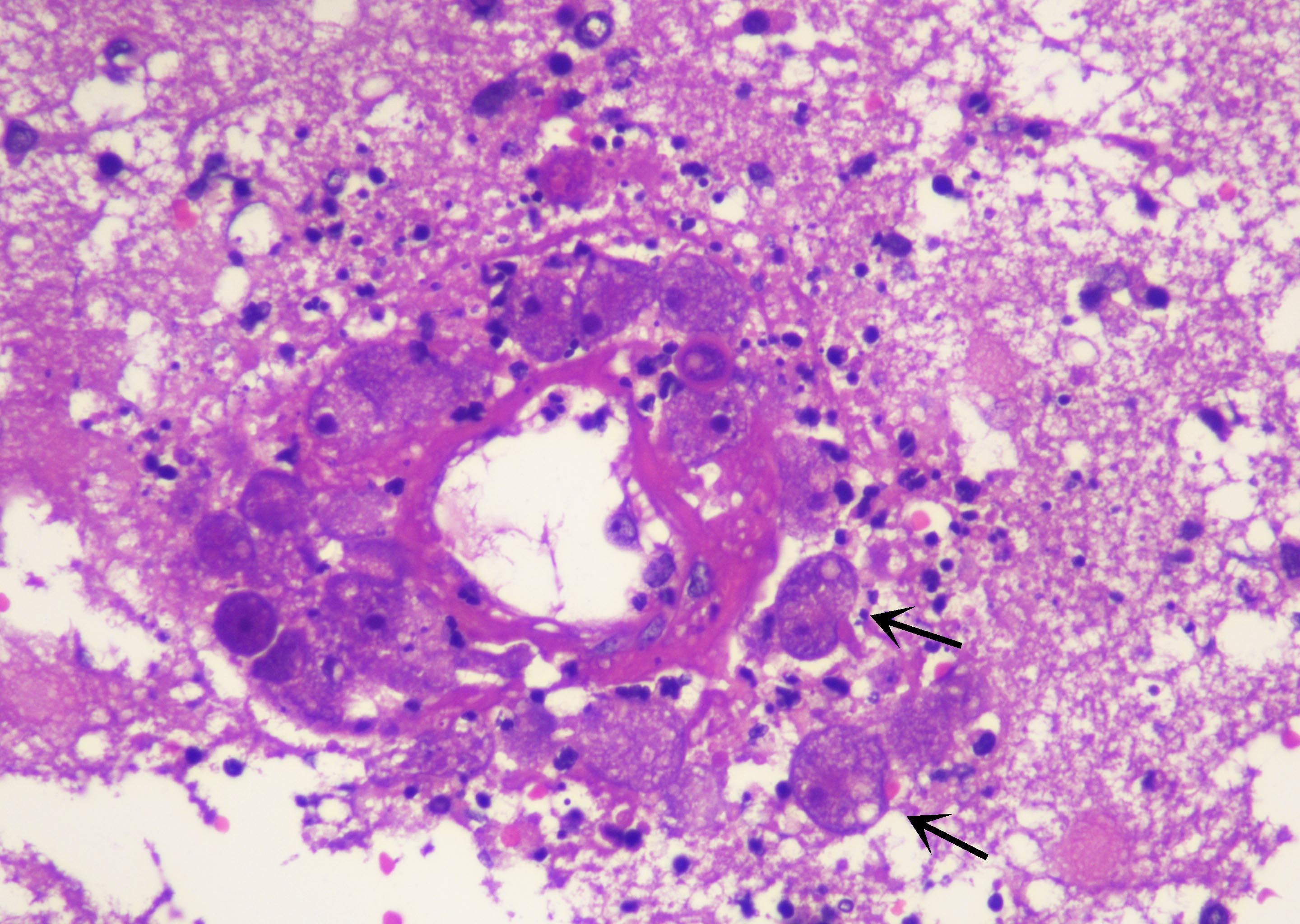
Microscopic (histologic) description
- Brain tissue shows massive, acute on chronic inflammatory cell infiltrate comprised of neutrophils, macrophages and a few eosinophils
- Necrotizing vasculitis, thrombosis, fibrinoid necrosis and a large number of round, large organisms, 15 - 25 μm, with vacuolated cytoplasm and single nuclei
- Leptomeningeal exudate is noted
- Direct wet mount preparation of CSF also reveals characteristic highly motile amoebic organisms and cysts
- Organism trophozoite form has a single nucleus with prominent nucleoli and exhibits vacuolated cytoplasm
- References: AJNR Am J Neuroradiol 2006;27:1217, Emerg Infect Dis 2004;10:1835, BMC Infect Dis 2017;17:532
Microscopic (histologic) images
Cytology description
- In CSF examination, N. fowleri trophozoites are large, round to pear shaped cells with a prominent, dark nucleus and scattered vacuoles (ACS Chem Neurosci 2016;7:1178)
Immunofluorescence description
- Fluorescent, cytoplasmic fine granules are noted
- Nfa1 detected by indirect immunofluorescence (Clin Diagn Lab Immunol 2005;12:873)
Positive stains
Negative stains
- Gram stain (should be avoided on laboratory testing as it can kill the amoeba)
Electron microscopy description
- Characteristic amoeba nuclei have a large nucleolus and distinctive mitochondria with coarse, granular cristae (J Med Microbiol 1979;12:363)
Electron microscopy description
Videos
Lab detection of N. fowleri
Sample pathology report
- Brain space occupying lesion, biopsy:
- Primary amebic meningoencephalitis (naegleriasis) (see comment)
- Comment: Histological examination of the sections reveal brain parenchyma predominantly exhibiting reactive gliosis along with dense inflammatory cell infiltrate comprised of neutrophils, lymphocytes and histiocytes. The intervening vascular channels show evidence of necrotizing vasculitis; a few scattered organisms are noted with centrally placed nuclei, a single prominent nucleolus and vacuolated cytoplasm. These organisms are highlighted on Wright-Giemsa stain and are positive for Nfa1 antibody on immunohistochemistry. The findings are suggestive of primary amebic meningoencephalitis (naegleriasis).
Differential diagnosis
- Other amebic infections:
- Balamuthia and Acanthamoeba brain infections can mimic PAM caused by N. fowleri; however, these infections are chronic and subacute in nature
- Both of these infections elicit a granulomatous response, which is absent in PAM (Mod Pathol 2007;20:1230)
- Brain abscess:
- Contains inflammatory cells along with macrophages
- Lacks N. fowleri trophozoites and Nfa1 is negative by immunohistochemistry
- Other bacterial, viral and protozoal causes of meningoencephalitis:
- Lack characteristic N. fowleri trophozoites and are negative for Nfa1 antibody (Patholog Res Int 2011;2011:290853, Handb Clin Neurol 2013;112:1171)
Board review style question #1
A 16 year old boy presented with acute onset of severe headache, emesis and fever after he went to a swimming camp at a lake. He was admitted into the emergency room. Cerebrospinal fluid (CSF) chemical analysis revealed leukocytosis, increased protein and decreased glucose. Microscopic examination of the CSF revealed predominance of neutrophils and scattered organisms with single nuclei, vacuolated cytoplasm and prominent pseudopodia. These organisms were highlighted on Wright-Giemsa stain. What is the most likely diagnosis?
- Acanthamoeba encephalitis
- Cytomegalovirus (CMV) encephalitis
- Herpes encephalitis
- Primary amebic meningoencephalitis
Board review style answer #1
D. Primary amebic meningoencephalitis (PAM). PAM is a waterborne disease caused by Naegleria fowleri and has rapid onset. The characteristic organism has a single nucleus, vacuolated cytoplasm and is highlighted on the Wright-Giemsa special stain. Answer A is incorrect because Acanthamoeba encephalitis has subacute onset of symptoms and is not associated with infected water. Answers B and C are incorrect because both CMV and herpes encephalitis cause acute viral encephalitis. The CSF findings are not suggestive of viral encephalitis and the organism morphology is also not typical of CMV or herpes infected cells.
Comment Here
Reference: Primary amebic meningoencephalitis
Comment Here
Reference: Primary amebic meningoencephalitis