Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Azimpouran M, Bannykh SI. Herpes simplex encephalitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnshsvencephalitis.html. Accessed March 31st, 2025.
Definition / general
- Inflammation of the brain parenchyma with neurologic dysfunction due to involvement of the brain by the herpes simplex viruses (HSV)
Essential features
- HSV encephalitis is the most common cause of acute necrotizing encephalitis
- HSV1 is responsible for > 90% of cases and affects older adults, with a median age of 57 years (J Neurol 2017;264:1204)
- HSV2 is responsible for disseminated neonatal encephalitis
- Polymerase chain reaction (PCR) is the diagnostic method of choice with a sensitivity of > 95% and specificity of ~99%
- Mortality without treatment is 70% (Clin Microbiol Rev 2020;33:e00105)
- With treatment the mortality drops to ~20% but 70% of survivors show neurological deficits (Clin Microbiol Rev 2020;33:e00105)
Terminology
- HSV encephalitis
ICD coding
- ICD-10: B00.4 - herpesviral encephalitis
Epidemiology
- Leading cause of encephalitis globally and accounts for > 33% of diagnosed cases in the United States (Med Mal Infect 2017;47:221)
- Most common cause of acute necrotizing encephalitis in immunocompetent individuals (Infect Disord Drug Targets 2011;11:235)
- Estimated annual incidence is 2 - 4 cases/million per year (Infect Disord Drug Targets 2011;11:235)
- HSV1 affects older adults with a median age of 57 years (J Neurol 2017;264:1204)
- There is no seasonality
- HSV2 infrequently causes postneonatal encephalitis but can be responsible for disease in immunosuppressed patients (Arch Neurol 2008;65:596)
Sites
- Asymmetric limbic system (medial temporal and frontal lobes), cingulate and insular cortex
- More diffuse presentation in neonatal HSV encephalitis
Pathophysiology
- Classic herpes simplex virus (HSV) encephalitis typically arises from HSV1, although HSV2 accounts for a minority
- Spread of HSV1
- Contact with infected saliva or respiratory secretions
- Primary infection by HSV1 typically involves the oropharyngeal mucosa
- Less common sites include the skin, particularly fingers and shoulders of wrestlers (herpes gladiatorum) (Sports Health 2013;5:423)
- Latent infection is caused by retrograde axonal transport along sensory fibers, leading to colonization of the primary sensory (such as trigeminal) ganglia (Mol Ther Methods Clin Dev 2020;18:33)
- 3 proposed routes of entry to the brain
- Spread of virus along olfactory nerve fibers and tracts
- Reactivation of latent virus in the trigeminal ganglia and its spread along either the centrally projecting nerve roots into the brain stem or the peripherally projecting sensory fibers that innervate the meninges of the anterior and middle cranial fossae
- Localized proliferation of the virus, accompanied by neuritic transport to the skin or mucosal tissues, results in the manifestation of cold sores
- Mechanisms of reactivation are unclear
- Reactivation may seem to be spontaneous, precipitated by local stimuli (e.g., trauma and ultraviolet [UV] irradiation) involving skin or mucosa innervated by latently infected neurons or may result from a range of systemic factors (e.g., pyrexia, emotional stress, physiological fluctuations in hormone levels during the menstrual cycle and immunosuppression)
- Reactivation of virus that has previously established latent infection within the brain (World Neurosurg 2016;89:731.e1)
- Neonatal HSV encephalitis
- HSV infection in neonates is infrequent
- Both HSV1 and HSV2 are implicated in causing neonatal herpes infection (Semin Perinatol 2018;42:168)
- Granulomatous HSV encephalitis
- HSV can cause granulomatous encephalitis in children, though its occurrence in adults has been rarely reported (Pract Neurol 2017;17:140)
- HSV induced autoimmune encephalitis
- Secondary immune mediated neurological deterioration triggered by HSV infection of the central nervous system (CNS)
- Mediated by neuronal autoantibodies, most commonly against the N-methyl-D-aspartate receptor (NMDAR) for the neurotransmitter glutamate (Clin Microbiol Rev 2020;33:e00105)
Etiology
- Herpes simplex virus 1 (HSV1) causes > 90% of cases
- Herpes simplex virus 2 (HSV2) predominantly causes disseminated neonatal encephalitis, with sporadic occurrences reported in elderly and immunocompromised individuals
- Predisposing factors
- Taking immunomodulatory drugs; e.g.,
- Azathioprine (Am J Gastroenterol 2010;105:240)
- Adalimumab (anti-TNFα monoclonal antibody) (Clin Infect Dis 2009;49:924)
- Fingolimod (antagonist of sphingosine-1-phosphate receptor) (Neurology 2015;84:2377)
- Natalizumab (monoclonal antibody targeting α-4 integrin) (Clin Infect Dis 2013;57:849)
- Genetic predisposition
- Defects in various signaling molecules in the TLR3 pathway (Science 2007;317:1522)
- Autosomal recessive deficiency in UNC93B (Science 2006;314:308)
- Mutations in TANK binding kinase 1 (TBK1) (J Exp Med 2012;209:1567)
- Mutations in NFκB essential modulator (NEMO), STAT1 and tyrosine kinase 2 (Genes Immun 2015;16:552)
- Taking immunomodulatory drugs; e.g.,
- Reference: Love: Greenfield’s Neuropathology, 9th Edition, 2015
Clinical features
- Combination of nonspecific features of encephalitis, along with focal neurological signs attributed to the engagement of the temporal and frontal lobes
- Fever, headache and confusion
- Focal neurological signs include aphasia and focal seizures
- While the onset may be fulminant, a substantial number of patients experience an influenza-like prodromal illness
- Personality changes and behavioral abnormalities might occur over several days (Neurol Sci 2013;34:1879)
Diagnosis
- Cerebrospinal fluid (CSF) HSV PCR
- Magnetic resonance imaging (MRI) of brain is the preferred imaging test
Laboratory
- Lumbar puncture, CSF
- May be normal in early stage
- Opening pressure: normal or slightly elevated
- Moderate lymphocytic pleocytosis (10 - 200/mm3)
- Variable numbers of red blood cells
- Elevation of protein, usually to 80 - 100 mg/dL
- Normal glucose
- HSV antibody titer in the CSF: 4 fold or greater rise
- Sensitivity is relatively poor and serological confirmation may not be possible for some weeks
- Culture of CSF is usually negative for HSV, although viral antigen can be demonstrated in the CSF in a high proportion of cases (Neurotherapeutics 2016;13:493)
- Increased levels of IFNγ, TNFα, IL6, IL2 receptor and CCL2
- IL1β/IL1Ra ratio > 0.55; high specificity (100%) and sensitivity (83%) for a poor outcome (Clin Microbiol Rev 2020;33:e00105)
- PCR based detection of HSV DNA in the CSF is the diagnostic method of choice
- Sensitivity: > 95%
- Specificity: ~99%
- Remains positive for several days after the commencement of treatment with acyclovir (Neurotherapeutics 2016;13:493)
- Brain biopsy is sensitive but aggressive and is replaced by PCR (Neurotherapeutics 2016;13:493)
- Elevated level of IL10 in serum is associated with a high Glasgow coma score (GCS) (Clin Microbiol Rev 2020;33:e00105)
- IgG antibodies against N-methyl-d-aspartate receptor (NMDAR) in the serum / CSF (Clin Microbiol Rev 2020;33:e00105)
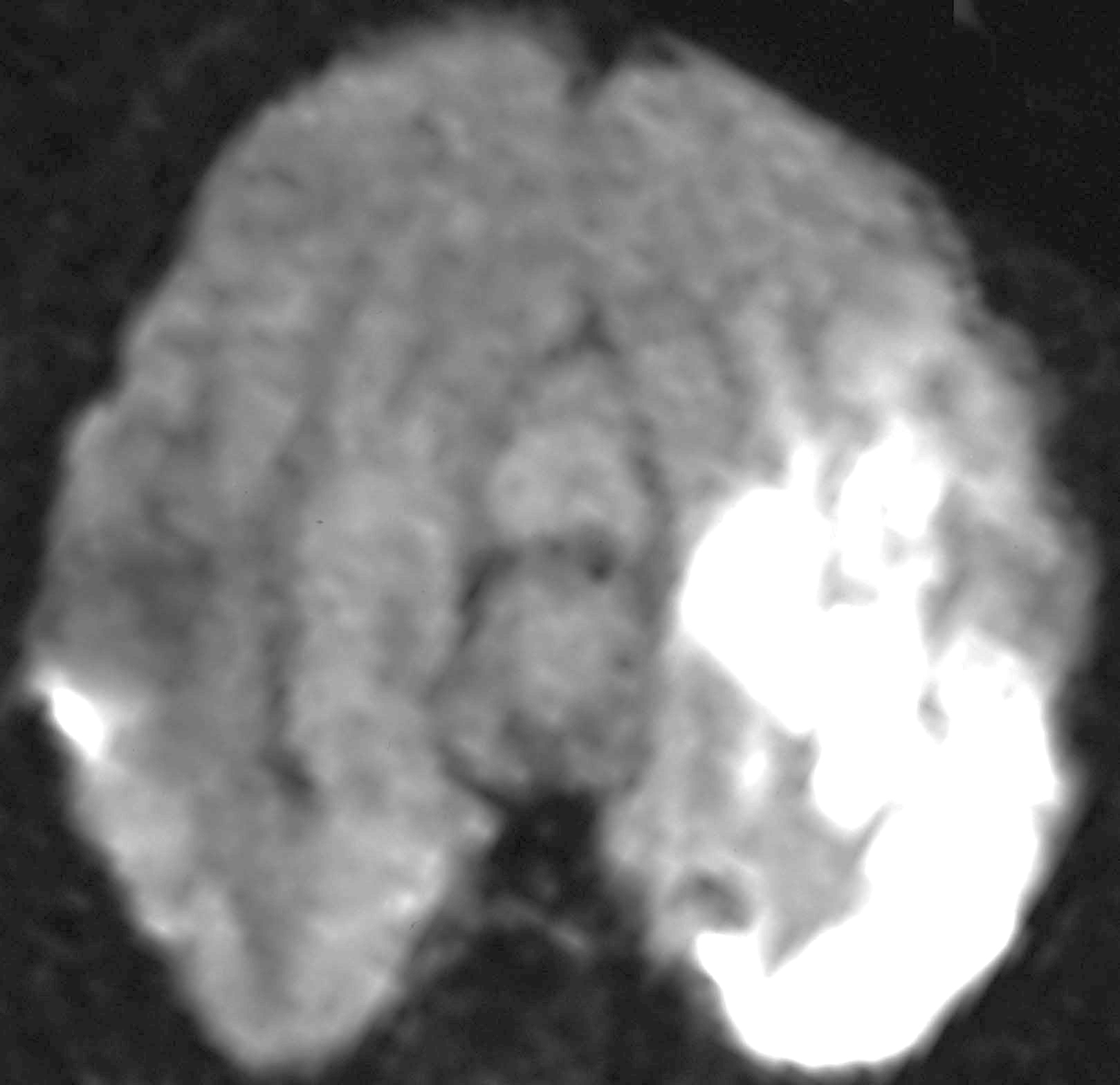
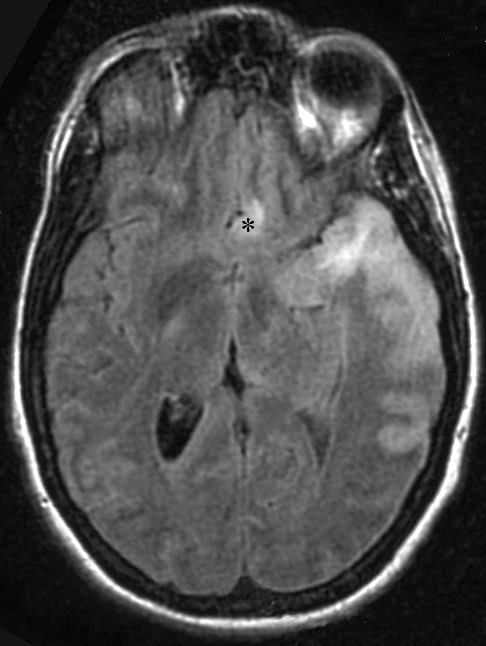
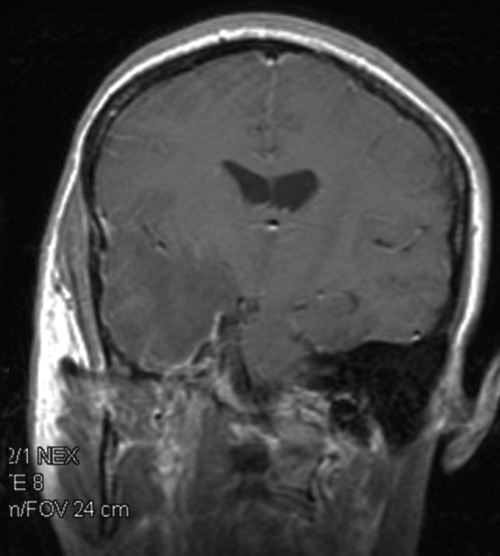
Radiology description
- MRI with and without contrast
- Most sensitive and specific imaging method
- T1: edema can be seen
- T1 with contrast: enhancement of temporal lobe in the affected area
- T2: asymmetric hyperintense lesions corresponding to areas of edema in the affected area
- Diffusion weighted imaging (DWI)
- More sensitive than T2 (in acute infection)
- Associated restricted diffusion may be seen due to edema (Acta Trop 2010;116:206)
- Computed tomography (CT) scans
- Hypodense lesions (typically in the temporal lobe), edema
- Low sensitivity, particularly early in the course of the illness
- Electroencephalography (EEG)
- Periodic discharges, focal or generalized slowing and electrographic seizures (JAMA Netw Open 2021;4:e2114328)
Radiology images
Contributed by Serguei Bannykh, M.D.
Images hosted on other servers:
Prognostic factors
- Mortality
- Without treatment is 70% (Clin Microbiol Rev 2020;33:e00105)
- With treatment is ~20%, with 70% of survivors suffering residual neurologic deficit (Clin Microbiol Rev 2020;33:e00105)
- Factors most frequently associated with mortality and morbidity
- Age: < 3 years and elderly (J Infect 2017;74:42, Front Neurol 2023;14:1130090)
- Pre-existing morbidity (Infection 2016;44:337)
- Fever on admission (Intensive Care Med 2019;45:1103)
- Duration of fever after start of treatment (Enferm Infecc Microbiol Clin 2009;27:143)
- Lower GCS or a higher acute physiology and chronic health evaluation (APACHE) score on admission (J Neurol 2016;263:277)
- Longer interval between onset of main symptoms and hospitalization (Front Neurol 2023;14:1130090)
- Pre-existing immunocompromised state in HSV2 (Mayo Clin Proc 2014;89:274)
- Status epilepticus, persistence of impaired consciousness, confusion or aphasia (J Neurol 2022;269:3625)
- Mechanical ventilation (J Neurol 2022;269:3625)
- Length of stay in the intensive care unit (ICU) (J Neurol 2022;269:3625)
- IL1β/IL1Ra ratio > 0.55 (Clin Microbiol Rev 2020;33:e00105)
- Neurofilament level (NFL) in CSF (Clin Microbiol Infect 2021;27:1131)
- Xanthochromia (BMC Infect Dis 2012;12:356)
- Involvement of more than 3 brain lobes as well as presence of abnormalities in the left thalamus by MRI (JAMA Netw Open 2021;4:e2114328)
- No direct correlation between viral load in CSF and clinical outcome has been found (J Neurol 2009;256:1243)
Case reports
- 23 year old woman presented with epileptic attack followed by psychiatric symptoms of confusion and irritation as well as cognitive deficits (Neurol Sci 2021;42:857)
- 27 year old man presented with severe headache and altered mental status 3 days after administration of ChAdOx1 nCoV-19 vaccine (BMC Infect Dis 2022;22:217)
- 27 year old man with a 3 day history of partial loss of consciousness and falls (J Neurovirol 2020;26:138)
- 78 year old woman with declining mental status 11 days after a posterior C3 T1 tumor resection (Case Rep Surg 2019;2019:2065716)
Treatment
- Antiviral therapy; acyclovir / foscarnet / ganciclovir (Clin Microbiol Rev 2020;33:e00105)
- Cerebral edema; mannitol / dexamethasone / hypertonic saline
- Active brain herniation, 23% saline (Neurotherapeutics 2016;13:493)
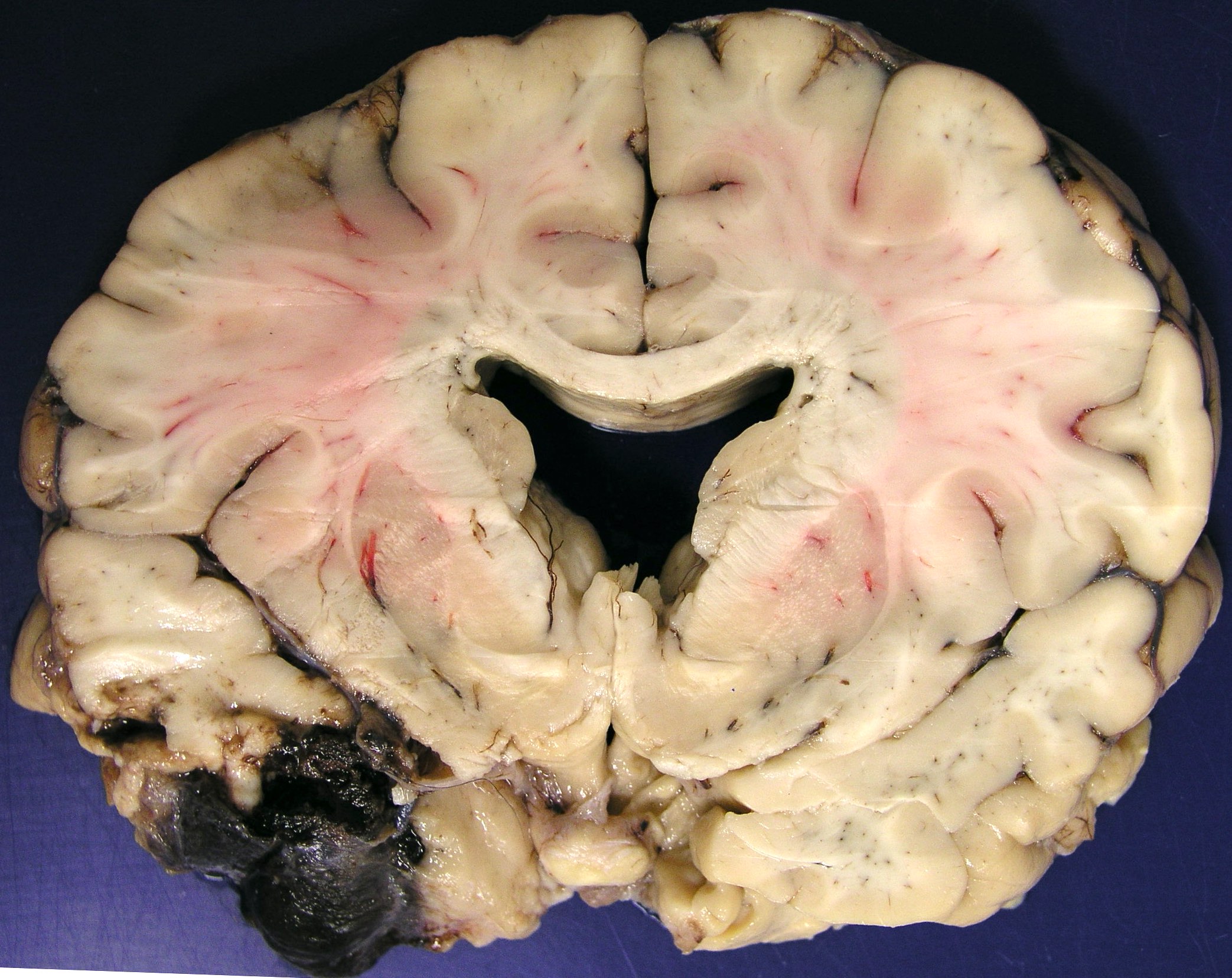
Gross description
- Acute phase
- Bilateral, usually asymmetrical, hemorrhagic necrosis involving the temporal lobes, especially anteriorly and inferiorly, and to a greater or lesser extent, the insulae, cingulate gyri, posterior orbital frontal cortices and underlying white matter
- Brain is usually edematous
- In the early phase, the lesions can be confined to the inferomedial part of 1 temporal lobe only or brain may even appear grossly normal
- Chronic phase
- In patients dying some weeks after the onset of untreated or unsuccessfully treated disease, the hemorrhagic necrosis progresses to cavitation and atrophy, with indentation or collapse of the affected temporal lobes, yellow to brown discoloration of the surrounding brain tissue and overlying meninges
- In longer term survivors, the affected parts of the brain appear shriveled and brown
- References: Love: Greenfield’s Neuropathology, 9th Edition, 2015, Clin Neuropathol 1995;14:45
Gross images
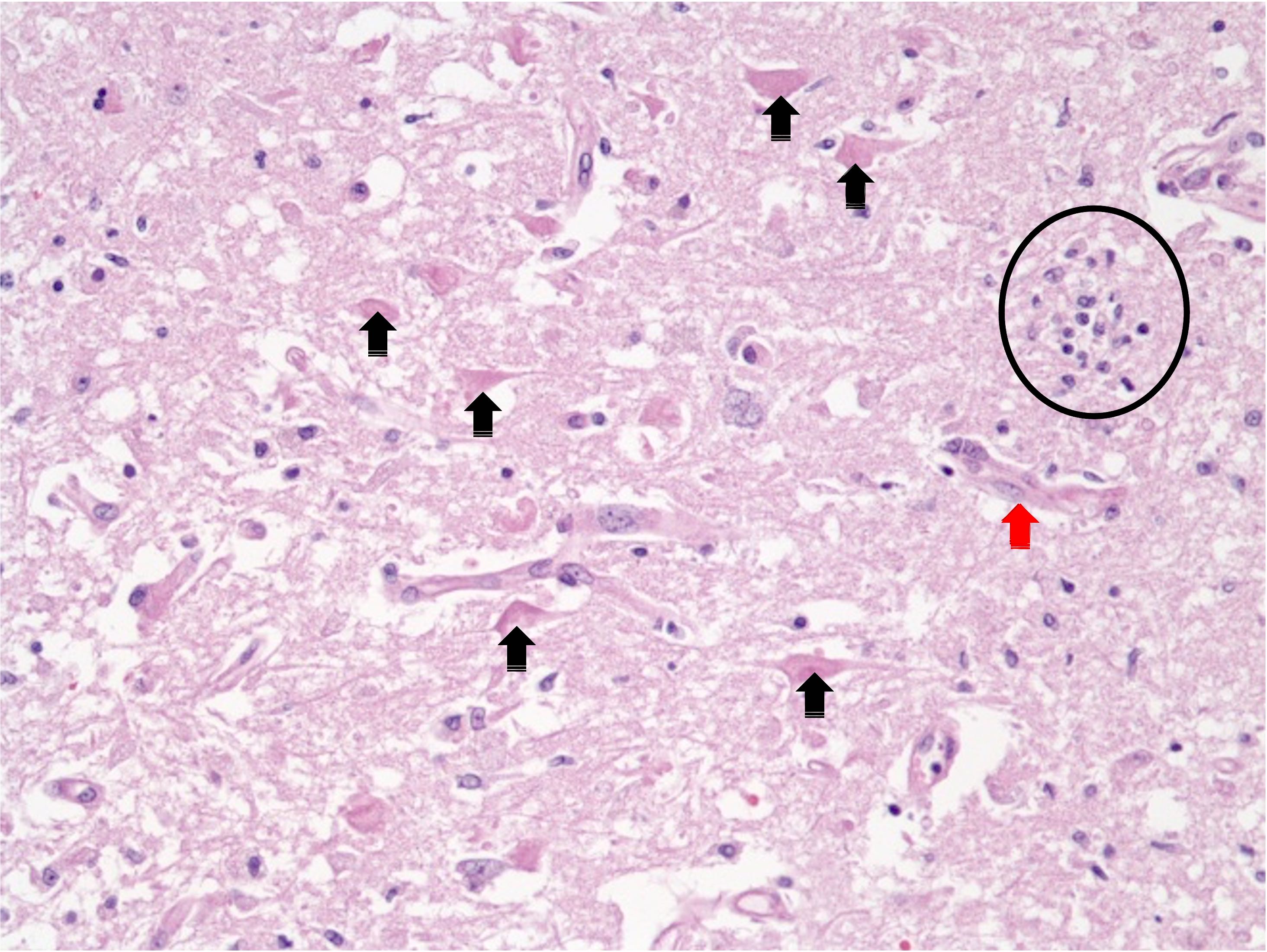
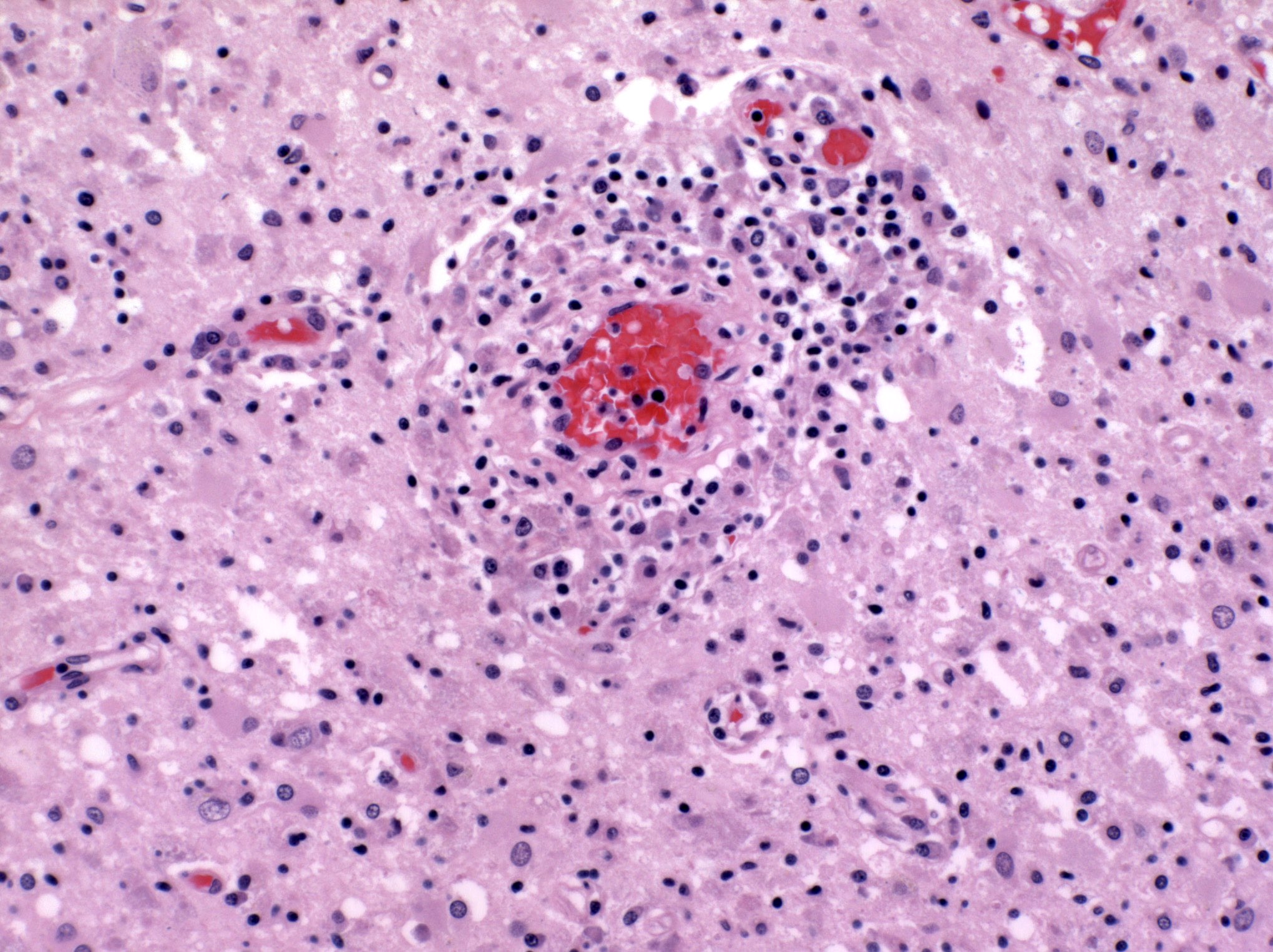
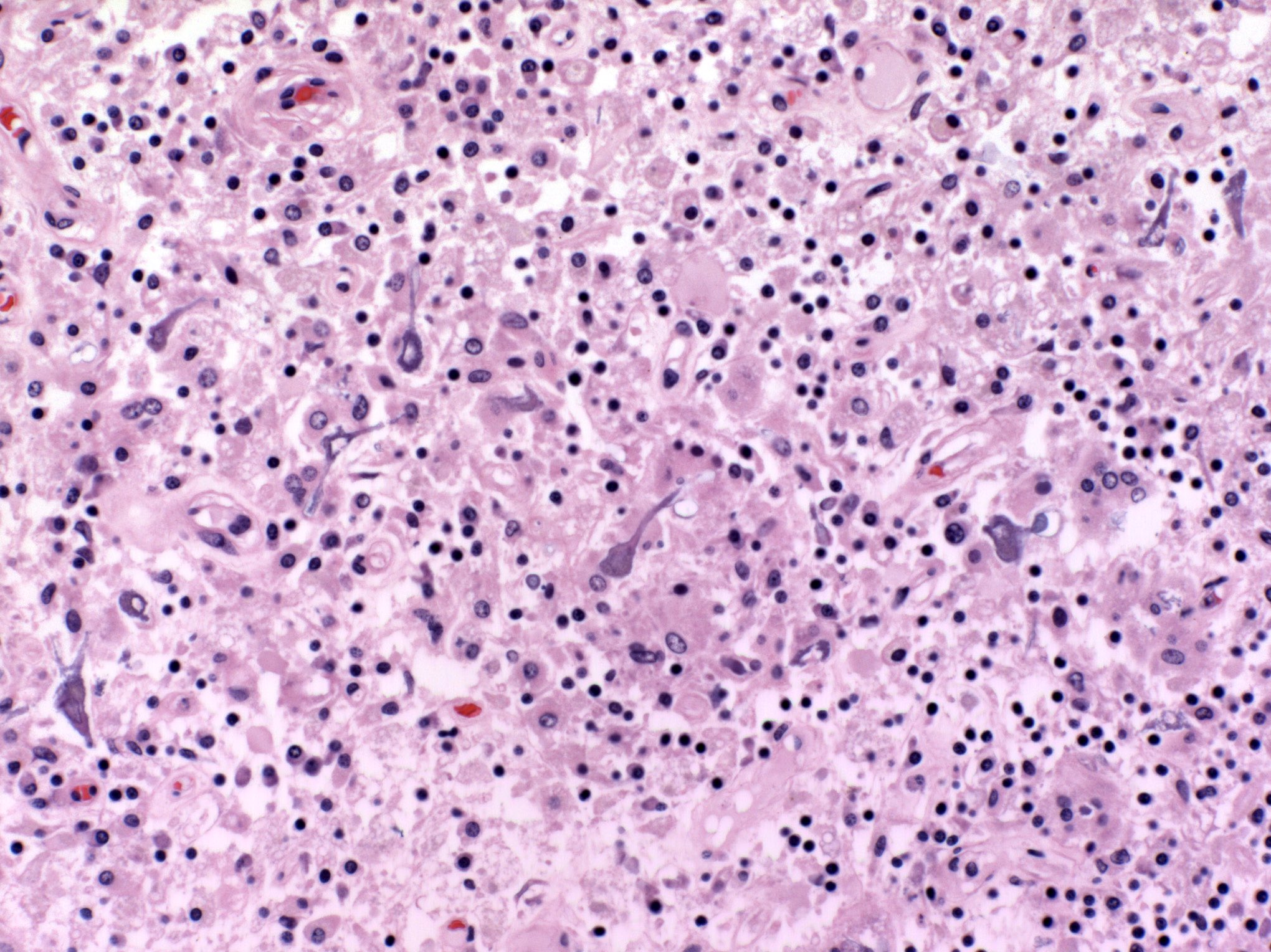
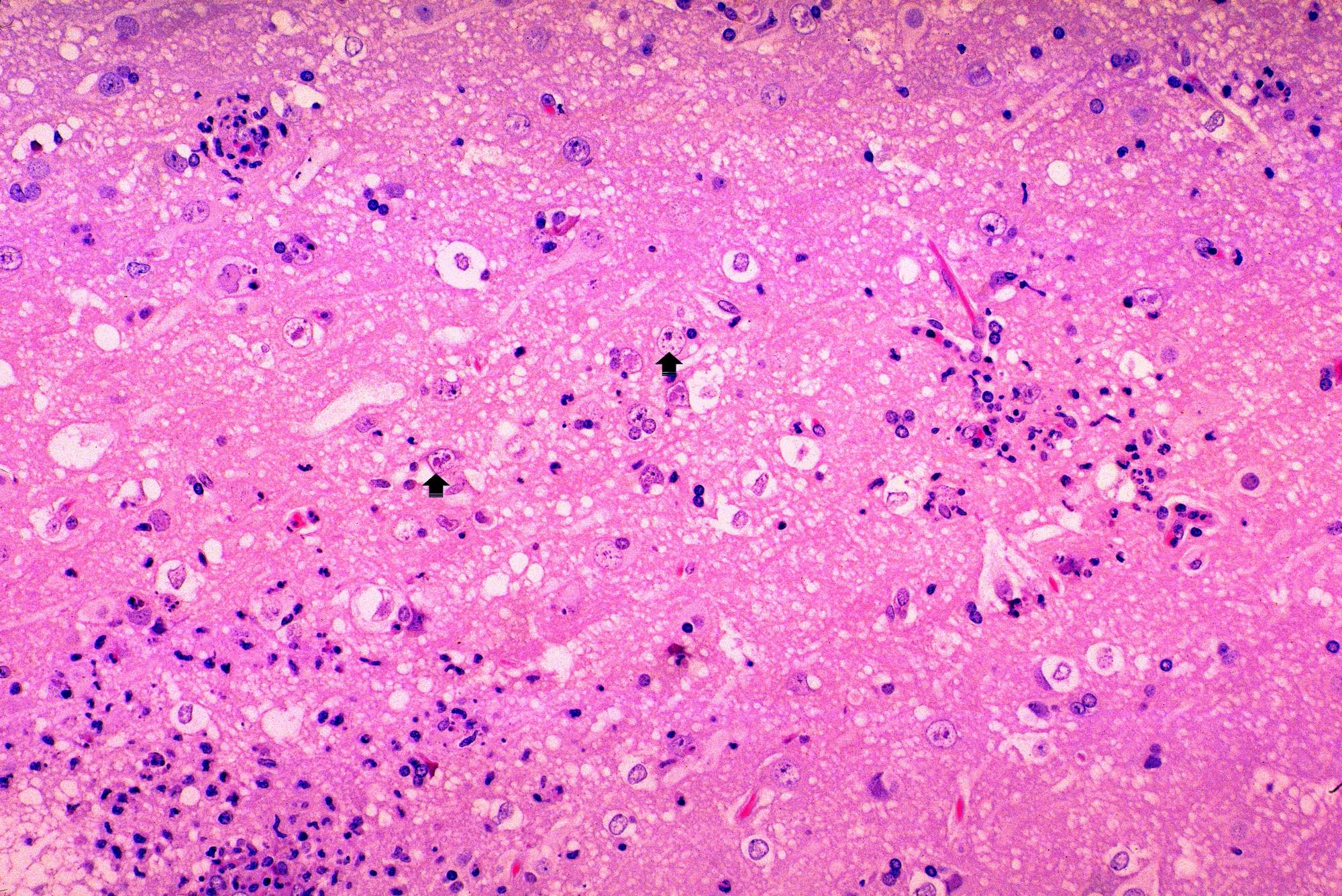
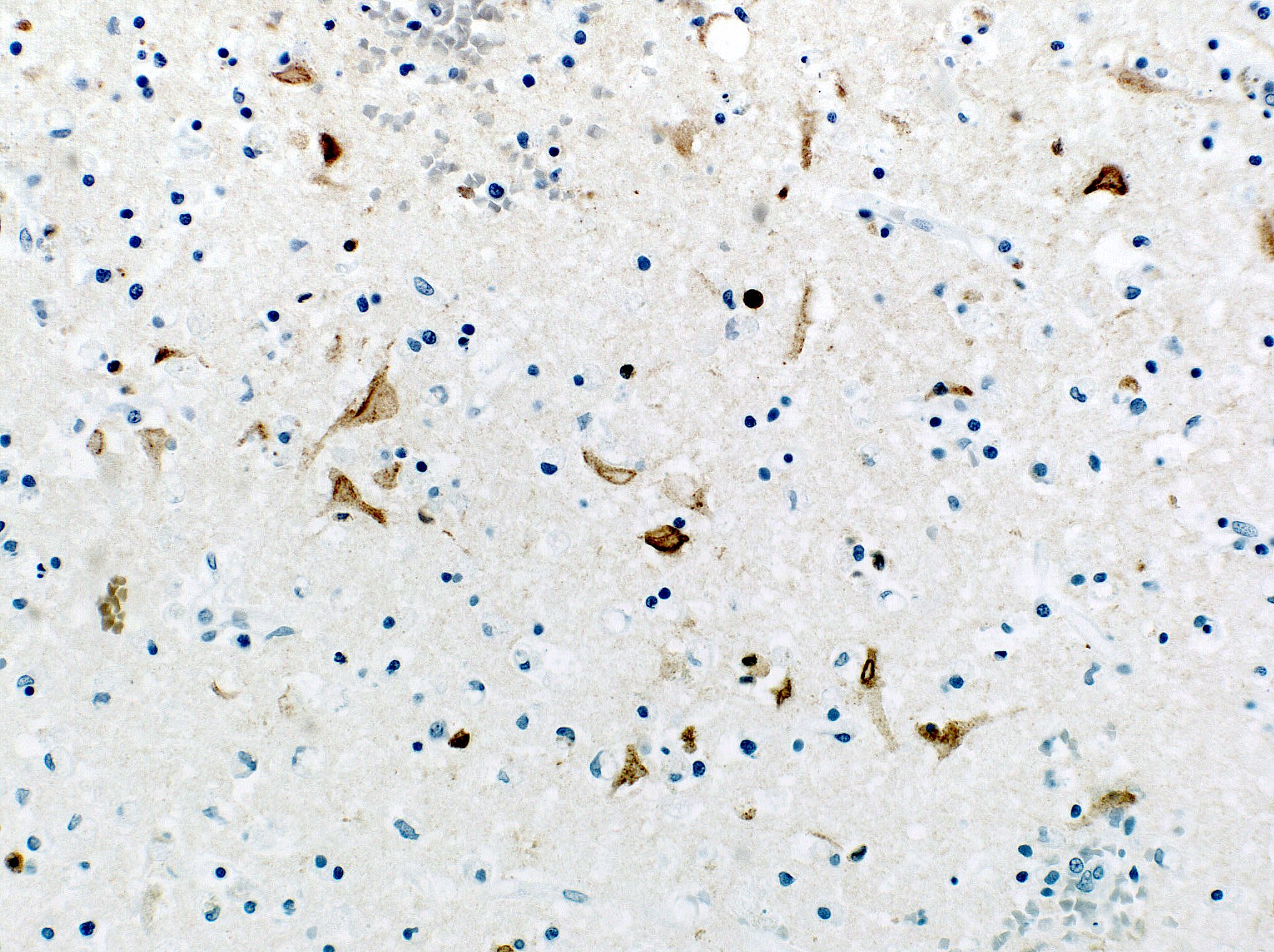
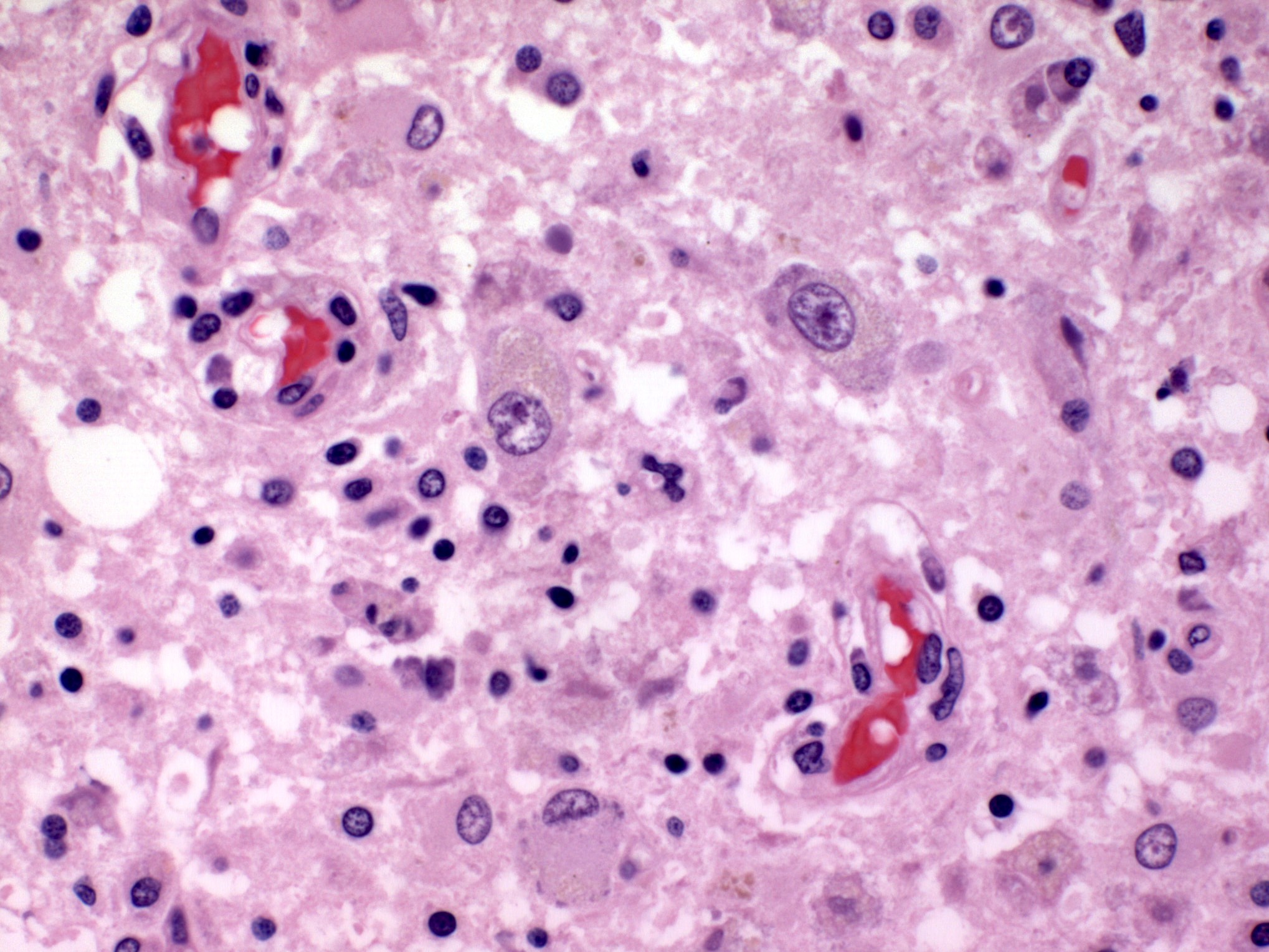
Microscopic (histologic) description
- Early phase of acute infection
- Little or no parenchymal inflammation
- Perivascular neutrophils and lymphocytes
- Affected neurons, glia and endothelial cells tend to have slightly hypereosinophilic cytoplasm
- Neuronal intranuclear eosinophilic or basophilic inclusions composed of nucleic acid and protein (Cowdry A inclusions)
- Clumps of eosinophilic inclusions in the cytoplasm
- Advanced phase of acute infection
- Ferrugination of necrotic neurons
- Resolving hemorrhage
- Perivascular and interstitial infiltrates of lymphocytes and sheets of foamy macrophages
- Neuronophagia and microglial nodules
- Nuclear inclusions are sparse at this stage (Acta Neuropathol 2016;132:433)
Microscopic (histologic) images
Electron microscopy description
- HSV hexagonal viral particles appear as arrays and scattered single particles (size: 185 - 225 nm) in the nucleus of a neurons
Electron microscopy images
Molecular / cytogenetics description
- PCR based detection of HSV DNA in the CSF is the diagnostic method of choice (Neurotherapeutics 2016;13:493)
- In situ hybridization with a cloned HSV DNA probe shows viral RNA in astrocytes, neurons and macrophages (Neuropathol Appl Neurobiol 1988;14:395, Virchows Arch A Pathol Anat Histopathol 1988;414:39)
Videos
HSV encephalitis
Sample pathology report
- Brain, right temporal, biopsy:
- Acute lymphocytic herpes virus encephalitis
- Positive for HSV1 by IHC
Differential diagnosis
- Primary or secondary CNS infections caused by mycobacteria / atypical organisms / viruses / prion / fungus or parasites:
- HIV encephalitis:
- Presence of subcortical microglial nodules with multinucleated microglial cells is virtually pathognomonic for HIV encephalitis in settings of HIV seropositivity
- Autoimmune or paraneoplastic limbic encephalitis:
- Onset and evolution tend to be more subacute than acute
- Nonnecrotizing histopathology consisting of perivascular lymphocytic infiltrates and microglia nodules
- Identification of autoantibodies helpful in this differential
- Primary intracranial or metastatic tumors:
- Biopsy or surgical resection required for definitive diagnosis
- Intravascular lymphoma:
- Highly atypical CD20 positive cell inside microvasculature
- Acute infarcts:
- Neurons with acute hypoxic / ischemic type histologic changes found in both
- No microglial nodules, neuronophagia or viral cytopathic effect
- Negative HSV staining
- Negative PCR test
- Hypoxemic and septic encephalopathies:
- Requires clinical correlation
- HSV negative on immunostaining
- No microglial nodules, neuronophagia or viral cytopathic effect
- Metabolic causes, including hepatic / uremic encephalopathies, Wernicke encephalopathy, mitochondrial encephalopathies, hypoglycemia, hyponatremia or hypernatremia, hypocalcemia or hypercalcemia:
- Neurons are relatively spared within many metabolic lesions
- HSV negative on immunostaining
- No microglial nodules, neuronophagia or viral cytopathic effect
- Requires clinical correlation for more definite diagnosis
- Vasculitis, systemic lupus erythematosus (SLE), Behçet disease:
- HSV negative on immunostaining
- No microglial nodules, neuronophagia or viral cytopathic effect
- Destructive granulomatous or lymphocytic vasculitis present for vasculitic lesions
- Microthrombi can be present in SLE associated CNS disease (Rheumatology (Oxford) 2017;56:77)
Board review style question #1
Which diagnostic method is commonly employed for the confirmation of herpes simplex virus (HSV) encephalitis, specifically involving the examination of cerebrospinal fluid?
- Magnetic resonance imaging (MRI)
- Microscopic analysis of brain biopsy
- Polymerase chain reaction (PCR)
- Serological testing for antibodies
Board review style answer #1
C. Polymerase chain reaction (PCR). PCR is a highly sensitive and specific technique that can detect and amplify specific DNA sequences. In the context of HSV encephalitis, PCR is used to amplify and identify HSV DNA in the cerebrospinal fluid (CSF). PCR allows for the early and rapid detection of viral DNA, providing a quicker diagnosis compared to other methods. This is crucial in the case of encephalitis, where prompt treatment is essential.
Answer D is incorrect because serological testing is valuable for detecting antibodies in the blood but may not directly confirm the presence of the virus in the CSF, which is crucial for diagnosing HSV encephalitis. Answer A is incorrect because while MRI is an important imaging modality for identifying brain abnormalities, it does not directly detect the presence of HSV in the CSF. It is often used as a complementary tool for diagnosis but is not the primary method for confirming HSV encephalitis. Answer B is incorrect because although brain biopsy can provide direct tissue samples for analysis, it is generally not the first line approach for diagnosing HSV encephalitis due to its invasiveness; moreover, CSF analysis through PCR is more commonly employed for its sensitivity and specificity in detecting HSV DNA.
Comment Here
Reference: Herpes simplex encephalitis
Answer D is incorrect because serological testing is valuable for detecting antibodies in the blood but may not directly confirm the presence of the virus in the CSF, which is crucial for diagnosing HSV encephalitis. Answer A is incorrect because while MRI is an important imaging modality for identifying brain abnormalities, it does not directly detect the presence of HSV in the CSF. It is often used as a complementary tool for diagnosis but is not the primary method for confirming HSV encephalitis. Answer B is incorrect because although brain biopsy can provide direct tissue samples for analysis, it is generally not the first line approach for diagnosing HSV encephalitis due to its invasiveness; moreover, CSF analysis through PCR is more commonly employed for its sensitivity and specificity in detecting HSV DNA.
Comment Here
Reference: Herpes simplex encephalitis
Board review style question #2
A 35 year old woman who delivered a healthy baby 2 weeks prior presented with confusion, memory problems and altered mental status. A subsequent MRI revealed a T2 hyperintense left medial temporal focally enhancing lesion and cerebrospinal fluid (CSF) analysis is pending. Given the possibility of uncal herniation, an open biopsy was performed and a representative H&E image is displayed above. Which of the following statements are accurate regarding the diagnosis of HSV (herpes simplex virus) encephalitis based on the provided information?
- Brain biopsy is indispensable for diagnosis of HSV encephalitis
- False negative rate of HSV1 / 2 PCR on CSF analysis is 50%
- Histologic findings in the above image are not supportive of a diagnosis of HSV encephalitis
- HSV encephalitis can result in short term memory failure
Board review style answer #2
D. HSV encephalitis can result in short term memory failure. HSV encephalitis can result in confusion and altered mental status and especially a short term memory failure as observed in this case. Confusion and altered mental status are common clinical manifestations of HSV encephalitis. The information provided in the question, where the patient presented with confusion, memory problems and altered mental status, aligns with the typical neurological symptoms associated with HSV encephalitis.
Answer B is incorrect because in HSV encephalitis, the sensitivity of PCR test is reported as 95%, therefore the false negative rate constitutes 5%. Answer A is incorrect because in an appropriate clinical setting with supporting CT or MRI findings, PCR based cerebrospinal fluid (CSF) analysis for HSV is sufficient for the diagnosis of HSV encephalitis, precluding a need for invasive brain biopsy. Answer C is incorrect because the characteristic features of viral encephalitis, such as inflammation and cellular changes, as shown in the above image, are indeed observed in the histological examination.
Comment Here
Reference: Herpes simplex encephalitis
Answer B is incorrect because in HSV encephalitis, the sensitivity of PCR test is reported as 95%, therefore the false negative rate constitutes 5%. Answer A is incorrect because in an appropriate clinical setting with supporting CT or MRI findings, PCR based cerebrospinal fluid (CSF) analysis for HSV is sufficient for the diagnosis of HSV encephalitis, precluding a need for invasive brain biopsy. Answer C is incorrect because the characteristic features of viral encephalitis, such as inflammation and cellular changes, as shown in the above image, are indeed observed in the histological examination.
Comment Here
Reference: Herpes simplex encephalitis