Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nisarga P, Gyure KA. Hepatic encephalopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnshepatic.html. Accessed March 30th, 2025.
Definition / general
- Spectrum of neurocognitive abnormalities occurring in patients with acute or chronic liver disease or portosystemic shunting
Essential features
- Clinical pattern and pathology are not dependent on the etiology of liver disease
- Characterized by neurocognitive abnormalities
- Elevated blood ammonia levels considered to play central role
- Histologic hallmark - Alzheimer type II astrocyte - enlarged, pale nuclei with a rim of chromatin
- Histology nonspecific (see Differential diagnosis)
Terminology
- Hepatic encephalopathy (HE)
- Portosystemic encephalopathy
ICD coding
Epidemiology
- Chronic alcoholism, acute drug poisoning, status post portosystemic bypass, hepatic failure patients
Sites
- Gray matter astrocytes
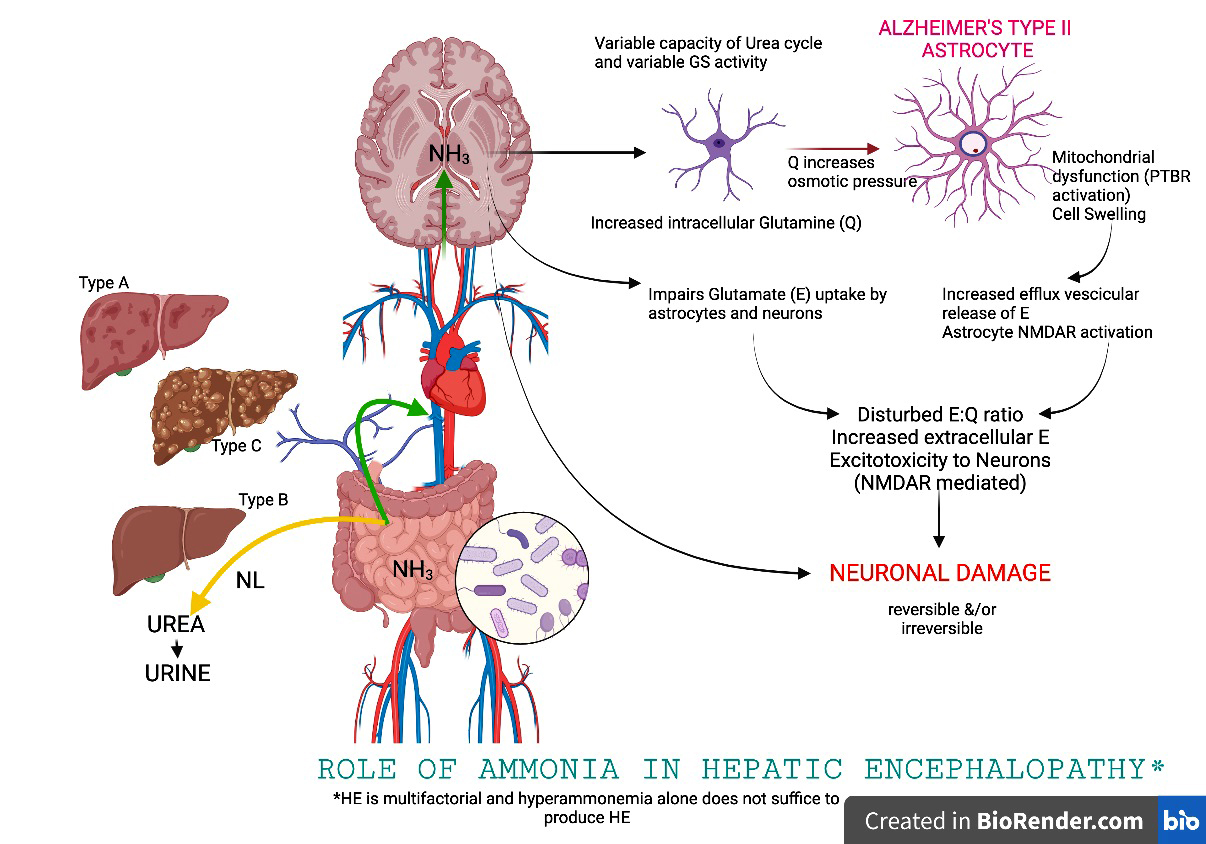
Pathophysiology
- Acute hepatic encephalopathy: cerebral edema and increased intracranial pressure (cause of death)
- Pathophysiology of hepatic encephalopathy is multifactorial
- Postulated agents include ammonia (NH3), inflammatory cytokines, manganese deposition in the basal ganglia, benzodiazepine-like compounds (GABA), microbiota and aromatic amino acids (Drugs 2019;79:17)
- Ammonia has been considered to play a central role in HE (see Diagrams / tables)
Etiology
- HE type A: HE associated with acute liver failure (e.g. acetaminophen overdose)
- HE type B: HE associated with portosystemic bypass in the absence of hepatic disease
- HE type C: HE associated with cirrhosis and portal hypertension or portosystemic bypass
- Reference: Hepatology 2002;35:716
Clinical features
- Disorientation, behavioral and personality changes, including somnolence, agitation, anger and restlessness
- Motor abnormalities, including Parkinsonism, choreoathetosis, spastic paraparesis with hyperreflexia and slowness of speech
- Dementia-like pattern and sleep disturbances
- May be precipitated by infection, gastrointestinal bleeding, medication noncompliance, electrolyte imbalance / renal failure or acute liver injury
- Clinical patterns: coma, rapidly developing confusion (somnolent or agitated), continuous mild mental dysfunction with recurrent episodes of severe confusion, predominant motor disorder (pyramidal and extrapyramidal) or mild brain dysfunction (J Clin Exp Hepatol 2018;8:432)
- Asterixis in alcoholic liver disease
Diagnosis
- Based predominantly on clinical features
- West Haven criteria used to grade severity (Hepatology 2002;35:716)
Laboratory
- Serum ammonia levels may be elevated
Radiology description
- Symmetric, hyperintense signal in the basal ganglia, especially the globus pallidus, on T1 weighted MR images
- Restricted diffusion in the cerebral cortex (diffusion weighted imaging)
- Reference: AJNR Am J Neuroradiol 2008;29:1612
Prognostic factors
- Prognosis based on percent of viable hepatic parenchyma in acute hepatic failure
- Necrosis > 50% in liver biopsy - threshold for liver transplantation (Clin Liver Dis 2018;22:257)
- Poor prognosis independent of severity of liver disease and despite treatment advances; 1 year survival approximately 20 - 40% (World J Gastroenterol 2020;26:2221)
Case reports
- 59 year old woman with status epilepticus as an initial manifestation of hepatic encephalopathy (World J Clin Cases 2020;8:6480)
- 59 year old woman with hepatic encephalopathy mimicking acute dominant middle cerebral artery ischemic stroke (Case Rep Neurol 2019;11:304)
- 71 year old woman, noncirrhotic, with persistent encephalopathy (ACG Case Rep J 2020;7:e00493)
Treatment
- Treatment of precipitating event
- Reduce blood ammonia concentration using nonabsorbable disaccharides or antibiotics
- Liver transplantation
- Reference: Aliment Pharmacol Ther 2010;31:537
Gross description
- Acute hepatic encephalopathy: cerebral edema with herniation
- Chronic hepatic encephalopathy: brain is typically normal grossly
- Reference: N Engl J Med 2016;375:1660
Microscopic (histologic) description
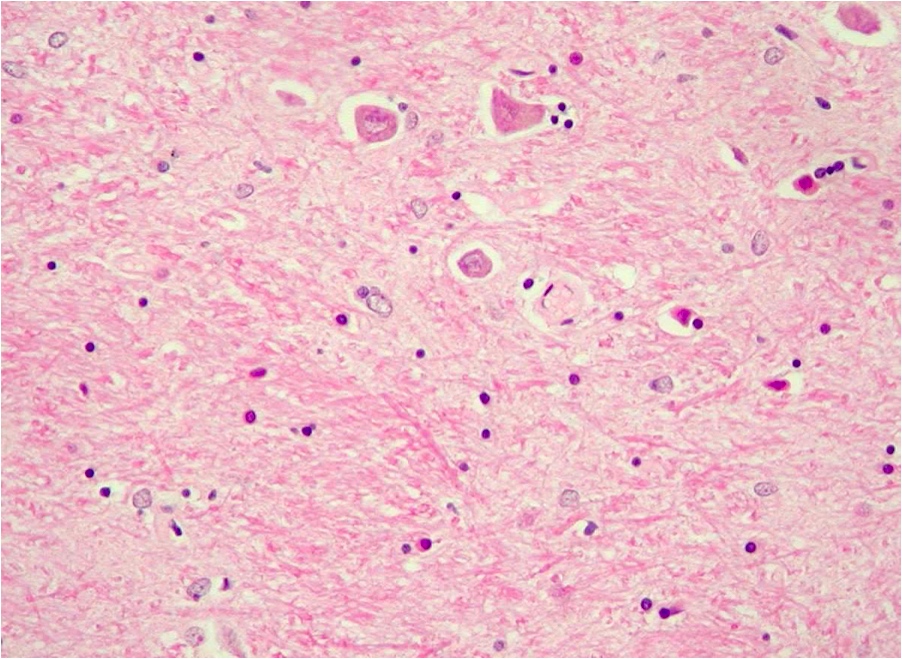
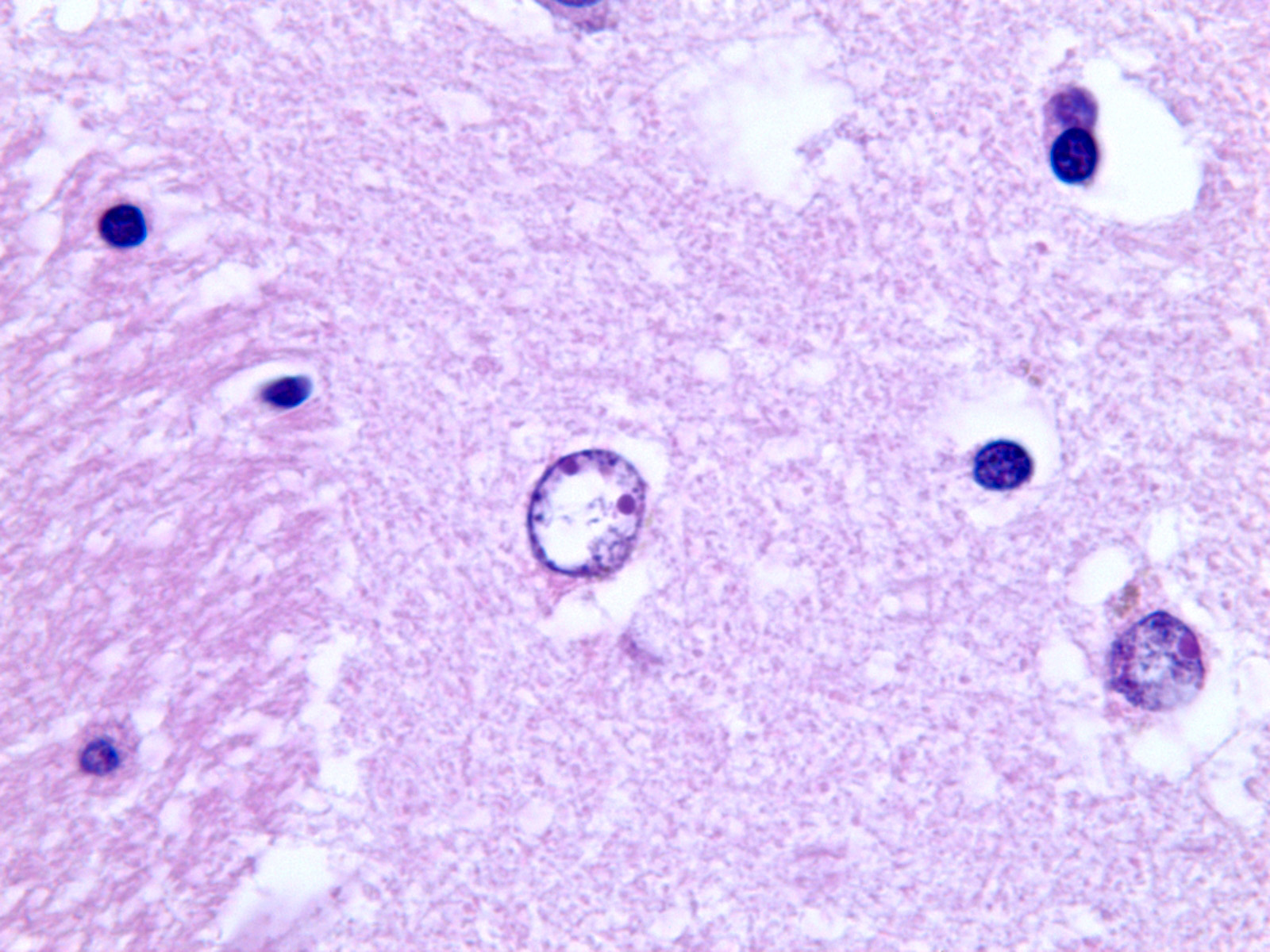
- Alzheimer type II astrocytes: enlarged, pale nuclei with a rim of chromatin and a prominent nucleoli
- Astrocyte doublets / pairs and triplets are seen
- Severe disease: astrocyte nucleus appears lobulated and contains glycogen granules
- Most commonly seen in gray matter regions, including globus pallidus, putamen, pons, thalamus, dentate nucleus and cortical gray matter (deep layers)
- Acute hepatic encephalopathy: brain edema due to swelling of perivascular astrocytes (Hepatology 1992;15:1060)
- Reference: J Neuropathol Exp Neurol 1994;53:213
Microscopic (histologic) images
Positive stains
- p62 highlights Alzheimer type II astrocytes but is nonspecific (Neuropathology 2020;40:358)
Negative stains
- Severe disease: astrocytes lose immunoreactivity to GFAP
Sample pathology report
- History of cirrhosis with hepatic encephalopathy
- Alzheimer type II astrocytosis
Differential diagnosis
- Differential diagnosis is investigated from a clinicoradiological standpoint
- Clinically should be distinguished from stroke
- Alzheimer type II astrocytes also seen in uremic encephalopathy, hypercapnic encephalopathy and in infants with hypoxia and hypoglycemia; their distinction from hepatic encephalopathy is based on clinical and radiologic features, not pathology
Additional references
Board review style question #1
Which of the following is the most likely cause of death in a patient with acute hepatic encephalopathy?
- Acute renal failure
- Bleeding diathesis
- Cerebral edema
- Hypoglycemia
- Myocardial necrosis
Board review style answer #1
C. Cerebral edema and herniation are common in acute hepatic encephalopathy
Comment Here
Reference: Hepatic encephalopathy
Comment Here
Reference: Hepatic encephalopathy
Board review style question #2
Board review style answer #2
A. Alzheimer type II astrocytes are most commoly found in the basal ganglia, especially the globus pallidus
Comment Here
Reference: Hepatic encephalopathy
Comment Here
Reference: Hepatic encephalopathy