Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Prayson BE, Prayson R. Focal cortical dysplasia (epilepsy related malformations). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnsfocalcorticaldysplasia.html. Accessed March 31st, 2025.
Definition / general
- Focal cortical dysplasia (FCD) represents a phenotypically diverse group of developmental disorders marked by abnormalities of cortical architecture
Essential features
- Focal cortical dysplasia is marked by cortical architectural abnormalities secondary to disruptions of cortical development
- Most patients clinically present with epilepsy and in a subset of pharmacoresistent cases, surgery may be employed in an attempt to control the seizures
- Some focal cortical dysplasia patterns may be grossly evident (e.g., polymicrogyria, pachygyria, heterotopia)
- The most common morphologic patterns encountered include disruptions in the cortical architecture in either a horizontal or vertical orientation; a subset of cases may demonstrate dysmorphic cortical neurons or balloon cells
- Focal cortical dysplasia may arise in association with other pathologies, most notably hippocampal sclerosis and tumors (gangliogliomas, dysembryoplastic neuroepithelial tumors)
Terminology
- Malformations of cortical development, microdysgenesis
ICD coding
- ICD-10: Q04.8 - other specified congenital malformations of brain
Epidemiology
- No gender predilection
- Most patients present early in life (first 2 decades) with epilepsy
- Variability in definitions and the spectrum of phenotypes for these disorders makes determining prevalence difficult - it is estimated that 15 - 25% of patients referred to epilepsy centers for intractable epilepsy have focal cortical dysplasia (Epilepsia 2011;52:158, Acta Neurol Scand 2006;113:72, J Epilepsy Res 2013;3:43)
- Comprises 15% of pathology in temporal lobe epilepsy resections and nearly 40% of extratemporal lobe resections for epilepsy (J Neuropathol Exp Neurol 1993;52:499, Arch Pathol Lab Med 2000;124:545)
Sites
- Any of the cortical lobes may be affected (frontal and temporal most common)
Pathophysiology
- Not known in most cases
Etiology
- Not known in most cases
- Related to disruptions or distortions of cortical developmental sequences
- Some may have a genetic underpinning minority of cases (e.g., cortical tubers of tuberous sclerosis) (Brain 2012;135:1348, Neuropathol Appl Neurobiol 2018;44:18)
Clinical features
- Seizures most commonly may be associated with developmental delays
- May be asymptomatic
- May not always be evident on imaging (Mod Pathol 2013;26:1051)
- In patients with severe or diffuse lesions: sleep apnea, poor feeding, hypotonia, opisthotonus, spastic quadriplegia, intellectual impairment
Diagnosis
- EEG and imaging studies (high resolution MRI) studies may be useful in localizing seizures
- Pathologic examination of excised tissues to confirm the diagnosis
Radiology description
- Subtle types may not be evident on imaging
- Cortical thickness changes, irregular cortical folding, abnormalities of the gray-white interface, white matter volume reduction, increased signals on FLAIR and T2 images, transmantle sign
Radiology images
Prognostic factors
- International League Against Epilepsy (ILAE) type II focal cortical dysplasia (with dysmorphic neurons or balloon cells demonstrate a high degree of epileptogenicity and do not do as well clinically)
- Widespread or multifocal disease generally also portends a worse prognosis (Pol J Radiol 2012;77:35)
Case reports
- Neonate with seizures occurring within the first day of life (Hum Pathol 2017;63:79)
- 3 year old boy presenting with epilepsia partialis continua (Neurologia 2017;32:478)
- 16 and 17 year old boys with intractable frontal lobe epilepsy associated with meningioangiomatosis (Epileptic Disord 2014;16:533)
- 18 and 35 year old women with seizures and focal cortical dysplasia in upper pre-central gyrus (Epileptic Disord 2015;17:479)
Treatment
- Pharmacologic management is first line treatment
- When epilepsy is pharmacoresistent, surgery may be employed
- Seizure free status range following surgery is 11 - 70%; dependent on a variety of factors including multifocality, presence of multiple pathologies and extent of resection (Neurosurg Clin N Am 2002;13:135)
- mTOR pathway inhibitors may be a novel targeted therapeutic option (Int J Mol Med 2016;38:1327)
Gross description
- Agyria (lissencephaly) and pachygyria: abnormally thickened cortical ribbon
- Polymicrogyria (micropolygyria): small, irregularly formed gyri with shallow sulci
- Heterotopias: nodular or band-like / laminar
- Hemimegalencephaly: asymmetric enlargement of the cerebrum
- Cortical tubers of tuberous sclerosis: expanded gyrus, firm to palpation due to gliosis and calcification
- Most forms show more subtle abnormalities including blurring of the gray-white interface or may not be grossly evident (Perry: Practical Surgical Neuropathology - A Diagnostic Approach, 2nd Edition, 2018)
Gross images
Frozen section description
- Frozen sections not typically used, unless there is a coexistent lesion (e.g., tumor) that is also being excised
Microscopic (histologic) description
- Agyria / pachygyria: 4 layer cortex
- Polymicrogyria: 2 to 4 layer cortex
- Heterotopias: disorganized gray matter tissue (nodular or laminar) situated in a location where it normally is not seen (such as within the white matter)
- Rare cases (some associated with Aicardi syndrome) are marked by accumulation of proteins in astrocytic cytoplasm (hyaline protoplasmic astrocytopathy) (Am J Clin Pathol 2016;146:503)
- ILAE Classification schema outlines patterns seen in focal cortical dysplasia (Epilepsia 2011;52:158):
- Type IA: isolated lesion presenting as radial dyslamination of neocortex
- Type IB: isolated lesion presenting as tangential dyslamination of neocortex
- Type IC: isolated lesion presenting as both radial and tangential dyslamination
- Type IIA: isolated lesion characterized by cortical dyslamination and dysmorphic neurons without balloon cells
- Type IIB: isolated lesion characterized by cortical dyslamination and dysmorphic neurons with balloon cells
- Type IIIA: focal cortical dysplasia in combination with hippocampal sclerosis
- Type IIIB: focal cortical dysplasia in combination with an epilepsy associated tumor
- Type IIIC: focal cortical dysplasia in combination with a vascular malformation
- Type IIID: focal cortical dysplasia in combination with another epileptogenic lesion acquired early in life (traumatic injury, ischemic injury or encephalitis)
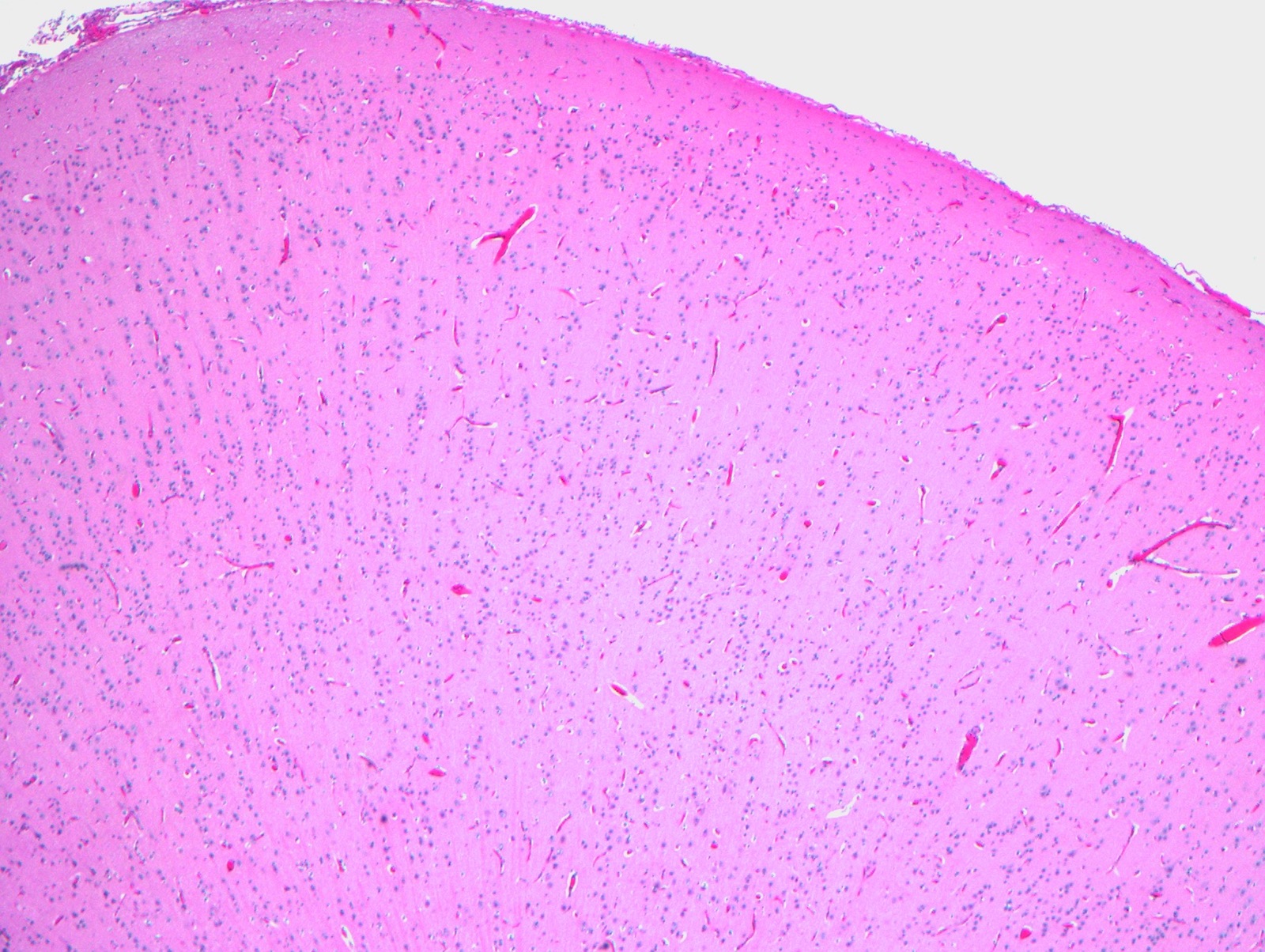
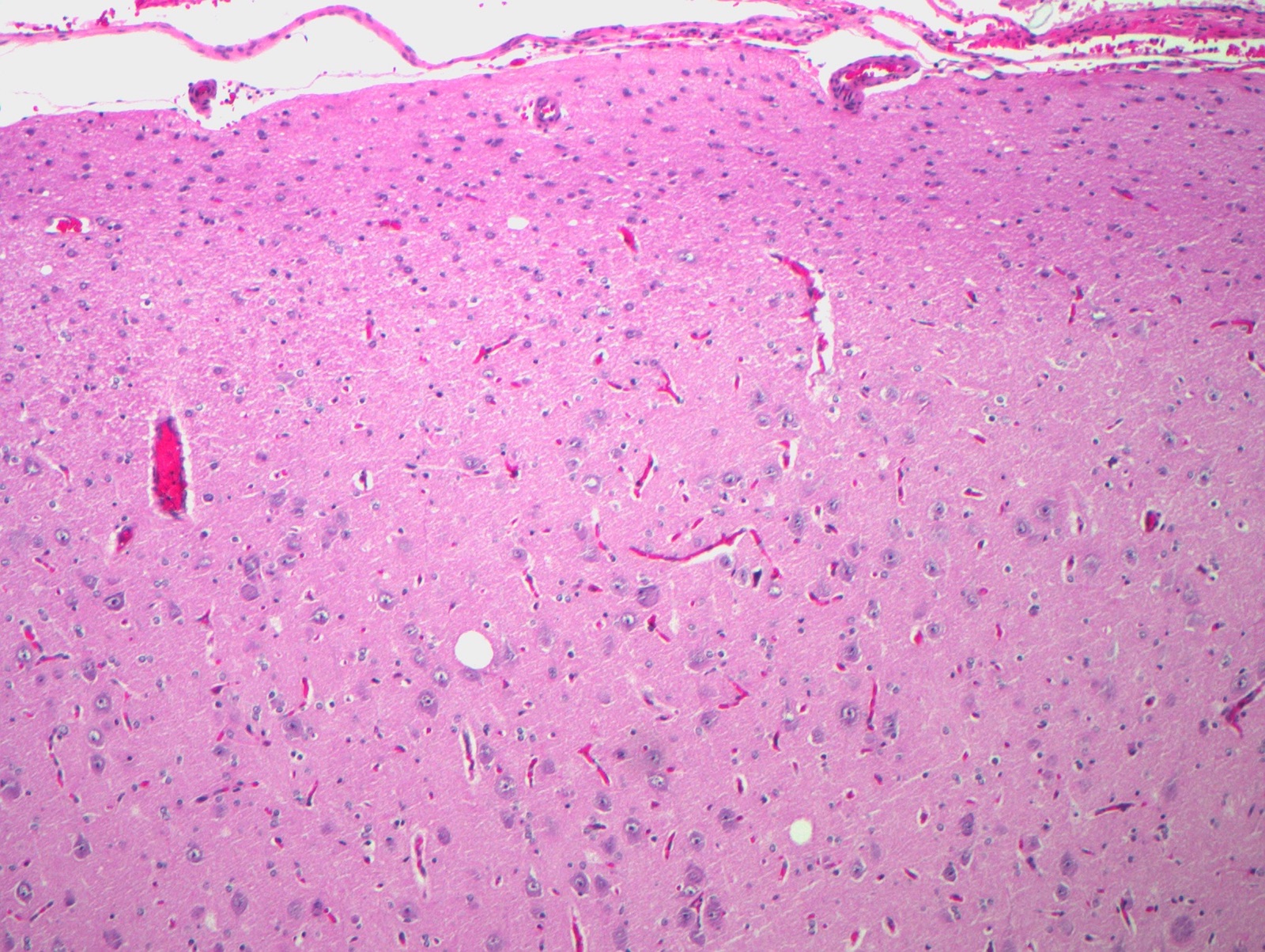
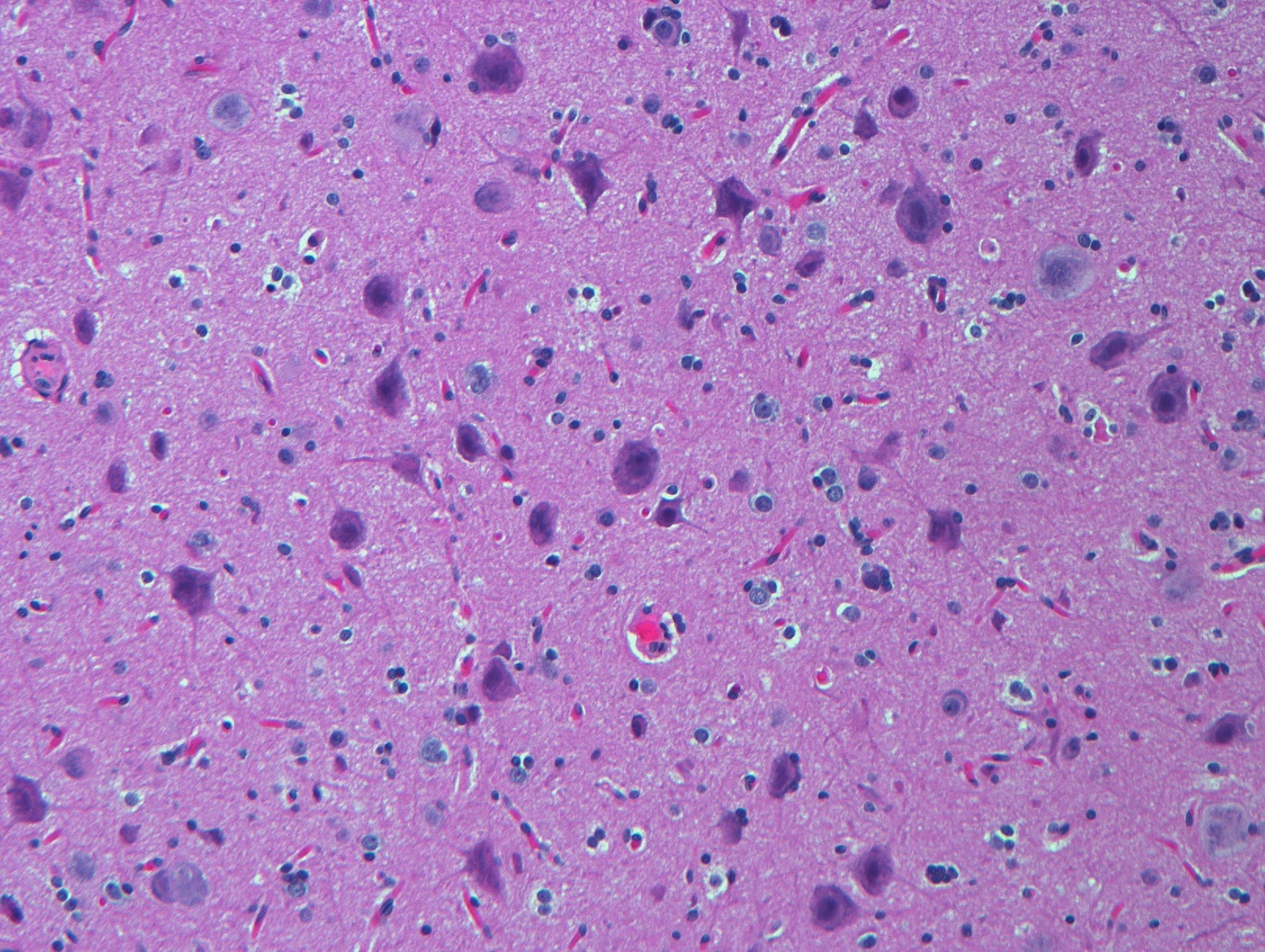
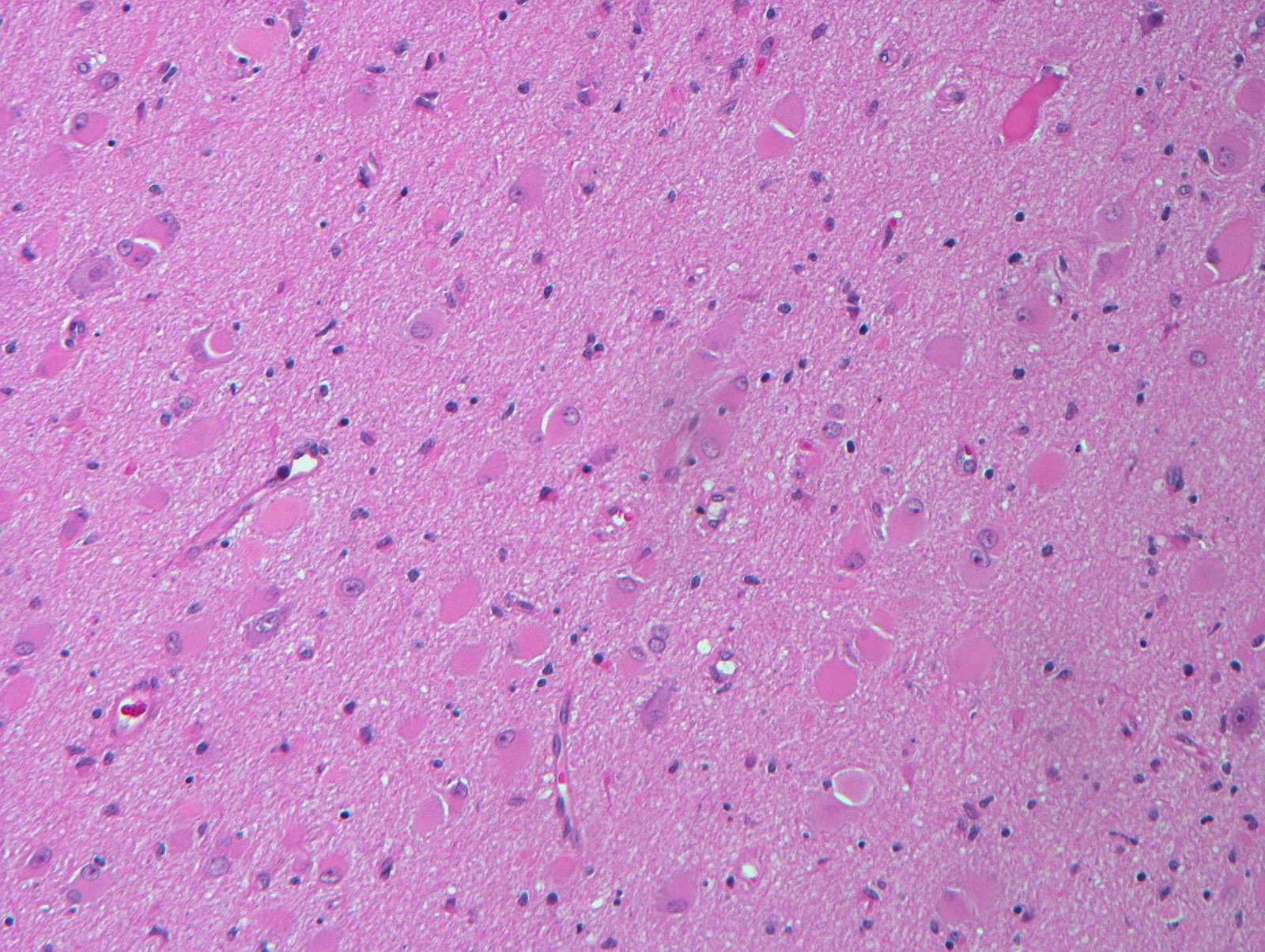
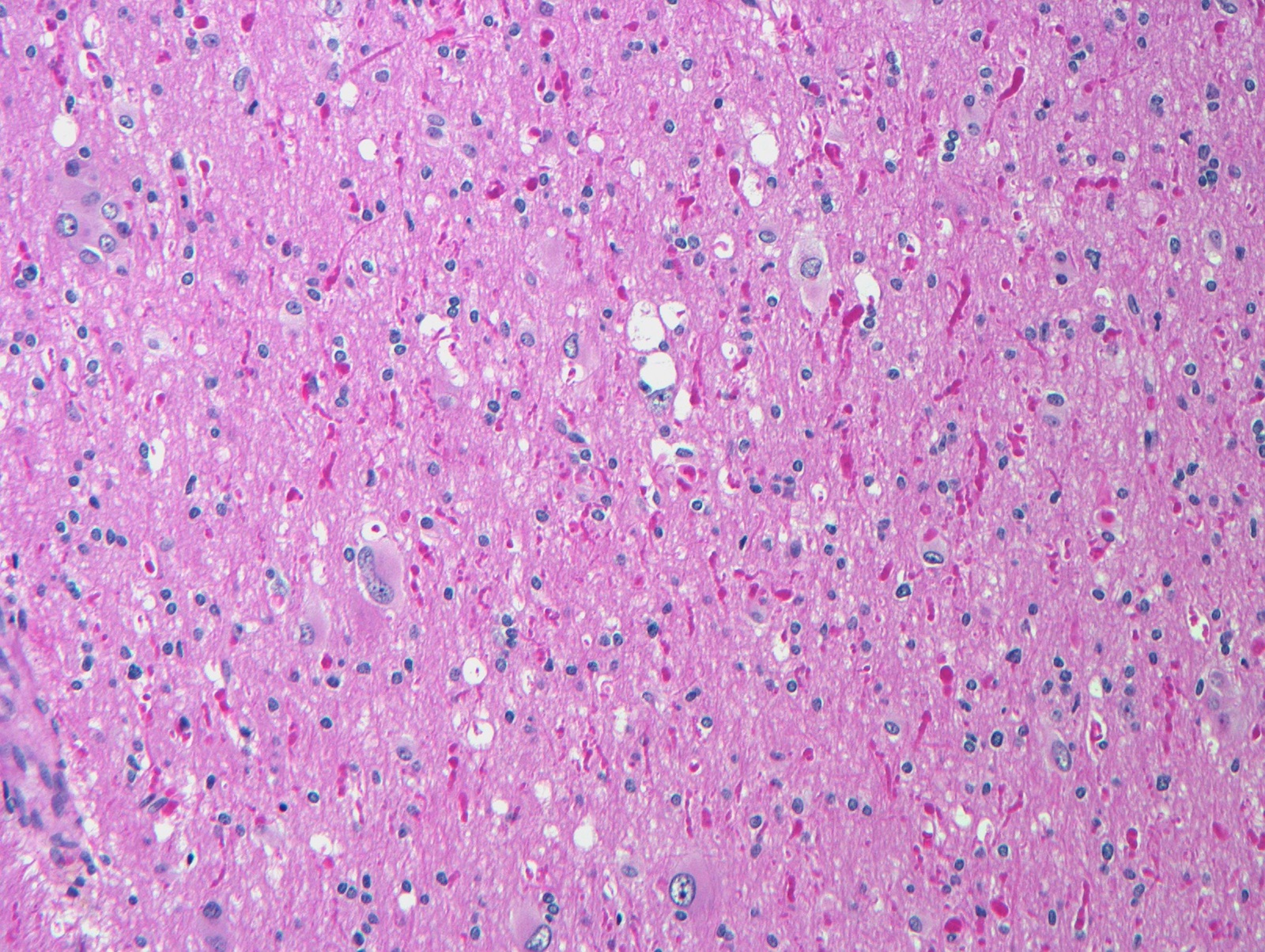
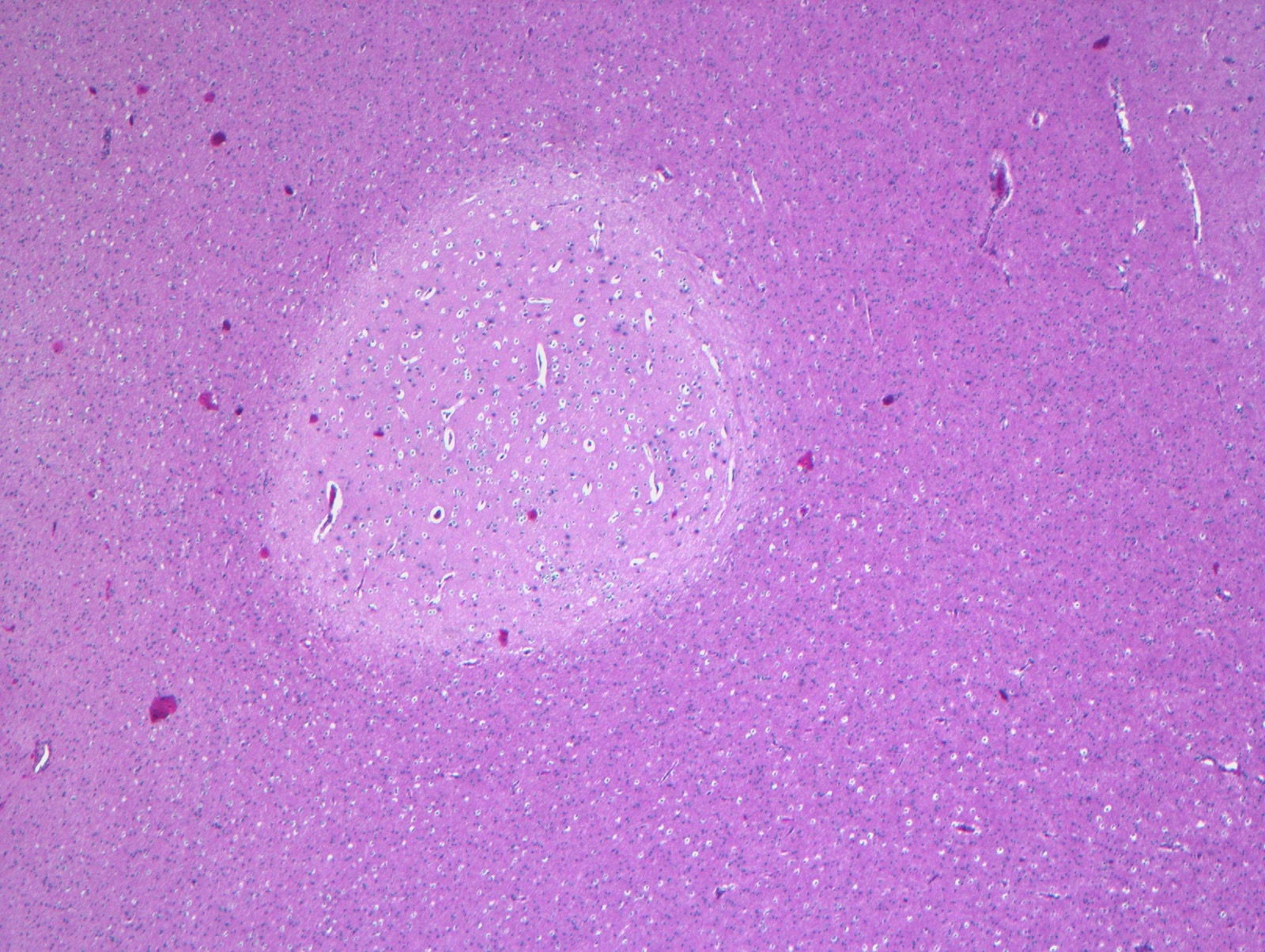
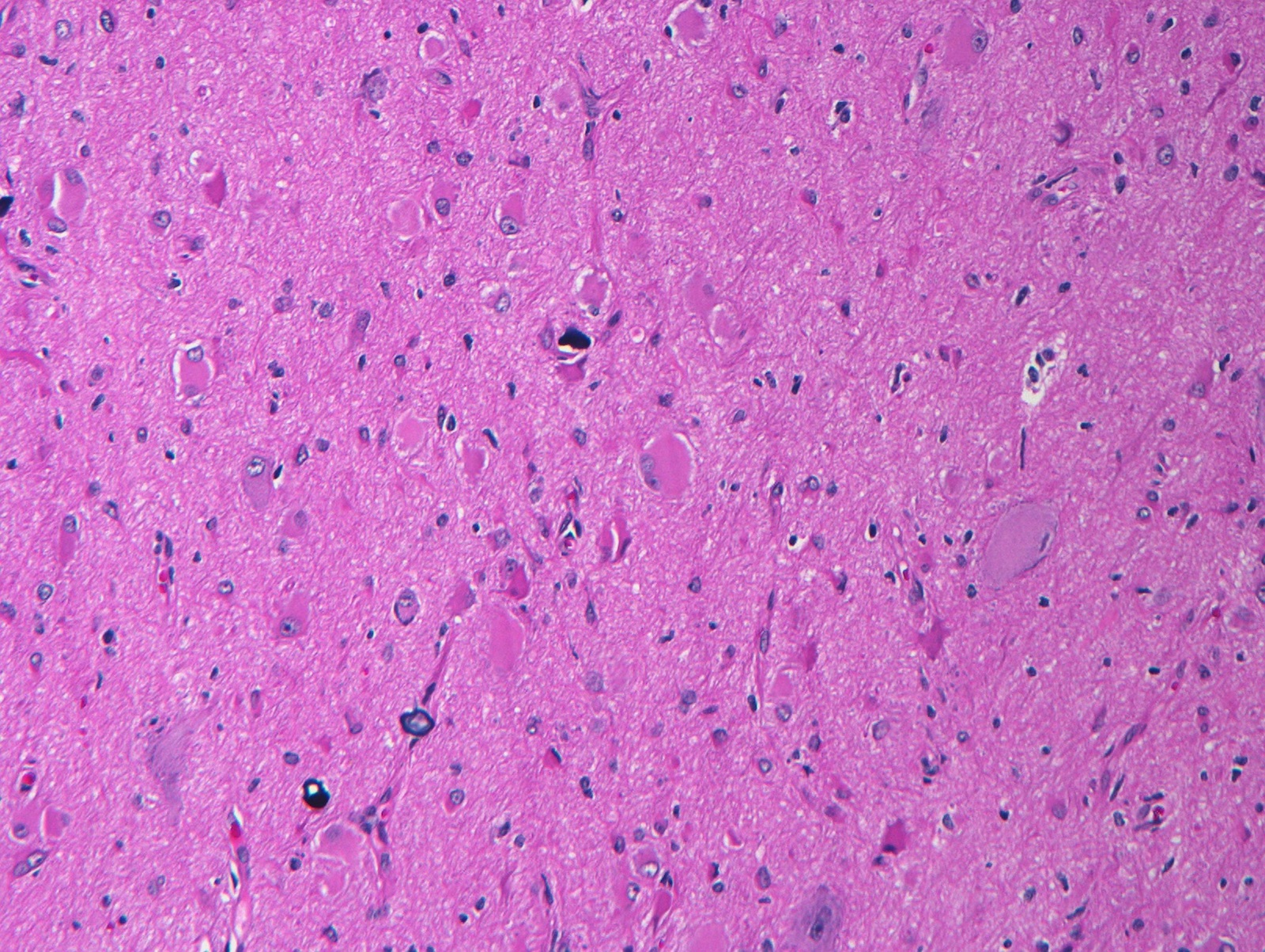
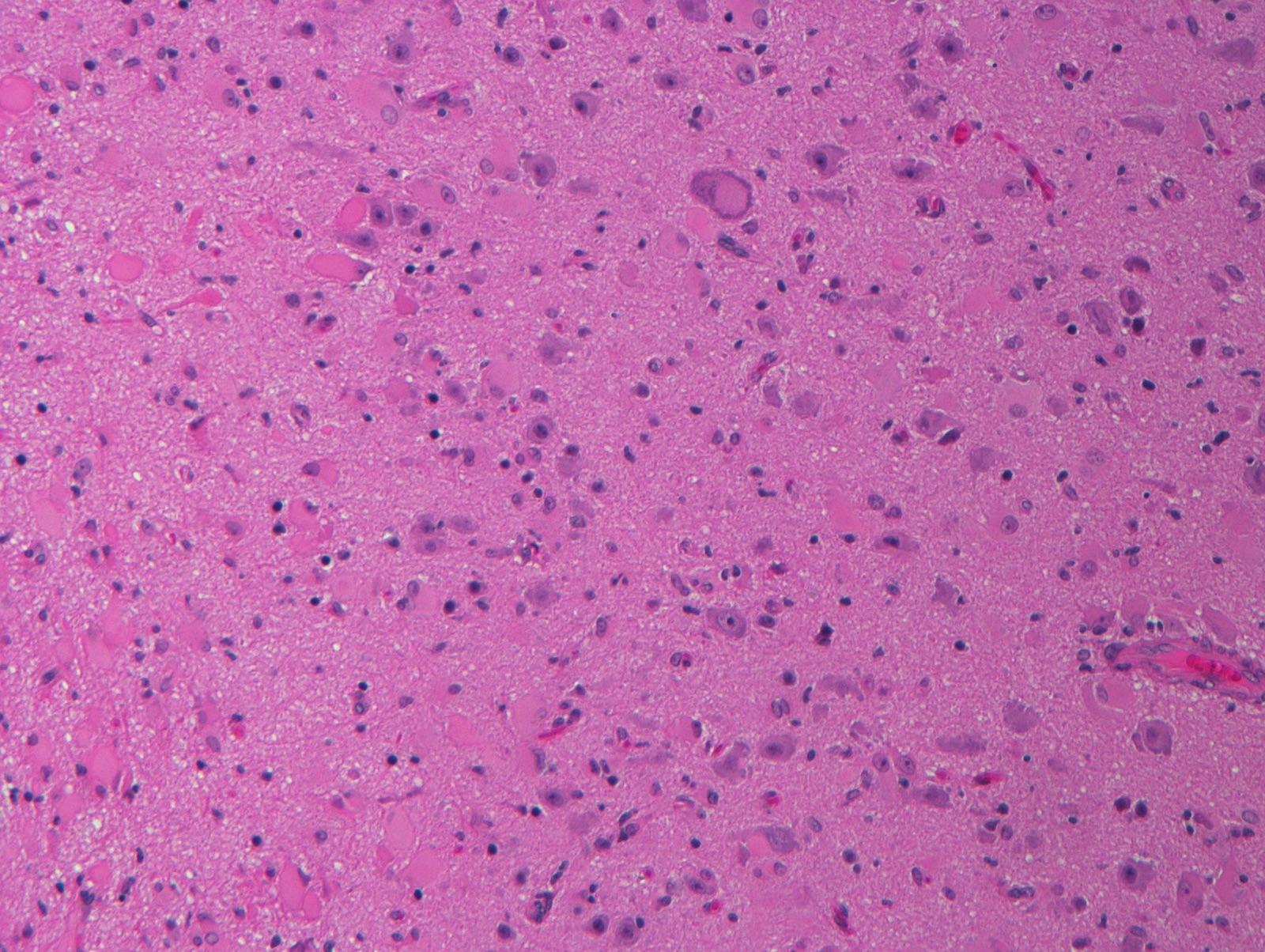
Microscopic (histologic) images
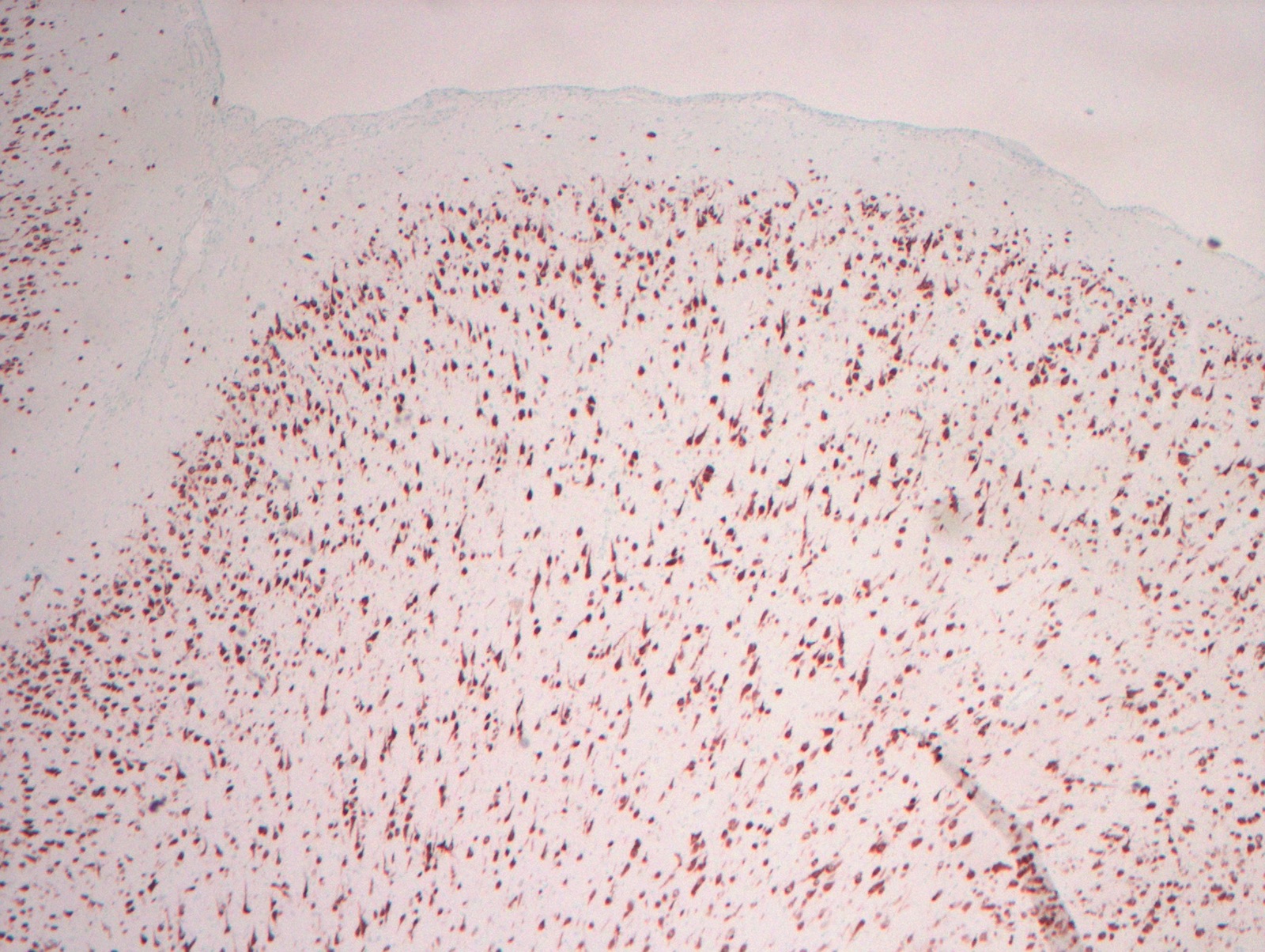
Positive stains
- NeuN highlights neurons and can be helpful in assessing cortical architecture
- GFAP can highlight patterns of gliosis
- MAP2 may be positive in normal neurons and their processes
- CD34 can highlight balloon cells (Epilepsia 2011;52:158)
Molecular / cytogenetics description
- ILAE type II focal cortical dysplasia and hemimegalencephaly: mosaic mTORopathies (abnormalities related to mTOR signalling dysregulation); glycosylation defects seen in a subset (about 30%) of type I focal cortical dysplasia (Acta Neuropathol 2019;138:885)
- Differential hierarchical cluster analysis of DNA methylation can distinguish major focal cortical dysplasia types (Epilepsia 2019;60:1091)
- Pharmacoresistence may be related to a number of factors: MDR1, MRP1, major vault protein (Public Health Nutr 2017;20:786)
Sample pathology report
- Temporal lobe mass, partial excision:
- Ganglioglioma, WHO grade I
- Focal cortical dysplasia (ILAE type IIIB)
Differential diagnosis
- Ganglioglioma:
- May be seen in association with focal cortical dysplasia (ILAE FCD IIIB)
- Have an atypical glioma component (GFAP, SOX10 or Olig2 positive) in addition to the atypical neuronal cell component
- May have eosinophilic granular bodies and may be BRAF V600E +
- Gangliocytoma:
- Presents as a mass, pure ganglion cell tumor
- Architectural changes adjacent to a remote infarct (especially early in life during brain development)
Additional references
Board review style question #1
A 6 year old female patient presents with a history of temporal lobe epilepsy since age 3 years. A variety of pharmacologic treatment regimens have been attempted to control the seizures with varying temporary success. On imaging, she has an area of vague enhancement in the right temporal lobe. Concerned about a possible tumor, the area of enhancement is excised. The pathology is shown here. What is the best diagnosis for the lesion seen here?
- Dysembryoplastic neuroepithelial tumor
- Focal cortical dysplasia ILAE type I
- Focal cortical dysplasia ILAE type II
- Ganglioglioma
- Pleomorphic xanthoastrocytoma
Board review style answer #1
C. Focal cortical dysplasia ILAE type II. The lesion is marked by the presence of dysmorphic neurons and occasional balloon cells, characteristic of focal cortical dysplasia IIB. Focal cortical dysplasia type I does not contain dysmorphic neurons or balloon cells. Dysembryoplastic neuroepithelial tumors are low grade glioneuronal neoplasms marked by multinodularity and a mixture of rounded oligodendroglial-like cells intermixed with normal appearing neuronal cells, often arranged against a microcytic background. Gangliogliomas have an atypical glial cell component along with dysmorphic ganglion cells. Pleomorphic xanthoastrocytomas are characterized by prominent cellularity with an atypical astrocytic component and variable numbers of xanthoastrocytes.
Comment Here
Reference: Focal cortical dysplasia (epilepsy related malformations)
Comment Here
Reference: Focal cortical dysplasia (epilepsy related malformations)
Board review style question #2
Which of the following tumors is most likely to be associated with coexistent focal cortical dysplasia?
- Fibrillary astrocytoma
- Ganglioglioma
- Meningioma
- Oligodendroglioma
- Pilocytic astrocytoma
Board review style answer #2
B. Ganglioglioma. Tumors known to be associated with coexistent focal cortical dysplasia include ganglioglioma, dysembryoplastic neuroepithelial tumor, angiocentric glioma and rare cases of pleomorphic xanthoastrocytoma. The other tumors listed as options with the question are not known to be associated with focal cortical dysplasia.
Comment Here
Reference: Focal cortical dysplasia (epilepsy related malformations)
Comment Here
Reference: Focal cortical dysplasia (epilepsy related malformations)