Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Diagrams / tables | Pathophysiology | Clinical features | Laboratory | Test indications | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Jin Z, Galior KD. Vitamin D. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/chemistryvitamind.html. Accessed April 3rd, 2025.
Definition / general
- Vitamin D plays an important role in the maintenance of calcium and phosphate homeostasis by regulating calcium absorption and osteoclastic / osteoblastic activity
- Plasma concentrations of vitamin D should be interpreted in context with other measures of calcium and phosphate homeostasis, such as parathyroid hormone, calcium, phosphate and alkaline phosphatase
Essential features
- Vitamin D3 is endogenously synthesized in skin exposed to sunlight, whereas vitamin D2 is the dietary form found in plants and fungi
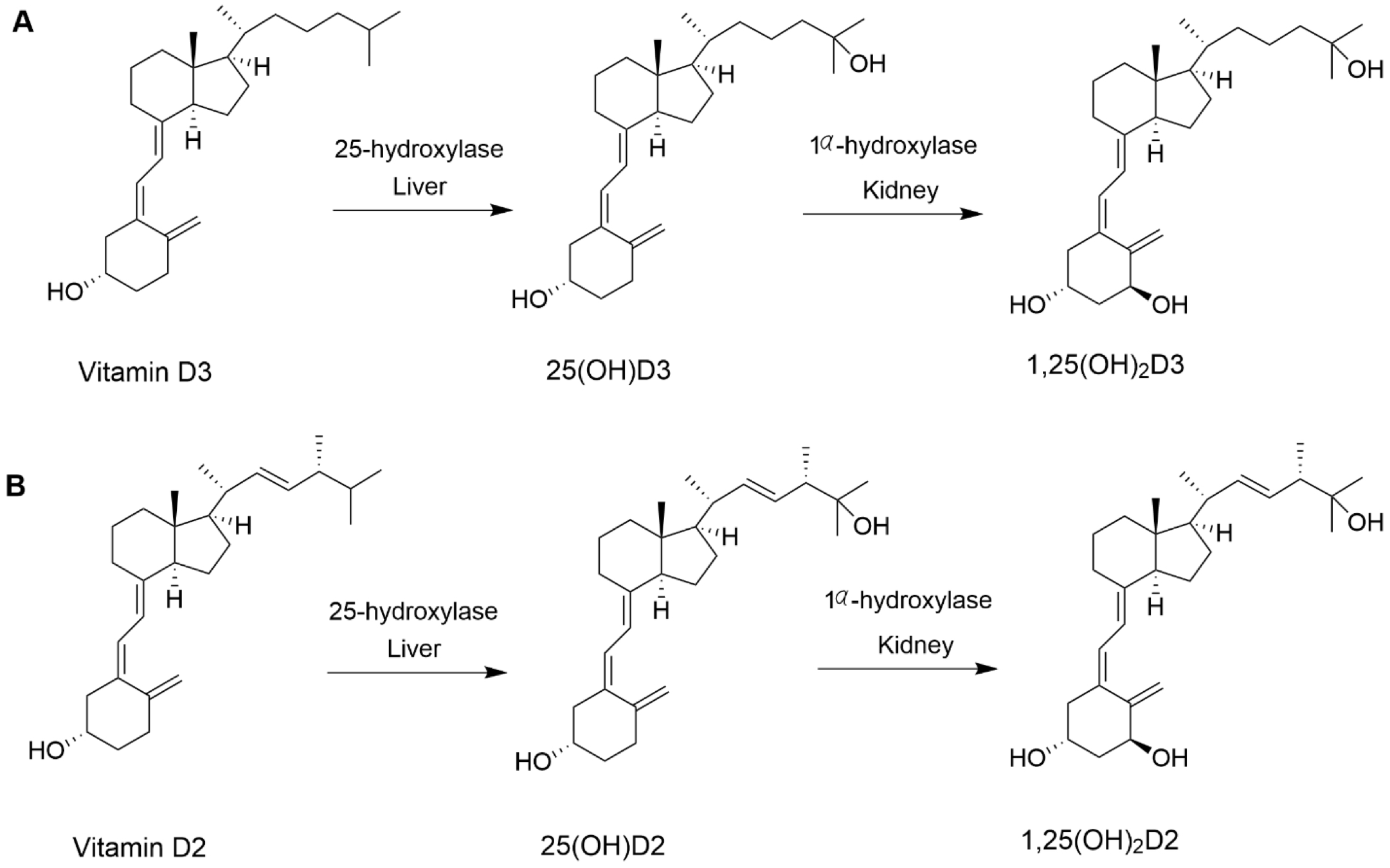
- Vitamin D2 and D3 are converted in the liver to 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3, respectively
- 25-hydroxyvitamin D [25(OH)D] has a long biological half life (2 - 3 weeks) and is the primary form of vitamin D in the body; therefore, it is the best biomarker to assess vitamin D deficiency
- 1,25-dihydroxyvitamin D [1,25(OH)2D] is the biologically active form of the vitamin but has a short half life (~4 hours) and is present in significantly lower concentrations than 25-hydroxyvitamin D
- In the United States, ergocalciferol or vitamin D2 supplement is provided as a high dose oral capsule (50,000 IU); various low dosage vitamin D3 capsule options exist
Terminology
- Vitamin D3: cholecalciferol
- 25-hydroxyvitamin D3: calcidiol, calcifediol, 25-hydroxycholecalciferol, 25(OH)D3
- Vitamin D2: ergocalciferol
- 25-hydroxyvitamin D2: 25-hydroxyergocalciferol, 25(OH)D2
- 1,25-dihydroxyvitamin D: calcitriol, 1,25(OH)2D
ICD coding
- ICD-10: E55 - vitamin D deficiency
Pathophysiology
- Vitamin D3 is synthesized from 7-dehydrocholesterol in the skin exposed to UVB radiation
- Vitamin D2 originates from dietary sources and is found in plants and fungi
- Vitamin D2 and D3 have similar functions; laboratory testing measures the total value of D2 and D3 in the blood
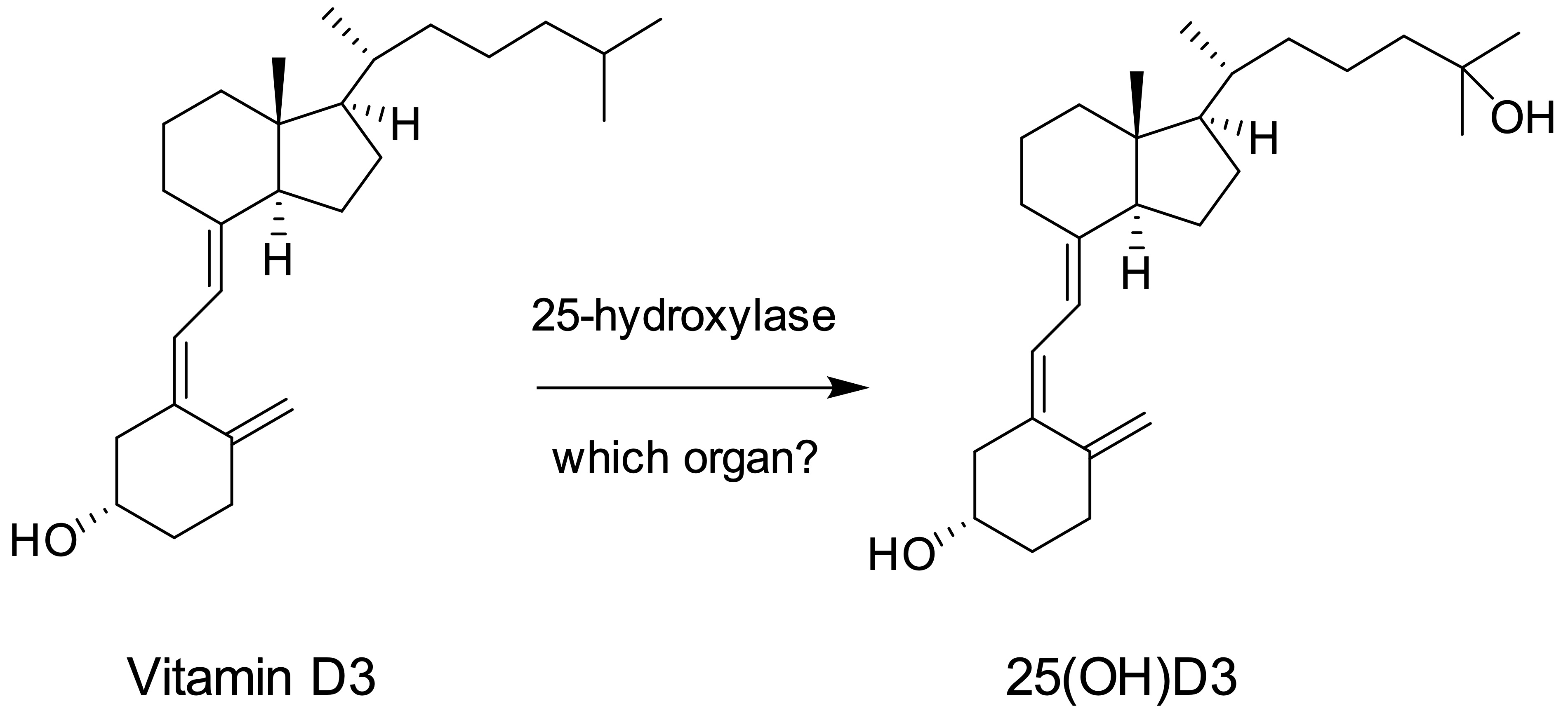
- In the liver, vitamin D is converted to 25(OH)D by 25-hydroxylase
- 25(OH)D is a prohormone that represents the main reservoir and transport form of vitamin D and is bound by a transport protein while in circulation (Am J Clin Nutr 2012;95:1357)
- In renal tubular cells, 25(OH)D is converted to the active form, 1,25(OH)2D, by 1-α-hydroxylase, which is tightly regulated by calcium, phosphate and parathyroid hormone (PTH) concentrations in the body (Nat Rev Endocrinol 2020;16:234)
- Overall effect of vitamin D in the body is to increase calcium and phosphate levels in the blood
- 1,25(OH)2D is transported in the bloodstream to the intestine via binding to vitamin D binding protein (DBP) and promotes absorption of calcium and phosphate in the small intestine
- 1,25(OH)2D also increases osteoclastic activity in bones
- In the kidney, 1,25(OH)2D increases calcium reabsorption by the distal renal tubules and phosphate reabsorption by the proximal tubules through its synergy with PTH (McPherson: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 23rd Edition, 2017)
- 24,25-dihydroxyvitamin D is an inactive vitamin D metabolite produced in the kidney by 24-α-hydroxylase
Clinical features
- Vitamin D deficiency risk factors
- Exclusively breast fed infants
- More common in dark skin than light skin individuals
- Intestinal diseases preventing absorption (e.g. Celiac disease, Crohn’s disease)
- Renal and liver diseases leading to insufficient enzymes for metabolism
- Medications (e.g. phenobarbital and rifampin) can activate hepatic p450 enzymes that lead to vitamin D degradation
- Consequences of vitamin D deficiency
- Hypocalcemia
- Hypophosphatemia
- Rickets (softening of bones in children)
- Osteomalacia and osteoporosis
- Unregulated production of 1,25-dihydroxyvitamin D in sarcoidosis or granulomatous diseases
- Uncommon cause of hypercalcemia
- Elevated calcium with low PTH level
Laboratory
- Methodology to measure levels
- Because of its relatively stable plasma concentration and longer half life, 25(OH)D is the best measure of overall vitamin D status
- Chemiluminescent immunoassay (CLIA) is commonly used on automated instruments for high throughput vitamin D assays in clinical settings
- Vitamin D binding protein concentration and binding kinetics may affect the accuracy of 25-hydroxyvitamin D measured by immunoassay
- Antibodies used in many immunoassays often have lower crossreactivity with 25-hydroxyvitamin D2 and therefore may underestimate total vitamin D activity (Hormones (Athens) 2020;19:97)
- Liquid chromatography tandem mass spectrometry (LC-MS / MS) method is the reference method for the quantification of 25(OH)D and 1,25(OH)2D and can accurately quantitate both vitamin D2 and D3 (Mass Spectrom Rev 2015;34:2)
- Under uncommon circumstances (e.g., chronic renal disease or hypercalcemia), 1,25(OH)2D testing may be indicated
- Diminished levels may be due to reduced 1α-hydroxylase enzyme activity in renal disease, leading to secondary hyperparathyroidism (parathyroid gland hyperplasia)
- Because of its relatively stable plasma concentration and longer half life, 25(OH)D is the best measure of overall vitamin D status
- Test limitations
- Antibodies used in immunoassays for vitamin D have variable reactivity toward 25-hydroxyvitamin D2 and D3, which may result in a bias between different vitamin D immunoassays (Rifai: Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 6th Edition, 2018)
- Presence of inactive vitamin D metabolites may introduce a positive bias for both immunoassays and LC-MS / MS methods (Mass Spectrom Rev 2015;34:2)
- Reference ranges
- Plasma vitamin D concentration is considered insufficient if < 20 ng/mL and deficient if < 10 ng/mL
- Reference range of 25(OH)D is 10 - 65 ng/mL in serum or plasma
- Vitamin D toxicity may occur at concentrations > 100 ng/mL (Rifai: Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, 6th Edition, 2018)
- Reference range of circulating 1,25(OH)2D is 15 - 60 pg/mL (McPherson: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 23rd Edition, 2017)
- Plasma vitamin D concentration is considered insufficient if < 20 ng/mL and deficient if < 10 ng/mL
Test indications
- Vitamin D deficiency results from inadequate dietary intake, intestinal malabsorption, decreased synthesis or defective vitamin D receptors, causing rickets in children and osteomalacia in adults (McPherson: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 23rd Edition, 2017)
- Vitamin D deficiency may cause hypocalcemia, which is followed by increased secretion of PTH (secondary hyperparathyroidism)
- 1-α-hydroxylase deficiency is caused by a mutation in CYP27B1 (chromosome 12q14.1), leading to vitamin D dependent rickets type I
- Hypercalcemia is commonly associated with primary hyperparathyroidism
- Elevated PTH increases the conversion of 25(OH)D to the active form 1,25(OH)2D in the kidney
- Increased 1,25(OH)2D and hypercalcemia may be associated with granulomatous diseases such as sarcoidosis, tuberculosis and granulomas (McPherson: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 23rd Edition, 2017)
Additional references
Board review style question #1
Board review style answer #1
C. Liver. Vitamin D is metabolized to 25(OH)D by 25-hydroxylase in the liver. 25(OH)D is converted to the active form 1,25(OH)2D by 1-α-hydroxylase in renal tubular cells.
Comment Here
Reference: Vitamin D
Comment Here
Reference: Vitamin D
Board review style question #2
- Which of the following is true about the major function of vitamin D?
- Increases the absorption of calcium and phosphate from the gastrointestinal tract
- Maintenance of normal bone formation, turnover and strength
- Raises the circulating calcium concentration while lowering phosphate concentration
- Responsible for the regulation of total body phosphate
- Stimulates parathyroid hormone synthesis and secretion
Board review style answer #2
A. Increases the absorption of calcium and phosphate from the gastrointestinal tract. The active form of vitamin D, 1,25(OH)2D, is transported to the small intestine and promotes absorption of calcium and phosphate from the diet.
Comment Here
Reference: Vitamin D
Comment Here
Reference: Vitamin D