Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) description | Positive stains | Negative stains | Flow cytometry description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Bledsoe J. IgG4 related lymphadenopathy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodesIgG4lymphadenopathy.html. Accessed December 24th, 2024.
Definition / general
- Lymphadenopathy attributable to IgG4 related disease, with distinct clinicopathologic features
Essential features
- Refers to lymphadenopathy that occurs in patients with established IgG4 related disease and is attributable to that disorder
- Because increased IgG4 positive plasma cells are relatively nonspecific in lymph nodes, the term IgG4 related lymphadenopathy should not be used as a general descriptor for a lymph node with increased IgG4 positive plasma cells in a patient without established extranodal IgG4 related disease
- Involved lymph nodes demonstrate both an absolute (> 100 IgG4 positive plasma cells per high power field [HPF]) and relative (IgG4:IgG plasma cell ratio > 40%) increase in IgG4 positive plasma cells
- Various morphologic patterns are described, many of which are nonspecific: 1) Castleman disease-like, 2) follicular hyperplasia, 3) progressive transformation of germinal centers, 4) interfollicular expansion, 5) inflammatory pseudotumor-like as well as infrequent patterns, including infectious mononucleosis-like features
- Features thought to be relatively specific for IgG4 related lymphadenopathy include increased IgG4 positive plasma cells (> 100 per HPF) and IgG4:IgG ratio (> 40%) within expanded interfollicular or fibrotic regions (i.e., interfollicular expansion and inflammatory pseudotumor-like patterns)
ICD coding
Epidemiology
- Most common in middle aged to older adults with a male predominance
- Extremely rare in children
- Lymphadenopathy occurs in at least 40 - 60% of patients with IgG4 related disease (Am J Surg Pathol 2010;34:1812, Arthritis Rheumatol 2015;67:2466)
Sites
- Localized lymphadenopathy in anatomic regions near the site of extranodal IgG4 related disease is most common but distant lymphadenopathy and multifocal / generalized lymphadenopathy occurs in some cases
Pathophysiology
- Pathophysiology of IgG4 related disease is poorly understood
- Both aberrant B cell and T cell activity has been implicated
- B cell depletion as a successful second line treatment for IgG4 related disease has implicated a role of activated B cells in IgG4 related disease; however, recent studies have favored abnormal T cells to be the underlying immunologic defect (N Engl J Med 2012;366:539, Haematologica 2019;104:444)
- T follicular helper cells have been implicated in contributing to IgG4 related disease through cytokines IL21 and IL4, which are thought to contribute to lymphoid follicle formation, class switch to IgG4 and plasmablast induction (Arthritis Rheumatol 2015;67:2476, Arthritis Res Ther 2016;18:167)
- Circulating Tfh2 cells have been shown to be increased in IgG4 related disease and to correlate with serum IgG4 levels (Arthritis Rheumatol 2015;67:2476)
- Treg cells also may contribute to IgG4 related disease through secretion of IL10 and TGF beta resulting in IgG4 class switching and fibrosis (Clin Nephrol 2010;73:385)
- Oligoclonal expansions of CD4+ cytotoxic T cells have been found in blood and tissues of IgG4 related disease patients and have been implicated in contributing to fibrosis (Autoimmunity 2017;50:19)
- Role of IgG4 positive plasma cells in the disease is uncertain
- Some have suggested that IgG4 positive plasma cells are a secondary phenomenon and may be produced in an attempt to dampen the inflammatory process (Clin Exp Allergy 2009;39:469, Gut 2018;67:728)
- IgG4 is a relatively inactive immunoglobulin subclass that is nonprecipitating and behaves much like monovalent antibodies
- IgG assay with the detection of labeled antigen fluid to solid phase cross linking showed that cross linking activity was usually absent in the presence of high serum levels of IgG4 (as measured by radioallergosorbent test [RAST])
- Some have suggested that IgG4 positive plasma cells are a secondary phenomenon and may be produced in an attempt to dampen the inflammatory process (Clin Exp Allergy 2009;39:469, Gut 2018;67:728)
Etiology
- Lymph node involvement by IgG4 related disease
Clinical features
- IgG4 related disease usually presents due to enlargement of an exocrine organ, most commonly submandibular glands, orbit / lacrimal glands or pancreaticobiliary tract, with systemic involvement in ~33% of cases
- Orbit is the most common site in children (Pediatr Rheumatol Online J 2016;14:18)
- Organ enlargement is detected by a visible mass in superficial sites (i.e., orbit or submandibular gland) or due to organ dysfunction from mass effect at deeper sites (i.e., pancreas)
Diagnosis
- Physical exam and imaging play a central role in the diagnosis of IgG4 related disease through demonstration of mass-like lesions and for investigation of lymphadenopathy
- In cases with characteristic organ involvement, physical exam or imaging may prompt consideration of IgG4 related disease and subsequent laboratory testing or biopsy
- However, in many cases, the etiology of the tumefactive lesion of IgG4 related disease is not recognized and there may be clinical suspicion for a neoplastic process, prompting biopsy (Mod Pathol 2012;25:1181)
Laboratory
- Elevated serum IgG4 levels are commonly touted (especially among pathologists) as defining IgG4 related disease; while useful, elevated serum IgG4 is neither sensitive nor specific for the diagnosis of IgG4 related disease
- Sensitivity of elevated serum IgG4 for the diagnosis of IgG4 related disease has been reported from ~50 to 90% and specificity ~60 - 80%, with higher IgG4 levels being more specific (Pediatr Rheumatol Online J 2016;14:18, Ann Rheum Dis 2015;74:14)
- Serum IgG4 levels may also be elevated in other inflammatory and immune disorders and neoplasms, including IgG4 positive plasma cell neoplasms and IgG4 positive B cell neoplasms with plasmacytic differentiation; in the latter, the elevated IgG4 may be associated with a clonal M component on serum protein electrophoresis (SPEP) / immunofixation electrophoresis (IFE) (Mod Pathol 2014;27:375, Am J Clin Pathol 2017;148:215)
- In contrast, the elevated serum IgG4 in IgG4 related disease is polyclonal
- Other useful laboratory values often seen in IgG4 related disease include elevated serum IgE or CRP, decreased complement (C3, C4) levels and peripheral eosinophilia (Pediatr Rheumatol Online J 2016;14:18)
Radiology description
- Imaging findings of mass-like enlargement or fibrosis plays a key role in diagnosis of IgG4 related disease
Prognostic factors
- IgG4 related lymphadenopathy is generally treated in the context of IgG4 related disease in an attempt to prevent irreversible organ damage rather than as an attempt to correct the lymphadenopathy (Int J Clin Exp Pathol 2017;10:10153)
- Natural history of IgG4 related disease is variable, ranging from spontaneous improvement in rare cases, a good and durable response to initial therapy in many cases, to progressive organ damage in some cases
- Involvement of vital organs including the heart, aorta and kidneys may be associated with more severe outcomes
- Flares of activity may result in complications such as exocrine dysfunction of various organs and diabetes mellitus in IgG4 related pancreatitis
- Morbidities associated with treatment, such as long term steroid therapy, are also a consideration (Clin Chest Med 2019;40:583)
Case reports
- 48 year old woman with longstanding lymphadenopathy and development of pancreatitis and kidney disease (Mod Rheumatol Case Rep 2023;7:192)
- 58 year old man with jaundice, elevated transaminases and inguinal and axillary lymphadenopathy (Surg Exp Pathol 2020;3:30)
- 66 year old woman with a thyroid mass and lymphadenopathy (Diagn Pathol 2018;13:3)
Treatment
- Treatment varies from watchful waiting in cases of IgG4 related disease with isolated lymphadenopathy or minimal salivary gland enlargement to prompt treatment of cases in which vital organs are involved
- Most patients have good responses to glucocorticoids but may relapse after treatment
- Rituximab is used as a second line agent in cases of recurrent or refractory disease (Arthritis Rheumatol 2015;67:1688)
- Other agents have been used in combination with glucocorticoids including cyclophosphamide, azathioprine or methotrexate
Gross description
- Lymph nodes are enlarged with variable cut surface ranging from fleshy to nodular and fibrotic
Microscopic (histologic) description
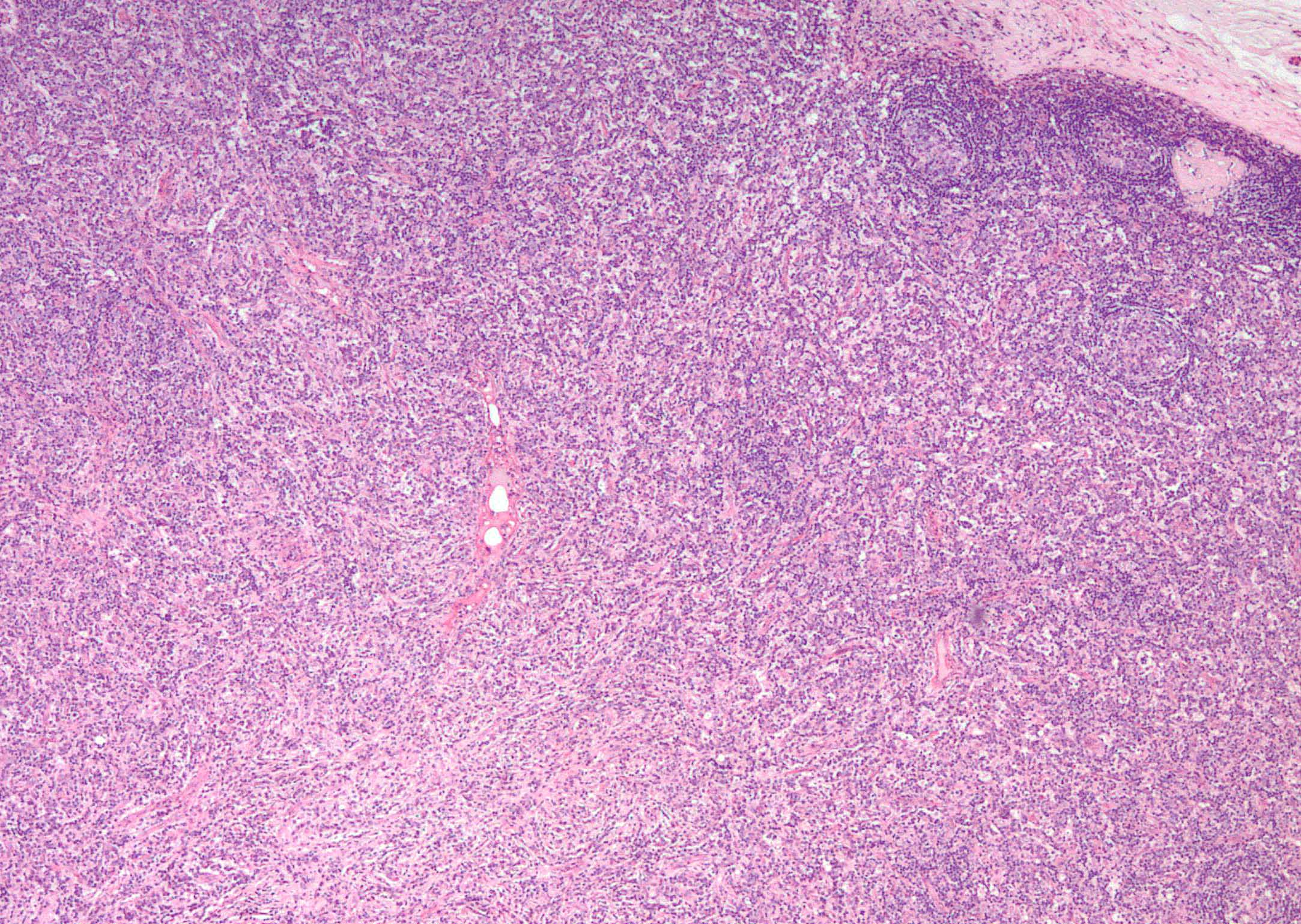
- Enlarged lymph node with various reactive morphologic patterns (described below), increased plasma cells typically in extrafollicular locations (i.e., between follicles) and variable fibrosis that may be capsular, parenchymal or inflammatory pseudotumor-like (Am J Surg Pathol 2021;45:178)
- Increased number (> 100 per HPF) of IgG4 positive plasma cells and increased ratio of IgG4:IgG positive plasma cells (> 40%) is required for the diagnosis of IgG4 related lymphadenopathy
- These parameters are increased in the lymph nodes of most patients with enlarged lymph nodes and established extranodal IgG4 related disease; however, in a subset of patients with known IgG4 related disease and enlarged lymph nodes, the lymph nodes will not show an increase of IgG4 positive plasma cells
- Eosinophils are almost always present admixed with the plasma cells in IgG4 related disease and IgG4 related lymphadenopathy, a useful morphologic clue
- Presence of increased IgG4 positive plasma cells and IgG4:IgG ratio in regions of nodal fibrosis or in extrafollicular regions appears more specific for true IgG4 related disease than an isolated increase in intrafollicular IgG4 positive plasma cells; increased IgG4 positive cells and IgG4:IgG ratio found only within follicles / germinal centers can be seen in many nonspecific causes of lymphadenopathy (Am J Surg Pathol 2021;45:178)
- 5 main morphologic patterns of IgG4 related lymphadenopathy are classically described
- These patterns are nonspecific in the absence of increased IgG4 immunostaining parameters as described above
- On H&E alone, none of these patterns are specific for IgG4 related disease but the presence of these patterns along with nodal plasmacytosis should prompt work up for IgG4 related lymphadenopathy
- Multicentric Castleman disease-like pattern
- Increased IgG4 positive cells outside of follicles
- Lollipop follicles with a penetrating vessel and onion skin arrangement of mantle zone B cells
- Variable fibrosis
- In true Castleman disease follicles are atrophic, whereas in this pattern of IgG4 related disease follicles are more often normal sized or hyperplastic
- Follicular hyperplasia pattern
- Enlarged reactive follicles
- Classically described with increased extrafollicular IgG4 positive plasma cells
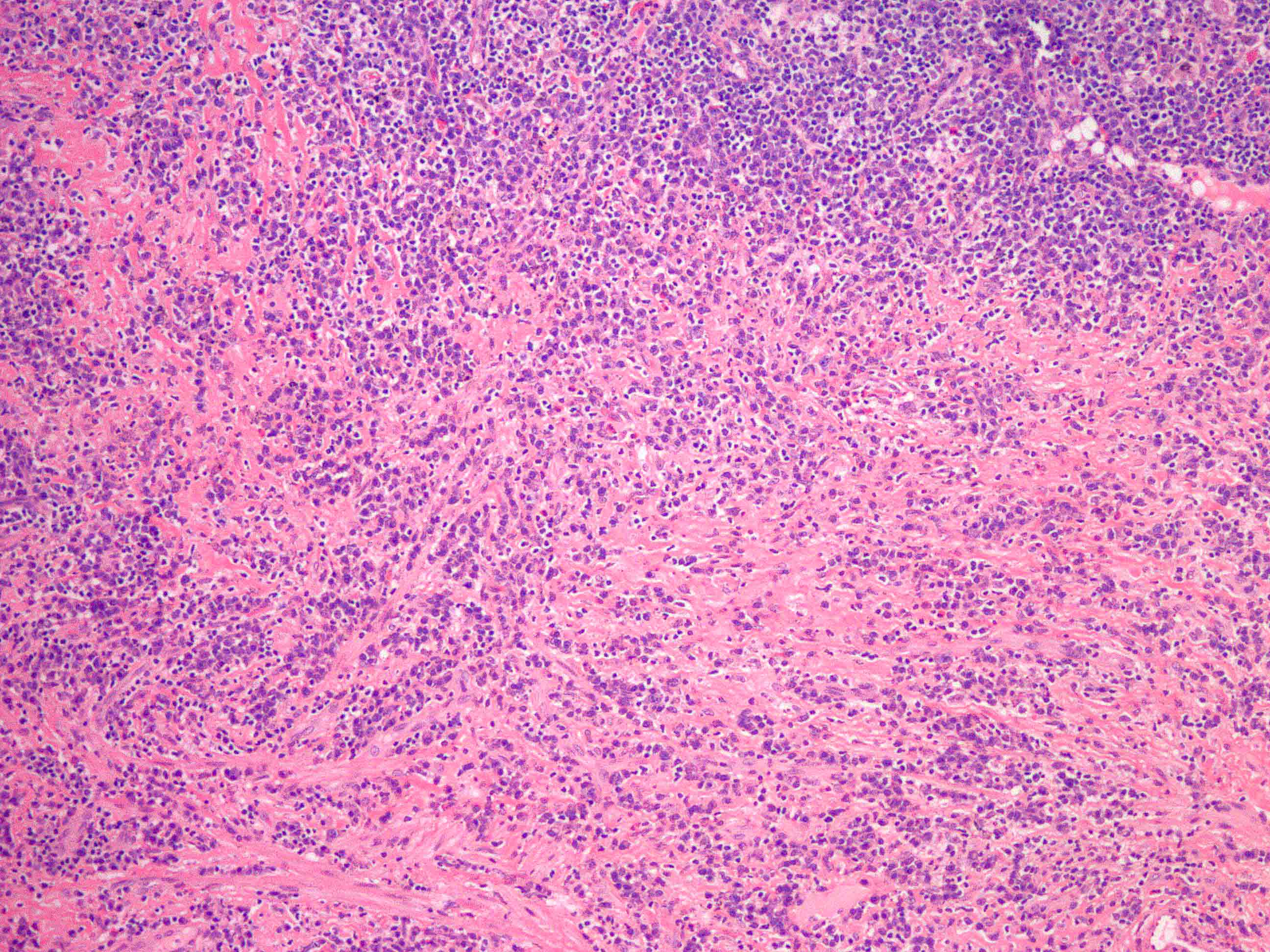
- Interfollicular expansion pattern
- Markedly expanded interfollicular zones with few widely separated residual follicles
- Interfollicular zones contain small lymphocytes, plasma cells, eosinophils, histiocytes and immunoblasts
- Plasma cells are predominantly IgG4 positive
- Morphologic features may be reminiscent of angioimmunoblastic T cell lymphoma
- This pattern has been shown to be highly specific for IgG4 related disease (Am J Surg Pathol 2021;45:178)
- Progressive transformation of germinal centers (PTGC) pattern
- Follicular hyperplasia with frequent PTGC
- This pattern is classically associated with increased intrafollicular IgG4 positive plasma cells
- Some studies have suggested that when this pattern is present in submandibular / cervical lymph nodes it is associated with concurrent of subsequent development of submandibular IgG4 related sclerosing sialadenitis (Mod Pathol 2012;25:956)
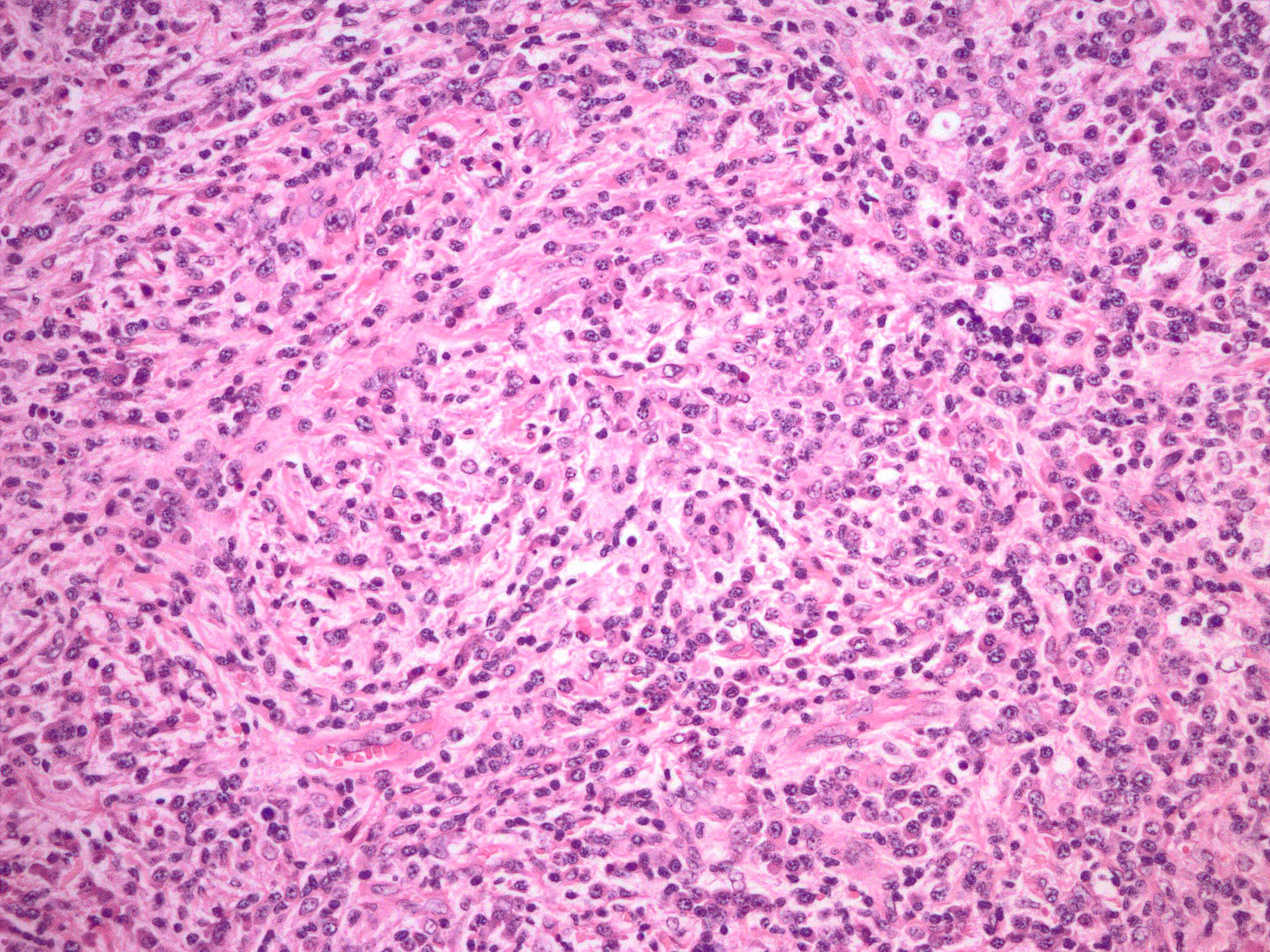
- Inflammatory pseudotumor-like pattern
- Broad areas of fibrosis replacing lymph node parenchyma
- Storiform fibrosis is common
- Increased IgG4 positive plasma cells and IgG4:IgG ratio within the fibrosis
- This pattern has been shown to be highly specific for IgG4 related disease (Am J Surg Pathol 2021;45:178)
- Multicentric Castleman disease-like pattern
- Other uncommon patterns have been described, including infectious mononucleosis-like and rarely Rosai-Dorfman-like changes (Am J Surg Pathol 2018;42:977)
- Other morphologic features that may be present include ring-like perifollicular granulomas or phlebitis
- Significant neutrophilic inflammation is typically not present in IgG4 related disease or IgG4 related lymphadenopathy
Microscopic (histologic) description
Positive stains
- IgG4: the presence of > 100 IgG4 positive plasma per HPF in the regions with the highest number of IgG4 positive cells (site dependent; i.e., highest in skin)
- IgG4:IgG: IgG4 positive plasma cells are > 40% of total IgG positive plasma cells in the regions with the highest number of IgG4 positive cells (regardless of site) (Haematologica 2019;104:444)
- CD138: may be useful to aid in quantification if IgG stain shows high background staining
- Kappa / lambda IHC or ISH: plasma cells are polytypic in IgG4 related disease; if monotypic, then consider an IgG4 positive plasma cell or B cell neoplasm with plasmacytic differentiation
- Elastic stain may be useful to demonstrate obliterative phlebitis, a useful feature for extranodal IgG4 related disease but uncommonly present in lymph nodes
Negative stains
- Spirochete / treponemal IHC and silver stains (syphilitic lymphadenitis may mimic IgG4 related lymphadenopathy) (Arch Pathol Lab Med 2024;148:633)
- HHV8 (excludes HHV8 positive Castleman disease)
- ALK1
- ROS1
Flow cytometry description
- Reactive pattern with polytypic B cells and plasma cells and immunophenotypically normal T cells
Molecular / cytogenetics description
- IgG4 related disease and IgG4 related lymphadenopathy are nonneoplastic disorders and should not show molecular or cytogenetic abnormalities
- When the differential diagnosis includes neoplastic entities, including IgG4 positive plasma cell neoplasms, IgG4 positive B cell lymphomas with plasmacytic differentiation, inflammatory myofibroblastic tumor or others, molecular / cytogenetic testing may be useful
Sample pathology report
- Lymph node, excision:
- Enlarged lymph node with fibrosis and increased IgG4 positive plasma cells (see comment)
- Comment: The lymph node is enlarged with follicular hyperplasia, capsular fibrosis and foci of parenchymal fibrosis. There are frequent plasma cells with fewer admixed eosinophils within the regions of fibrosis and present between follicles. Immunohistochemistry for IgG4 and IgG show increased IgG4 positive plasma cells (up to 165 per HPF) and IgG4:IgG ratio of ~70% within interfollicular and fibrotic regions. Plasma cells demonstrate polytypic expression of kappa and lambda light chains by in situ hybridization. A spirochete (Treponema) immunostain is negative.
- Increased IgG4 positive plasma cells may be seen in lymph nodes in various conditions including IgG4 related disease, Castleman disease and other inflammatory and infectious processes. The presence of increased IgG4 staining parameters within fibrosis and interfollicular regions of enlarged lymph nodes, as seen in this case, has been described as a relatively specific finding for IgG4 related disease. Therefore, in this patient without a history of established extranodal IgG4 related disease, the findings are suspicious for IgG4 related lymphadenopathy; however, further investigation for an extranodal site of IgG4 related disease and laboratory testing including serum IgG4, IgE and complement (C3 / C4) levels may be useful for definitive diagnosis of IgG4 related disease.
Differential diagnosis
- Increased IgG4 positive plasma cells can be seen in various reactive and neoplastic disorders involving lymph nodes
- Rosai-Dorfman disease (RDD):
- May have increased IgG4 positive plasma cells and IgG4:IgG ratio
- Hallmark is enlarged histiocytes with atypical nuclei and emperipolesis
- RDD histiocytes are positive for S100, OCT2 and cyclin D1 (Am J Surg Pathol 2021;45:35, Br J Haematol 2019;186:837)
- Histiocyte emperipolesis may be seen extremely rarely in IgG4 related lymphadenitis as a focal finding and without cytologic atypia
- Castleman disease:
- Lymph nodes in hyper-IL6 syndromes, including Castleman disease and rheumatoid arthritis, may contain increased IgG4 positive plasma cells, typically in the setting of interfollicular plasmacytosis
- Plasma cell type of Castleman disease typically contains regions with sheets of plasma cells without admixed eosinophils and with associated hemosiderin, a finding that would be uncommon in IgG4 related disease
- Neutrophils may be seen in lymph nodes of hyper-IL6 syndromes and are not seen in IgG4 related lymphadenopathy
- Castleman disease follicles are typically atrophic while follicles in the Castleman disease-like pattern of IgG4 are more often normal sized to hyperplastic
- HHV8 positive plasmablasts within Castleman disease type follicles supports the diagnosis of HHV8 associated Castleman disease
- Plasma cell neoplasm expressing IgG4:
- IgG4 positive plasma cells are clonal by IHC / ISH for kappa and lambda light chains
- Serum IgG4 may be elevated
- SPEP / IFE may show M component
- B cell lymphoma with plasmacytic differentiation expressing IgG4:
- Usually nodal or extranodal marginal zone lymphoma
- IgG4 positive plasma cells are clonal by IHC / ISH for kappa and lambda light chains
- Serum IgG4 may be elevated
- SPEP / IFE may show M component
- Inflammatory myofibroblastic tumor (Am J Surg Pathol 2019;43:314):
- May demonstrate marked morphologic overlap with IgG4 related disease, including storiform fibrosis, plasmacytosis with increased IgG4 positive plasma cells and IgG4:IgG ratio and even obliterative phlebitis
- Stromal cells demonstrate cytologic atypia, a finding not seen in IgG4 related disease
- ALK1 and ROS1 immunohistochemistry or fusion analysis may be useful when inflammatory myofibroblastic tumor is suspected
- Angioimmunoblastic T cell lymphoma (AITL):
- Morphologic overlap with interfollicular expansion pattern of IgG4 related lymphadenopathy
- IgG4 positive plasma cells are not typically increased in AITL
- T cells demonstrate a Tfh immunophenotype and clonal TCR gene rearrangement, may demonstrate aberrant loss of pan-T cell markers and are associated with expanded follicular dendritic cell meshworks
- Syphilitic lymphadenitis:
- May closely mimic the morphology of IgG4 related disease and IgG4 related lymphadenopathy, including plasmacytosis, fibrosis and phlebitis
- Treponemal immunohistochemistry demonstrates spirochetes
- Laboratory for syphilis may be useful
- IgG4 positive plasma cells are usually not increased in syphilis but can be in some cases (Am J Surg Pathol 2018;42:472)
- Chronic infections including mastoiditis, aortitis
- Kimura disease:
- More extensive eosinophil infiltrates including eosinophilic microabscesses
- IgE deposition in follicles
- IgG4 positive plasma cells not typically increased in Kimura disease
- Angiolymphoid hyperplasia with eosinophilia / epithelioid hemangioma:
- Nonspecific inflammation adjacent to other tumors:
- Increased IgG4 positive plasma cells can be seen in soft tissue adjacent to other tumors; correlation with imaging and clinical suspicion is needed in such cases to avoid misdiagnosis as IgG4 related disease
Board review style question #1
A 65 year old man presents with bilateral enlargement of the submandibular glands and submandibular lymph nodes. An enlarged submandibular lymph node is excised. What stain is most likely to aid in rendering the correct diagnosis?
- Cyclin D1
- EBER in situ hybridization
- HHV8
- IgG and IgG4 immunostains
- Toxoplasma immunostain
Board review style answer #1
D. IgG and IgG4 immunostains. The photomicrographs show marked fibrosis with a mixed inflammatory cell infiltrate including many plasma cells and eosinophils. Areas of storiform fibrosis are present. Along with the clinical history of bilateral submandibular gland enlargement, the morphologic findings should prompt consideration of the inflammatory pseudotumor-like pattern of IgG4 related lymphadenopathy. IgG4 and IgG immunostains are necessary for further evaluation.
Answer A is incorrect because cyclin D1 is positive in Rosai-Dorfman disease. Answer B is incorrect because while EBER positivity can occasionally be seen in IgG4 lymphadenopathy, it would not aid in diagnosis. Answer C is incorrect because HHV8 positive plasmablasts support the diagnosis of HHV8 associated Castleman disease. Answer E is incorrect because this positive immunostain would indicate Toxoplasma infection.
Comment Here
Reference: IgG4 related lymphadenopathy
Answer A is incorrect because cyclin D1 is positive in Rosai-Dorfman disease. Answer B is incorrect because while EBER positivity can occasionally be seen in IgG4 lymphadenopathy, it would not aid in diagnosis. Answer C is incorrect because HHV8 positive plasmablasts support the diagnosis of HHV8 associated Castleman disease. Answer E is incorrect because this positive immunostain would indicate Toxoplasma infection.
Comment Here
Reference: IgG4 related lymphadenopathy
Board review style question #2
A 60 year old woman presents with jaundice, a pancreatic mass and abdominal lymphadenopathy. Biopsy of the pancreas and peripancreatic lymph node demonstrates marked fibrosis with a storiform pattern, frequent plasma cells and obliterative phlebitis in the pancreas. What is the most likely diagnosis?
- Desmoplastic small round cell tumor
- IgG4 related disease and IgG4 related lymphadenopathy
- Lymphoma
- Pancreatic ductal adenocarcinoma
- Pancreatic neuroendocrine tumor
Board review style answer #2
B. IgG4 related disease and IgG4 related lymphadenopathy. The morphologic description, including storiform fibrosis, obliterative phlebitis and plasmacytosis, is classic for IgG4 related disease. Immunohistochemistry for IgG4 and IgG will show increased IgG4 positive plasma cells and IgG4:IgG ratio.
Answers A and D are incorrect because although these entities show marked desmoplasia, desmoplastic small round cell tumor lacks plasma cells and has a characteristic EWSR1::WT1 gene fusion and pancreatic ductal adenocarcinoma is composed of infiltrating, well to poorly formed glandular / ductal structures. Answer C is incorrect due to the lack of lymphoma cells. If the plasma cells were atypical, a plasma cell neoplasm might be in the differential. Answer E is incorrect because pancreatic neuroendocrine tumors typically lack marked desmoplasia and are composed of small, round, monotonous cells that have coarse salt and pepper nuclear chromatin and minimal atypia but do not resemble plasma cells.
Comment Here
Reference: IgG4 related lymphadenopathy
Answers A and D are incorrect because although these entities show marked desmoplasia, desmoplastic small round cell tumor lacks plasma cells and has a characteristic EWSR1::WT1 gene fusion and pancreatic ductal adenocarcinoma is composed of infiltrating, well to poorly formed glandular / ductal structures. Answer C is incorrect due to the lack of lymphoma cells. If the plasma cells were atypical, a plasma cell neoplasm might be in the differential. Answer E is incorrect because pancreatic neuroendocrine tumors typically lack marked desmoplasia and are composed of small, round, monotonous cells that have coarse salt and pepper nuclear chromatin and minimal atypia but do not resemble plasma cells.
Comment Here
Reference: IgG4 related lymphadenopathy